Alcohol use disorders generate considerable cost to society and the health system in particular. In the UK it is estimated that alcohol use disorders are linked to 22 000 premature deaths and cost the economy £20 billion annually. 1 A recent national alcohol needs assessment found that over 7 million adults in England are hazardous or harmful drinkers and a further 1.1 million are alcohol dependent. Reference Drummond, Oyefeso, Phillips, Cheeta, DeLuca and Perryman2 Alcohol is a leading cause of morbidity and mortality, and reducing alcohol-related harm is a key priority of the UK government with publication of the National Alcohol Harm Reduction Strategy 3 and the Choosing Health White Paper. 4
There are now 13 meta-analyses and/or systematic reviews of brief alcohol interventions, including five specifically focused on primary care. Reference Kaner, Beyer, Dickinson, Pienaar, Campbell and Schlesinger5–Reference Bertholet, Daeppen, Wietlisbach, Fleming and Burnand9 The greatest evidence of efficacy is in populations identified in primary care settings. Overall, there is a 20–30% reduction in alcohol consumption following brief intervention compared with control conditions, and several studies have found significant reductions in healthcare utilisation in the brief intervention group. One review of 34 brief intervention studies indicates that brief interventions are only more effective than control conditions in people who drink excessively identified by opportunistic screening rather than in those seeking alcohol treatment. Reference Moyer, Finney, Swearingen and Vergun10
Among this wealth of positive evidence regarding efficacy there is also some ambivalence towards the effectiveness of brief interventions. Heather Reference Heather11,Reference Heather12 suggests that brief interventions delivered in naturalistic settings would probably have smaller effects than efficacy studies tend to suggest. Edwards & Rollnick Reference Edwards and Rollnick13 suggest we should exercise some caution in generalising from efficacy studies to effectiveness. Studies of efficacy often have systematic biases associated with the population under study and tend to be an evaluation of an intervention delivered by motivated practitioners. An appropriate methodology for evaluating effectiveness should involve a pragmatic balance between internal and external validity providing a better indication of ‘naturalistic effectiveness’. Howard Reference Howard14 also noted the limitations in rigorous economic evaluations in the area of brief interventions – there is a clear need for pragmatic randomised clinical trials of brief interventions that address effectiveness and cost-effectiveness aspects of brief interventions.
A further problem with the research literature on brief interventions stems from the varying definitions of interventions used in different studies. Reference Heather11,Reference Jonson, Hermansson, Rönnberg, Gyllenhammar and Forsberg15 What is considered a brief intervention in one study is considered an extended intervention in another. A number of reviews and meta-analyses fail to take this intervention heterogeneity into account. Reference Heather11,Reference Drummond16
Screening for alcohol use disorders identifies a wide range of needs, varying from hazardous and harmful drinking to severe alcohol dependence, that are likely to require a range of types and intensities of treatment. Stepped care interventions offer a potentially resource-efficient means of meeting the needs of individuals in more severe cases. Stepped care provides a means of delivering high-intensity and more costly interventions only to those who fail to benefit from less intensive interventions, more in keeping with the way clinical care is typically delivered than the application of blanket brief interventions. Further, evidence from surveys of primary care practitioners highlights a reluctance to implement brief interventions, in part because they lack the skills to deal with the more severe cases identified. Reference Deehan, Templeton, Taylor, Drummond and Strang17 Stepped care approaches have gained acceptance in the smoking cessation field, Reference Orleans, Orleans and Slade18,Reference Abrams, Orleans, Niaura, Goldstein, Prochaska and Velcier19 as well as other areas of medicine such as hypertension treatment, but they also represent an important development in the alcohol treatment field. Reference Sobell, Sobell, Baer, Marlatt and McMahon20,Reference Breslin, Sobell, Sobell, Buchan and Cunningham21
Stepped care provides a pragmatic clinical algorithm that addresses the needs of a spectrum of alcohol use disorders and provides appropriate interventions for those who fail to benefit from brief interventions. This is a pragmatic pilot study to assess the feasibility, effectiveness and cost-effectiveness of a stepped care alcohol intervention in primary care comparing stepped care with brief interventions alone.
Method
Study design
A prospective pragmatic randomised controlled trial in which eligible consenting participants where randomised with equal probability to either stepped care or minimal intervention. Randomisation was conducted remote from the research centres by the trial randomisation service at the University of York. Block randomisation with seeded random elements was used to minimise the possibility of subversion. Follow-up was conducted at 6 months post-randomisation by a researcher masked to the allocated group.
Sample size
The closest study of opportunistic screening and intervention in a UK primary care population is that of Wallace et al. Reference Wallace, Cutler and Haines22 In this study the standardised effect size between intervention and control was 0.36 for males. To replicate this effect requires 177 participants to gain 80% power to detect a difference at the 5% significance level. Assuming that only 75% will be followed up at 6 months inflates this figure to 236, 118 in each randomised group. However, we managed to recruit 112 individuals in total in the time available. So this is best regarded as a pilot study to establish feasibility and to determine the effect size on which to power a larger study.
Participants
Participants were consecutive male attendees at six primary care practices in South Wales. Females were excluded since at the time of designing the trial meta-analyses suggested smaller effect sizes of brief alcohol interventions in women than in men, which would have required a much larger sample size than the funding for the study would allow. However, subsequent research suggests equivalence of outcomes in males and females, and our ongoing research (see below) includes both genders.
Eligible male patients were aged 18 years or more, had a self-completion Alcohol Use Disorders Identification Test (AUDIT) Reference Saunders, Aasland, Babor, De La Fuente and Grant23 score ≥8 and/or a diagnosis of an alcohol use disorder assessed using ICD–10 criteria at baseline assessment (using the CIDI Alcohol Use Disorders interview 24 conducted by the research assessor) and/or were drinking above Department of Health guidelines for hazardous drinking as assessed by the Time Line Follow Back Reference Miller25 measure of alcohol consumption (see below) (>21 units/week or >8 units/day), lived within commuting distance of the primary care practice, had not received treatment for an alcohol use disorder in the previous 180 days and were willing to consent to receive either treatment and take part in follow-up assessments.
Patients were not eligible if they had a primary drug dependence other than alcohol, suffered from a severe mental or physical illness, severe cognitive impairment or had legal issues that might have interfered with follow-up.
Procedure
Patients attending primary care practices were asked by a practice nurse to complete an AUDIT questionnaire embedded within a general lifestyle questionnaire, which was scored by the practice nurse. Any patient who scored 8 or more was then provided with an information sheet about the study and asked if they would consider taking part. Those willing to participate were offered an appointment with the research assessor within 1 week of screening.
At the initial research assessment, eligibility criteria were established and those eligible invited to consent to participation in the study. Those who were eligible and consented were randomised using the remote randomisation service at the University of York and allocated to either stepped care (intervention group) or minimal intervention (control group).
Six months after randomisation, patients were contacted by the research assessor, who made an appointment for a follow-up interview. The research assessor was masked to the patients' allocation.
Interventions
Control group
Patients received a 5-minute directive advice session from a practice nurse addressing the need for them to reduce their alcohol consumption. Patients also received a short self-help booklet outlining the consequences of excessive alcohol consumption and including details on where to seek help locally for alcohol problems.
Intervention group
Patients received a sequential series of interventions according to need and response after each successive step.
Step 1. All patients randomised to this group were offered a 40-minute session of behaviour change counselling Reference Rollnick, Butler, Allison, Barth, Rosengren, Balliostes, Miller and Rollnick26 from a trained practice nurse. Each patient was invited for follow-up with the same nurse 28 days after the initial session. Patients who had consumed >21 units of alcohol in any one week or >10 units in any one day during the 28-day period were referred to step 2.
Step 2. All patients referred to step 2 were offered a maximum of four 50-minute sessions of motivational enhancement therapy Reference Miller, Zweben, DiClemente and Rychtarik27 conducted by a trained alcohol counsellor. Sessions were held at the primary care practice and scheduled for one per week over a 4-week period. Each patient was invited for a follow-up with the practice nurse 28 days after the final session. Patients who had consumed >21 units in any one week or >10 units in any one day in the 28-day period were referred to step 3.
Step 3. Patients were referred to the local community alcohol team for specialist intervention. There was no limit on duration or intensity of treatment, which could encompass, where necessary, detoxification, in-patient treatment, out-patient counselling, relapse prevention and drug therapy. The clinical protocol included a caveat that any patient in the intervention group who needed urgent referral to step 3 at any stage could be referred without going through intermediate care steps.
Study measures
Primary outcome
The primary outcome measure was alcohol consumption as measured over 180 days using the Time Line Follow Back method. Reference Miller25 This method generates three outcomes: total alcohol consumed in the period, mean number of drinks per drinking day and percentage of days abstinent.
Secondary outcomes
Motivation was measured using the Readiness to Change Questionnaire (RTCQ), Reference Rollnick, Heather, Gold and Hall28 specifically designed to assess stages of change in opportunistic brief interventions for people who drink excessively. The 12-item RTCQ allocates scores for each of three stages of change: pre-contemplation, contemplation and action. Scores range from −10 (pre-contemplation) to +10 (action).
Alcohol dependence was measured using the Severity of Alcohol Dependence Questionnaire, Reference Stockwell, Hodgson, Edwards, Taylor and Rankin29 which addresses five components of alcohol dependence: physical withdrawal, affective withdrawal, withdrawal relief, alcohol consumption and rapidity of reinstatement. The instrument is self-completed and provides a severity score ranging from 0 (no dependence) to 60 (very severe dependence).
Alcohol-related problems were measured using the Alcohol Problems Questionnaire (APQ). Reference Drummond30 The APQ contains 44 items across eight problem domains (friends, money, police, physical, affective, marital, children and work). The first 23 items are applicable to all individuals and are referred to as the ‘common’ subscale. This subscale ranges from 0 (no problems) to 23 (many problems).
Self-efficacy was measured using the Situational Confidence Questionnaire. Reference Annis and Graham31 This questionnaire assesses an individual's confidence to resist the urge to drink in a variety of situations. The overall score provides a range from 0 (not at all confident) to 100 (very confident).
Quality of life was measured using an established generic quality-of-life measure, the Short Form–12 (SF–12). Reference Ware, Kosinski and Keller32 The SF–12 generates two component scores relating to physical and mental health. The scores are standardised and norm-based on UK populations. The scores range from 0 to 100 with a standardised population mean of 50.
Economic evaluation
The economic evaluation involved four different components: the costs of training; the costs of the interventions; changes in social costs; and changes in quality-adjusted life-years (QALYs). The costs of training and interventions were derived from therapist and participant take-up recorded at the time of the trial. Local costs of salaries, overheads and premises were used with the take-up data to estimate costs. We calculated participant social costs from a specifically designed questionnaire to ascertain healthcare, social care and accident-related service utilisation along with criminal offences committed 6 months prior to and 6 months after randomisation. Unit costs were derived from national references for service utilisation Reference Netten, Rees and Harrison33,Reference Coyle, Godfrey, Hardman and Raistrick34 and government sources for the cost of crime. Reference Brand and Price35 Health outcomes were assessed using QALYs using the EQ–5D at baseline and 6 months with population values. 36–Reference Richardson and Manca38 The EQ–5D is a generic instrument that measures health on five scales (mobility, self-care, usual activities, pain and discomfort, anxiety and depression).
Analysis
Owing to the pragmatic design of the trial, analysis was conducted as an intention-to-treat analysis whereby participants were analysed according to the group they were allocated to rather than the treatment they received. Comparison between groups at 6 months was adjusted using analysis of covariance (ANCOVA) to take into account variability in corresponding baseline scores.
From the economic data we calculated the net costs of stepped care and minimal intervention (treatment costs less any difference in social costs at 6 months compared with baseline social costs). Quality-adjusted life-years were calculated for both interventions measuring the area under the curve joining the points at baseline and 6 months. Reference Brooks, Rabin and de Charro37 As economic data tend to be skewed, we used bootstrapping techniques to obtain more reliable confidence interval estimates. As the assumptions required to use analysis of covariance are not assumed to hold with these economic data, we followed the advice of Vickers, Reference Vickers39 who suggests that comparing baseline less follow-up values for both intervention groups is an acceptable alternative. We divided the differences in the net costs of interventions by the difference in QALY gains to yield the incremental cost-effectiveness ratio. We estimated the sampling distribution of this ratio from 1000 bootstrapped samples and derived cost-effectiveness acceptability curves. Reference Fenwick, Claxton and Sculpher40 These curves plot the resulting probability that one intervention is better than the other against the maximum decision makers might pay for an additional QALY.
Analysis was conducted using SPSS version 13 for Windows and STATA version 10 for Windows.
Results
Sample characteristics
A total of 1794 male primary care attenders were screened at six primary care practices in South Wales. All patients approached by the practice nurse completed the screening questionnaire. Of these, 447 (25%) scored positive for an alcohol use disorder (AUDIT ≥8), all of whom met the eligibility criteria to take part in the study. Overall, 112 (25%) gave consent and were randomised: 54 to the intervention group and 58 to the control group. Those consenting to take part were older (mean 42.7 years v. 37.7 years) and had higher AUDIT scores (mean 13.7 v. 11.9). All participants randomised to the control group received minimal intervention and 96% (52/54) of those randomised to the intervention group received step 1. A further 31% (17/54) of the intervention group were referred on for step 2 and only one participant was referred on to step 3 for detoxification. In the latter case this occurred on presentation for step 1 because of symptoms of severe alcohol withdrawal.
Of those who were randomised, 81% were followed up at 6 months, 90% in the control group and 72% in the intervention group; Fig. 1 shows the full CONSORT diagram for the study. A total of 81% follow-up is acceptable for alcohol research studies.
The average age of participants was 43 years and they had drunk alcohol on average 62% of the previous 180 days, consuming on average 14 units of alcohol per drinking day (1 unit = 8 g ethanol). Both groups were evenly matched on demographics, primary and secondary outcomes at randomisation (Table 1).
Table 1 Mean (s.e.) participant demographics, and primary and secondary outcomes at baseline
| Intervention group (n = 54), mean (s.e.) | Control group (n = 58), mean (s.e.) | |
|---|---|---|
| Age, years | 41.4 (2.3) | 42.1 (1.9) |
| AUDIT score a | 13.6 (0.8) | 13.3 (0.7) |
| Alcohol consumption (previous 180 days) | ||
| Total number of drinks consumed in period b | 1699.6 (194.8) | 1423.0 (113.3) |
| Drinks per drinking day b | 15.2 (1.1) | 12.9 (0.8) |
| Percentage of days abstinent | 37.9 (3.8) | 36.6 (3.4) |
| Readiness to Change Questionnaire c | ||
| Precontemplation | 0.4 (0.6) | -0.5 (0.5) |
| Contemplation | 0.6 (0.6) | 1.0 (0.5) |
| Action | 0.1 (0.7) | 0.6 (0.6) |
| Alcohol Problems Questionnaire d | 5.6 (0.6) | 4.7 (0.4) |
| Severity of Alcohol Dependence Questionnaire e | 8.2 (0.9) | 8.8 (1.2) |
| Situational Confidence Questionnaire f | 72.8 (18.0) | 74.9 (17.8) |
| Quality of Life (SF-12) g | ||
| Physical health | 40.5 (1.0) | 40.6 (1.0) |
| Mental health | 45.6 (1.8) | 49.2 (1.4) |
AUDIT, Alcohol Use Disorders Identification Test; SF-12, Short Form-12.
a. Scores from 0 (low) to 40 (high).
b. One standard drink = 1 unit = 8 g of ethanol.
c. Scores from -10 (low) to +10 (high).
d. Alcohol Problems Questionnaire, common scale; scores from 0 (low) to 23 (high).
e. Scores from 0 (low) to 60 (high).
f. Scores from 0 (low) to 100 (high).
g. Scores from 0 (low) to 100 (high).
Primary outcomes
At 6 months both groups had reduced their consumption considerably from baseline (Table 2). Greater reduction was observed in the intervention group in terms of total alcohol consumed (–408.6 g v. −238.8 g) and drinks per drinking day (–2.4 v. −1.0) with an adjusted mean difference of 145.6 (95% CI −101.7 to 392.9) and 1.1 (–0.9 to 3.1) (Table 3) respectively. This difference was not significant at the 0.05 level, but the standardised effect sizes for drinks per drinking day and total alcohol consumed were comparable with previous studies of brief intervention (0.27 and 0.23 respectively).
Table 2 Mean (s.e.) participant primary and secondary outcomes change at 6 months from baseline
| Intervention group (n = 39), mean (s.e.) | Control group (n = 52), mean (s.e.) | |
|---|---|---|
| Alcohol consumption (previous 180 days) | ||
| Total number of drinks consumed in period a | -408.6 (128.2) | -236.8 (95.9) |
| Drinks per drinking day a | -2.4 (0.8) | -1.0 (0.8) |
| Percentage of days abstinent | 4.0 (2.9) | 6.21 (2.9) |
| Readiness to Change Questionnaire b | ||
| Precontemplation | 0.5 (0.7) | 0.5 (0.4) |
| Contemplation | 0.1 (0.6) | 0.1 (0.5) |
| Action | 2.7 (0.7) | 0.8 (0.7) |
| Alcohol Problems Questionnaire c | -1.5 (0.3) | -1.1 (0.4) |
| Severity of Alcohol Dependence Questionnaire d | -1.5 (0.6) | -1.2 (0.8) |
| Situational Confidence Questionnaire e | 3.0 (1.6) | 2.3 (1.5) |
| Quality of Life (SF-12) f | ||
| Physical health | -0.1 (0.6) | 0.1 (0.6) |
| Mental health | 3.2 (1.5) | 1.2 (1.0) |
| Health utility (EQ-5D) g | <0.1 (0.1) | <0.1 (0.1) |
a. One standard drink = 1 unit = 8 g of ethanol.
b. Scores from -10 (low) to +10 (high).
c. Alcohol Problems Questionnaire, common scale; scores from 0 (low) to 23 (high).
d. Scores from 0 (low) to 60 (high).
e. Scores from 0 (low) to 100 (high).
f. Scores from 0 (low) to 100 (high).
g. Scores from 0 (low) to 1 (high).
Table 3 Adjusted mean (s.e.) participant primary and secondary outcomes at 6 months a
| Intervention group (n=39), mean (s.e.) | Control group (n=52), mean (s.e.) | Difference in favour of intervention (95% CI) | |
|---|---|---|---|
| Alcohol consumption (previous 180 days) | |||
| Total number of drinks consumed in period b | 1028.5 (94.1) | 1174 (81.4) | 145.6 (-101.7 to 392.9) |
| Drinks per drinking day b | 10.8 (0.7) | 11.9 (0.6) | 1.1 (-0.9 to 3.1) |
| Percentage of days abstinent | 11.1 (0.9) | 11.8 (0.8) | -0.7 (-1.8 to 3.2) |
| Readiness to Change Questionnaire c | |||
| Precontemplation | 0.8 (0.5) | 0.6 (0.4) | -0.2 (-1.7 to 1.1) |
| Contemplation | 0.4 (0.5) | 0.7 (0.4) | -0.3 (-1.7 to 1.1) |
| Action | 2.0 (0.6) | 0.2 (0.5) | 1.8 (0.2 to 3.3)* |
| Alcohol Problems Questionnaire d | 2.9 (0.3) | 3.2 (0.3) | 0.3 (-0.6 to 1.8) |
| Severity of Alcohol Dependence Questionnaire e | 5.5 (0.7) | 6.1 (0.6) | 0.6 (-1.4 to 2.5) |
| Situational Confidence Questionnaire f | 77.5 (1.5) | 77.1 (1.3) | 0.4 (-4.3 to 3.5) |
| Quality of Life (SF-12) g | |||
| Physical health | 39.5 (0.6) | 39.7 (0.5) | -0.2 (-1.6 to 1.8) |
| Mental health | 50.5 (1.4) | 49.9 (1.2) | 0.6 (-4.2 to 3.0) |
| Health utility (EQ-5D) h | 0.7 (0.1) | 0.8 (0.1) | -0.1 (-0.1 to 0.1) |
a. Adjusted by analysis of covariance for corresponding baseline score.
b. One standard drink = 1 unit = 8 g of ethanol.
c. Scores from -10 (low) to +10 (high).
d. Alcohol Problems Questionnaire, common scale; scores from 0 (low) to 23 (high).
e. Scores from 0 (low) to 60 (high).
f. Scores from 0 (low) to 100 (high).
g. Scores from 0 (low) to 100 (high).
h. Scores from 0 (low) to 1 (high).
* Significant at <0.05 level.
Secondary outcomes
At 6 months both groups had a slight increase in attributes associated with precontemplation (intervention group 0.5 v. control group 0.5), contemplation (0.1 v. 0.1) and action (2.7 v. 0.8) stages of change. Adjusted analysis indicates that the mean difference between the groups showed that the control group had a greater level of precontemplation (–0.2; 95% CI −1.7 to 1.1) and contemplation (–0.3; 95% CI −1.7 to 1.1) but that the intervention group scored higher on action (1.8; 95% CI 0.2–3.3), which was significant at the 0.05 level.
Alcohol-related problems and dependence decreased and self-efficacy increased in both groups, but none of these was significantly different between groups. No significant differences in quality of life or mental health were seen between groups at follow-up.
Economic outcomes
The cost assumptions are shown in Table 4. In the control group participants received 5 minutes of brief advice and a self-help booklet. Using 2001 prices Reference Netten, Rees and Harrison33 the cost per minute of practice nurse time is £0.22; this includes salary, employer's National Insurance, superannuation and an 8% management overhead. We also add premises costs, at £0.54/m2 per hour, assuming a room of 8 m2, and the cost of the booklet at £0.13. Thus, the total cost for the minimal intervention is £1.59.
Table 4 Intervention costs per participant (£ sterling) associated with each group
| Intervention group, £ per participant | Control group, £ per participant | |
|---|---|---|
| Opportunistic screening costs for 1794 screened | ||
| General lifestyle questionnaire | 0.80 | 0.80 |
| 5 minutes of practice nurse interpretation a | 17.50 | 17.50 |
| Minimal intervention brief advice | ||
| 5 minutes of practice nurse time b | 0.00 | 1.10 |
| Premises costs Reference Drummond, Oyefeso, Phillips, Cheeta, DeLuca and Perryman2 | 0.00 | 0.36 |
| Self-help booklet | 0.00 | 0.13 |
| Stepped care | ||
| Step 1: motivational interview | ||
| Training cost for practice nurses | 148.15 | 0.00 |
| 40-minute interview, including staff and premises cost c | 12.74 | 0.00 |
| Follow-up telephone call | 0.68 | 0.00 |
| Follow-up interview with practice nurse | 3.18 | 0.00 |
| Step 2: motivational enhancement therapy | ||
| Four 50-minute sessions with therapist, including premises | 75.67 | 0.00 |
| Therapist's administration time d | 12.61 | 0.00 |
| Practice nurse follow-up telephone call | 1.30 | 0.00 |
| Step 3: specialist alcohol services, specialist intervention Reference Netten, Rees and Harrison33 | 735.00 | 0.00 |
a. Includes salary, National Insurance, superannuation and 8% management cost. Reference Netten, Rees and Harrison33
b. Premise size of 8m2 at £0.54/m2/hour for 5 minutes. Reference Netten, Rees and Harrison33
c. Actual training cost £8000 divided by 54 participants.
d. 10 minutes per session.
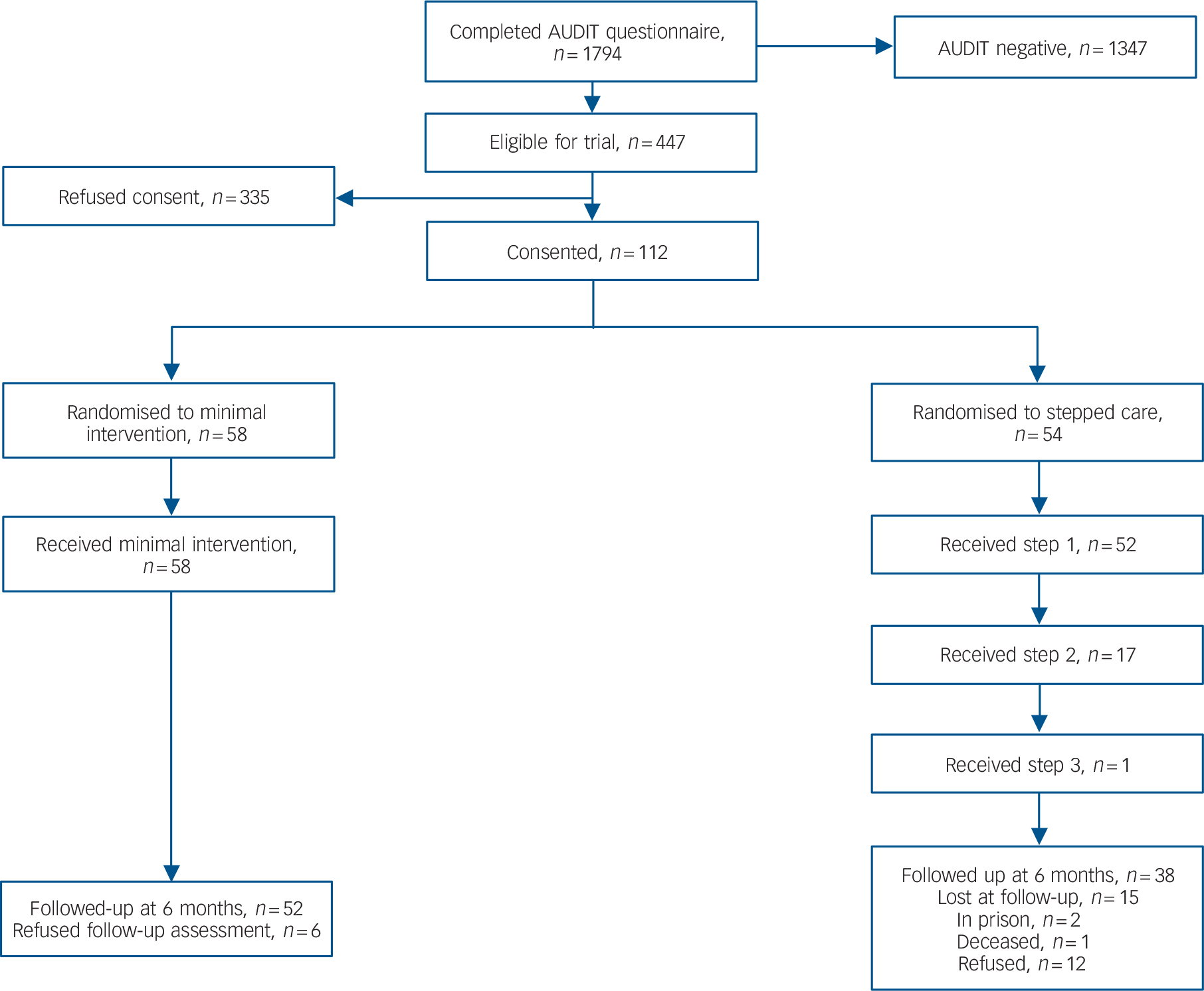
Fig. 1 CONSORT diagram for the study. AUDIT, Alcohol Use Disorders Identification Test.
In step 1 of the stepped care intervention participants received 40 minutes of motivational interviewing delivered by a practice nurse, at a cost of £12.74 including salary and premises costs. This was followed by a telephone call 2 weeks later, estimated to last 1.5 minutes at a cost of £0.68. A month after the motivational interview the practice nurse conducted an interview with the participant to assess their current alcohol consumption – this was estimated to take 10 minutes at a cost of £3.18 including staff and premises costs. The total cost of step 1 was estimated at £16.60 per participant.
Step 2 consisted of four 50-minute sessions of motivational enhancement therapy delivered by a trained alcohol counsellor. Sessions attended were costed using full salary costs, including overheads and a management cost of 8% of salary. The cost of the 8 m2 room was added together with a 10-minute administration time cost. Two weeks after step 2, a 5-minute telephone call was made to the participant at a cost of £1.30. Costs associated with extra telephone calls and letters were recorded and included in the analysis. For sessions where the participant failed to attend a scheduled session, a 5-minute cost was included on the basis that therapists use the time to engage in other tasks. Reference Coyle, Godfrey, Hardman and Raistrick34
Step 3 costs are associated with only one participant and no specific data were available on treatments received within the specialist agency: a standard cost of £735 is assumed. Reference Netten, Rees and Harrison33
In addition to treatment costs, 1794 participants were screened to identify 112 eligible and consenting participants. The cost of general lifestyle questionnaires and 5 minutes of practice nurse time to interpret the questionnaires is included for all 1794 screened participants divided by 112 consenting participants to arrive at a screening cost of £18.30 per participant. Further, in order to deliver motivational interviewing, practice nurses were trained and supervised at a total cost of £8000 divided by the 54 participants in the intervention group to arrive at a training cost of £148.15 per participant. It is possible that the training costs for stepped care are overestimated in that staff trained to deliver stepped care can continue to apply these skills after the trial is completed. However, as we have no way of knowing how far this would be applied after the trial was completed and all of the staff were redeployed to other posts after the end of the study, we have made a conservative estimate of the training costs in terms of cost-effectiveness.
Social costs for each group at baseline and 6 months are reported in Table 5 along with estimated treatment costs, including training, for patients with follow-up data only. The social costs include healthcare and social care costs, and costs associated with accidents. Crime costs are based on the estimated cost per offence, which includes an allowance for the victim's costs of crime. In the intervention group, mean total costs were £5692 at baseline and £2534 at follow-up, compared with £6851 and £12 637 in the control group. At 6 months, the intervention group had a mean 0.3849 QALYs compared with 0.3876 in the control group, a difference of 0.0027 (95% bootstrapped 95% CI −0.0535 to 0.0500). Patients in the control group gained 0.0074 QALYs between baseline and follow-up compared with a decrease of 0.0046 in the intervention group. A cost-effectiveness acceptability curve Reference Fenwick, Claxton and Sculpher40 was constructed, which indicated that stepped care had the greater probability of being the most cost-effective intervention, provided that the value of a QALY was less than £912 000. This result suggests that at an acceptable value of a QALY, between £20 000 to £30 000 in the UK, stepped care would be 98% likely to be the most cost-effective option.
Table 5 Mean (s.d.) costs in £ sterling for each group at baseline and 6-month follow-up (patients with follow-up data only)
| Intervention group (n = 51), mean (s.d.) | Control group (n = 39), mean (s.d.) | |||||
|---|---|---|---|---|---|---|
| Baseline | 6 months | Baseline | 6 months | |||
| Service utilisation | ||||||
| Healthcare | 295.48 (597.89) | 284.64 (771.94) | 383.26 (696.05) | 179.70 (316.13) | ||
| Social care | 46.51 (93.66) | 14.21 (45.68) | 38.42 (104.88) | 47.03 (136.30) | ||
| Criminal justice | 1725.67 (7284.72) | 0.0 (0) | 2478.78 (8837.58) | 8109.98 (32002.64) | ||
| Accidents | 3624.36 (6623.54) | 2009.49 (5203.22) | 3950.78 (8040.47) | 4280.39 (15705.63) | ||
| Treatment | 215.84 (113.08) | NA | 20.02 | NA | ||
NA, not applicable.
Discussion
Summary and relevance of findings
A total of 1794 male attendees at primary care practices were screened using the AUDIT questionnaire. Twenty-five per cent scored positive for hazardous or harmful alcohol consumption, an indication of the prevalence of alcohol use disorders in this population. We have demonstrated the high level of sensitivity and specificity of the AUDIT in this population. Reference Coulton, Drummond, James, Godfrey, Parrott and Peters41
Our study showed that it was feasible to implement a stepped care intervention in this population. Alcohol consumption reduced in both groups following intervention in this non-treatment-seeking population. Differences in terms of actual alcohol consumed were greater, but not significantly, in the intervention group, with an effect size difference in the order of 0.23 and 0.27 for mean daily and total alcohol consumed. These effect sizes are comparable with those found in meta-analyses of brief alcohol interventions. Reference Moyer, Finney, Swearingen and Vergun10 This will be helpful in designing a definitive trial of stepped care intervention and for meta-analysis. Secondary outcomes indicated a similar trend towards better outcomes for the intervention group but none of these was significantly different except for greater motivation to change, which is consistent with the motivational intervention approaches used in the intervention group. However, from this pilot study it is not possible to conclude with confidence that stepped care intervention is superior in terms of clinical effects to minimal intervention because of the possibility of type 2 error.
Other limitations of the study include the relatively small proportion of potential participants who actually gave consent to participate (25%). We also found those who agreed to participate were older and had higher AUDIT scores. This may indicate that those who took part were not truly representative of the population from which they were drawn. It may also be the case that these differences reflect not only differences in willingness to take part in research, but also a difference in willingness to receive alcohol interventions if offered. In common with other trials of brief alcohol interventions in primary care, we excluded patients with severe mental illness on the basis that their needs were unlikely to be met by the control intervention. In typical practice, brief interventions are not intended for this population except in the context of more comprehensive mental healthcare. The pragmatic nature of the study aimed to maximise the generalisability, and the proportion agreeing to take part is similar to that found in meta-analysis of primary care brief intervention studies. Reference Beich, Thorsen and Rollnick42 However, as we and others have pointed out, as a public health measure, questionnaire screening for alcohol use disorders in primary care is highly cost-effective, as the cost of administering the questionnaire is small and interventions are only offered to those screening positive. Reference Coulton, Drummond, James, Godfrey, Parrott and Peters41,Reference Saitz43 We will however be exploring the reasons for non-participation, including patient and therapist characteristics, in a subsequent study. Further, based on the experience of this study, our ongoing research includes a considerably reduced baseline research assessment process to maximise willingness to participate as this may have presented a barrier to participation. In line with current methodological research, no collateral measures to verify self-report were included, as collateral reports and blood investigations are not sufficiently reliable or valid compared with self-report obtained by the Time Line Follow-Back interview. Reference Babor, Steinberg, Anton and Del Boca44
Cost-effectiveness
The cost-effectiveness analysis indicated that the stepped care intervention costs ten times that of the minimal intervention (£216 v. £20) as expected. However, social costs in the control group are greater 6 months after randomisation than in the intervention group: the mean social cost per patient in the 6-month period preceding follow-up was £2308 in the intervention group and £12 617 in the control group. These costs are very variable and not statistically significantly different. The analysis of the bootstrapped cost-effectiveness ratios suggest that in 818 (81.8%) of the 1000 cases, stepped care is less costly and more effective, in 165 (16.5%) cases stepped care is less costly and more effective, in 14 (1.4%) cases stepped care is more costly and more effective, and in only 3 (0.3%) cases stepped care is more costly and less effective. The cost-effectiveness applicability curve shows that at accepted values for a QALY, decision makers could have confidence of approximately 98% that the stepped care approach would be more cost-effective than the minimal intervention approach. The net cost saving is almost £9000 ($15 000 USD) in stepped care compared with minimal intervention.
As a result of this study, a large-scale pragmatic randomised controlled trial of stepped care alcohol intervention in primary care has begun. Reference Coulton, Watson, Bland, Drummond, Kaner and Godfrey45 As stepped care is, in research terms, a complex intervention, future research will need to establish the key effective ingredients of stepped care, including the necessary duration, intensity and content of stepped care needed to deliver effective outcomes. This will require more complex trial design and process measurement.
Implementation
On a practical level we found that stepped care offered a new practical clinical approach to the treatment of alcohol use disorders encountered in everyday primary care and a positive inter-agency protocol shared between primary care and specialist alcohol treatment agencies. There is a clear need for the training of primary care staff to implement screening and deliver behaviour change counselling interventions, which include the need for follow-up and reviews of progress. We found that the only way we could implement either of the two interventions was to specifically recruit and train practice nurses rather than seek secondment from existing practice nurse posts. This was due to reported pressures on primary care staff in providing existing care, and was only possible to implement with additional funding to cover the full costs of the screening and interventions. So there are likely to be capacity, financial and workforce issues in implementing an alcohol-screening stepped care intervention in the National Health Service. Stepped care appears to offer a practical clinical methodology suitable for addressing the allocation of limited resources.
Funding
The study was funded by the Wales Office for Research and Development. All of the authors are independent of the funding body.
Acknowledgements
We would like to thank Colin Reeves, Carol Sturgess and Dr Lynn Jones, Swansea Mental Health NHS Trust, and all the staff at the following primary care practices: Sway Road Surgery, Morriston, Cwmfelin Medical Centre, Ty Elli Group Practice, Skewen Surgery, Gowerton Surgery, Manselton Surgery. Thanks are also due to Melanie Perry, William Chandler, William Webber, Lynda Jenkins of Prism, Carmarthen; Dr Roy Sherwood, King's College Hospital, London; Dr Roger Monroe, Morriston Hospital, Swansea; and the practice nurses Dianne Catterson, Mandy Clarke, Helen Davies, Phillip Jones, Alison Terry, June Wheel, and Lead Nurse Margaret Blewitt.









eLetters
No eLetters have been published for this article.