The proportion of people living with HIV (PLWHIV) that are older than 50 years has been growing worldwide and, according to predictive models, up to 50% of PLWHIV in high-income countries will be over 50 years old (yo) in the next few years [Reference Kirk and Goetz1, Reference Smit2]. Globally, an estimated 110 000 people aged 50 years or over acquire HIV every year [3]. The latter and increases in life-expectancy of PLWHIV contribute to this demographic change [Reference Kirk and Goetz1]. This trend poses important challenges to health systems, such as the provision of care for co-morbidities resulting from natural aging, effects of chronic inflammation, polypharmacy and lack of guidelines for comprehensive care of elderly patients [Reference Martin, Fain and Klotz4].
According to UNAIDS, between 13% and 15% of adults living with HIV in Latin America and the Caribbean are currently aged 50 or more [5]. In fact, this region has experienced one of the fastest and largest growths of PLWHIV older than 50 years [5]. Nonetheless, these figures come from mathematical models with limited empirical validation [Reference Silhol6]. Previous studies have found discrepancies in model estimates that were likely due to lack of representativeness among certain subpopulations, such as local region, gender or age groups [Reference Silhol6–Reference Eaton8]. More information about the growth of this population can contribute to improved precision and accuracy of regional estimates of the aging population living with HIV. Moreover, as older PLWHIV are more likely to have comorbidities than similarly aged people without HIV, [Reference Guaraldi9] accurate estimates of the numbers older than 50 and temporal trends in our region would help to build models of care and costs for this group in the coming years. Also, PLWHIV ⩾50yo and aging in care may contribute differently to the burden of non-communicable diseases than those who are diagnosed or infected later in life [Reference Guaraldi9–Reference Belaunzaran-Zamudio12]. Therefore, in this study we aimed to quantify the proportion of people receiving care for HIV that are 50 years or older (⩾50yo) in a multi-site cohort of clinics in Latin America and the Caribbean between 2000 and 2015 and to estimate the contribution that people enrolled before or after 50 years of age had on the growth of this population over time.
We used data from all adult patients (⩾18 years), actively receiving care for HIV during each calendar year (2000–2015) in centers affiliated with the Caribbean, Central and South American network for HIV Epidemiology (CCASAnet). CCASAnet comprises a consortium of HIV health care centers from seven countries (Argentina, Brazil, Chile, Haiti, Honduras, Mexico and Peru) established in 2006 that share anonymised clinical data to study the epidemiology of HIV-infection in our region [Reference McGowan10]. For every calendar year between 2000 and 2015, we generated a cohort of adult patients retained in care for that year. We defined ‘retained in care’ as those patients who had at least one visit after 15 July for that year and assessed whether they were ⩾50yo (i.e., older HIV patients) on that date. Among those classified as older HIV patients, we further distinguished between those who were younger than 50 years when HIV care was initiated and reached 50 during his/her care (<50yo at enrolment) and those who initiated care at 50 or older (⩾50yo at enrolment). Each year, patients <50yo at enrolment increased either because patients turned 50 that year or because they turned 50 in previous years and survived and were retained in care at least up to that year. Similarly, patients ⩾50yo at enrolment may have enrolled in the cohort that year or enrolled after turning 50 in previous years, survived and retained in care up to that year.
Centers from the CCASAnet cohort included in this study have different periods of enrolment of their patients. The periods included by country are as follows: Argentina from January 1996 to January 2015, Brazil from January 1996 to December 2015, Chile from January 1996 to December 2013, Haiti from November 1999 to November 2012, Honduras from January 1996 to September 2015, Mexico from November 1997 to December 2015 and Peru from February 1996 to August 2015.
We calculated the percentage of older HIV patients relative to the total number of patients retained in care by the calendar year, the distribution of older patients in care who enrolled <50yo at enrolment vs. ⩾50yo at enrolment and the percentage of patients entering the group of older HIV each year. We compared sociodemographic characteristics based on age at enrolment using Wilcoxon Rank Sum tests for continuous variables and Chi-square tests for discrete variables. Separate logistic regression models were fit to assess trends in the proportion of older HIV patients over time for each center and overall; calendar year was included in the model using natural splines with three knots. Analyses were performed at INCMNSZ-Mexico using R Statistical Software (www.R-project.org). Analysis scripts are available at biostat.mc.vanderbilt.edu/ArchivedAnalyses.
Among 24 317 adult patients retained in care at any given year during the study period, 5505 were older than 50 years of age. Of these, there were 2789 (51%) <50yo at enrolment who aged in care and 2716(49%) already ⩾50yo at enrolment. Demographic and clinical characteristics at enrolment in care for these two groups of patients are presented in Table 1. The percentage of male patients, frequency of heterosexual transmission and frequency of AIDS at enrollment were fairly similar between groups. In contrast, people aging in care had a slightly, but statistically lower median CD4 count at enrolment than people who enrolled in care after 50yo.
Table 1. Comparison of demographic and clinical characteristics at enrolment in CCASAnet centers between patients that were younger than 50 years at enrolment (<50 years at enrolment) and patients enrolled at 50 years or older (⩾50 year at enrolment) (2000–2015)
a Continuous variables are reported as medians (interquartile range).
b Not applicable.
c Patients who started ART prior to enrolment were assigned a time of 0 months.
d FH-Argentina: Fundación Huesped, Buenos Aires, Argentina ; FC- Brazil: Instituto Nacional de Infectologia Evandro Chagas-Fiocruz, Rio de Janeiro, Brazil; FA-Chile: Fundación Arriarán, Santiago, Chile; IHSS/HE-Honduras: Instituto Hondureño de Seguridad Social and Hospital Escuela, Tegucigalpa, Honduras; INCMNSZ-Mexico: Instituto Nacional de Ciencias Médicas y Nutrición Salvador Zubirán, Mexico City, Mexico; IMTAvH-Perú: Instituto de Medicina Tropical Alexander von Humboldt, Lima, Peru.
The percentage of older HIV patients receiving care in CCASAnet increased from 8% in 2000 to 24% in 2015 (Fig. 1a). This upward trend was observed at all CCASAnet centers (Fig. 1b and Table S1). Among all the older HIV patients, the percentage who were <50yo at enrolment substantially increased over time, from 20% (n = 17/86) in 2000 to 57% (n = 1134/1983) in 2015. Moreover, the percentage of <50yo at enrolment that turned 50yo each calendar year, ranged from 57% (n = 21/37) in 2001 to 18% (n = 209/1134) in 2015. Additionally, the percentage of ⩾50yo at enrolment that was newly enrolled each year also decreased over time, ranging from 72% (n = 50/69) in 2000 to 5% (n = 47/849) in 2015.
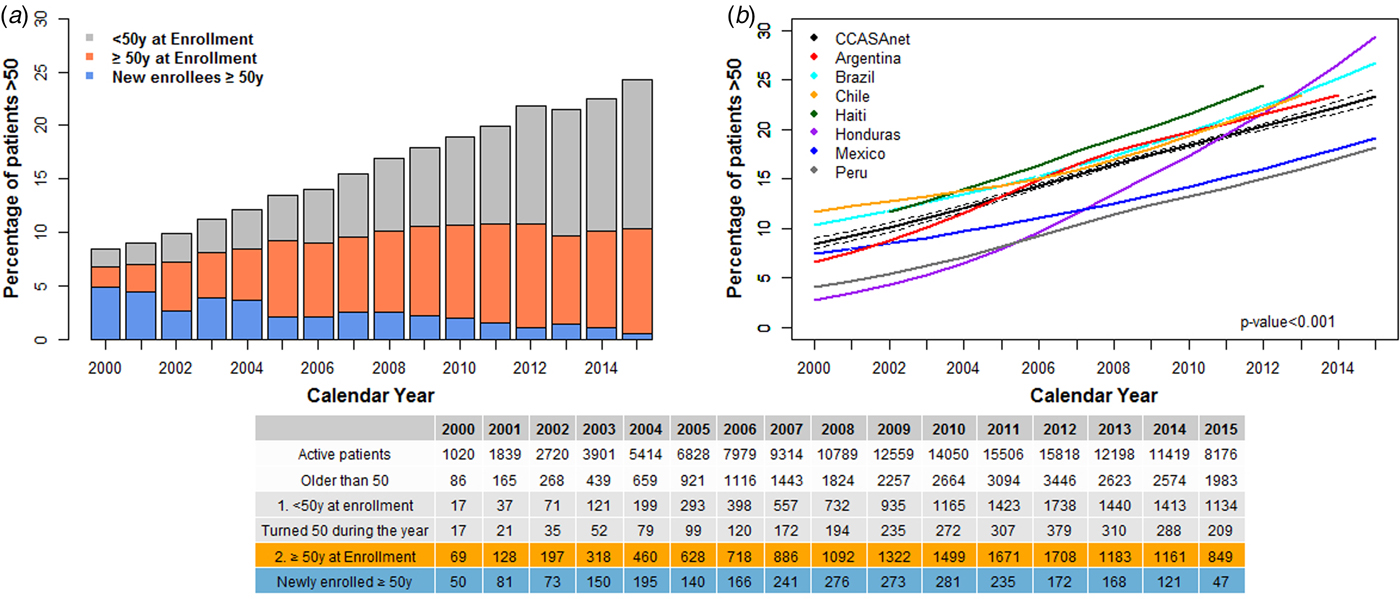
Fig. 1. (a) Percentage of HIV + patients older than 50 years actively receiving care by a group of age and calendar year and (b). The trend of percentage of patients older than 50 among active patients by site and calendar year. (a) Groups of age at enrolment were: (1) <50yo at enrolment and (2) ⩾50 at enrolment. In the <50yo at enrolment group we included active patients who enrolled in care with less than 50 years and aged to over 50 while in care (gray). In the ⩾50 at enrolment group, we included patients who enrolled in care at 50 years or older (blue + orange). Percentage of new patients enrolled older than 50 at each year are shown by the blue bar. (b) The increase in the percentage of patients older than 50 along time is statistically significant for each site (P-values for a test of tendency are <0.001 for each country and for the whole cohort). The curves are predictions from logistic models adjusted by year and site. The absolute number of all active patients, those who are older than 50 and their classification according to age at enrolment by year, are shown in the table; decreases in active patients from 2013 to 2015 were due to lack of available data from Haiti.
In summary, we observed that by 2015, 24% of patients receiving care for HIV in seven centers in the Caribbean and Latin America were older than 50 years. This figure is a threefold increase in the last 15 years and higher than the UNAIDS mathematical model estimates of 15% [5]. Notably, clinics in Haiti, Honduras and Peru had the fastest upward trend in the relative proportion of people older than 50yo receiving care over time. People turning 50yo each year and the newly enrolled after 50yo, decreased proportionally over time. Thus, in our cohort, most of the growth of this population can be explained by the increasing survival and retention in care of all patients regardless of their age at enrolment, but to a greater extent by those who enrolled younger and aged in care (see Fig. 1a). By the end of the observation period, those enrolled in previous years that survived and were retained in care accounted for the majority of older HIV patients.
While we cannot be certain why our estimates differ from the UNAIDS mathematical model, we posit discrepancies may be due to differences in available data. For example, centers in the CCASAnet cohort typically started provision of care early during the HIV epidemic and were already fully operating during the expansion of universal access to ART in our region between 2002 and 2004, before most patients in the region were started on ART [Reference Belaunzarán-Zamudio11]. If this resulted in higher survival rates, our findings, despite coming from a large number of individuals, might not fully represent the whole region. Alternatively, the parameters used by UNAIDS could be affected by the lack of availability and quality of specific surveillance and survey data in each country. In contrast, our data are collected in real settings for a long period of time and include large numbers of patients, which allow us to perform appropriate descriptions of demographic trends among HIV patients in care along time in the region.
Our findings suggest that current models may be underestimating the proportion of older PLWHIV in Latin America and the Caribbean. In any case, with improvements in life expectancy among patients on ART and continued new HIV diagnoses (and new HIV infections) in those aged over 50 years, [Reference Sabin and Reiss13] we can anticipate this trend towards an older HIV population to continue. This demographic shift will impact the needs of care due to the multiple comorbidities and the high risk of disability associated with ageing [Reference Ávila-Funes14]. The former implies specialised care in tertiary facilities and higher costs. Estimating such costs through modelling studies could help plan an integral approach to the care of older PLWHIV and their future needs.
Supplementary material
The supplementary material for this article can be found at https://doi.org/10.1017/S0950268818001346.
Acknowledgments
The Caribbean, Central and South America Network for HIV Epidemiology (CCASAnet) includes the following sites: Fundación Huesped, Argentina: Pedro Cahn, Carina Cesar, Valeria Fink, Omar Sued, Patricia Patterson, Emanuel Dell'Isola, Hector Perez, Jose Valiente, Cleyton Yamamoto. Instituto Nacional de Infectologia-Fiocruz, Brazil: Beatriz Grinsztejn, Valdilea Veloso, Paula Luz, Raquel de Boni, Sandra Cardoso Wagner, Ruth Friedman, Ronaldo Moreira. Universidade Federal de Minas Gerais, Brazil: Jorge Pinto, Flavia Ferreira, Marcelle Maia. Universidade Federal de São Paulo, Brazil: Regina CeÂlia de Menezes Succi, Daisy Maria Machado, Aida de Fátima Barbosa Gouvêa. Fundación Arriarán, Chile: Marcelo Wolff, Claudia P. Cortes, Maria Fernanda Rodriguez, Gladys Allende. Les Centres GHESKIO, Haiti: Jean William Pape, Vanessa Rouzier, Adias Marcelin, Christian Perodin. Hospital Escuela Universitario, Honduras: Marco Tulio Luque. Instituto Hondureño de Seguridad Social, Honduras: Denis Padgett. Instituto Nacional de Ciencias Médicas y Nutrición Salvador Zubirán, México: Juan Sierra Madero, Brenda Crabtree Ramirez, Pablo F. Belaunzarán-Zamudio, Yanink Caro Vega, Rocío Velázquez Pastrana and Luis Enrique Gómez. Instituto de Medicina Tropical Alexander von Humboldt, Peru: Eduardo Gotuzzo, Fernando Mejia, Gabriela Carriquiry. Vanderbilt University Medical Center, USA: Catherine C McGowan, Bryan E Shepherd, Timothy Sterling, Karu Jayathilake, Anna K Person, Peter F Rebeiro, Mark Giganti, Jessica Castilho, Stephany N Duda, Fernanda Maruri, Hilary Vansell, Sally Bebawy and James Logan. We gratefully acknowledge all patients, caregivers and data managers involved in the CCASAnet cohort.
Financial support
This work was supported by the NIH-funded Caribbean, Central and South America network for HIV epidemiology (CCASAnet), a member cohort of the International Epidemiologic Databases to Evaluate AIDS (leDEA) (U01AI069923). This award is funded by the following institutes: Eunice Kennedy Shriver National Institute of Child Health & Human Development (NICHD), National Cancer Institute (NCI), National Institute of Allergy and Infectious Diseases (NIAID), National Institute of Mental Health (NIMH) and the Office of The Director, National Institutes of Health (OD).
Conflicts of interest
Y Caro-Vega, PF Belaunzaran-Zamudio, Jessica L Castilho, B Crabtree-Ramírez, BE Shepherd, F Mejia, MJ Giganti, D Padgett, Beatriz Grinsztejn, Jean W Pape and P Patterson have no conflicts of interest to declare. Catherine C McGowan reports grants from the US NIH. Dr Sierra-Madero reports personal fees and non-financial support from Gilead, non-financial support from MSD, grants from BMS, grants from Pfizer, personal fees from Jansen all outside the submitted work.





