Anxiety disorders and depression are among the most common mental disorders worldwide. Reference Pedersen, Mors, Bertelsen, Waltoft, Agerbo and McGrath1 Together they account for over 50% of the global disease burden in terms of disability-adjusted life years attributable to mental health disorders and substance use. Reference Whiteford, Degenhardt, Rehm, Baxter, Ferrari and Erskine2 The association between depression and mortality is now well established, Reference Chang, Lin, Lee, Lin and Pfeiffer3–Reference Wulsin, Vaillant and Wells11 particularly higher rates of suicide have been reported among people diagnosed with depression, Reference Chang, Lin, Lee, Lin and Pfeiffer3,Reference Osby, Brandt, Correia, Ekbom and Sparen12 but the excess mortality risk extends to natural causes. Reference Cuijpers, Vogelzangs, Twisk, Kleiboer, Li and Penninx13 In contrast, data on mortality risk in people with anxiety disorders are conflicting, providing more equivocal results of an absent, Reference Holwerda, Schoevers, Dekker, Deeg, Jonker and Beekman10,Reference Markkula, Härkänen, Perälä, Partti, Peña and Koskinen14 favourable, Reference Mykletun, Bjerkeset, Dewey, Prince, Overland and Stewart5,Reference Lee, Wadsworth and Hotopf15 unfavourable Reference Denollet, Maas, Knottnerus, Keyzer and Pop16–Reference Laan, Termorshuizen, Smeets, Boks, De Wit and Geerlings18 or even U shape relationship. Reference Mykletun, Bjerkeset, Øverland, Prince, Dewey and Stewart6 These conflicting data might be because of the heterogeneity in sample size, gender, anxiety subtypes, somatic comorbidities Reference Batterham, Christensen and Mackinnon8,Reference Wulsin, Vaillant and Wells11 and causes of death studied. Further, only a few studies have assessed mortality risk among patients with different specific anxiety disorders. Reference Markkula, Härkänen, Perälä, Partti, Peña and Koskinen14,Reference Carrière, Ryan, Norton, Scali, Stewart and Ritchie17 Large prospective studies taking into account such factors are thus still missing in this area. In order to gain better insight in the mortality risk among patients with (specific) anxiety disorders we conducted a detailed population-based study using nationwide Danish register data.
We comprehensively assessed mortality rates across varying causes of death among people diagnosed with anxiety disorders. Given the clinical heterogeneity of anxiety diagnoses, we calculated mortality rates across the spectrum of specific anxiety disorders. As anxiety disorders are highly comorbid with depression Reference Pedersen, Mors, Bertelsen, Waltoft, Agerbo and McGrath1 , we were specifically interested in independent and synergistic effects of these disorders on mortality risk. We therefore assessed whether mortality rates were elevated in individuals with anxiety disorders independent of comorbid depression and whether patients with both diagnoses were at an especially enhanced risk of dying. As a last step we assessed potential mediating effects of somatic comorbidity and substance misuse on mortality risks. A better understanding of excess mortality – and its causes – among patients with anxiety disorders could help to prevent these deaths.
Method
Study setting
We conducted a nationwide follow-up study. The main exposure variables were defined as a first psychiatric in-patient or outpatient contact for anxiety disorders. The outcome variable was defined as death by any natural cause (diseases and medical conditions) or unnatural cause (suicide, accidents and homicide) within the follow-up period. Data were collected on the cohort of people born in Denmark between 1 January 1955 and 31 November 2006. The follow-up time started on their first birthday or 1 January 2002, whichever came later, in order to ensure complete information on cohort members. Follow-up ended at date of emigration from Denmark, date of death or 31 December 2011, whichever came first. This provided a maximum follow-up period of 10 years and a maximum age of 57 for the cohort members. We focused on deaths among younger age groups of the population in order to reduce probable biases because of selective survival. Data on cohort members were collected through linkage of four Danish population registers (see online supplement DS1). All residents of Denmark, including immigrants, have a unique personal identification (CRS) number that is used in all national registers, which enables data to be linked across these registers. The study was approved by the Danish Data Protection Agency. All personal information from the registers is anonymised when used for research purposes, and by Danish law, informed consent is not needed for register-based studies.
Exposure variables
The main exposure variables were defined as treatment for anxiety disorder. Using the Danish Psychiatric Central Register Reference Mors, Perto and Mortensen19 and the Danish National Patient Register Reference Andersen, Madsen, Jorgensen, Mellemkjoer and Olsen20 we identified all patients diagnosed with anxiety disorders (ICD-10: F40.00–F40.20, F41.00–F41.10, F42.00–F43.10). 21 Date of onset was defined as the day of the first contact for the diagnosis in question.
Outcome variables
The outcome of interest was time to death. The date and cause of death were identified from the Danish Register of Causes of Death. Reference Helweg-Larsen22 All-cause mortality was defined as ICD-10 codes A00–Y98 and categorised into the following groups: deaths from diseases and medical conditions (natural death) ICD 10: A00–R99, and deaths from external causes (unnatural death) ICD-10: V01–Y98. Unnatural causes of death comprised suicides (ICD-10: X60–X84, Y10-Y34), homicides (ICD-10: X85–Y09, Y87.1) and accidents (ICD-10: V01–X59, Y10–Y86, Y87.2). Natural causes comprised death by cancer (ICD-10: C00–D48), cardiac diseases (ICD-10: I00–I99), respiratory diseases (ICD-10: J00–J99), digestive conditions (ICD-10: K00–K93) and remaining causes.
Covariates
Information on age, gender, calendar period, maternal and paternal age at time of birth, and place of residence was obtained from the Danish Civil Registration System. Reference Pedersen23 Somatic comorbidities were assessed using the Charlson Comorbidity Index (CCI), which is based on 19 severe chronic diseases weighted from one to six corresponding to the severity of the disease. Reference Charlson, Pompei, Ales and Mackenzie24 Information on substance misuse (ICD-8 25 code 291.xx, 303.xx, 304.xx, 571.09, 571.1x and ICD-10 code F10–F16, F18, F19, I85, K70) and depression (ICD-8 code: 296.x9, 298.09, 298.19, 300.49, 301.19; ICD-10 code: F32.00–F33.99, F34.10–F34.90, F38.00–F39.99) was retrieved from the Danish Psychiatric Central Register Reference Mors, Perto and Mortensen19 and the Danish National Patient Register. Reference Andersen, Madsen, Jorgensen, Mellemkjoer and Olsen20
Sibling control studies
To account for possible familial confounding, we performed additional analyses that used unaffected full siblings of patients as controls. In this analysis, we identified as cases those individuals with anxiety disorders who also had full siblings without anxiety disorders, and these individuals were compared with their unaffected full siblings using matched conditional Cox regression.
Data analyses
Mortality rate ratios (MRRs) were calculated for natural and unnatural causes of death as well as all causes. We fitted three statistical models to these outcomes, using the log-linear Poisson regression with the GENMOD procedure in SAS, version 9.3. In the first model we adjusted for demographic characteristics, in the second model somatic comorbidity, which was defined as a CCI of 0, 1, 2, 3 or more, and in the third model effects were adjusted for depression. Of special interest was an evaluation of whether the MRRs varied between lifetime diagnoses of anxiety disorders only, depression only or both disorders by testing for statistical interaction. As anxiety disorders and depression are also frequently comorbid with substance misuse, Reference Kessler, Berglund, Demler, Jin, Koretz and Merikangas26 we additionally adjusted results for comorbid substance misuse. Finally, we studied potential mediating effects of somatic comorbidity and substance misuse on mortality risk. In our sensitivity analyses, we assessed differences in the psychiatry–mortality associations by gender and time since diagnosis. A more detailed description can be found in online supplement DS1.
Results
From 1 January 2002 to 31 December 2011 a total of 3 270 650 people were included in the study cohort contributing 31 213 252 person-years at risk. In 51 373 (1.6%) cohort, members follow-up ended before the end of the study; 50 521 emigrated from Denmark and 852 were lost to follow-up. The mean follow-up time for the cohort members was 9.7 years. In total, 27 236 individuals in our cohort died during the follow-up period, corresponding to a mortality rate of 8.7 per 10 000 person-years. Within this cohort we identified 50 683 with anxiety disorders and 76 202 with depression (69 227 (61.6%) girls and women and 43 211 (38.4%) boys and men). Individuals diagnosed with anxiety disorders contributed a total of 293 866 person-years of observation. Among people diagnosed with anxiety disorders, 14 447 (28.5%) had a comorbid diagnosis of depression. A total of 1066 people with anxiety disorders (2.1%) died during the follow-up period, including 410 (2.8%) individuals with comorbid anxiety disorders and depression (Table DS1).
All-cause mortality rates in people with anxiety disorders
The fully adjusted all-cause MRR for individuals diagnosed with anxiety disorders was 1.66 (95% CI 1.56–1.77) compared with people from the background population without these diagnoses (reference group, Table 1). Although diagnoses of anxiety disorders were consistently associated with higher mortality rates, MRRs varied by time since first diagnosis (Table DS2). Interaction between gender and anxiety disorders seemed clinically relevant, but did not reach statistical significance for anxiety disorders (P = 0.08, Table DS3). The MRRs were significantly elevated among individuals with anxiety disorders independent of comorbid somatic disorders (Table DS4). Allcause MRRs for people diagnosed with anxiety disorders were slightly attenuated by taking comorbid substance misuse into account (1.24, 95% CI 1.16–1.32, Table DS5). We observed a significant dose–response relationship between the number of different anxiety disorders and mortality risk, especially in individuals with more than two anxiety disorders, who were at increased risk (Table 2).
Table 1 Mortality rate ratios of people with anxiety disorders (2002–2011)
| Mortality rate ratio (95% CI) | ||||
|---|---|---|---|---|
| First adjustment a | Second adjustment b | Third adjustment c | Fourth adjustment d | |
| All causes | 3.71 (3.49–3.94) | 3.74 (3.29–4.24) | 2.16 (2.03–2.30) | 1.66 (1.56–1.77) |
| Unnatural causes | 6.47 (5.86–7.14) | 6.85 (5.74–8.60) | 4.63 (4.17–5.13) | 2.46 (2.20–2.73) |
| Natural causes | 2.89 (2.67–3.13) | 2.77 (2.37–3.24) | 1.58 (1.46–1.71) | 1.39 (1.28–1.51) |
a. Mortality rate ratios derived from comparison with population controls adjusted for calendar year, age, gender and the interaction of age with gender.
b. Mortality rate ratios derived from comparison with sibling controls adjusted for calendar year, age, gender and the interaction of age with gender.
c. Mortality rate ratios derived from comparison with population controls adjusted for calendar year, age, maternal and paternal age, gender, place of residence at time of birth, somatic comorbidity and the interaction of age with gender.
d. Mortality rate ratios derived from comparison with population controls adjusted for calendar year, age, maternal and paternal age, gender, place of residence at time of birth, somatic comorbidity, depression and the interaction of age with gender.
Table 2 Mortality rate ratios of people with specific anxiety disorders and number of diagnoses (2002–2011)

| Mortality rate ratio (95% CI) | |||
|---|---|---|---|
| All causes | Unnatural causes | Natural causes | |
| Anxiety diagnosis a | |||
| Acute stress reaction | 1.69 (1.52–1.88) | 2.94 (2.49–3.46) | 1.30 (1.12–1.49) |
| Agoraphobia | 1.31 (1.03–1.64) | 1.55 (1.00–2.28) | 1.24 (0.92–1.62) |
| Generalised anxiety disorder | 1.62 (1.35–1.93) | 2.55 (2.00–3.19) | 1.64 (1.36–1.95) |
| Panic disorder | 1.31 (1.11–1.54) | 1.83 (1.45–2.28) | 1.32 (1.12–1.55) |
| Post-traumatic stress disorder | 1.58 (1.31–1.87) | 2.70 (2.06–3.46) | 1.17 (0.90–1.48) |
| Social phobia | 1.50 (1.20–1.84) | 2.19 (1.70–2.77) | 1.51 (1.21–1.85) |
| Specific phobia | 1.50 (1.09–1.99) | 1.76 (0.94–2.96) | 1.40 (0.96–1.95) |
| Number of anxiety disorders b | |||
| 1 anxiety disorder | 2.09 (1.95–2.23) | 4.34 (3.88–4.85) | 1.56 (1.43–1.70) |
| 2 anxiety disorders | 2.46 (2.06–2.91) | 6.50 (4.93–8.39) | 1.65 (1.30–2.06) |
| >2 anxiety disorders | 3.27 (2.33–4.42) | 8.85 (5.18–13.69) | 2.18 (1.39–3.22) |
a. Mortality rate ratios were adjusted for calendar year, age, maternal and paternal age, gender, place of residence at time of birth, somatic comorbidity, depression and the interaction of age with gender.
b. Mortality rate ratios were adjusted for calendar year, age, maternal and paternal age, gender, place of residence at time of birth, somatic comorbidity and the interaction of age with gender.
Causes of death in people with anxiety disorders
In total, 1066 individuals diagnosed with anxiety disorders died during the follow-up period; 641 (60.1%) died from natural causes and 425 (39.9%) from unnatural causes. Among people diagnosed with anxiety disorders, the fully adjusted MRR was 1.39 (95% CI 1.28–1.51) for natural causes of death and 2.46 (95% CI 2.20–2.73) for unnatural causes of death, compared with individuals without anxiety disorders (Table 1). The MRRs for natural and unnatural causes of death did not differ between men and women (Table DS3) diagnosed with anxiety disorders. The MRRs for natural and unnatural causes of death were significantly elevated among people with anxiety disorders independent of comorbid somatic disorders (Table DS4). After taking comorbid substance misuse into account, only MRRs for unnatural causes of death were significantly elevated among individuals with anxiety disorders, whereas MRRs for natural causes fell short of significance (MRR = 1.07, 95% CI 0.98–1.16, Table DS5). The analyses exploring the effect of specific anxiety disorders did not indicate that just one specific type of anxiety disorder was driving all associations (Table 2). All specific anxiety disorders were associated with higher overall mortality rates. The risk for natural death was increased among patients with acute stress reaction, generalised anxiety disorder, panic disorder and social phobia. Specific phobia was the only anxiety disorder that did not increase the risk of dying by unnatural causes; the risk for unnatural death was more than doubled in patients with acute stress reaction, generalised anxiety disorders, post-traumatic stress disorder and social phobia. We further observed a significant dose–response relationship between the number of comorbid anxiety disorders and unnatural causes of death; this effect was less prominent for natural causes of death (Table 2).
With the exception of cancer (anxiety disorders MRR = 0.88, 95% CI 0.73–1.03), MRRs for all specific causes of death were significantly elevated among individuals with anxiety disorders compared with the general population. The cause-specific MRRs were highest for accidents (MRR = 2.60, 95% CI 2.24–3.01) among people with anxiety disorders; to enable comparability we added results for depression (Table 3). In addition, we compared patients with anxiety disorder with their unaffected siblings for all-cause mortality, natural causes and unnatural causes. All risk estimates remained raised (Table 1). We found no evidence of familial confounding for causes of death (since risk estimates were significant and of the same magnitude as for the population controls).
Table 3 Mortality rate ratios of people with anxiety disorders and/or depression stratified by causes of death (2002–2011) a
| Causes of death | Depression | Anxiety disorders |
|---|---|---|
| Unnatural causes | ||
| Suicide | 11.36 (10.25–12.52) | 2.44 (2.11–2.80) |
| Accident | 4.02 (3.57–4.51) | 2.60 (2.24–3.01) |
| Homicide | 2.57 (1.30–4.62) | 2.34 (1.02–4.67) |
| Natural causes | ||
| Respiratory disease | 2.07 (1.51–2.77) | 1.31 (0.82–1.99) |
| Cancer | 0.82 (0.72–0.92) | 0.88 (0.73–1.03) |
| Digestive condition | 1.71 (1.45–2.00) | 2.00 (1.63–2.44) |
| Cardiac disease | 1.75 (1.49–2.06) | 1.50 (1.20–1.86) |
| Other disease | 1.59 (1.50–1.69) | 1.39 (1.28–1.51) |
a. Mortality rate ratios were derived from multivariate analysis and adjusted for calendar year, age, maternal and paternal age, gender, place of residence at time of birth, somatic comorbidity and the interaction of age with gender.
Influence of comorbid anxiety disorders
The MRRs of people diagnosed with comorbid anxiety disorders and depression (MRR = 3.02, 95% CI 2.73–3.32) were higher than the MRRs of those diagnosed with anxiety disorders alone (MRR = 2.10, 95% CI 1.94–2.27) or depression alone (MRR = 2.57, 95% CI 2.45–2.70) (Fig. 1(a)). Individuals diagnosed with comorbid anxiety disorders and depression (MRR = 11.72, 95% CI 10.11–13.51) had higher MRRs for unnatural causes of death than those diagnosed with anxiety disorders alone (MRR = 4.25, 95% CI 3.70–4.85) or depression alone (MRR = 7.87, 95% CI 7.26–8.53) (Fig. 1(b)). No such effects were observed for natural causes of death (Fig. 1(c)). The MRRs for deaths caused by accidents were especially increased among people with comorbid anxiety disorders and depression (MRR = 8.02, 95% CI 6.47–9.81) compared with people with only one disorder (anxiety disorder MRR = 3.28, 95% CI 2.71–3.92; depression MRR = 4.38, 95% CI 3.86–4.95, Fig. 1(d)). The MRRs for suicides were further strikingly high among individuals diagnosed with comorbid anxiety disorders and depression (MRR = 18.32, 95% CI 15.21–21.86), and higher than among people with a single disorder (anxiety disorder MRR = 5.69, 95% CI 4.70–6.86; depression MRR = 13.41, 95% CI 12.10–14.84, Fig. 1(e)). The MRRs for unnatural causes and all-cause mortality were higher among people without comorbid somatic disorders and without comorbid substance misuse (Tables DS6 and DS7).
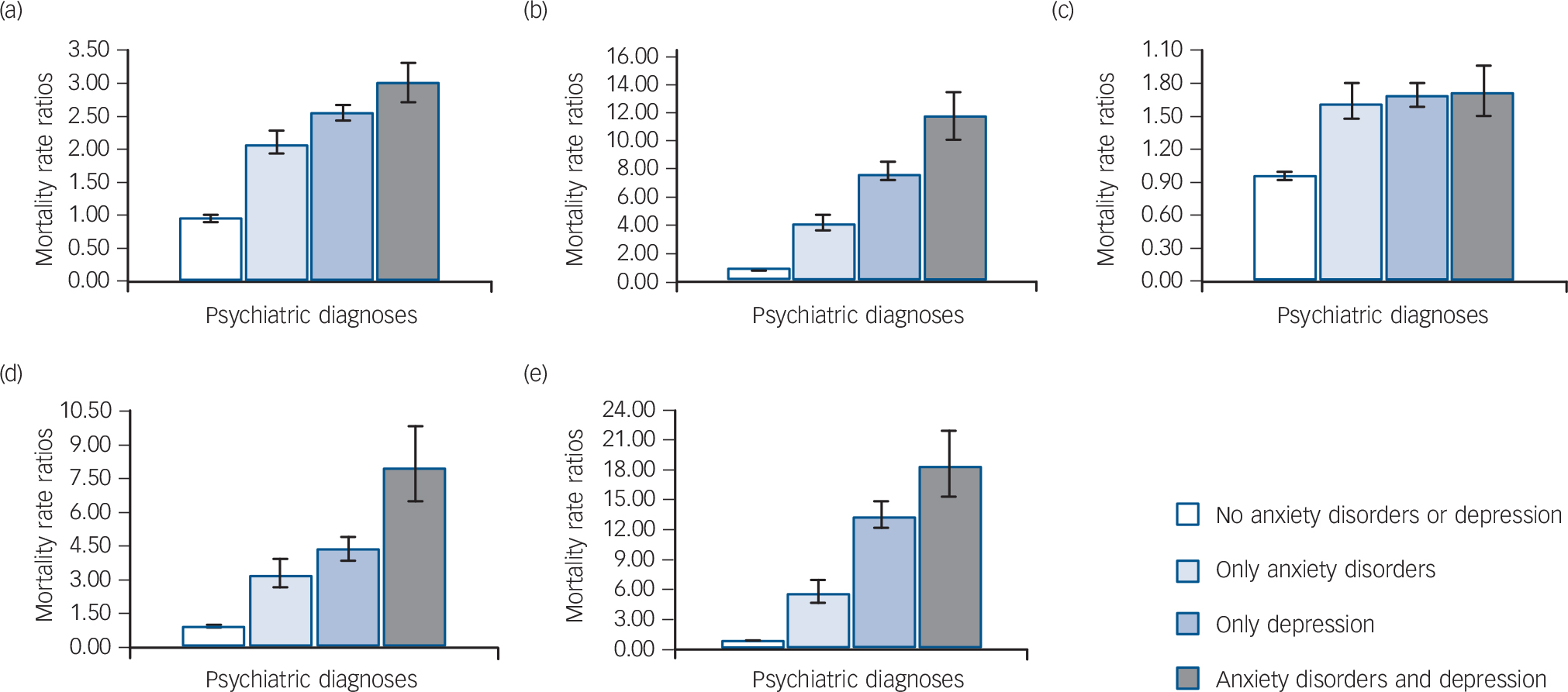
Fig. 1 Influence of comorbid anxiety disorders on mortality in people with and without depression (2002–2011).
(a) All causes, (b) unnatural causes, (c) natural causes, (d) accidents and (e) suicides. Mortality rate ratios were derived from multivariate analysis and adjusted for calendar year, age, maternal and paternal age, gender, place of residence at time of birth, somatic comorbidity and the interaction of age with gender. Error bars reflect 95% confidence intervals.
Discussion
In this nationwide prospective cohort study, we explored independent and synergistic effects of anxiety disorders and depression on various causes of mortality, carefully evaluating potential moderating effects. We report three main findings. First, the adjusted odds of all-cause mortality, which followed people diagnosed with anxiety disorders until they were 57 years old, were 1.7 compared with the general population. Around 40% of all deaths in people with anxiety disorders were from unnatural causes. Second, we found evidence that anxiety disorders constitute a significant risk factor for premature mortality independent of comorbid depression. In addition, sibling-control analyses revealed no familial confounding for causes of death. With the exception of suicides, the MRRs for varying causes of death were comparable for individuals diagnosed with anxiety disorders and those diagnosed with depression. Finally, we observed a significantly enhanced risk for all-cause mortality and unnatural causes of death in people diagnosed with comorbid anxiety disorders and depression compared with those with a single disorder. We hypothesised that these findings could be explained by anxious depression being a more severe form of psychiatric disorder, which might have important implications for clinical practice by underlining the need for treatment of both anxiety disorders and depression.
The MRRs for varying causes of deaths were significantly elevated among people with anxiety disorders while controlling for comorbid depression. To account for the heterogeneity of anxiety disorders, we individually assessed the impact of seven specific anxiety disorders on mortality risk. The mortality risks for specific anxiety disorders were overall rather similar, indicating that not just one specific type of anxiety disorder was driving all associations. Several specific anxiety disorders were observed to increase the risk of natural and unnatural causes of death. Acute stress reaction, generalised anxiety disorder, post-traumatic stress disorder and social phobia more than doubled the risk of dying from an unnatural cause of death. Previous studies reported several specific anxiety disorders to be associated with all-cause mortality Reference Carrière, Ryan, Norton, Scali, Stewart and Ritchie17 as well as suicidal ideation and suicide attempts, Reference Sareen, Cox, Afifi, de Graaf, Asmundson and ten Have27,Reference Nock, Hwang, Sampson, Kessler, Angermeyer and Beautrais28 but other causes of death have not been studied so far. In addition, we observed a higher mortality risk among individuals diagnosed with multiple anxiety disorders.
Among people with anxiety disorders, the highest MRRs were observed for deaths from unnatural causes (i.e. accidents, homicide and suicide). This pattern of high mortality from unnatural causes among people diagnosed with anxiety disorders has been previously observed. Reference Sareen, Cox, Afifi, de Graaf, Asmundson and ten Have27,Reference Crump, Sundquist, Winkleby and Sundquist29–Reference Bohnert, Ilgen, Ignacio, Mccarthy, Valenstein and Blow31 However, in this study we were able show for the first time that the increased mortality from unnatural causes in people with anxiety disorders could not be fully explained by comorbid depression. Similarly, Laan et al observed that the risk for suicides was enhanced among individuals with anxiety disorders but lower than in people with depression. Reference Laan, Termorshuizen, Smeets, Boks, De Wit and Geerlings18 Comorbidity strongly affected the suicide risk in anxiety disorders; individuals with comorbid anxiety disorders and depression were at significantly higher risk of dying by suicide than those with a single type of disorder. The risk of suicide among psychiatric patients has been studied extensively, whereas less attention has been given to the risk and prevention of accidental death, even though the latter is more common. Here, we observed the highest MRRs in people with anxiety disorders for death by accidents, most notably among those with a double diagnosis of anxiety disorders and depression. In addition, we found an increased risk of homicide among people diagnosed with anxiety disorders.
In absolute numbers, most persons diagnosed with anxiety disorders died from natural causes. Thus, the escalation of deaths from diseases and medical conditions in people with anxiety disorders is an important component of the observed excess mortality. Interestingly, comorbid depression did not result in an excess death risk from natural causes in individuals with anxiety disorders, despite the fact that most people with depression died from natural causes. Only a few mortality studies have examined gender-specific effects of anxiety disorders, providing conflicting results. Reference Carrière, Ryan, Norton, Scali, Stewart and Ritchie17,Reference Van Hout, Beekman, De Beurs, Comijs, Van Marwijk and De Haan32 In our study we found that in individuals with anxiety disorders no gender-specific effects on mortality risk could be observed.
Severe psychiatric disorders have been shown to be associated with an increased risk of somatic comorbidity Reference Campayo, De Jonge, Roy, Saz, de la Cámara and Quintanilla33,Reference Surtees, Wainwright, Luben, Wareham, Bingham and Khaw34 and psychiatric patients might be underdiagnosed and undertreated for medical conditions. Reference Laursen, Munk-Olsen, Agerbo, Gasse and Mortensen35 In addition, substance misuse is more common in anxiety disorders and depression, as depressed and anxious individuals may turn to drugs or alcohol as a form of self-medication. Reference Fergusson, Boden and Horwood36,Reference Robinson, Sareen, Cox and Bolton37 In this study we could confirm mediating effects of somatic comorbidities and substance misuse on the mortality risk in people with anxiety disorders. However, in individuals with anxiety disorders mediating effects were nearly absent for unnatural causes of death. Other hazardous health styles such as physical inactivity, Reference Whooley, De Jonge and Vittinghoff38,Reference De Wit, Fokkema, Van Straten, Lamers, Cuijpers and Penninx39 increased smoking rates, Reference Dierker, Avenevoli, Stolar and Merikangas40,Reference Moylan, Jacka, Pasco and Berk41 unhealthy eating patterns Reference Holahan, Moos, Holahan, Cronkite and Randall42–Reference Mason, Flint, Roberts, Agnew-Blais, Koenen and Rich-Edwards46 and lack of treatment seeking, Reference Lack, Holt and Baldwin47 as well as stress and biological dysregulation, Reference Vogelzangs, Beekman, De Jonge and Penninx48–Reference Wium-Andersen, Orsted, Nielsen and Nordestgaard50 might have further contributed to the observed excess mortality in people with anxiety disorders.
Strengths and limitations
We studied a nationwide population-based cohort that included all individuals born in Denmark between 1955 and 2006, with almost complete follow-up data for up to 57 years. Thus, our findings are unlikely to be explained by biases in selection of the study population or non-differentiated attrition during follow-up. There are, however, two main limitations in this study. First, we used patient registers to identify individuals diagnosed with anxiety disorders, since it was necessary to use routinely collected data to provide precision for the fairly rare outcomes investigated. Register-based diagnoses are clinical diagnoses and not the result of systematic, well-described uniform assessments. Despite a generally acceptable accuracy of anxiety disorder diagnoses in the registers, Reference Meier, Petersen, Mattheisen, Mors, Mortensen and Laursen51 individuals with milder forms of anxiety disorders are less likely to present to secondary services and therefore might be underrepresented in our study. Thus, our findings might not be representative of the entire spectrum of anxiety disorders. We carefully adjusted for factors that might affect treatment seeking among people diagnosed with anxiety disorders, such as somatic and mental comorbidity. However, significant predictors of clinical outcome such as symptom severity or acceptance of the disorder might still differ between patients with or without treatment. Second, some of the causes of death may be prone to misclassification. Whereas most deaths classified as suicides reflect true suicides, it is possible that some deaths classified as accidental are in fact suicides.
Implications
This study further underlines that anxiety disorders constitute a major clinical and public health problem. Anxiety disorders were associated with a significantly increased mortality risk, and the co-occurrence of these disorders resulted in an additionally increased death risk. Because of the high prevalence of anxiety disorders, the associated excess mortality has an immense impact on public health. A recent meta-analysis indicated that approximately five million deaths worldwide are attributable to mood and anxiety disorders each year. Reference Walker, McGee and Druss52 For clinicians, it is also important to realise that anxiety disorders and depression are associated with increased mortality from both natural and unnatural causes, and that the assessment of physical health in these patients is always important.
Funding
This study was supported by the Lundbeck Foundation, within the context of the Lundbeck Foundation Initiative for Integrative Psychiatric Research, iPSYCH, and Mental Health in Primary Care (MEPRICA). S.M.M. received further funding from the Mental Health Services, Capital Region, Copenhagen, Denmark, and M.M. from the Stanley Medical Research Institute.







eLetters
No eLetters have been published for this article.