Introduction
Over 100 million family members worldwide are estimated to be affected by the addictive behaviours of a relative, and the negative impact is similar in family members across the world (Copello et al., Reference Copello, Templeton, Orford and Velleman2010a, Reference Copello, Templeton and Powell2010b; Orford et al., Reference Orford, Velleman, Natera, Templeton and Copello2013b). There has been a substantial increase in alcohol users over the years in India, with the annual alcohol consumption rates having increased by 38% between 2010 and 2017 (from 4.3 to 5.9 litres per adult) (Manthey et al., Reference Manthey, Shield, Rylett, Hasan, Probst and Rehm2019). This increase will have caused a corresponding rise in the prevalence of affected family members (AFMs), and this will be largely hidden because AFMs are a ‘silent group’. The experiences of living with a person with drinking problems may make family members vulnerable to mental ill-health including mood and substance use disorders, trauma and stress-related conditions (Patel, Reference Patel2007; Ray et al., Reference Ray, Mertens and Weisner2009; Copello et al., Reference Copello, Templeton, Orford and Velleman2010a, Reference Copello, Templeton and Powell2010b; Orford et al., Reference Orford, Velleman, Natera, Templeton and Copello2013b). The limited number of studies from India demonstrate a high burden of alcohol use on families, including stress, disruptions in family interactions and routine, financial difficulties (Mattoo et al., Reference Mattoo, Nebhinani, Kumar, Basu and Kulhara2013) and domestic violence and stigma (Patel et al., Reference Patel, Kirkwood, Pednekar, Pereira, Barros, Fernandes, Datta, Pai, Weiss and Mabey2006; Gururaj et al., Reference Gururaj, Murthy, Girish and Benegal2011).
Traditionally, family members have been viewed as a cause for the addiction, with the female spouse most often blamed (Orford et al., Reference Orford, Natera, Copello, Atkinson, Mora, Velleman, Crundall, Tiburcio, Templeton and Walley2013a); and the focus of treatments for substance use is limited by engaging solely with the person with drinking-related problems (Copello et al., Reference Copello, Velleman and Templeton2005). In India too, the treatment response has primarily focussed on long-term tertiary care for the person with drinking-related problems; which is fraught with further challenges of inaccessibility for the majority of the population (Benegal et al., Reference Benegal, Chand and Obot2009). Consequentially, AFMs experience high unmet needs as they play a peripheral role in formal care and are neglected because services are not equipped to address their problems (Copello and Orford, Reference Copello and Orford2002; Orford et al., Reference Orford, Velleman, Natera, Templeton and Copello2013b; Orford, Reference Orford2017).
The 5-Step Method is an evidence-based brief psychosocial intervention for helping AFMs and is derived from the theoretical framework of the Stress-Strain-Coping-Support (SSCS) model (Velleman et al., Reference Velleman, Arcidiacono, Procentese, Copello and Sarnacchiaro2008; Copello et al., Reference Copello, Templeton, Orford, Velleman, Patel, Moore, MacLeod and Godfrey2009, Reference Copello, Templeton, Orford and Velleman2010a, Reference Copello, Templeton and Powell2010b; Orford et al., Reference Orford, Copello, Velleman and Templeton2010a, Reference Orford, Velleman, Copello, Templeton and Ibanga2010b; Rey et al., Reference Rey, Mora-Ríos, Sainz and Aguilar2010; Velleman et al., Reference Velleman, Orford, Templeton, Copello, Patel, Moore, Macleod and Godfrey2011; Orford et al., Reference Orford, Natera, Copello, Atkinson, Mora, Velleman, Crundall, Tiburcio, Templeton and Walley2013a). The 5-Step Method was adapted and evaluated in the SAFE (Supporting Addiction Affected Families Effectively) program, using the Medical Research Council's guidance on developing and evaluating complex interventions (Craig et al., Reference Craig, Dieppe, Macintyre, Michie, Nazareth and Petticrew2008; Rane et al., Reference Rane, Church, Bhatia, Orford, Velleman and Nadkarni2017; Church et al., Reference Church, Bhatia, Velleman, Velleman, Orford, Rane and Nadkarni2018; Nadkarni et al., Reference Nadkarni, Bhatia, Velleman, Orford, Velleman, Church, Sawal and Pednekar2019). This paper describes the second phase of the SAFE program, and its objectives are to test the feasibility and acceptability of processes for a definitive randomised controlled trial (RCT) (e.g. recruitment, data collection, intervention delivery); test the indicative impact of the intervention in improving clinical outcomes in AFMs; and understand how the intervention can be further refined, based on these findings.
Methods
Study design
Parallel arm, single-blind, feasibility RCT. The CONSORT statement can be accessed in supplementary material.
Setting
Communities in four sub-districts of Goa, India (population 1.4 million). Unlike most of India, Goa has a ‘more liberal, wet culture’ with the drinking patterns characterised by low rates of abstinence, and a high prevalence of hazardous drinking in men (Silva et al., Reference Silva, Gaunekar, Patel, Kukalekar and Fernandes2003; D'costa et al., Reference D'costa, Nazareth, Naik, Vaidya, Levy, Patel and King2006; Pillai et al., Reference Pillai, Nayak, Greenfield, Bond, Nadkarni and Patel2013).
Participants
The sources of recruitment were referrals from community gatekeepers (e.g. professional and community health workers, priests, village council members), and self-referrals (through word-of-mouth publicity and advertisements in healthcare and community settings). The inclusion criteria were (1) family member (⩾18 years) reporting that the relative's drinking had been a major source of distress in the previous 6 months, (2) the relative had been drinking problematically at some point during the previous 6 months, (3) the family member and the relative who had been drinking problematically had been living in the same house at some point in the previous 6 months, or had face-to-face contact at least three times a week. Eligible participants who gave informed consent were administered the baseline assessments and randomised to receive either SAFE or enhanced usual care (EUC).
Randomisation, allocation concealment and blinding
An independent researcher developed a randomisation code using computer-generated random numbers. Sequentially Numbered Opaque Sealed Envelopes were used to maximise allocation concealment. The envelope was opened only after the participant information was written on its cover, which helped create an audit trail. The 3-month outcome assessments were administered by research assistants, who had no previous engagement in the trial, and were ‘blind’ to the treatment allocation. The primary outcome assessment was administered prior to all other assessments; and participants were requested not to disclose their allocation status during the outcome interview.
Interventions
The intervention arm received SAFE, a contextually adapted version of the 5-Step Method (Nadkarni et al., Reference Nadkarni, Bhatia, Velleman, Orford, Velleman, Church, Sawal and Pednekar2019) (Fig. 1), delivered in five sessions over 10 weeks. The intervention was delivered face-to-face, at a mutually convenient venue (e.g. home). The control arm received EUC, which consisted of an information leaflet highlighting the nature and impact of alcohol-related problems, and sources of help for the AFM. In both arms, we referred participants with serious concerns (e.g. suicidal ideation) for further specialised treatment or urgent care.
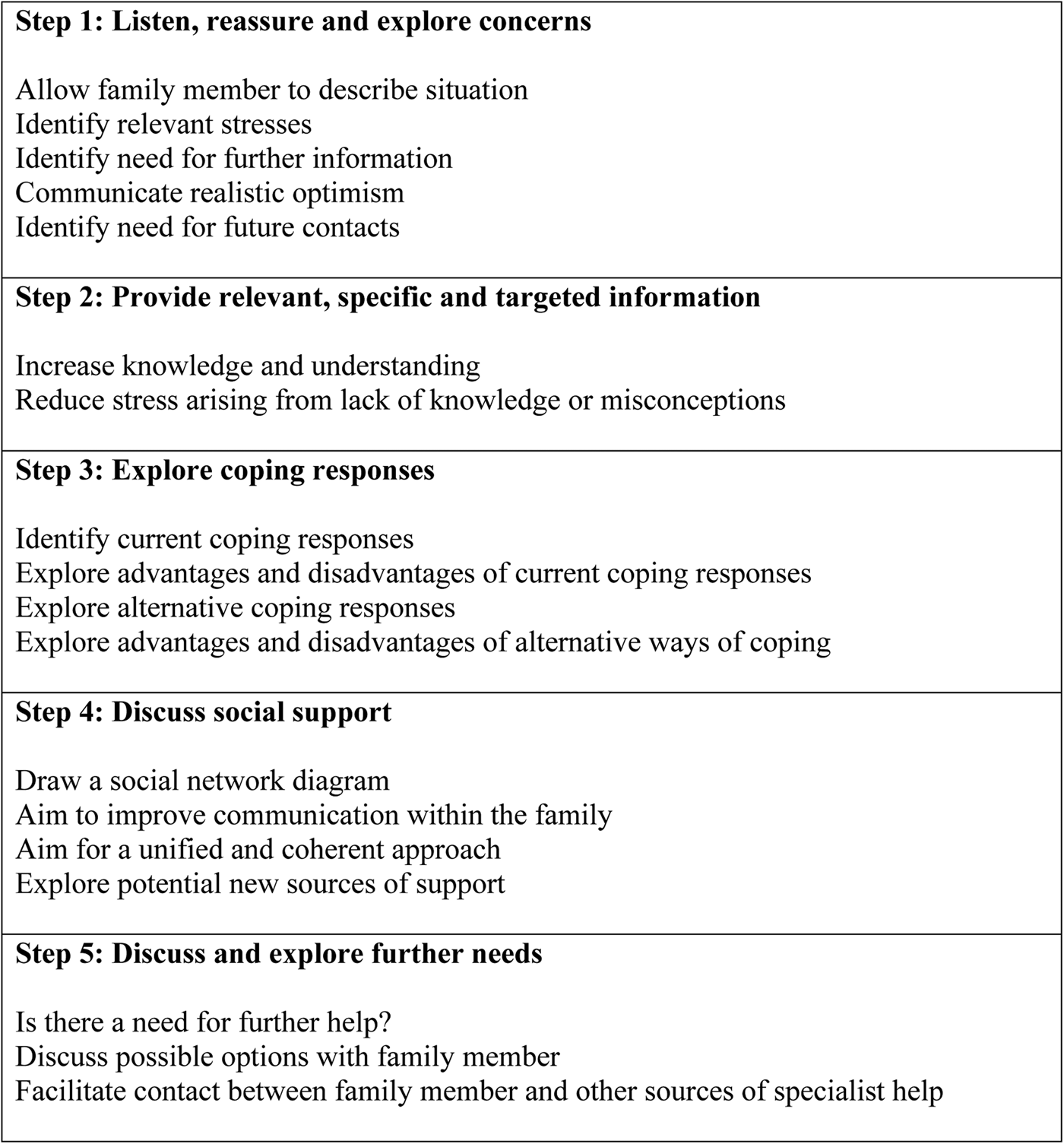
Fig. 1. The 5-Step Method: 5 steps to support family members affected by addiction problems.
Interventionists
We recruited lay counsellors through referrals from community gatekeepers, advertisements and word-of-mouth publicity. The lay counsellors had no previous formal training in the field of mental health, were from the same community as the target population and were fluent in the vernacular languages. The lay counsellors were chosen after a thorough competency evaluation process and underwent rigorous training and supervision. Training entailed expert-led sessions on the 5-Step Method, followed by refresher trainings to address any identified learning needs. Supervision included both, individual and group, peer and expert-led supervision, where the counsellors discussed ratings on randomly selected recorded sessions on the SAFE therapy quality scale developed for the study, and also discussed feedback on challenges and barriers during sessions.
Baseline assessments
All eligible participants who consented to participate were administered the following baseline assessments: socio-demographic questionnaire, Coping Questionnaire (CQ) (Orford et al., Reference Orford, Templeton, Velleman and Copello2005) measuring the AFM's coping strategies, Symptom Rating Test (SRT) (Kellner and Sheffield, Reference Kellner and Sheffield1973) measuring physical and psychological symptoms, Family Member Impact (FMI) questionnaire (Orford et al., Reference Orford, Templeton, Velleman and Copello2005) measuring the impact of the alcohol use on various aspects of the AFM's life, and Alcohol, Drugs and the Family Social Support Scale (ADF-SSS) (Toner and Velleman, Reference Toner and Velleman2014) measuring social support for the AFM. The CQ, SRT, FMI and ADF-SSS are standardised tools and have undergone rigorous psychometric testing for reliability and validity.
Process indicators
Process evaluation was conducted to examine acceptability and feasibility of recruitment procedures and treatment, fidelity of implementation, moderation of impact and contextual factors associated with outcomes.
Outcomes
The primary outcome was the difference in mean SRT scores at 3 months. The secondary outcomes were mean differences in CQ, FMI and ADF-SSS scores at 3 months. Lower scores on all the measures, except the ADF-SSS, denote fewer symptoms, fewer attempts at coping and fewer negative incidents impacting the family member, respectively (Kellner and Sheffield, Reference Kellner and Sheffield1973; Orford et al., Reference Orford, Templeton, Velleman and Copello2005; Toner and Velleman, Reference Toner and Velleman2014). Other secondary outcomes included experience of physical and sexual violence. We conducted the outcome assessments between August and November 2016. The trial was completed in November 2016 when the 3-month outcome assessment ended.
Sample size
We aimed to recruit 50 participants in each arm, which was assumed to be sufficient to examine feasibility and acceptability of the intervention and trial procedures.
Statistical methods
Quantitative analyses were performed using STATA (version 14). The primary analysis was intention-to-treat at the 3-month endpoint, and secondary analyses at the 3-month endpoints, adjusted for baseline values. Per-protocol analysis was conducted in those who completed the trial. Missing outcome data were imputed by multiple imputation using baseline characteristics. An estimate of the effects of the intervention (relative to EUC), in terms of effect sizes are reported as crude and adjusted odds ratios (aOR) and standardized mean differences (s.m.d.) with 95% confidence intervals, as appropriate.
Ethics
Ethical approval was sought from the Institutional Review Board of the host institution and the Indian Council of Medical Research (reference number: UB_2016_022).
Results
Between May and August 2016, we recruited 101 participants in the study, of whom 51 were randomly allocated to the SAFE arm and 50 to the EUC arm (Fig. 2).
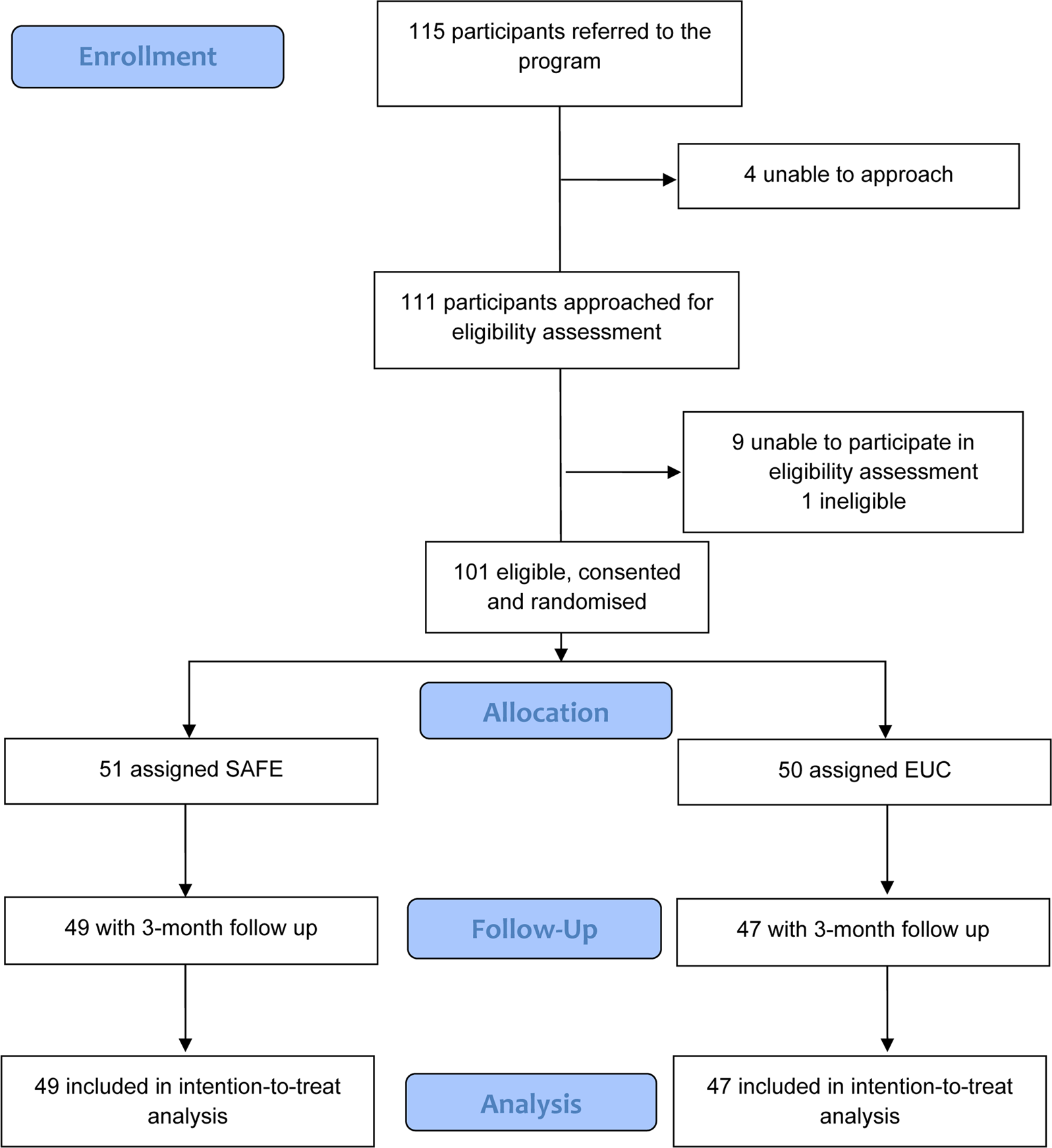
Fig. 2. CONSORT flowchart for reporting pilot and feasibility trials'
Baseline characteristics
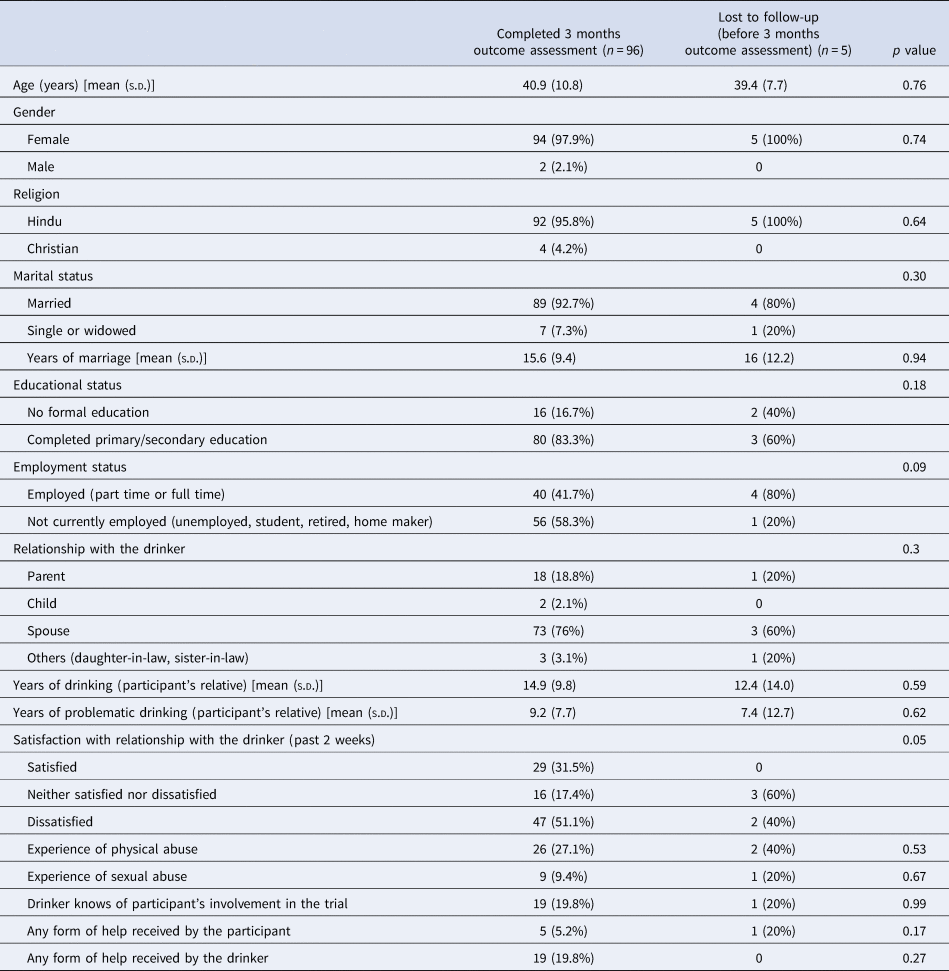
All of our participants were female apart from two who were both fathers of sons with drinking problems (Tables 1 and 2). Baseline characteristics were similar between the two arms, except for educational status and help-seeking by the drinking relative. A significantly higher proportion of those in the SAFE arm completed primary/secondary education compared to those in the EUC arm (90.2% v. 74%, p = 0.03). About 20% reported that their drinking relative had received treatment in the previous 3 months, and these were disproportionately recruited into the treatment arm (27% v. 10%, p = 0.02). Ninety-six participants (95%) completed outcome assessments (96% in the SAFE arm and 94% in the EUC arm).
Table 1. Baseline characteristics of trial participants by arm
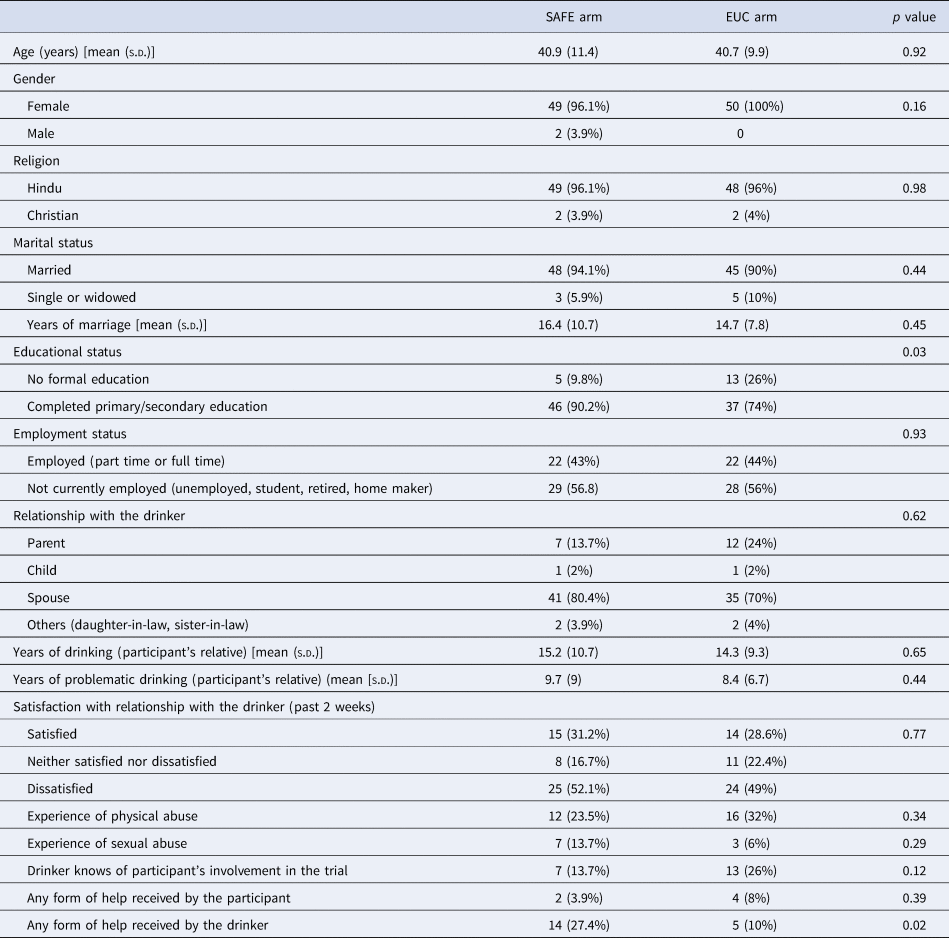
Table 2. Baseline characteristics of participants who completed outcome evaluation and those who were lost to follow-up
Experiences of family members
Across both arms, as reported by the AFMs at baseline, the average duration of the relatives' drinking was 14.7 (s.d. 10.0) years, and the average duration of problematic drinking behaviours was 9.1 (s.d. 7.9) years (Tables 1 and 2). At baseline, 28.7% of the participants expressed being ‘satisfied’ with their relationship, 18.8% reported being neither satisfied nor dissatisfied, and 48.5% expressed being dissatisfied. In total, 27.7% of participants reported being physically abused, and 9.9% reported being sexually abused. Only 5.9% of the participants had received any form of help in the past 3 months for the difficulties that they were experiencing in relation to the drinking behaviours of their relative. There were no significant differences between arms on satisfaction with relationship, experience of violence and help-seeking by the participant.
Indicative impact of the intervention
At follow-up, the mean SRT, CQ, FMI and ADF-SSS scores were all higher in the SAFE arm compared to the EUC arm, however, the between-group adjusted mean differences were only statistically significant for ADF-SSS scores (AMD −6.05, 95% CI −10.98 to −1.12, p 0.02) (Tables 3–6). The SSCS model suggests that higher scores on each of the outcome measures (except ADF-SSS) suggest worse outcomes. Hence, the only outcome which went in the positive direction in the SAFE arm was ADF-SSS (i.e. social support). In comparing the change scores at 3 months (i.e. extent of change from baseline to outcome per arm), the change in CQ and ADF-SSS was greater in the SAFE arm, with the former changing in a negative direction (i.e. higher score indicating worse coping) and the latter changing in a positive direction (i.e. higher score indicating better social support). The change in SRT and FMI was greater in the EUC arm, with both changing in a positive direction (i.e. lower SRT score indicating lesser strain and lower FMI score indicating lesser stress). However, the between-group adjusted mean differences were not significant for any of these outcomes. In comparing sub-scale scores, there was a significant increase only in ‘engaged style’ of coping and ‘positive functional support’ in the SAFE arm. With regards to the experience of abuse, a greater (although non-significant) proportion of participants reported experiencing physical abuse in the EUC arm than in the SAFE arm (21.3% v. 12.5%, aOR 1.86, 95% CI 0.59–0.84, p = 0.29), while for sexual abuse, the difference was of 2.9% in the EUC arm v. 2.6% in the SAFE arm (aOR 1.27, 95% CI 0.08–21.28, p = 0.86).
Table 3. Intervention effect on SRT, CQ, FMI and ADFSSS scores at 3 months

a Adjusted for educational status, any form of help received by the drinker at baseline and counsellor effects at baseline.
Table 4. Change scores (total score) at 3 months
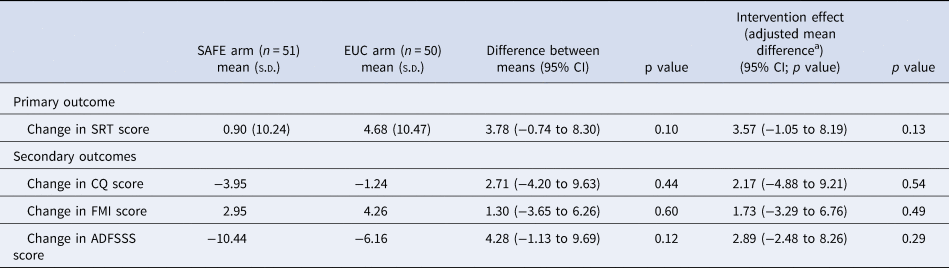
a Adjusted for educational status, any form of help received by the drinker at baseline and counsellor effects at baseline.
Table 5. Intervention effect on SRT, CQ, FMI and ADFSSS sub-scale scores
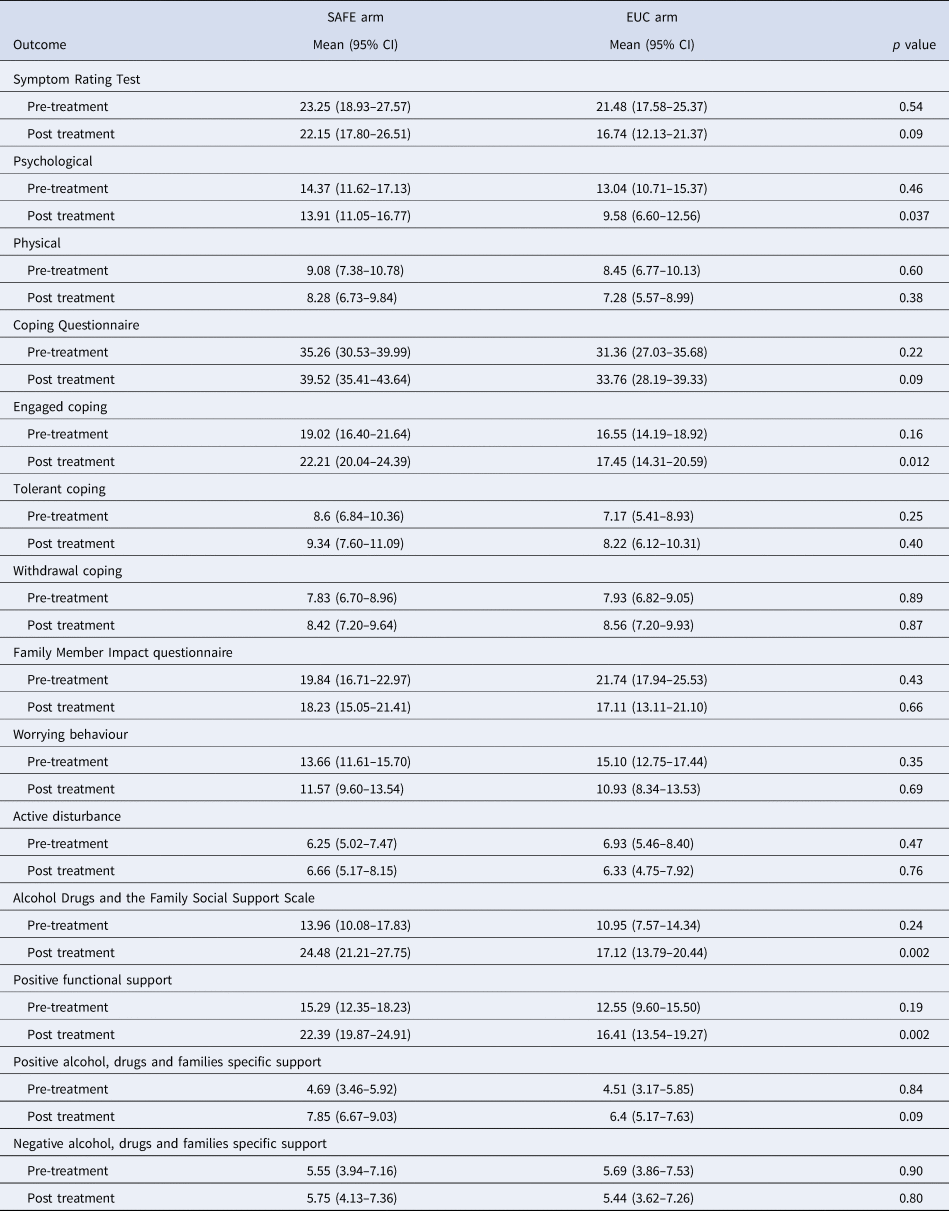
Table 6. Intervention effect on change in SRT, CQ, FMI and ADFSSS sub-scale scores

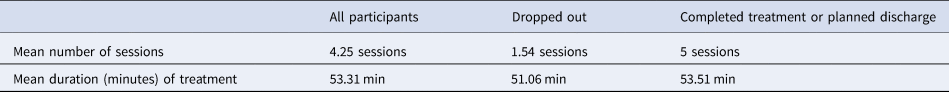
Acceptability and feasibility of the intervention
One hundred fifteen participants were referred to the trial; 95 were referred by community gatekeepers and 20 (17.4%) were self-referred (Tables 7 and 8). One hundred eleven were approached to assess eligibility, and 102 completed eligibility assessment. One hundred one participants were eligible, consented to randomisation and completed baseline assessments. Of the 51 participants who entered treatment, 40 (78%) completed treatment/had a planned discharge (i.e. all five sessions). There were no statistically significant differences in baseline characteristics between those who completed treatment and those who did not. Of the remainder (n = 11), three dropped out before the first session, five dropped out after the second session and three dropped out after the third session. The average number of sessions conducted was 4.25. The mean duration of sessions was 53 min. The mean duration reduced from session 1 to session 3 before increasing again in the final session. For the majority of the participants, the first session was conducted in the clinic, and this proportion gradually reduced over the duration of treatment, with most sessions being conducted at participants' homes by the fourth session. Finally, the mean number of days between sessions increased as the treatment progressed from session 1 to session 4 (from 16 to 31 days). There were seven serious adverse events (three in the SAFE arm, and four in the EUC arm) reported over the trial period. All of the serious adverse events reported were violence perpetrated by the drinking relative (and in two cases, violence was reported to be experienced by other family members).
Table 7. Details of counselling sessions
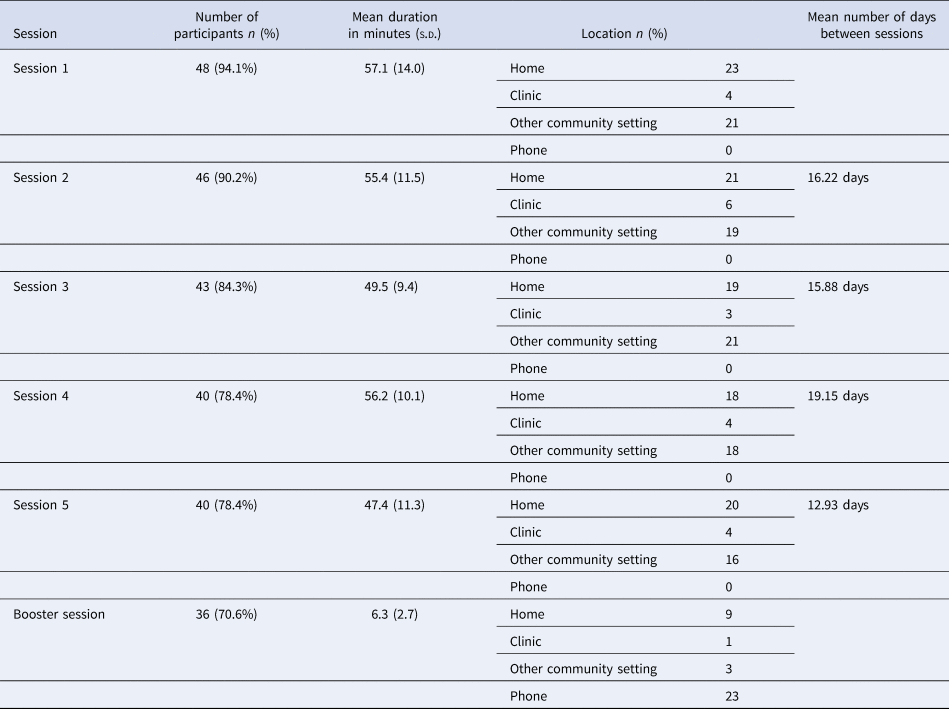
Table 8. Details of counselling sessions in treatment completers and dropouts
Discussion
Our pilot RCT has demonstrated that the intervention has good acceptability and feasibility, but has only shown positive indicative impact on one of the social support measures: positive functional support. These findings are consistent with our previous work, where we conducted a case series with a uncontrolled treatment cohort of AFMs, and again found positive changes only in social support [in fact, that study showed positive changes in both positive functional support and positive alcohol, drugs and families specific support, as well as an increase in strain and engaged coping (Nadkarni et al., Reference Nadkarni, Bhatia, Velleman, Orford, Velleman, Church, Sawal and Pednekar2019)]. However, these findings are inconsistent with most other 5-Step Method work outside India. In almost all major evaluations of the intervention, the 5-Step Method has led to significant reductions in strain, and a reduction in engaged and tolerant coping (Copello et al., Reference Copello, Templeton, Orford and Velleman2010a, Reference Copello, Templeton and Powell2010b). A key question therefore is how to account for these differences. One potential attribution is that they might be related to how culture influences the experiences of AFMs. It has been suggested that different cultures and contexts influence the accumulated burden that AFMs hold, and the social support available for them; and that these differences may influence the core AFM experience (Orford, Reference Orford2017). This is especially true for our setting where our previous work has demonstrated both high levels of burden and the inaccessibility of effective social support (Church et al., Reference Church, Bhatia, Velleman, Velleman, Orford, Rane and Nadkarni2018).
The high uptake and completion of the intervention suggest that it was acceptable to family members; and indicate that there was a felt need for the intervention, it was possible to identify AFMs through gatekeeper or self-referrals, and it was acceptable to participants. Also, it implies that a program focused on AFMs can be implemented in this context with good initiation and follow-up rates. Further, in resource-constrained settings, it is feasible and acceptable to train lay counsellors to deliver a psychosocial intervention for families in community settings. From the perspective of evaluation research, it is possible to efficiently implement procedures that are critical in conducting a definitive RCT of the SAFE intervention, which had been our planned next step.
However, despite the fact that feasibility studies are not powered to assess effectiveness, our quantitative findings raise several questions. Does the fact that, for the participants receiving SAFE, stress and strain did not significantly reduce, and there was an increased use of coping methods which studies in other countries have suggested may be less helpful ways of coping, suggests that the intervention may (or does) not work in our context? Although our study cannot empirically answer that question, we can speculate about a number of potential explanations. First, the philosophical focus of the intervention may not be the best ‘cultural fit’ for the Indian context. The intervention is focused solely on empowering family members in their own right, and is thus a significant shift from the traditional neglect or token involvement of family members to direct engagement/focus on family members. In a ‘collectivist’ culture such as India which ascribes greater importance to the family as a unit, the focus of the SAFE intervention on the individual may have led to a mismatch. To illustrate this point, we would like to draw upon one of our anecdotal experiences from our process and qualitative work. AFMs strongly asserted that although they were burdened, their primary interest was not to receive help for themselves; instead their preference was that their drinking relative should engage in any form of treatment, and change his drinking behaviours, which would make ‘all their problems go away’. Hence, it may be that AFMs in our context retained a focus on the drinking relative and did not see the appropriateness or the possible usefulness of an intervention which might exclusively support the AFMs. The intervention was developed and has been used elsewhere in order to help AFMs in their own right by focusing on their coping and support systems; and it is possible that the AFMs whom we recruited in this context did not want this or understand its potential helpfulness, and instead wanted an intervention which would persuade their drinking relatives to seek treatment. As a result, by focusing on how they as AFMs were experiencing the impact of their drinking relative, our intervention may have increased stress and strain in family members.
Another possibility could be that the health of these AFMs did not improve because their situation remained the same: the drinker had not stopped drinking (which was their primary perceived need), and hence their perception might have been that ‘nothing had changed’ and hence they did not change either.
A related point is that this sample scored considerably lower on especially stress (FMI), but also on strain (SRT) than have other samples drawn from other countries and cultures [pre-treatment FMI scores in other countries are typically in the range of 30, whereas pre-treatment FMI scores in this sample were 19.84 (SAFE arm) and 21.74 (EUC arm); pre-treatment SRT scores range from 28.5 to 36.8, whereas here they were 23.25 (SAFE) and 21.48 (EUC)] (Copello et al., Reference Copello, Templeton, Orford and Velleman2010a, Reference Copello, Templeton and Powell2010b). The culture in India creates a situation where women are made to ‘accept their lot’ and as a result accept that they have to live with men who drink too much, and that sometimes they suffer as a result of that; and hence many women are relatively fatalistic about this (Stanley, Reference Stanley2012). Perhaps, by getting AFMs to undergo five sessions of a counselling intervention which got them to reflect on this situation, and by discussing change, it may have allowed these AFMs to realise that the impact and the effects on themselves were even worse than they had previously considered. Related to this, the intervention focuses on ‘alternatives to current ways of coping’ but in the study context it is possible that many of these AFMs might have felt that their alternatives were so limited that they could not change their situations. Hence our intervention may have raised awareness and self-reflection (e.g. regarding the negative impacts and their own responses), without alleviating any problems (e.g. getting the husband to stop drinking; or generating reasonable alternatives to current ways of coping). Again, there is some corroboration for this view, in that the style of coping which increased in this sample was engaged coping, one in which the focus is very much on the drinker and the drinking.
One further alternative explanation could be that the brief nature of our intervention was not adequate to lead to any longer-term positive changes in AFMs, especially in a context where ‘talking therapies’ are a novel and quite alien concept (Murthy, Reference Murthy2014).
A different explanation might relate to the competency of counsellors in delivering the 5-Step Method, which in previous studies has been delivered by specialists (Copello et al., Reference Copello, Templeton, Orford, Velleman, Patel, Moore, MacLeod and Godfrey2009; Velleman et al., Reference Velleman, Orford, Templeton, Copello, Patel, Moore, Macleod and Godfrey2011). It could be argued that the treatment quality could have been affected because the delivery agents were not trained professionals, but were lay counsellors. However, there is an extensive evidence base of the effectiveness of non-specialist health worker-delivered mental health interventions in LMICs (van Ginneken et al., Reference van Ginneken, Tharyan, Lewin, Rao, Meera, Pian, Chandrashekar and Patel2013; Nadkarni et al., Reference Nadkarni, Weiss, Weobong, McDaid, Singla, Park, Bhat, Katti, McCambridge, Murthy, King, Wilson, Kirkwood, Fairburn, Velleman and Patel2017; Patel et al., Reference Patel, Weobong, Weiss, Anand, Bhat, Katti, Dimidjian, Araya, Hollon and King2017; Singla et al., Reference Singla, Kohrt, Murray, Anand, Chorpita and Patel2017).
Our recruitment strategy may also explain the characteristics of participants, and the mixed results we found. We recruited participants through self and gatekeeper referrals, which meant that our sample would have included both those who were treatment seekers, and those who were not seeking treatment for their experiences or problems. Recruiting non-treatment seekers meant that there may have been a sub-group of participants who were less likely to fully engage in treatment, and report positive change (the lower levels of reported stress and strain offer some corroboration for this). Finally, it may be that the quantitative measures we have used are not culturally sensitive and adequate enough to capture actual and relevant changes that AFMs experience in their lives.
The second fundamental question is about the differential direction of change across the various domains of the experience of AFMs: Why did only social support scores increase? One of the predictors of future help-seeking is past experience of accessing help. In an Australian study, AFMs reported that positive help-seeking experiences in the past made them more likely to access services (McCann and Lubman, Reference McCann and Lubman2018). Our intervention provided AFMs with a safe space where they felt heard, and attempted to empower them to cope better; but for many this was the first such help that they had ever accessed. It is possible that the positive experiences that AFMs experienced during the SAFE sessions may have increased the likelihood of further help-seeking and hence led to an increase in social support scores.
Despite the improvement in perceived support, there was no positive change in the other domains of the SSCS model, and this could suggest a number of possibilities. One is that positive impact in this sample may only be seen over a longer time span. Alternatively, the available social support structures were perhaps not adequate, in terms of whether these were accessible, or even the quality of support offered. Hence, although there may have been increased support, the impact of the support in terms of improving the situation of AFMs may not have been positive. Given the relatively inextricable contexts that AFMs come from, this increased support may have not led to any significant change in the stress, strain and coping of AFMs. Finally, the increased support reported by the AFMs could actually be the support provided by lay counsellors through the SAFE intervention. This explanation is also likely given that our previous work has demonstrated the inaccessibility of social support (Church et al., Reference Church, Bhatia, Velleman, Velleman, Orford, Rane and Nadkarni2018).
To conclude, there are five major implications of our results. First, the fast recruitment and high acceptance rates for the intervention demonstrate that there is a great need for interventions aimed at AFMs in this context; and the high adherence rates demonstrate that the AFMs found the experience of receiving the intervention relevant and helpful. Both our anecdotal and qualitative data suggest that the large majority of the AFMs who received the intervention felt that they needed an intervention, stated that they felt better as a result of it and appreciated their meetings with their counsellors. These findings then reinforce what is known from other studies in India and elsewhere: that AFMs carry a high burden and a there is a major need for interventions to reduce this burden.
Second, we now have a better understanding of how this intervention worked in the setting. We found that AFMs in both arms showed at the time of the 3-month follow-up greater levels of stress and strain than at baseline, and that those in the intervention arm both increased the amount of engaged coping they used and reported greater changes in positive social support. Clearly this study was not powered to demonstrate significant results, but these preliminary findings strongly suggest that this intervention did not lead to expected changes – that is to reductions in especially strain (symptoms) and in AFMs generally feeling more empowered and more ‘in control’ of their situation. The rise in engaged coping suggests instead that, by focusing their attention on their situations, the intervention caused these AFMs to attempt to intervene at an even higher level than they had done before, yet with them still not being able to change the situation.
This relates to a third implication; that the intervention did not address the most pressing problem for these AFMs, which was to ensure that their relative with a drinking problem received effective treatment and stopped drinking. In some ways this is not an uncommon issue within the 5-Step Method, where many AFMs come for help with a focus on their problem relative. But in this context, it proved extremely challenging to assist these AFMs to see that if they were able to change their own behaviour, and to develop alternative ways of dealing with the problem, this might improve relationships in the family, and reduce their stress and strain. Our counsellors reported that many AFMs seemed extremely ‘stuck’, or alternatively lived in contexts where change seemed exceedingly difficult, and found it very problematic to generate alternative coping strategies, even with considerable help from the counsellors. One solution to this might be to broaden the scope of such interventions, for instance, planning horizontal approaches to care, primarily addressing the needs of both, the relative with the drinking problem and their AFMs. Keeping in line with this proposed shift of focus, there is scope to explore the relevance of offering 5-Step Method with a supplemented focus on the relative with the drinking problem, as well as other systemic and collaborative approaches to family-based interventions such as the Community Reinforcement and Family Training where family members and their relative with the drinking problem are jointly engaged (Copello et al., Reference Copello, Velleman and Templeton2005).
Fourth, the findings from this pilot RCT corroborated our earlier findings from both our formative work and other work undertaken within India, which is that domestic violence is a major and unresolved problem for many AFMs. Some of this violence is alcohol-related; but some is simply endemic to a culture where violence against women is an accepted and often largely ignored part of the landscape. Further work is needed to create interventions for AFMs which address this wide range of needs and complex situations (Copello et al., Reference Copello, Templeton and Velleman2006). This point leads into a wider implication from this study: how socio-cultural factors influence the impact of interventions. Almost all of our participants were women, who reported experiences which clearly emphasised how patriarchal structures continue to disadvantage them (e.g. the high prevalence of violence). Although the focus of this intervention was on empowerment, it was not uncommon for women to express their needs through the lens of their partners and children, to report multiple burdens as a result of assuming the primary caregiver's role, to report various expressions of violence, and to report poor social support (Church et al., Reference Church, Bhatia, Velleman, Velleman, Orford, Rane and Nadkarni2018; Nadkarni et al., Reference Nadkarni, Bhatia, Velleman, Orford, Velleman, Church, Sawal and Pednekar2019). It is important to note that these experiences are not unique to Goa: previous studies with AFMs have found similar stories, particularly from women (Rey et al., Reference Rey, Mora-Ríos, Sainz and Aguilar2010; Stanley, Reference Stanley2012). This interplay of gender with the experience of being an AFM suggests the need for the inclusion of other perspectives (e.g. a feminist understanding) in planning psychosocial interventions (Orford et al., Reference Orford, Velleman, Copello, Templeton and Ibanga2010b). An example of this feminist approach is from a Mexican qualitative study with AFMs, where female participants experienced positive change in their lives by learning how to change their locus of control (moving from ‘women being objects to subjects of their own destiny’) (Rey et al., Reference Rey, Mora-Ríos, Sainz and Aguilar2010).
Some limitations of our study include one of the ways in which we recruited participants (through self-referrals), which may result in a non-representative sample, as participants who volunteer for a trial may disproportionately possess characteristics related to the outcome. Another important limitation was the reliance on self-reports for outcome evaluation, which introduce an element of subjectivity, and are prone to response bias.
The following characteristics are key strengths of our study. First, we focused on a target population that is considered to be a ‘hidden’ or ‘silent’ and hard-to-reach group. The primary platform through which we recruited our sample was the community, which expanded the potential reach of our study, and improved the representativeness of our sample. Second, to the best of our knowledge, this is the first study that has systematically examined an evidence-based intervention for AFMs ‘in their own right’ in the Indian context. Third, our community-based participatory research approach allowed for a range of community stakeholders to inform the design, conduct and evaluation of the intervention.
Conclusion
Our study aids the process of translational research by adopting frameworks that have an established evidence base and implementing these frameworks in a culturally appropriate manner to newer underserved populations. Given our mixed findings, further work is required to unpack how the intervention affects AFMs and what further adaptations are required to make the intervention relevant to the Indian context.
Supplementary material
The supplementary material for this article can be found at https://doi.org/10.1017/gmh.2022.41.
Acknowledgements
We would like to acknowledge and are grateful for the support from our local community stakeholders, including community gatekeepers, counsellors and the research team of the SAFE program.
Author contributions
UB drafted the manuscript and all authors reviewed and approved it. UB, RV and AN were responsible for design of the overall trial; UB, RV, GV and AN were responsible for training, supervision and competency assessments of the intervention delivery agents; UB, RV and AN were responsible for intervention content and data gathering instruments; UB was responsible for trial conduct and database curation and management; and UB was responsible for the analyses and was supported by AG and AJ. Protocol: Available on ClinicalTrials.gov
Financial support
This research was funded by a Wellcome Trust DBT India Alliance Research Training Fellowship grant to UB (IA/RTF/15/1/1018). The funder had no role in the study design, data collection, data analysis or writing of the manuscript. UB has full access to all the data collected in the study and had final responsibility for the decision to submit the manuscript for publication.
Conflict of interest
None.
Ethical standards
The authors assert that all procedures contributing to this work comply with the ethical standards of the Sangath Institutional Review Board, national guidelines on human participant research and with the Helsinki Declaration of 1975, as revised in 2008.













