P-09-01
Comorbid disorders in the potential initial prodrome of psychosis and in first-episode schizophrenia
S. Ruhrmann, F. Schultze-Lutter, J. Klosterkӧtter, I. Becker. Depart, of Psychiatry & Psycho, Cologne, Germany
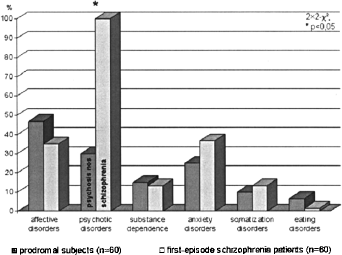
Objective: Comorbid disorders in and before the first episode of schizophrenia were frequently found. Thus, they should also be present in comparable frequency and type in persons with an assumed initial prodrome of psychosis.
Methods: 60 ‘prodromal’ subjects and 60 first-episode schizophrenia patients were examined with the German version of the Structured Clinical Interview for DSM-IV Axis I disorders (SKID I) and compared for past and present psychiatric disorders.
Results: 57% of the schizophrenic and 68% of prodromal subject reported any past or present non-psychotic disorder. No group differences in present or past diagnoses were found for affective, anxiety, somatization and eating disorders and substance abuse, yet social phobia was significantly more present in the schizophrenic group (32 vs. 8%).
Conclusion: Comorbid disorders can indeed be found as frequently among potentially prodromal subjects as among first- episode schizophrenia patients. This finding underlines the need for treatment in this high-risk group as well as the necessity to consider their risk for psychosis when treating the comorbid condition.
Past and present axis I disorders in potentially prodromal and first-episode schizophrenia subjects:
P-09-02
A new instrument for the prediction of schizophrenia
H. Picker, F. Schultze-Lutter, S. Ruhrmann, A. Wieneke, E.-M. Steinmeyer, J. Klosterkӧtter. University of Cologne FETZ, Dept, of Psychiatry, Cologne, Germany
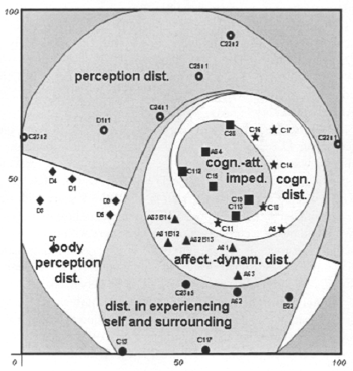
Objective: The prospective Cologne Early Recognition (CER) study demonstrated the predictive value of cognitive-perceptive basic symptoms for first-episode schizophrenia as assessed for their presence/absence with the Bonn Scale for the Assessment of Basic Symptoms. Based on these findings, a new scale was developed, the Schizophrenia Prediction Instrument, Adult version (SPI-A), which not only allows a more economic assessment, but also a severity rating.
Methods: Applying cluster and facet analyses to the CER-data and data of 346 remitted schizophrenia patients, the 40-item scale with 6 dimensions was derived and a seven-stage severity rating introduced. It was evaluated prospectively on potentially prodromal individuals in a 2-years follow-up and cross-sectionally in comparison to first-episode schizophrenia and non-psychotic mood-disordered patients.
Results: The construct validity could broadly be confirmed by FSSA with separation indices between 1.0 for the prodromal and 0.5 for the affective group. Comparison of baseline data of the three groups and of transited and not-transited “prodromal” patients again confirmed the importance of self-experienced cognitive disturbances in predicting psychosis. Furthermore, results from longitudinal analyses will be presented.
Conclusion: The SPI-A appears to be a useful instrument to evaluate the risk for psychosis in an early state when attenuated and transient psychotic symptoms might not (yet) be present.
Construct validation of SPI-A dimensions. Axional result of confirmatory Faceted Smallest Space Analysis (FSSA) of prodromal group.:
P-09-03
Premorbid characteristics of first-admitted patients with schizophrenia in Poland
K. Goma, K. Goma, K. Jaracz, F. Rybakowski, J. Rybakowski. Poznan, Poland
Objective: The aim of the study was to describe demographic and preclinical variables in patients with first-episode schizophrenia in Poland.
Methods: The study included 86 (34 female, 52 male) subjects hospitalized with the first episode of psychosis. Semi-structured interviews from patients and caregivers were used. Level of functioning in 1 year before hospitalization was established with Global Assessment Scale (GAS). Statistics were calculated with SPSS software.
Results: At first admission mean age of patients was 25.5 yrs. (SD 5.8), and 62.8% of patients were before 22 years. Females were significantly (2.8 years) older than male patients (t=2.26, p<0.05). Seventy-two percent of patients were active at first admission (job, education, housework, child rearing). Psychiatric disorders were present in 30.2% of first-degree relatives of patients. The mean GAS score 1 year before admission was 44.5 (SD 15.1) and in 59% of patients GAS score was below 50. Age at onset of first disturbances of functioning was 21 years (SD 5.7) (range 9-45 yrs), and the mean period from the first symptoms to hospitalization was 2.8 years (SD 3.7). Mean duration of psychotic symptoms until hospitalization was 38.0 weeks (SD 51.0) and mean period of untreated psychosis (DUP) was 26.2 weeks (SD 51.7).
Conclusion: Premorbid characteristics of patients with schizophrenia ie. DUP are comparable to results obtained in other populations. Because shorter duration of untreated psychosis might be associated with better outcome, these results may suggest the need for more active intervention in both individual and public health levels in psychotic disorders.
P-09-04
Psychopathological symptoms as determinants of quality of life and social functioning in a first episode of schizophrenia
K. Goma. Poznan, Poland
Objective: To evaluate patients’ quality of life (QOL) and social functioning (SF) associated with illness characteristics in schizophrenia.
Methods: Eighty six patients, age range 17-47 were assessed 1 and 13 months after a first hospitalization (respectively T1 and T2). Psychopathological symptoms were examined with PANSS based on 5-factor model of schizophrenia symptoms: positive, negative, agitation, cognitive and depression/anxiety. QOL and SF were assessed using WHOQOL and Social Functioning Scale (SFS) respectively. WHOQOL BREF contains 4 domains: Physical (Ph), Psychological (Ps), Social (S) and Environmental (E). Social Functioning Scale (SFS) is a 79-item in-strument comprising 7 areas.
Results: In T1 and T2 mean PANSS score did not show significant differences. In both assessments SFS global score was highly negatively correlated with PANSS. In T1 SFS score was predicted with 2 of 5 schizophrenia dimensions. Thirty nine percent of variance was explained with negative symptoms and 1% with positive symptoms. In T2 follow-up only negative symptoms explained 36% of variance in SFS score. In Tl, main predictors of WHOQOL were anxiety/depression, positive symptoms and negative symptoms. They explained from 27 to 38% of the variance in the examined domains. In T2, the main predictors of WHOQOL were negative symptoms and anxiety/depression, explaining 14 to 39% of the variance in the domains.
Conclusion: SF were predominantly dependent on the level of negative symptoms either shortly after the hospitalization and in 1 year follow-up. QOL however was dependent mainly on anxiety/ depression one month after the hospitalization and on negative symptoms in 1 year follow-up.
P-09-05
Early schizophrenia prevention help center in Ukraine
I. Martsenkovsky, L. Butenko, Y. Bikshaeva. Institute of Social Psychiatry Child Psychiatry, Kiev, Ukraine
Objective: As a study purposes were identified early revealing, early intervention, social rehabilitation, recovering maintenance and preventive strategies effectiveness exploration by adolescents with psychoses arising till 18 years on the basic of Kyiv center “Friendly clinic”, that was organized in 1992 specially for this aims realization. Program-target approaches service assumed: 1) hospitalization refusal; 2) early long-term atypical antipsychotic therapy; 3) objective risks groups preventive therapy; 4) suffered adolescent supporting and retention at school and micro-social referent group; 5) adolescent and family members psychoeducation; 6) compliance-therapy; 7) stress-management; 8) social-emotional skills training.
Methods: 120 adolescents 11 till 18 with family members were included into the program. Therapy results were compared with traditional therapy indices. Clinical effectiveness (PANSS), cognitive functioning (CANTAB, COGTEST), social functioning (SAFE), life quality (ILK) were measured.
Results: Cognitive infringements expressiveness by COGTEST at adolescents’ schizophrenia patients in the greater degree correlates with a social functioning level by SAFE, than negative infringements expressiveness by PANSS. At atypical antipsychotic therapy correlation degree between social functioning level by SAFE and cognitive infringements expressiveness by CANTAB and COGTEST with negative infringements expressiveness by PANSS do not depend on disease duration and psychotic episodes number in anamnesis.
Conclusion: Such approaches allow to achieve in 94% cases integration into micro- and macrosocial society levels, less stigmatization and disorder relapses level, expressed high enough school adaptation parameters, that are comparable with health pupils control group and significantly better than for traditionally treated patients.
P-09-06
The Basel FEPSY Study: Sample description and transition to psychosis of individuals at risk
J. Aston, U. Gschwandtner, S. J. Borgwardt, M. Drewe, M. Pflüger, R.-D. Stieglitz, A. Riecher-Rossler. Psych. Outpatient Department, Basel, Switzerland
Objective: The study aims to establish a scientific basis for the early detection of schizophrenic psychosis and to develop a “risk index”. The approach is a prospective and multilevel assessment of individuals at risk, and, after transition to psychosis, a post-hoc validation of the risk factors assumed a priori. Here, we describe the recruitment of the at-risk sample, the psychopathological features, and the transition to psychosis.
Methods: We established a specialised early recognition clinic at our psychiatric outpatient department. All referrals, suspected to be at risk for psychosis, were screened consecutively. Our specifically developed screening instrument ( “Basel FEPSY Screening Instrument“) assesses prodromal signs (DSM III-R), as well as other indicators of the beginning disease and known risk factors. Transition to psychosis was assessed with the BPRS and defined according to Yung et al. 1998.
Results: From 01.03.2000-28.02.2004, we screened 234 individuals. 91 were already psychotic. In 37, no risk for psychosis was found. 106 were identified as being “at risk”, n= 65 consented to participate, mean age 26.43 (SD 8.57), 39 (60%) male, 26 (40%) female. Of 53 remaining in follow-up up to September 2004, 18 have made the transition to clear cut psychosis.
Conclusion: Many of the referred patients were already psychotic and in need of neuroleptic treatment, which underlines the necessity of specialised clinics. The amount of transitions to psychosis of at-risk individuals shows that our screening instrument is a useful tool for the identification of individuals at risk.
P-09-07
Dysfunctional working models of self and others and psychopathological symptoms of schizophrenia
K. Katarasinska-Pierzgalska, A. Jarek, A. Gruszczynska- Mlodozeniec, M. Jedrasik, T. Szafranski, A. Szaniawska- Bartnicka. Institute of Psychiatry & Neuro III Department of Psychiatry, Warszawa, Poland
Objective: Dysfunctional cognitive schemata may influence individual vulnerability to schizophrenia. To measure dysfunctional working models of self and others Dysfunctional Working Models Scale (DWM-S) was developed by Perris and collaborators. The aim of the study was to assess the relationship between DWM-S scores and duration and severity of psychopathology of schizophrenia.
Methods: Forty inpatients with ICD-10. schizophrenia or schizoaffective psychosis were rated with PANSS, Calgary Depression Scale (CDSS), Hamilton Anxiety Rating Scale (HAMA) and InterSePT Scale for Suicidal Thinking (ISST). Patients completed self-report questionnaire DWM-S as well as State-Trait Anxiety Inventory (STAI).
Results: The mean age of the patients was 34,3 ± 14 years, they had mean 12,8 ± 3,2 years of education. The mean duration of illness was 10 ± 9,8 years, the mean number of previous hospitalisations was 6,1 ± 8. Mean DWM-S score was 130,6 ± 28,9. There was no significant correlation of DWM-S score with age, length of education, duration of illness, number of hospitalisations. We found positive correlation of DWM-S score with total PANSS score (Spearman R = 0,5, p<0,005) as well as disorganisation (cognitive) PANSS factor (R = 0,47, p< 0,009); but there were no significant correlations with depression or anxiety measures.
Conclusion: The score of DWM-S was not influenced by: age, sex, education, and duration of schizophrenic illness. Symptoms of anxiety or depression did not influence on DWM-S score. There was positive correlation of DWM-S and PANSS disorganisation factor.
P-09-08
Is patients’ self-report of the anxiety symptoms in schizophrenia reliable?
A. Jarek, A. Gruszczynska-Mlodozeniec, M. Jedrasik, K. Pierzgalska- Katarasinska, A. Szaniawska-Bartnicka, T. Szafranski. IPiN Dept, of Psychiatry> III, Warszawa, Poland
Objective: Anxiety symptoms are common in schizophrenia. However there is a paucity of data regarding prevalence, prognostic value and treatment of anxiety in schizophrenia. The methods of assessment of anxiety symptoms in schizophrenia are questionable. The aim of the study was to compare self-report measure of anxiety: Spielberger's State and Trait Anxiety Inventory (STAI) with different observer-rated anxiety scales in a sample of schizophrenic inpatients.
Methods: Forty inpatients with ICD-10. schizophrenia or schizoaffective psychosis were administered STAI. Then patients were rated with Hamilton Anxiety Rating Scale (HAM-A), Clinical Anxiety Scale (Snaith) and Covi's Anxiety Scale. Additionally independent investigators assessed psychopathology and side effects with different scales: 1) PANSS, 2) Calgary Depression Scale (CDSS) and Barnes Akathisia Scale (BAS), 3) Targeting Abnormal Kinetic Effects (TAKE) and InterSePT Scale for Suicidal Thinking (ISST).
Results: The mean age of the patients was 34,3 ± 14 years, the mean duration of illness was 10 ± 9,8 years. The median score for the STAI trait-anxiety sub-scale (TASS) was 46,5 and for state- anxiety sub-scale (SASS) was 52. TASS correlated moderately with observer rated measures of anxiety: Covi (R=0,46), HAM-A (R=0,43), Snaith (R=0,38) (all p<0,05). SASS correlated highly with Covi (R=0,79), Snaith (R=0,73), HAM-A (R=0,68) (all p<0,0001) as well as CDSS (R=0,58, p<0,001), ISST (R=0,41, p<0,05), total PANSS (R=0,45, p< 0,05) and PANSS positive factor (R=0,39, p<0,05).
Conclusion: Inpatients with schizophrenia can reliably report their anxiety symptoms and Spielberger's State and Trait Inventory may be a useful measurement of anxiety in schizophrenia.
P-09-09
Is it possible to assess depression and anxiety separately in schizophrenia?
A. Szaniawska-Bartnicka, A. Jarek, A. Gruszczynska-Mlodozeniec, M. Jedrasik, K. Katarasinska-Pierzgalska, T. Szaffanski. Poland
Objectives: In line with Kay's factor analysis of PANSS the correlation between anxiety and depression is substantial. Depressive and anxiety symptoms are usually analyzed jointly as they cluster together forming a distinct affective factor. On the other hand, it is suggested that anxiety and depression should be considered as separate dimensions of psychopathology in schizophrenic patients as they may differ in patophysiology, prevalence, and prognostic value. The aim of this study was to examine relationship of depressive and anxiety symptoms in schizophrenic inpatients.
Methods: Anxiety and depression was assessed in 40 inpatients with ICD-10. schizophrenia independently by different investigators. One of them administered Hamilton Anxiety Rating Scale (HAM-A), Clinical Anxiety Scale (Snaith) and Covi's Anxiety Scale. The other administered Calgary Depression Scale (CDSS). Spearman Rank Order Correlations were calculated for measures of depression and anxiety. Patients were also compared categorically with high (CDSS>3) or low depression and high (HAM-A>16) or low anxiety.
Results: The mean score for CDSS was 4,5 ± 4. Total CDSS score correlated with all anxiety measures: Covi (R=0,61), HAMA (R=0,64) and Snaith (R=0,67) (all p<0,0005). Both depressive mood (Cl) and observed depression (item C9 from CDSS) correlated with anxious mood (HI item HAM-A) (R=0,41; p<0,05 and R=0,7; p<0,001 respectively). 87,5% patients had the same level (low or high) of depression and anxiety.
Conclusions: There is a high correlation of depression (CDSS scores) and anxiety rating scales scores in schizophrenic inpatients.
P-09-10
Gender differences in negative symptoms among patients with first episode psychosis and patients with chronic schizophrenia
Z. Bronowska, T. Szaffanski. Poland
Objectives: The aim of this study was to compare psychopathological symptoms in the group of patients with first episode psychosis (FE) with patients with chronic, multi-episode schizophrenia (ME).
Methods: Fifty, drug naive, patients hospitalised with the first- episode psychosis (ICD-10: F20-F29), and fifty-four patients hospitalised due to exacerbation of schizophrenia (ICD-10: F20) were assessed with PANSS. PANSS symptoms were analysed according do Kay's five- factor model. There were 27 females and 23 males in FE and 28 females and 26 males in ME group. Differences between the groups were tested with Mann-Withney U Test.
Results: The difference in total PANSS score between FE and ME group (100,1 ± 17,5 vs. 108,3 ± 24,3) was not significant (Z= - 1,83; p= 0,067). Nor there were the differences in PANSS-positive, PANSS-disorganization and PANSS-depression factors. FE patients had less prominent negative symptoms: (PANSS-negative 21,4 ± 6,9 vs. 24,9 ± 6,7; Z=-2,73; p<0,01) as well as symptoms of agitation (10,9 ± 5,3 vs. 13,9 ± 7; Z=-2,l; p<0,04). Subsequent analysis revealed no significant differences in symptoms dimension between FE and ME females. Significant differences were found in males, with lower scores in FE versus ME group: PANSS total 96 ± 12,1 vs. 110,8 ± 20,4; Z=-2,4; p<0,02 and PANSS-negative 19,9 ± 6,6 vs. 25,9 ± 5,7; Z=-3,03; p<0,005.
Conclusions: There are significant differences in severity of negative symptoms between males with first episode psychosis and those with chronic multi-episode schizophrenia.
P-09-11
The influence of mechanisms of psychological defence on chronization and resistance of acoustic hallucinations at paranoid schizophrenia
A. S. Kim, E. Manjos, J. Thai. Russia
Objective: The paranoid schizophrenia patients with chronic acoustic hallucinations have the specific and limited repertory of mechanisms of psychological defense (mpd. The duration of the disorder and dominating affect are one of the basic factors, which causes the specificity of mental adaptation.
Methods: We surveyed 93 patients with paranoid schizophrenia at RCMH, Bishkek city. We used Clinical, clinical- cwanticic, Spielberg-Khanin's scale for the evaluation of anxiety, Zung's scale for the evaluation of depression, Plutchik- Kellerman-Kont's inquirer of vital styles.
Results: Patients suffering over 5 years (57%) had steady and stereotype acoustic hallucinations. In this category of patients was observed moderate (50%), minimal (32%) depressions, the high level of anxiety (91%) and prevalence of intensity of mpd projection 0.36 (P <0.01). Prevalence of mpd depending on duration of the disorder: less than 3 years: suppression 0.086 (P <0.01), and denying 0.086 (P <0.01), more than 3 year:, hypercompensation 0.183 (P <0.01), and rationalization 0.279 (P <0.01).
Conclusion: 1. The anxiety affect plays a role in development of chronization and resistance of acoustic hallucinations 2. Prevalence moderate (50%), minimal (32%) depressions is a personal reaction to mental disorder, stirring of functioning of the limited repertory of mpd. 3. The correlation of affective disorder and the mpd forms the stereotype of clinical-psychopathological disorder. 4. The limitation of repertory of mpd at patients with chronic acoustic hallucinations is the factor preventing from development of intensity of hypothymic affect
P-09-12
Depressive symptoms among patients with first episode psychosis and patients with chronic schizophrenia
T. Szaffanski, Z. Bronowska. Institute Psychiatry & Neurolo III Department of Psychiatry, Warszawa, Poland
Objective: The aim of this study was to compare depressive symptoms in first episode psychosis with patients with chronic, multi-episode schizophrenia.
Methods: Fifty, drug naive, patients hospitalised with the first- episode psychosis (ICD-10: F20-F29), and fifty four patients . hospitalised due to exacerbation of schizophrenia (ICD-10: F20) were assessed with PANSS and Calgary Depression Scale (CDSS) at admission. There were 27 females in first episode group (FE) and 28 females in chronic schizophrenia - multi-episode group (ME). Mean number of hospitalisations in ME group was 13,8 ± 10,5, mean duration of illness 18,1 ±9,1 years.
Results: Significant depressive symptoms (CDSS total score >7) were present in 50% of first-episode patients and 37% of patients with chronic schizophrenia (Chi2 = 1,78 p= n.s.). Depression was more common in females (52,7% vs. 32,6%; Chi2 = 4,25 p< 0,04). Depressive symptoms were more severe in FE group: CDSS total score 7,9 ± 5,2 vs 5,9 ± 5,8 (Mann-Whitney Z=- 2,07 p < 0,04). Symptoms of depression (Cl), self-depreciation (C3) and morning depression (C6) were more prominent whereas early wakening (C7) was less prominent in FE group than in ME group. The only difference statistically significant after Bonferroni correction (p<0,003) was more profound lowering of mood (C1) in FE (1,6 ±0,97 vs. 0,89 ± 1,04).
Conclusion: Depressive symptoms are common among patients with acute psychotic symptoms; these symptoms are more prominent in patients with first episode psychosis but the differences are not substantial.
P-09-13
Atypicality: A clinical study concerning atypical psychoses
S. Tuinier, F. Van der Heijden, W. Verhoeven, R. Kahn. Vincent van Gogh Institute Dept, of Psychiatry, Venray, Netherlands
Objective: In general, psychoses that do not fir neatly in either affective or schizophrenic disorders are commonly assigned to one of them, depending on the orientation of the investigator. The alternative, the schizoaffective disorder, still has an unclear clinical and nosological status.
Methods: If relevant symptoms and signs are recognized, cycloid psychoses as well as catatonia can be diagnosed. The nosological status of cycloid psychoses is not inferior to that of the functional psychoses in the DSM. On the contrary, the cycloid psychosis has a specific outcome, no genetic endowment and a specific treatment. Catatonia should be regarded as a syndrome that may accompany various somatic, neurological and psychiatric disorders and, if properly treated, is often reversible.
Results: In a group of consecutively admitted patients (n=136), the prevalence of cycloid psychosis appeared to be 13% while for catatonia a percentage of 18 was found. Although the cycloid psychosis according to the Perris and Brockington criteria (1981) showed some overlap with the ICD-10. category of Acute Polymorphous Psychotic Disorder and with the Brief Psychotic Disorder from the DSM-IV, the phenotype is by no means identical.
Conclusion: Catatonic symptoms occurred in a broad variety of DSM-diagnoses such as schizophrenia, schizoaffective disorder, depressive disorders and bipolar disorders. Catatonic symptoms, as rated with the Busch Francis Catatonia Scale, showed a bimodal distribution which suggests that catatonia can be considered as a separate diagnostic entity.
P-09-14
Change of diagnoses from schizophrenia to bipolar disorder in long-term course
J. Roder, B. Pflug. Main-Taunus-Kliniken Hofheim Abteilung fur Innere Medizin, Frankfurt, Germany
Objective: The present study investigated the syndrome shift during the course of disease in five patients with schizophrenic disorder (1 catatonic, 4 paranoid). The mean observation time was 46 years. All of them are initial diagnosed as schizophrenic and after 10,4 averagely develop into manic-depressive psychosis.
Methods: Retrospective study in five patients Results: Most of the published studies in the past point to a shift from affective or schizoaffective to schizophrenic psychosis. Our aim was to demonstrate the diagnostic shift in the opposite direction and further to give an extreme careful report about the change in psychopathological symptoms during the course.
Conclusion: It's an observation concerning a real diagnostic shift which is also demonstrated by the better outcome of our patients according to the outcome of bipolar disorders.
P-09-15
Heredity burden and sexual self-perception in schizophrenic patients
M. Vucic Peitl, A. Peitl, E. Pavlovic. KBC Rijeka Psychiatry, Rijeka, Croatia
Objective: The aim of this investigation was to establish possible difference between sexual self-perception (in accordance with seven aspects of sexual self-perception) in acute and chronic schizophrenic patients, taking into consideration their hereditary liability.
Methods: Two groups of schizophrenic patients were analyzed (acute - 100 and chronic -100), treated in Psychiatric clinic Rijeka, in the period 1998-1999., taking into consideration their hereditary liability, influence of that liability on the seven aspects of sexual selfperception (sexual self-scheme, sexual consciousness, readiness for sexual action, inclination towards sexual adventures, level of negative emotions towards one's sexuality, perception of one's sexual selfcompetence, level of satisfaction with one's sex life).
Results: Results of this investigation indicate that hereditary liability in acute schizophrenic patients has no influence on the aspects of sexual self-perception, while hereditary liability in chronic schizophrenic patients has a negative influence on the aspects of sexual self-scheme and the level of satisfaction with one's sex life.
Conclusion: Thus those with hereditary liability achieve lower results than the ones without hereditary liability.
P-09-16
Transsexual behaviour and schizophrenia: A case report
L. Borras, A. Eytan, E. Constant, P. Huguelet. University Hospital of Geneva Dept, of Psychiatry, Bruxelles-Belgique, Belgium
Objective: Adult males suffering from Gender Identity Disorder (GID) may ask for sex-reassignment surgery. It is therefore important to differenciate GID, characterized by a strong and persistent cross-gender identification and discomfort with one's own sex, from schizophrenic delusions.
Methods: We report the case of a 40 year old male patient suffering from chronic schizophrenia who developed intrusive gender identity preoccupations over the years. He repeatedly asked for sex-reassignment surgery, but regretted the operation shortly afterwards, considering it as “a mistake” and asking for reconstruction surgery
Results: Although schizophrenia and GID may coexist in very rare cases only, it is sometimes difficult to disentangle both conditions. In schizophrenia, there may be delusions of belonging to the other sex. Cross-gender identification in GID is not considered as delusional, because what is meant is that the person feels like a member of the other sex rather than truly believes that he or she is a member of the other sex.
Conclusion: The case we report illustrates the stakes of making a comprehensive diagnostic assessment of patients asking for sex- reassignment surgery, especially if a psychotic disorder is suspected. Considering the irreversible consequences of surgery and it's medico-legal implications, we suggest that, in case of persisting of an uncertain diagnostic and before approving any legal changes or even sex reassignment surgery, the transsexual wish should have remained unchanged under otherwise successftil antipsychotic treatment. Morever, the patients must be able to translate in reality the desired sexual role in their social environment.
P-09-17
Sexuality disorders of schizophrenics
I. V. Miclutia, R. Macrea. Univ. of Medicine & Pharmacy Cluj- Napoca, Dept. Psych. Cluj-Napoca, Romania
Objective: Disordered sexual behavior is common in schizophrenia, being, partly secondary to the disturbances of thought and perception. These disturbances affect the subjective experiences and the overt sexual behavior.
Methods: Two main periods in the evolution schizophrenia are evaluated: at the beginning and in cronicity. Various neuroleptics and novel antipsychotics are analyzed regarding the sexual adverse effects.
Results: The major disturbances of the sexuality of schizophrenics are: the quantitative and qualitative disorders regarding the sexual appetence, sexual practices due to the illness itself; sexual dysfunctions due to the antpsychotic medication. The disorders secondary to the illness refer to: lack of sexual interest, sexual apathy, anhedonia, libidinal impotence, although the opposite behavior may be observed as well especially at the beginning of the illness. The prepsychotic and early phases of schizophrenia, the cronicity have a hallmark in the field of sexuality: autoeroticism, mechanic masturbation, autofellatio. The forensic complications of sexual behavior are patognomonic for severely disturbed personalities (1). The sexual dysfunctions caused by antipsychotic medication may include dampening of sexual interest and desire, erection difficulties, ejaculatory problems, anorgasmia. Even novel antipsychotics are responsible for various sexual side effects (2).
Conclusion: We can assume that the sexuality of schizophrenics alters both qualitative through regression to mechanic masturbation and quantitative (sexual apathy, anhedonia). The range of sexual side effects of novel antipsychotics is less than those produced by neuroleptics. This fact could contribute to the long term acceptance of and adherence to antipsychotic medication of sexually active persons suffering from schizophrenia.
P-09-18
Assessing the ability to express sexual consent in a population of acute psychotic patients.
S. Ferracuti, M. C. De Marco, S. Zangaro, D. Accorrà, M. Raja, A. Azzoni, R. Tatarelli. Ospedale S. Andrea University “LaSapienza”, Roma, Italy
Objective: Sexual activity reflects the capacity to undertake interpersonal relationships, thus it is a significant index of the global functions of the patient and plays a fundamental role in quality of life. Establishing the actual freedom to express a consent to sexual activity in psychiatric patients is a complex problem, with insufficient presence in medical literature. The objective of the study was to evaluate the capacity to express a consent to sexual activity in a population of psychotic patients.
Methods: In order to evaluate this capacity a questionnaire deriving from a work by C. H. Kennedy e J. Niederbuhl in 2001 was designed, able to produce criteria to evaluate the awareness of sexual behavior in mentally retarded patients, such as fundamental and essential knowledge of the consequences of sexual activity, safety for themselves and others. Sixty patients were selected from the ones hospitalized in the Psychiatric Unit of the Ospedale Santo Spirito in Rome, affected by bipolar disorder with psychotic symptoms and by schizophrenic disorder (according to DSM-IV). The scores of the questionnaire about sexual awareness were correlated to those of the Progressive Matricies 38 test (P.M. 38), used to evaluate the intellective ability, and to those of the Brief Psychiatric Rating Scale (B.P.R.S.), used to evaluate the degree of psychopathology.
Results: The preliminary results seem to show that the designed questionnaire correlates with the level of psychopathology and with the intellective level of the patients.
Conclusion: The present study is a work in progress and it will be extended to a broader population, to obtain a deeper evaluation of the observed correlations.
P-09-19
Parents personality characterized of schizophrenic patients
F. Shamsaei, F. Cheraghi. University of Med. Science Faculty of Nursing, Hamedan, Iran
Objectives: Schizophrenia is a complex form of psychopathology usually characterized by the presence of hallucinations and delusions. Schizophrenia is the most disabiling of major mental disorders. Typically, schizophrenia begins in late adolescence or early adulthood, usually appearing before age 30 years and appearing in men earlier than in women. The family environment has a powerfoul influence on the course of illness in a thought disorder, so much that researchers once believed family environment was a causative factor in schizophrenia. The aim of this study is to survey of parents personality characterized of schizophrenic patients.
Methods: The design was a descriptive study. Participants in this study are fathers and mothers of schizophrenic patients. The participants consist of 60 parentes were selected by rendomize sampling. Data were collected in MMPI questionnaire that assessed 8 items, included: depression, hysteria, paranoia, hypochondriasis, schizophrenia, mania, pesicastenia, and anti social behavior. The analytical method described by mean and standardeviation(sd) was used.
Results: Outcome showed the mean age of the participants was 52.96 years. Most of them completed elementary education most of schizophrenia mothers and fathers had a depression, grieving and inferioritly feelings, and hostilety, anxiety and personal disorders. Overall, mean scores of histeria, depression, pesicastenia, antisocial and schizophrenia were high in parents.
Conclusion: The feeling enviroment and parents personal has powerful influence on the course of illness in a patient with a schizophrenia disorder so that, The parents of this patients have problematic communication patterns with their childems, therefore prevalence of ambivalanci, anxiety, hostilety and other signs of psychological disorder are high in them.
P-09-20
Aspects of Piaget's cognitive developmental psychology and neurobiology in psychotic disorders
S. Gebhardt, M. T. Huber. Universitat Marburg Psychiatrie und Psychotherapie, Marburg, Germany
Objective: Psychological, neurobiological and neurodevelopmental approaches have frequently been used to provide pathogenetic concepts for psychotic disorders. However, aspects of cognitive developmental psychology have almost not been considered in current models.
Methods: Using a hypothesis-generating approach, an integration of cognitive developmental psychological and neurobiological concepts has been carried out. A disorder of adaptation processes will be postulated.
Results: Assimilation and accommodation as forms of maintenance and modification of cognitive structures (schemata) according to Piaget (1896-1980) represent complex processes of the brain. Based on afferent signals cognitive schemata and cortical representations are developed resulting in a conception of the world, which realistic validity and actuality is still controlled and modified. Within this conceptual framework psychotic disorders may result from a disproportion of environmental demands and the ability to activate required adaptation processes. As a consequence autonomous cognitive schemata are generated, which fail to adjust with reality, resulting in psychotic symptomatology. With respect to the underlying neurobiology, neuromodulatory and neuroplastic processes in neural networks seem to play a crucial role.
Conclusion: Integration of cognitive developmental psychology into the existing pathogenetic concepts of psychotic disorders might lead to interesting insights into basic disease mechanisms and might also guide future research in the cognitive neuroscience of such disorders.
P-09-21
Perspective evaluation of psychotic patients treatment in a “parents and sons” ambulatory
C. Cecchetto, S. Bressan, M. Civiero, M. Pierri. Clinica Psichiatrica Dip.di Neuroscienze, Padova, Italy
Objective: The aim of this study is the evaluation at 3 and 6 years of a 44 psychotic or with severe borderline personality disorder patients population, aged 18-45, after the taking in cure at the “Ambulatory of Consultation and Psychotherapy for Parents and Sons” of the Mental Health Center (III Psychiatric Service) of the University of Padua.
Methods: A first diagnostic and clinical analysis of the sample was carried out in 1998 trough a semistructured interview, the Brief Psychiatric Rating Scale -BPRS- and Global Assessment of Functioning -GAF- (fifth axis of the DSM multiaxial evaluation).
Results: The first follow up of a 32 patients sample, in 2001, does not show significant differences in BPRS total score, while it points out a modification in the symptomatology: decrease of positive psychotic symptoms and of some depressive symptoms, worsening of self carelessness, conceptual disorganization and of some symptoms related to activation. GAF shows an improvement in the total score. The second follow up of a 22 patients sample was carried out in 2004 after a territorial redistribution process of Psychiatric Services and the consequent end of the taking in cure at the Ambulatory for Parents and Sons.
Conclusion: A preliminary analysis reveals a significant worsening in BPRS total score compared to 1998. There is not a significant modification in GAF total score. Findings will be discussed.
P-09-22
Life quality in patients with schizophrenia
D. Degmecic, I. Pozgain, N. Blagojevic-Damasek, V. Perekovic,
M. Grgic. Psychiatric Cirtic Clinical Hospital Osijek, Osijek, Croatia
Objective: The aim of this prospective study was to determine if there was any difference in the life quality of patients treated with conventional antipsychotics and patients treated with new generation antipsychotics.
Methods: The authors examined two groups of patients who fullfilled ICD-10. criteria for schizophrenia.The first group(N=30) was treated with conventional antipsychotics(flufenazin, haloperidol), and the second group (N=30)was treated with new generation of antipsychotics (risperidone,olanzapine, quetiapine). All of the patients were treated at our clinic for at least six months. Both groups of the patients were tested with questionaire with epidemiological data, with Clinical Global Impression scale, than Quality of life scale, and with Multidimensional Scale of Percived Social Support. The authors used t-test in the statistical analysis.
Results: Epidemiological data- Mean age of the female patients was 44,33 years, and for male patients was 42,80 years. In both groups most of them were unemployed and married with finished high school. There was no significant statistical difference on the Clinical Global Impression Scale, as well as on the Multidimensional Scale of Percived Social Support Scale, but on the Quality of Life Scale the authors found statisticaly significant difference. Also we anlysed every item separately of Quality of Life Scale and we found statisticaly significant difference on two items (Item 13. Socialisation, and Item 14. Reading, listening to the music).
Conclusion: We can conclude that patients who are treated with new generation antipsychotics have subjective feeling that they are living with more quality in their lifes than patients who are treated with conventional antipsychotics.



Comments
No Comments have been published for this article.