Introduction
Embracing multicultural diversity, equity in healthcare, and inclusion of community voices in healthcare settings are critical steps toward understanding and addressing healthcare needs of vulnerable and marginalized populations[Reference Woolf, Zimmerman, Haley and Krist1–Reference Holzer and Kass4]. To this end, there is a growing appreciation of including the community voice in all phases of the research processes toward improving healthcare services[Reference Sprague Martinez, Carolan, O.'Donnell, Diaz and Freeman5–Reference Selby, Forsythe and Sox6]. Collective voices from a culturally diverse community can 1) alleviate negative perceptions about healthcare research, 2) effectively discuss health inequities in marginalized patients, 3) address structural racism and discrimination in healthcare, and 4) promote trust in the research process [Reference Elder, Evans and Funes7–Reference Skinner, Williams and Richmond9].
While the practice of cultural diversity, equity, and inclusion (DEI) is abundantly endorsed in biomedical, healthcare, and academic medical teaching settings [Reference Bennett10–Reference Holley22], evidence of stepwise implementation of these endorsements is not extensively evaluated or documented [Reference Steinkamp, Deuel, Lucre and Zavala23–Reference Peek, Allen, Pacala, Nickerson and Westby25].
To evaluate DEI practices, steps toward achieving a unified DEI that supports a sustainable community-academic partnership (CAP) need further documentation.
The overarching goal of the Community Research Advisory Council (C-RAC) of the Johns Hopkins Institute for Clinical and Translational Research (ICTR) has been to build a trustworthy relationship [Reference Gilfoyle, MacFarlane and Salsberg26] among community members and academic researchers through education, and service activities. Specific objectives of the C-RAC have been to develop, implement, and monitor health services research-related activities that benefit both the academic and community partners indirectly or directly within the Greater Baltimore-Washington region.
Since its inception, the C-RAC has striven to build a sustainable community-academic partnership toward promoting successful community-engaged research (CER) and dissemination of research findings. Accordingly, this report illustrates DEI strategies and practices that have enhanced and sustained CER among Johns Hopkins researchers.
The concepts and constructs presented in this special communication are highlights of DEI activities as a result of successful community-academic partnership in healthcare research over the years. Several constructs presented here are in the process of being structured and operationalized for future reports.
Materials and Methods
Ongoing Community-academic Partnership Activities on DEI
The C-RAC was created in 2009 to provide a space where co-learning can take place between researchers and the community being served. Over its 14 years of existence, the C-RAC has evolved into a model fostering DEI in an insular, academic research setting. With bylaws on governance structure and subcommittees run by community partners, a working model was established to help shift the power dynamic between the research institute and the community with community partners seen as trusted experts based on lived experiences and environments in which they reside. Specific activities of the C-RAC include: (1) ensuring cultural diversity in race/ethnic, age, gender, sexual orientation, and occupational backgrounds in the C-RAC membership composition, (2) facilitating equitable access to healthcare research to address health disparities and social justice, (3) improving community awareness, trust, knowledge, understanding, and inclusion in all phases of the research continuum in relevant community-engaged research, and (4) documenting the engagement steps and processes to evaluate researcher commitment to a fully engaged community within the entire research process. These steps are routinely monitored by the community partners of the C-RAC with a unified approach and goal toward improving health outcomes and reducing health disparities.
Conceptualizing and Operationalizing Trust
Since its inception, the C-RAC has adhered to seven operationalized [Reference Gilfoyle, MacFarlane and Salsberg26,Reference Gilfoyle, Salsberg, McCarthy, MacFarlane and MacCarron27] domains of trust as integral to DEI. These multi-dimensional domains included (1) acknowledging and working to address vulnerability among the community partners to fully understand research, (2) encouraging academic partners to fully explain the nuances and critical phases of the research continuum, (3) enhancing the belief that community partners will act and follow a set of guided principles of research, (4) sharing on values, visions, and goals toward trust-promoting plans and activities, (5) facilitating a set of collaborative tasks based on perceived skill set, expertise, and experience of each partner, (6) ensuring reliability and reciprocity of timely research tasks performed by both partners; and (7) power sharing and co-ownership of partnership activities. Steps and processes are currently in progress toward developing structured surveys on trust dimensions with the aims of psychometric testing, analysis and dissemination of findings in relation to community-engaged research.
The conceptual framework (Fig. 1) illustrates a unifying model for a successful community-academic partnership in research. A key feature in this framework is a sincere recognition by the academic partners of the mistrust and the negative perception about health services research and delivery that exist in the community. The unifying model promotes bidirectional engagement to build sustainable trust and ensure DEI for critical community issues. Using DEI strategies, the C-RAC translates community inputs to assist academic researchers throughout the research continuum and vice versa. These iterative processes facilitate both community and academic partners to listen, understand, and reciprocate concerns of both sides toward building a successful community-engaged research. Consequently, these iterative interactions and engagements generate a sustainable trustworthy community-academic partnership among researchers who solicit community inputs to succeed in their research endeavors (Fig 1).
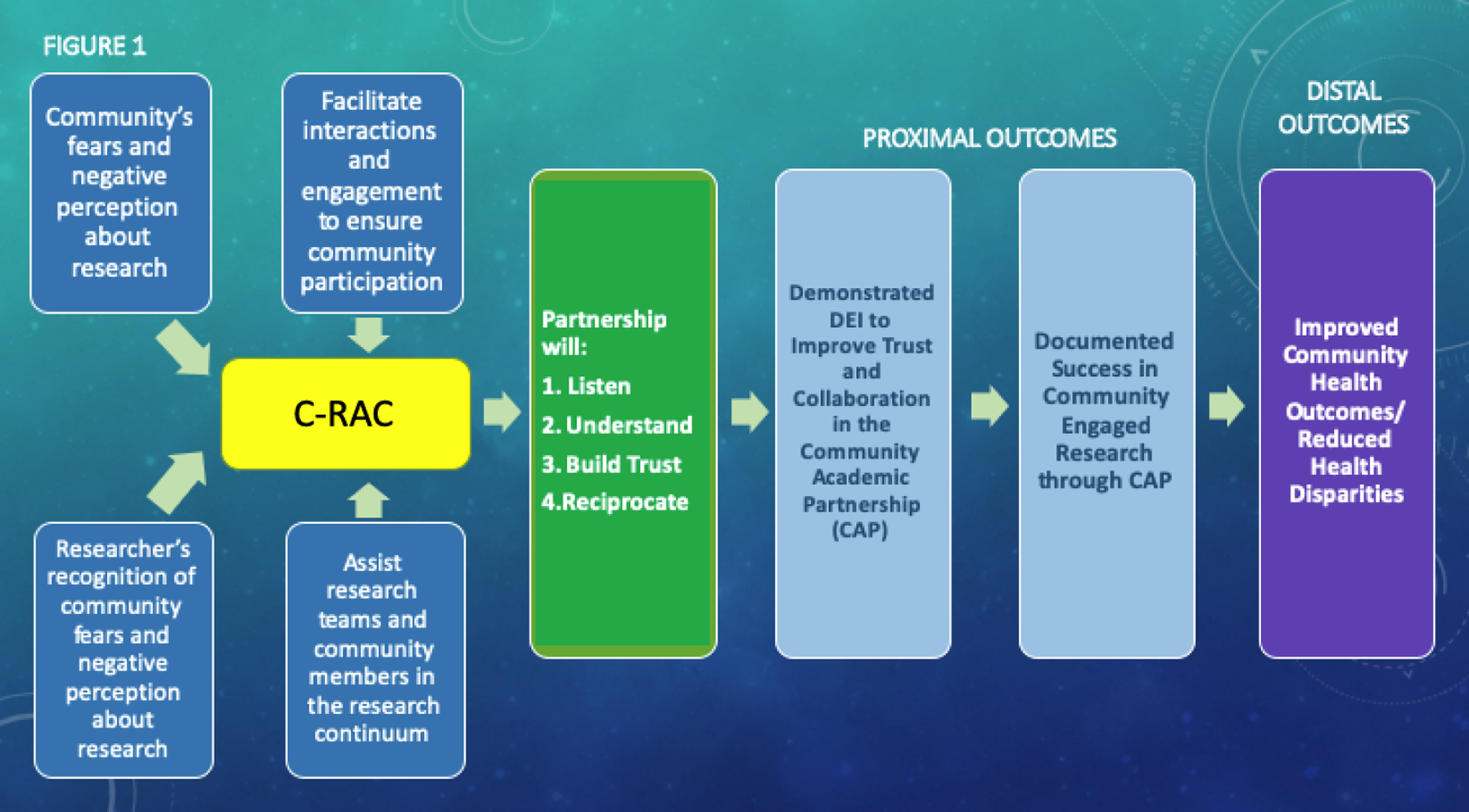
Figure 1. Unifying framework toward a sustainable community-academic partnership in research. C-RAC, Community Research Advisory Council.
The C-RAC’s activities adhere to structural and logical steps within the unifying DEI model. As an instructive road map to illustrate the resources or inputs required to achieve the DEI goals, the logic model in Fig. 2 depicts the step-by-step relationship among resources, planned work, and intended DEI results. The logic model also guides processes to evaluate desired goals and objectives. The logic model describes how inputs and activities based on DEI-relevant queries and objectives will lead to intended DEI outcomes.

Figure 2. Logic model for DEI practices in the community-academic partnership. CAP, community-academic partnership; C-RAC, community- research advisory council; TL1, predoctoral training program.
The inputs, activities, and outputs circumscribe a unifying approach to DEI within the C-RAC and follow outcomes that address a specific inquiry or objective. For example, to evaluate that the C-RAC has a culturally and racially diverse membership, its composition is periodically recalibrated. Furthermore, to ensure equity in community voices in the research process, community leaders are invited to participate in ad hoc forums to identify and prioritize unmet health needs, thus paving the way toward future research endeavors. Similarly, the extent to which researchers reciprocate community feedback and document revisions in their research protocol has been a yardstick to demonstrate the inclusion of community voices toward achieving DEI goals in the CAP.
Outcomes of DEI Efforts
The C-RAC strives to function as a DEI team within the community-academic partnership. Each DEI activity has shown promise that community voices can be heard toward alleviating the mistrust in the research continuum.
Diversity
Per bylaws, C-RAC membership constitutes more than half of nonacademic, community partners. Cultural and geographic diversity (five counties) of the thirty-two members reflect five age groups (30–83 years), six race/ethnic groups (twenty-one Blacks/African Americans, five Whites, two Latinas, three Asians, one African), two-third females, three LGBTQ individuals, employed, retirees, and semi-retirees, community health navigators, activists, federal, state, and local administrators, academic support staff and faculty. Additionally, the C-RAC membership represents diverse stakeholder groups, e.g. community leaders, research participants, patients, lawyers, faith-based and business community, students, staff, and faculty. Overall, membership included seventeen community partners and fifteen faculty and staff from Johns Hopkins, herein termed as academic partners. On an average, each member attended sixteen out of the twenty-two scheduled meetings in a calendar year, served as member for at least 2 years, and actively participated in at least one subcommittee. Almost three-fourth (23 of 32) of C-RAC members have been actively participating in activities for 8–10 years.
Equity
The C-RAC is engaged in three major efforts throughout the year: (1) research reviews as consultative services from community partners who provide guidance/advice to research teams throughout the grant writing and post-award research processes, (2) community outreach through two annual programs to provide cutting-edge information on prevention, treatment, research, and ethics of community prioritized clinical topics, and (3) availability of clinicians and researchers at local markets to discuss medical and research topics of interest to community members. To this end, the inputs of both the community and academic partners are equitably distributed in order to achieve measurable success of the aforementioned efforts. Overall, the academic partners have been very supportive of C-RAC with a goal to ensure that benefits of the collaborative knowledge-sharing activities flow equitably between community and academic partners.
Another example of equity in power sharing in the CAP is the composition of three (research and training; governance; community outreach) committees, each with a chair (elected by the C-RAC members) from community partners. A major task of each committee is to ensure DEI in C-RAC matters. Currently, ten community partners and three academic partners constitute the governance committee.
In matters of equity in CAP, community partners needed more direct, clear, and articulated communication with the academic partners. Community partners frequently indicated that they needed to clearly and comprehensively understand what researchers discussed on a particular topic. Thereupon, the “Teach Back” was a critical process on the part of both the community and academic partners that ensured discussion issues remained understandable, iterative, comprehensive, and transparent. The Teach-Back methodology, adapted from the Agency for Healthcare Research and Quality’s Health Literacy Universal Precaution Toolkit [28], encompasses several steps practiced by community partners in response to community consultations requested by the TL 1 research scholars. The TL 1 research scholar program is a competitive predoctoral scholarship as part of the CTSA to increase the translational research workforce and enhance career development of future leaders of the biomedical research workforce. The C-RAC’s teach-back process begins with one community partner (1) being assigned to the TL 1 research scholar who had requested C-RAC consultation services, as part of triaging, (2) having a thorough understanding of the research topic and its relevance to health disparity and health equity through iterative communication and formal tracking of activities with the TL 1 research scholar, (3) actively participating during the presentation of the research topic by the TL 1 research scholar at the C-RAC meeting, (4) presenting his/her understanding of the research topic, personal experience, and implications for community benefits of the presented research, and (5) reflecting again to demonstrate understanding and evaluate the extent to which suggestions were implemented by the TL 1 scholar who illustrates on the research results at a 4–6 month follow-up session. Teach-Back sessions led by community members of C-RAC are now implemented in programs where established and aspiring researchers formally share information with the community.
To acquire a better understanding of equity in healthcare research, community partners took an initiative to increase their knowledge about the regulatory definitions and types of research that involve human subjects as participants. This community-initiated effort culminated in 12 community partners getting certified with the human subject research training (online) provided by the U.S. Office of the Human Research Protections
The CAP around equity issues made both sides realize that there was a strong need to improve the health literacy of community around research topics presented by the academic partners. Efforts are on the way from researchers to design and implement more innovative ways to communicate their research with the community.
Inclusion
One metric of successful DEI is the increase in community representation provided by community partners on academic forums that needed community input and active participation toward a shared CAP agenda. These include community representation at the Johns Hopkins ICTR Leadership Council, National Institutes of Health (NIH) Community Engagement Alliance (CEAL) for the District of Columbia, Maryland, and Virginia Executive Committee, and the NIH CEAL Team Publication Committee.
A critical tenet of these committees is to develop and practice initiatives that incorporate community voices into their agenda. All of the above committees required involvement in activities requiring substantive time during the workday. The community representatives were given herein the opportunity to provide community voices, give feedback on issues that impact the community, and subsequently discuss these issues at the C-RAC meetings.
With these meaningful inputs and engagement throughout the entire research process, the CAP demonstrated that community input has the potential to impact funding, recruitment and retention, research participant informed consent, quality of educational materials, and dissemination of research.
Evidence of DEI in Successful Community-Engaged Research
Albeit brief, this special communication illustrates several DEI strategies toward successful and continued community-engaged research that benefits community partners directly or indirectly. Most of these strategies are initiated, implemented, and routinely monitored for quality improvement purposes, mostly by community partners. Thus far, incorporation of community inputs using DEI strategies in academic research has resulted in eleven grant proposals submitted to the National Institutes of Health and the Patient-Centered Outcomes Research Institute. Six of these applications have been awarded funds for community-based participatory research. The CAP has also contributed to twelve research publications. Table 1 shows data supporting program successes in dissemination of research findings to academic and community audiences. In addition to the C-RAC membership composition to demonstrate CAP diversity, providing research-based information to diverse consumer groups in local community markets has also strengthened the CAP. Community-initiated annual conferences (Healthy Aging), outreach activities (Day At The Market), formal feedback reflecting community concerns, as well as shared governance in the C-RAC organizational structure also reflect a growing equitable distribution of shared responsibility (Table 1). Conversely, inclusion of community partners in the decision-making process throughout the research continuum, and providing research-related training, although nascent, demonstrate the extent of inclusivity in the CAP.
Table 1. Outcomes of community-academic partnership (CAP) activities to ensure DEI

Table 1 illustrates that the overall CAP activities embrace a DEI paradigm with overlapping activities. Overall, successful DEI in the CAP is clearly reflected by the funding awards, journal publications, and committee membership as part of a growing relationship.
To promote equity in the community-academic partnership, issues that impact the community are initiated by community partners at scheduled meetings of the C-RAC. In these interactive community grand round forums, invited community leaders present details of current health issues that affect their communities. On different occasions and upon invitation by community partners, academic partners present their research that impacts the community’s health. In both instances, feedback and suggestions from community members are noted for incorporating them into future research practices. The ongoing annual Healthy Aging Forum has been a community-initiated forum that has in recent years incorporated topics such as “sister circle” and “man cave” to discuss cutting-edge research-based applications on men’s and women’s health, respectively. These small group, open-ended, interactive sessions have been popular by overwhelming demands from the lay community in the past five years. The C-RAC is currently in the preparatory process of a Handbook of Community Engagement in Healthcare in this regard.
Benefits for Community Partners
The current structure in the CAP has been, to a large extent, focused on community consults and is initiated by academic research partners. However, in recent years, the C-RAC has been developing mechanisms for intellectual benefits to community partners. Tangible and intangible benefits received by community partners include: (1) being invited, and compensated as subsequent research team member, (2) sharing governance of the ICTR and C-RAC, (3) getting training and certifications on human subject research, (4) initiating manuscript writing processes (including this report) for peer-reviewed journals, (5) membership in national and regional community advisory boards e.g. CEAL and Community Connect, and (6) receiving financial compensation for attending C-RAC meetings.
Benefits for Researchers
CAP benefits received by academic partners include: (1) successful applications for federal, state, local, public, and private funding opportunities, (2) improved recruitment and retention of research participants, (3) streamlining of informed consent and IRB applications, (4) publications in peer-reviewed journals, acknowledging contributions from community partners.
Measuring the researcher’s ability to conduct successful community-engaged research also included a recent semi-structured survey among researchers on whether the C-RAC consultation improved the quality of their research, and whether the community consultations provided feedback on proposal development, informed consent, recruitment and retention, and dissemination. More than two-thirds reported positively on the benefits received from community consultations and inputs on participant recruitment and retention. Overall, investigators who utilized the consultation service reported a wide range of positive impacts on research projects, including ability to apply for funding, and development of long-term partnerships.
Example of Co-Learning Opportunities in CAP
Figure 3 illustrates evidence of successful CAP when utilizing the DEI paradigm. Researchers reported increased understanding of community views on research and health priorities of the community toward a successful community-engaged research. Community members stated that participating in consultations gave them an opportunity to educate researchers about the concerns of people living in their community and reported increased understanding of the research process. Figure 3 illustrates evidence of equity and inclusion via active participation, iterative discussions, strategic actions, and improved trust among the partners. Additionally, a fifty-nine percent (425 out of 719) follow-up in the project demonstrates a successful CAP resulting in participant retention when the principles of DEI are applied.

Figure 3. Co-learning opportunities in CAP and successful DEI.
Discussion
This report describes steps implemented by JH-ICTR C-RAC to achieve DEI via successful CAP. The C-RAC adheres to the framework shown in Fig. 1. The commitment to listening, understanding, improving trust, and reciprocating community voices (“give back”) has resulted in dynamic DEI engagement and innovative strategies initiated by community partners and supported by academic partners. C-RAC activities that are responsive to roadblocks via DEI strategies are shown in Table 2.
Table 2. Community-Research Advisory Council (C-RAC) activities that are responsive to roadblocks via DEI strategies

Unique Strategies in Implementing DEI
In this report, we have noted a number of unique and intended DEI strategies, which have been beneficial to both the community and academic partners.
The C-RAC is reflective of many unique characteristics that are not visible, at least in similar literature, and interactions with other CTSA awardees in the nation. For example, as part of the enriched consultations, the academic partners from the four independent divisions (Medicine, Nursing, Public Health, and the Hospital) continuously engage with the community partners on a weekly basis toward the monitoring and improvement of a community-engaged research from the beginning of a grant solicitation application and throughout the research continuum process.
A second unique partnership effort as part of Hopkins Opportunity for Participant Engagement initiated by the C-RAC in the past three years has resulted to date in recruitment with consent, of more than seven thousand research participant volunteers who are then triaged to disease/treatment specific researcher/provider specialist.
A third unique and notable partnership characteristic has been the recent linkage between academic cardiovascular research partners and C-RAC community partners who are engaged in substance abuse and mental illness treatment and recovery services for vulnerable population such as drug addicts and the homeless in urban settings. Such partnership not only provides promising practices to study and offers cardiovascular (Linked BP and Linked Heart Studies) services for substance abusers but also focuses both on the limitations and potential of unique and successful community-engaged research that improve health outcomes among vulnerable, urban populations.
Three general themes in the broader CAP framework emerged when community partners were asked to suggest ways of improving DEI: (1) Ensuring that community members of diverse backgrounds are involved and well-informed about the research continuum process, terms, importance, and value of their input through advance preparation of community-engaged research activities with simple, understandable, and clear communication format; (2) incorporating bidirectional feedback from the community members and researchers throughout the process (“consistent feedback of what input and advice from the community has been used”): all researchers were required to send a completed report of their project findings that commensurate with community feedback, and lastly, (3) marketing of the community consultation services to ensure that the community advice benefits future researcher with similar domains/specialties.
As presented earlier, the community partners' initiation of the Community Grand Rounds demonstrates equity wherein invited community leaders have discussed issues of structural racism and discrimination, white supremacy, and unmet health services/research needs in their respective communities and what is important to them from research perspective.
Community partners have expressed interest in an array of activities relevant to “inclusion“ including receiving training/workshops about topics from researchers so as to improve: (1) disseminating research results to study participants and the community, (2) learning about different research methods, (3) preparing community driven grant proposals, (4) successful and sustainable strategies to maintain research partnerships or programs that become critical to community-engaged research projects, (5) developing a research question, (6) best ways to recruit and keep research participants in studies, and (7) the nuts and bolts underlying research ethics including informed consent.
Lessons Learned/Current Challenges
The community-academic partnership, albeit a successful venture, frequently faces challenges that need to be efficiently addressed toward improving mutual trust in research. For example, learning the dynamics of a complex research process, from definition, methodology, conduct, and dissemination as explained by seasoned researchers, has been a challenging learning process for the nonacademic community partners. On the other hand, academic researchers, while grappling with the cumbersome tasks of recruiting hard-to-reach, mistrusting, vulnerable, eligible research participants, have to rely heavily on community partners to learn successful recruitment and retention strategies. Rather than budgeting reasonable resources to recruit hard-to-reach eligible participants, the perception that participant recruitment needs the least resources may need serious reconsideration.
The CAP frequently faces two other critical challenges that are related to successful research: (1) transparency and disclosure of tangible benefits that the research would bring to community where the research is being conducted, and (2) dissemination of research findings to the same community who participated in the research. Current research protocols, including those submitted to IRBs, only abbreviate these activities but do not expand them, which could improve research participation.
As a continuously evolving process, the partnership sets forth quarterly meetings to introspect critical activities toward strengthening the partnership. Issues that community partners have raised are (1) use of budget lines to formally include interested community partners in grant proposals with post-funding roles and responsibilities, (2) developing mechanisms for community partners to actively participate in the research decision-making process, (3) allocating time and space for community partners to discuss partnership governance, administration, and financial and technical support issues, (4) expediting the compensation process, (5) evaluating the power dynamics of the CAP related to the structural hierarchy in academic settings, (6) tapping into community talent while respecting community time, and (7) recruiting younger generation (e.g. less than 30 years of age) as community partners to learn the dynamics of a CAP. Each of these challenges is currently being addressed as joint CAP endeavors.
Sustainability
How to sustain an evolving CAP has been a continuing challenge among both community and academic partners, particularly on resource allocation and time commitment toward bidirectional communication in achieving desired CAP impact. Currently, community partners are working toward generating resources by tapping into public or private funds that are available to community-based organizations that address structural racism and discrimination and improve health outcomes.
Future Direction to Measure Effectiveness of DEI
To an extent, the CAP works in synergy and collaboratively by designing and implementing practical training and exercises to reinforce DEI efforts in the community-partnered research decision-making process. By continuously refining the logic model, the community partners will be able to understand the structure, process, and outcome of rigorous research by the academic partners, and learn that each research follows specific steps encompassing the research continuum that can be measured and documented.
Regardless of whether a research problem or issue is initially identified by either community or academic partners, a fully engaged CAP will need, from the very onset, to jointly develop a research question, formulate a hypothesis, and design the methodology, data analysis, and plan to disseminate results. Such opportunities will provide the optimal environment for community partners’ appreciation of the intricate research process, and in reciprocation, enable the academic partners to build on the partnership to identify innovative ways to improve the community-engaged, bidirectional research [Reference White, Patel and Cossari29,30].
In summary, the CAP effectively utilizes the C-RAC to provide (1) expanded knowledge towards creating a bidirectional learning community, (2) shared governance with built-in trust, (3) a sustainable diverse membership, and (4) community-aligned solutions in a diverse, equitable, and inclusive environment.
Acknowledgments
Community Partners: Caroline Henderson, Sharon Hunt, Janet Johnson, Aurelia Laird, LA Macrae, Tyrone Qualls, Inez Robb, Melanie Reese, Michael Thompson
Academic Partners: Barbara Bates-Hopkins, Lee Bone, Samuel Byringiro, Patricia Carroll, Crystal Evans, Panagis Galiatsatos, Cassie Lewis-Land, Frederick Luthardt, Darcenia McDowell, Tracey Newsome, Ana Rule, Sarah Stevens, Mia Terkowitz, Monica Vazquez, Christine Weston, Cheri Wilson, Donald Young.
Funding statement
This publication was made possible by the Johns Hopkins ICTR, a component of the National Institutes of Health (NIH), and NIH Roadmap for Medical Research and by funding for the Johns Hopkins C-RAC, which is funded in part by Grant Number 1-UL1TR003098 (authors JN, JH, RC, CL, PO, CH). The contents of this manuscript are solely the responsibility of the authors and do not necessarily represent the official view of Johns Hopkins University, Morgan State University, or NIH.
Competing interests
The authors have no conflict of interest to declare.







