Introduction
The unprecedented and unpredictable nature of the coronavirus disease 2019 (COVID-19) pandemic has triggered a focus on the psychological and mental health problems of the health care staff involved (Greenberg et al., Reference Greenberg, Docherty, Gnanapragasam and Wessely2020; Vindegaard and Benros, Reference Vindegaard and Benros2020). Physicians being key frontline workers are among the most affected of health care staff professions. A cross-sectional study based on an investigation involving 34 hospitals in China reported that frontline healthcare workers often experienced depressive symptoms, anxiety, sleep disturbances, and distress whilst managing patients with COVID-19 (Lim et al., Reference Lim, Cha, Chae and Jo2015). The situation is similar in many countries and particularly challenging in low-resource settings (Greenberg et al., Reference Greenberg, Docherty, Gnanapragasam and Wessely2020).
The first case of COVID-19 in Bangladesh was announced on 8 March 2020 and the first death was documented on 18 March 2020 (Hasan et al., Reference Hasan, Hossain, Saran and Ahmed2020; Islam et al., Reference Islam, Sultana, Khan, Hossain, Sikder, Hasan and Li2021). Over time, the number increased to 1 950 124 as reported on 17th March 2022 with a death toll of 29 112 patients whilst the total number of affected physicians was 3182 with a tragic loss of 190 doctors (BMA, 2021; DGHS, 2021). In Bangladesh, a severe dearth in resources and support has been observed since the initial phase of the pandemic for front line physicians (Khan et al., Reference Khan, Howlader and Islam2020). Hasan et al. (Reference Hasan, Hossain, Saran and Ahmed2020) expressed the concerns of Bangladeshi physicians in terms of infecting their own families, considering the tradition of congested, multifamily accommodation with limited quarantine opportunities. They also described, in addition to risking their own physical well-being, that frontline physicians are enduring significant emotional burdens both at work and at home (Hassan et al., Reference Hassan, Monjur, Styczynski, Rahman and Banu2021).
Therefore, it is essential to identify and characterize the mental health difficulties experiencing by the Bangladeshi physicians during the pandemic in such a challenging setting. There is a few published evidence on mental health issues among Bangladeshi physicians related to COVID-19, generating relatively little knowledge on a matter of severe concern (Khatun et al., Reference Khatun, Parvin, Rashid, Alam, Kamrunnahar, Talukder, Rahman Razu, Ward and Ali2021; Rahman et al., Reference Rahman, Deeba, Akhter, Bashar, Nomani, Koot, Koly, Bin Salah, Haverlag and Anwar2021; Repon et al., Reference Repon, Pakhe, Quaiyum, Das, Daria and Islam2021). This is especially pertinent with the uncertainty surrounding an outbreak of such unparalleled magnitude in Bangladesh & similar low resource countries. Therefore, this study aims to investigate the levels of anxiety and depressive symptoms and to identify associated factors among Bangladeshi registered physicians during the COVID-19 outbreak.
Materials and methods
Study design, participants and sampling techniques
A cross-sectional study was conducted among Bangladeshi registered physicians from April 21 to May 10, 2020, when the COVID-19 pandemic and the enforced lockdown was in its initial phase in the country. To be eligible, the respondents had to be adults (>18 years), Bangladeshi registered physicians, able to read and understand English, and to be living in Bangladesh at the time of the COVID19 outbreak. The Sample size was calculated from prevalence estimate using following formula: n = (z 2p(1 − p)/d 2), where, where n = number of samples; z = 1.96 for 95% confidence level (CI), p = ‘best guess’ for prevalence and d = precision of the prevalence estimate. However, a recent study by Al Banna et al. (Reference Al Banna, Sayeed, Kundu, Christopher, Hasan, Begum, Kormoker, Dola, Hassan, Chowdhury and Khan2020) reported that the prevalence of anxiety symptoms and depressive symptoms among general population was 33.7% and 57.9% during COVID-19 pandemic in Bangladesh (Al Banna et al., Reference Al Banna, Sayeed, Kundu, Christopher, Hasan, Begum, Kormoker, Dola, Hassan, Chowdhury and Khan2020). We assumed that the psychological difficulties might be 50% among the physicians of Bangladesh and so the calculated sample size was 384 participants. Assuming 15% non-response rate we calculated the sample size as 442. We approached to 442 physicians & 412 provided consent for participation.
We used convenience sampling method to identify & recruit appropriate participants. Considering the risky data collection inside the hospital setting amid the pandemic, an online survey was posted on closed social media (Facebook) groups of registered physicians of Bangladesh and open request was placed by the team of investigators to complete the survey. Also, five volunteers (medical doctors) from different medical institutions were employed to circulate details of the survey among their professional networks in addition to regular posting in social media groups. They were instructed to be inclusive, open and to circulate details of the survey periodically for maximum reach. Email addresses of the participants were collected upon proper clarification and informed, written consent was obtained. There was more reach of physician in these groups than different hospitals or regions as we followed an online data collection method amid the pandemic.
Data collection tool
Data were collected using a structured online questionnaire created in Google form (in English). The questionnaire had 3 parts: (i) demographic questions, (ii) COVID19-related questions, (iii) Hospital Anxiety and Depression Scale (HADS; higher scores on the subscales indicate higher levels of depression and anxiety symptoms) (Zigmond and Snaith, Reference Zigmond and Snaith1983).
The HADS is widely used self-reported scale developed by Zigmond and Snaith (Reference Zigmond and Snaith1983) consisting of 14 questions including 2 subscales (i.e. 7-item anxiety and 7-item depression) with a four-point Likert scale ranging from 0 to 3 and the overall scores ranging from 0 to 21 for each subscale (Repon et al., Reference Repon, Pakhe, Quaiyum, Das, Daria and Islam2021). The cutoff (>8) utilized to screen for symptoms for anxiety and depression for each subscale was the same as used previously in the Bangladeshi population (Chowdhury et al., Reference Chowdhury, Karim, Selim, Ahmed, Azad, Maksud, Rahaman, Uddin and Chowdhury2017; Tasnim et al., Reference Tasnim, Sujan, Islam, Ritu, Bin Siddique, Toma, Nowshin, Hasan, Hossain, Nahar, Islam, Islam, Potenza and van Os2021). In our study, we have found the good reliability of the HADS scale for assessing the anxiety and depression where the Cronbach's α of the anxiety and depression subscales were 0.85 and 0.76, respectively, and overall Cronbach's α of the HADS scale was 0.88.
Statistical analysis
All statistical analyses were carried out using SPSS (version 25.0). Frequency distribution with percentage was used to present categorical variables while mean with standard deviation (s.d.) was used to present continuous variables. Chi-square (χ 2) test was used to determine any difference between groups. Both bivariate and multiple logistic regression models were used to find out the predictors of anxiety and depressive symptoms among Bangladeshi physicians during COVID-19 pandemic. Statistical significance level was set at p-value <0.05 and 95% confidence interval (CI).
Ethics
The study was conducted following the Checklist for Reporting Results of Internet ESurveys (CHERRIES) guideline (Eysenbach, Reference Eysenbach2004). The authors ensured that all procedures contributing to this work comply with the ethical standards of the relevant national and institutional committees on human experimentation and with the Helsinki Declaration of 1975, as revised in 2008. The study was approved by the Ethical Review Committee, Shaheed Suhrawardy Medical College, Dhaka, Bangladesh (ShSMC/Ethical/2020/12).
Results
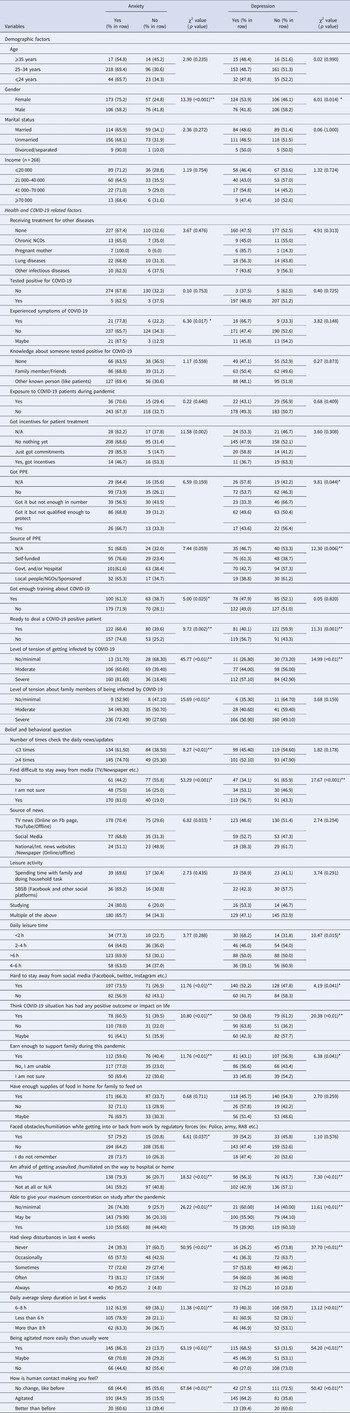
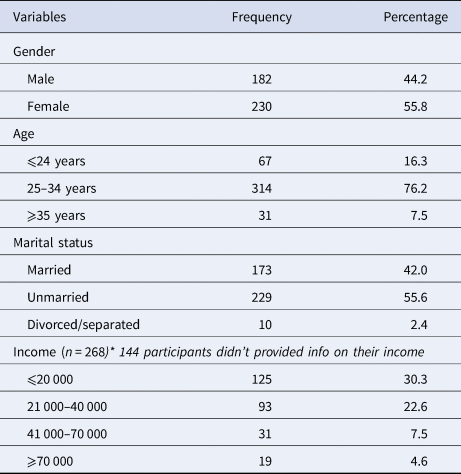
A total of 412 participants (response rate 93.21%) took part in the study and completed the survey. Most physicians were female (55.8%), the majority were aged between 25 and 34 years (76.2%), and most were unmarried (55.6%). More than half of the study participants (52.9%) reported having an income of 40000 BDT (365 GBP) per month or less (see Table 1).
Table 1. Sociodemographic characteristics of the study participants
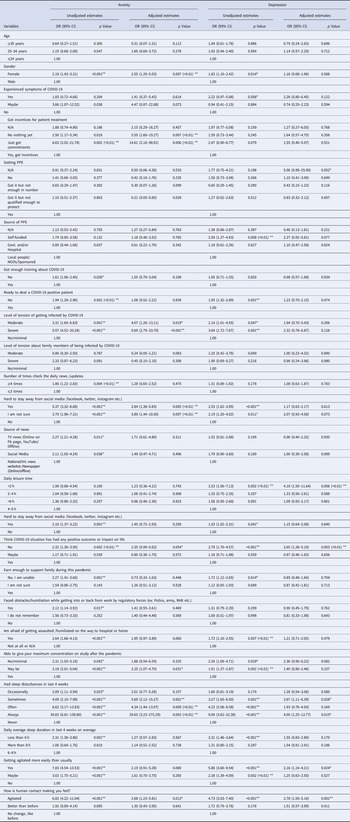
The study showed that females (75.2%) suffered more from anxiety than males (58.2%) which was statistically significant (p < 0.001). Similarly, depression was more prevalent among females (53.9% v. 41.8% male, p = 0.014). Addition to that, respondents (77.8%) experiencing COVID-19 symptoms were suffering from anxiety than those not experiencing symptoms of COVID-19 (65.7%) that was statistically significant (p = 0.017). Anxiety was more prevalent among respondents those feel that they were not provided with training about COVID-19 (71.9%) than respondents those feel that they were provided enough training about COVID-19 (61.3%) and it was found statistically significant (p = 0.025). Moreover, respondents those were not ready to deal a COVID-19 positive patient suffered more from anxiety (74.8% v. 60.4% respondents ready to deal a COVID-19 positive patient, p = 0.002).
Furthermore, depression was also more prevalent among respondents not ready to deal a COVID-19 positive patient (56.7% v. 40.1% respondents ready to deal a COVID-19 positive patient, p = 0.001). Anxiety was more common among respondents severely tensed about being infected by COVID-19 (81.60% v. 31.70% respondents not tensed at all or minimally tensed, p < 0.01). In the same way, depression was also seen to be common among respondents severely tensed about being infected by COVID-19 (57.10% v. 26.80% respondents not tensed at all or minimally tensed, p < 0.01). However, variables such as receiving treatment for other diseases, and having knowledge about someone tested positive for COVID-19 had no statistically significant relationship with anxiety or depression (see Table 2).
Table 2. Factors associated with anxiety and depression among physicians in Bangladesh
The study also showed that respondents checking news updates more than four times a day, having hard time staying away from media (e.g. TV, newspaper etc.), having less than 2 h of leisure, being unable to earn enough to support the family, facing any obstacles or humiliation by regulatory forces (e.g. Police, Rapid Action Battalion etc.) on the way to work from home and vice versa, being agitated more easily than usual, being agitated with human contact had higher occurrence of either anxiety or depression or both in some cases (see Table 2).
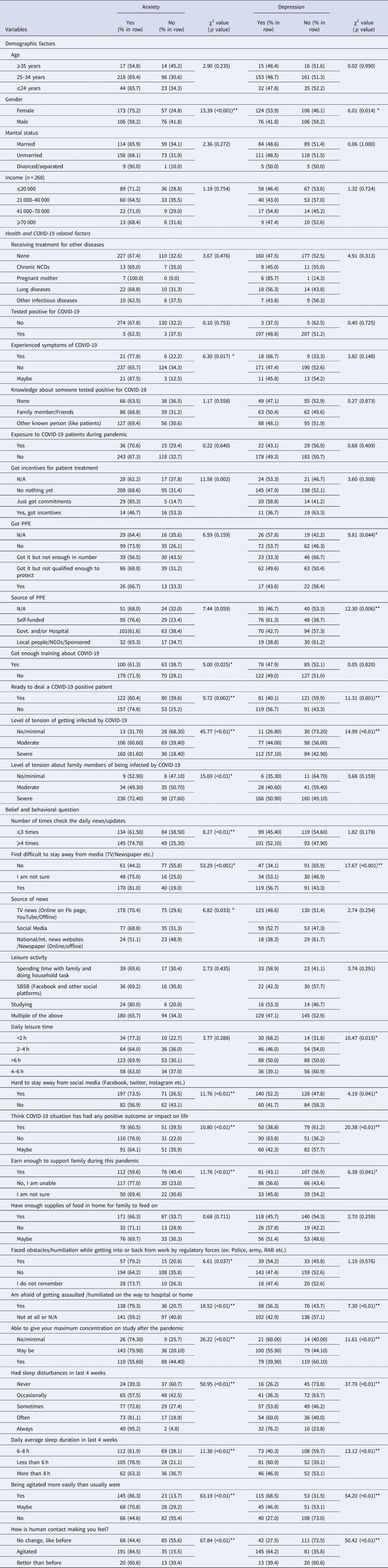
Regression analysis showed that, females were about 2.5 times more likely to be in anxiety than males (p < 0.01). Addition to that, respondents experiencing COVID-19 had higher odds to suffer from depression than respondents not experiencing COVID-19 symptoms (OR 1.63; 95% CI 1.10–2.42). Furthermore, it was seen that respondents spending less than 2 h a day for leisure activity were about 4 times more likely to suffer from depression than respondents spending 4 to 6 h for leisure activity (p < 0.01). Moreover, respondents those felt agitated by human contact had higher likelihood for anxiety (AOR = 2.68; 95% CI 1.23–5.81) and depression (AOR = 2.78; 95% CI 1.50–5.16) than those not feeling any changes by human contact. Similarly, respondents being unable to give maximum concentration on job after this pandemic, having fear of getting assaulted or humiliated on the way to work or home, having no positive outcome or impact on life through this pandemic, having hard time to stay away from social media (e.g. Facebook, Twitter, Instagram etc.), sleeping less than 6 h had significant association with higher odds of both anxiety and depression (Table 3).
Table 3. Odds of binary logistic regression of predictive study variables with anxiety and depression among physicians in Bangladesh
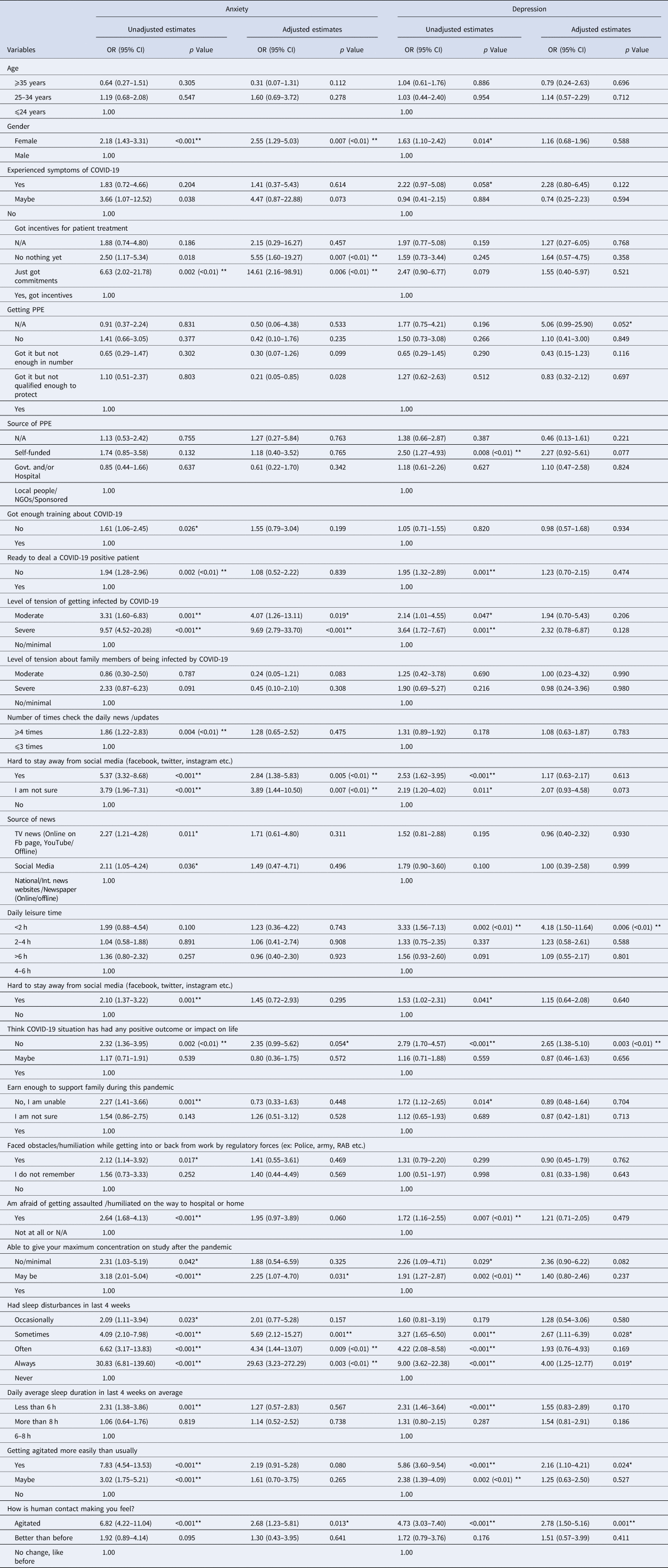
Apart from these, respondents being moderately or severely tensed about being infected by COVID-19, not getting any incentives for patient treatment, feeling that they had not been provided with enough training about COVID-19, not being ready to deal a COVID-19 patient, having news updates from various sources (e.g.TV news, social media, online or offline newspapers etc.) and having sleep disturbances from occasionally to always had significant association with higher odds of either anxiety or depression or both in some cases. (Table 3)
Discussion
This cross-sectional study investigated the prevalence of anxiety and depressive symptoms in registered Bangladeshi physicians amid the COVID-19 pandemic, and to identify the factors associated with these psychological issues. To the best of our knowledge, very few previous studies have taken place among physicians in context of Bangladesh to determine the level of anxiety and depression and their contributing factors related to this pandemic.
Our findings revealed that, in terms of HADS cut-off points, the prevalence of anxiety and depression among registered physicians was 67.72% and 48.54% respectively. Several factors were found to be associated with this higher prevalence of depression and anxiety. For instance, among female gender, physicians who had experienced symptoms of COVID-19, not received incentives/only received compliments, reliance on self-funded personal protective equipment (PPE), inadequate training, lacking perceived self-efficacy while helping COVID positive patients, greater perceived stress of being infected, fear of getting assaulted/humiliated, use of social media, lower income level to support family, feeling more agitated, being agitated while contacting other people, less than 2 h of leisure activity a day, assuming no positive outcome/impact in life, sleep disturbance, and short sleep duration were found to be positively associated with physicians' anxiety and depression symptoms in the unadjusted and in the adjusted statistical models.
Worldwide, throughout the pandemic front-line physicians are not only at the risk of physical challenges but also of experiencing significant mental health and psychosocial issues. (Chen et al., Reference Chen, Liang, Li, Guo, Fei, Wang, He, Sheng, Cai, Li, Wang and Zhang2020; Kang et al., Reference Kang, Li, Hu, Chen, Yang, Yang, Wang, Hu, Lai, Ma, Chen, Guan, Wang, Ma and Liu2020). In line with our findings, an estimated 50.4% and 44.6% healthcare staffs self-reported anxiety and depression respectively in a cross-sectional survey in China (Lai et al., Reference Lai, Ma, Wang, Cai, Hu, Wei, Wu, Du, Chen, Li, Tan, Kang, Yao, Huang, Wang, Wang, Liu and Hu2020). On the other hand, a significantly lower prevalence of anxiety and depression (14.5% and 8.9% respectively) have been found in a Singapore-based study involving physicians (Tan et al., Reference Tan, Chew, Lee, Jing, Goh, Yeo, Zhang, Chin, Ahmad, Khan, Shanmugam, Chan, Sunny, Chandra, Ong, Paliwal, Wong, Sagayanathan, Chen, Ng, Teoh, Ho and Sharma2020). The variances between study results could be explained by methodological differences, level of resources available in each of those countries and the subsequent demands on physicians and adoption of different scales and cut-off scores in different surveys, as well as true differences.
One Iranian study utilized the same research instrument (HADS) as our study. In line with our study findings, more than 68% of doctors and nurses had experienced anxiety symptoms, whereas depressive symptoms were reported approximately 52% (Hassannia et al., Reference Hassannia, Taghizadeh, Moosazadeh, Zarghami, Taghizadeh, Dooki, Fathi, Navaei and Hedayatizadeh-Omran2020). Overall, a recent systematic review and meta-analysis quantified the cumulative prevalence of anxiety and depression experienced by medical staff during COVID-19 by pooling data from 13 studies with a reported 23.2% anxiety and 22.8% depression (Pappa et al., Reference Pappa, Ntella, Giannakas and Giannakoulis2020). The disproportionately higher prevalence of anxiety and depression (67.72% and 48.54% respectively) among Bangladeshi physicians could be described by the extreme shortage and mal-distribution of health workforce, (Ahmed et al., Reference Ahmed, Hossain, RajaChowdhury and Bhuiya2011) coupled with significantly higher rates of infection and death among health professionals, extended working hours, ultimate shortage of PPE, lack of adequate training, and social assault/humiliation.
As expected, Bangladeshi female physicians experienced higher psychological distress than their male counterparts during this pandemic. This finding agrees with the established gender gap for more frequent anxious and depressive symptoms among women (Alexander et al., Reference Alexander, Dennerstein, Kotz and Richardson2007; Albert, Reference Albert2015). In parallel with Wang et al. (Reference Wang, Di, Ye and Wei2021) study findings, where three-fold higher anxiety disorder was observed among women (Wang et al., Reference Wang, Di, Ye and Wei2021), the current study identified females suffering from anxiety symptoms 2.5 times greater than their counterparts. Biological mechanisms and hormonal influences may demonstrate the relationship of higher perceived psychological distress in women (Albert, Reference Albert2015). Although age and associated physical and mental comorbidities are identified as major predisposing factors for anxiety and depression among doctors (Guo et al., Reference Guo, Liao, Wang, Li, Guo, Tong, Guan, Zhou, Wu, Zhang and Gu2020; Kisely et al., Reference Kisely, Warren, McMahon, Dalais, Henry and Siskind2020; Özdin and Bayrak Özdin, Reference Özdin and Bayrak Özdin2020), surprisingly, we found no statistically significant differences between depression symptoms and anxiety levels and the above-mentioned variables, which warrants future research.
Our study revealed that, less than 6 h of sleep compared to normal sleep duration (6–8 h) and any level of sleep disturbances experienced in the past four weeks in comparison to no sleep disturbance, were linked to prevalence of anxiety and depressive symptoms. A survey conducted by Wang et al. (Reference Wang, Xie, Xu, Yu, Yao and Xiang2020) among Chinese pediatric physicians, found independent association between sleep disturbances and depression, however, anxiety reveled statistically non-significant relationship, although physicians with sleep problems reported higher anxiety than their counterparts (Wang et al., Reference Wang, Xie, Xu, Yu, Yao and Xiang2020). Another study exhibited similar findings that represented Taiwanese local physicians during SARS pandemic (Chen et al., Reference Chen, Wu, Yang and Yen2005). Moreover, depression, but not anxiety, was found approximately 4 times higher among physicians those spent less than 2 h on leisure activities than that of 4–6 h in this current study.
Following COVID-19 outbreak, physicians took initiatives to support the strained health sector and struggled to protect the health of the public (Xiao, Reference Xiao2020), however, they became the foremost victims of this pandemic concerning the exaggerated psychological pressure of varying factors. For example, direct contact with COVID positive patients, suspected patients hiding medical history, concern about inadequate PPE, extended working hours, infection of colleagues, separation from family, fear of infecting family members, physical fatigue, and medical violence may in turn accelerate their existing stress level (Dai et al., Reference Dai, Hu, Xiong, Qiu and Yuan2020; Godlee, Reference Godlee2020; Kang et al., Reference Kang, Li, Hu, Chen, Yang, Yang, Wang, Hu, Lai, Ma, Chen, Guan, Wang, Ma and Liu2020; Liu et al., Reference Liu, Luo, Haase, Guo, Wang, Liu, Xia, Liu, Yang and Yang2020). Along with these, Lu et al. (Reference Lu, Wang, Lin and Li2020) emphasized on worrying about being infected, duty in the isolation ward, feeling lonely due to detachment from the loved ones, being frustrated with unsatisfactory results on work, and the fear of an uncontrollable epidemic, leading to psychological distress (Lu et al., Reference Lu, Wang, Lin and Li2020). The level of anxiety and depressive symptoms even more prominent among Bangladeshi doctors, contributed by several factors, such as self-funded PPE, absence of incentives, lack of proper training to deal with COVID patients, perceived stress of being infected, and fear of getting assaulted/humiliated while returning home from workplace. Addressing the above-mentioned factors by the policymakers and organizational authorities are paramount to excel the strength of HCWs and support their mental well-being to reach to their highest level of aspirations to serve the humanity.
This study provides concerning findings on anxiety and depressive symptoms among Bangladeshi physicians during COVID-19 pandemic, however we cannot overlook the limitations. The cross-sectional nature of the study design could not establish causal relationship between the dependent and independent variables. This study was carried out by conducting a web-based survey, which might generate sampling bias by excluding the physicians who do not have access to internet or inactive in social medias, and thus limit the generalizability of the findings. Besides, self-reported responses on anxiety and depression symptoms only provided subjective data which may greatly differ from objective data, leading to response bias. Finally, although we tried to address major risk factors, several relevant variables, such as residence status (urban or rural), having children, domestic violence, moral dilemma to manage such complex patients and information on physician's work hours or perceived workloads were not included in the survey.
Despite these limitations, our study has several clear public health implications. Our results suggest vulnerability of Bangladeshi physicians for anxiety and depressive symptoms during the pandemic which should be closely monitored. Previous studies emphasized on alarmingly higher rates of ‘physician burnout’, characterized by emotional exhaustion, depersonalization, and low personal accomplishments (West et al., Reference West, Dyrbye and Shanafelt2018) and alternatively increased risk of suicidal ideation and suicidal attempts in physicians (Rothenberger, Reference Rothenberger2017). Moreover, Montemurro reported suicides in India and Italy during this pandemic, as physicians experienced helplessness, acute psychological stress, and utmost fear of dying (Montemurro, Reference Montemurro2020). As physician's psychological health and patient safety and satisfaction are inextricably linked (Panagioti et al., Reference Panagioti, Geraghty, Johnson, Zhou, Panagopoulou, Chew-Graham, Peters, Hodkinson, Riley and Esmail2018), promotion of mental well-being of physician is paramount and there is an urgent call for personal, social, and policy-level interventions before it is too late. Given the importance of the risk factors associated with physician's anxiety and depression symptoms identified in this study, provision of adequate PPE, proper training before deployment in the isolation ward, additional incentives, and on-going monitoring and remote psychological support may aid in reducing physician's psychological strain.
Conclusion
This study reports a real concern about the prevalence of anxiety and depression symptoms with identification of associated factors among Bangladeshi physicians during the COVID-19 pandemic. Such mental health difficulties are higher than normal scenario. Given the vulnerability of the physicians and other health care staff in this extraordinary condition whilst they are shouldering the overwhelming weight of the epidemic, fighting social stigma and putting their lives at risk to help the affected, health authorities should be addressing their psychological needs and formulate effective strategies, standard operating procedures (SOPs) and appropriate interventions to support these frontline fighters at such difficult times.
Data
Data will be available upon reasonable request.
Acknowledgements
The authors would like to express their gratitude to Jannatul Ferdous, Wasi Uddin Ahmad, Sakib Hasan, Iftekhar Ahmed Sakib, Lubana Nasreen Tushi, Syed Ramiz Ahnaf, Al Hasnat Turab, Faria Islam Ria, Sajibur Rahman and Md Asifur Rahman for their support in collecting data. Authors would also like to thank all the participants for their spontaneous and voluntary participation in the study. GT is supported by the National Institute for Health Research (NIHR) Applied Research Collaboration South London at King's College London NHS Foundation Trust, and by the NIHR Asset Global Health Unit award. The views expressed are those of the author(s) and not necessarily those of the NHS, the NIHR or the Department of Health and Social Care. GT also receives support from the National Institute of Mental Health of the National Institutes of Health under award number R01MH100470 (Cobalt study). GT is supported by the UK Medical Research Council in relation the Emilia (MR/S001255/1) and Indigo Partnership (MR/R023697/1) awards.
Authors contribution
Conceptualization: M.Tasdik Hasan, Syeda Fatema Alam, Md. Abdur Rafi, Vivek Podder, S.M Quamrul Akther, Fatema Ashraf. Data analysis: Afifa Anjum, Sahadat Hossain. Investigation: M. Tasdik Hasan, Syeda Fatema Alam, Md. Abdur Rafi, Vivek Podder, Dewan Tasnia Azad, Rhedeya Nury Nodi. Methodology: M. Tasdik Hasan, Sahadat Hossain. Resources: M. Tasdik Hasan, Farhana Safa, Syeda Fatema Alam, Sahadat Hossain, Supervision: S.M Quamrul Akther, Fatema Ashraf. Writing – original draft: M. Tasdik Hasan, Farhana Safa, Abid Hasan Khan, Afifa Anjum, Sahadat Hossain. Writing – review and editing: M. Tasdik Hasan, Shahadat Hossain, Afifa Anjum, Farhana Safa, Abid Hasan Khan, Kamrun Nahar Koly, Syeda Fatema Alam, Md. Abdur Rafi, Vivek Podder, Tonima Islam Trisa, Rhedeya Nury Nodi, Dewan Tasnia Azad, Fatema Ashraf, S.M Quamrul Akther, Helal Uddin Ahmed, Simon Rosenbaum, Graham Thornicroft. All authors read and approved the final manuscript.
Financial support
None.
Conflict of interest
None.
Patient and public involvement statement
Patients and/or the public were not involved in this study.
Patient consent for publication
Not required.