1. Introduction
Over the last few decades, there has been growing evidence that the natural course of borderline personality disorder (BPD) is characterised by its plasticity, with consecutive periods of remission and relapse, and shows a trend towards symptomatic amelioration over time. Despite that, adults with BPD appear to frequently suffer from poor psychosocial functioning in the long-term [Reference Biskin1, Reference Paris2, Reference Ng, Bourke and Grenyer3]. Bearing this in mind, Paris suggested that treatment efficacy should be assessed in terms of their contribution to enhance the natural process of the disorder. In this respect, it is noteworthy to study the impact of psychotherapeutic interventions in patients with BPD in the long-term, both in the symptomatic and functional domains [Reference Paris2, Reference Ng, Bourke and Grenyer3].
Two main prospective studies provided evidence on a wide range of aspects related to the long-term course of adults with BPD: the McLean Study of Adult Development (MSAD) and the Collaborative Longitudinal Personality Study (CLPS) [Reference Skodol, Gunderson, Shea, McGlashan, Morey and Sanislow4, Reference Zanarini, Frankenburg, Hennen, Reich and Silk5, Reference Zanarini6]. Both research projects demonstrated that it is common for BPD patients to experience periods of symptomatic remission over time, reporting high cumulative rates by 10 years (85% 12-month remission in CLPS; 93% 2-year remission in MSAD) [Reference Zanarini6]. At 16 years, the MSAD also reported that 78% of BPD patients had achieved a long-lasting remission of eight consecutive years [Reference Zanarini, Frankenburg, Reich and Fitzmaurice7]. Nevertheless, the recovery of psychosocial functioning was less consistent than symptomatic remission, oscillating between a steady functional impairment reported by the CLPS and a slight improvement by the MSAD [Reference Zanarini6]. Besides, patients with BPD were mostly not able to achieve normal levels of functioning in the long-term: only 33% had good functioning after 6 years in MSAD; and just 21% did so after 10 years in CLPS [Reference Zanarini, Frankenburg, Hennen, Reich and Silk8, Reference Gunderson, Stout, McGlashan, Shea, Morey and Grilo9].
Apart from the longitudinal research conducted in the US population, other naturalistic studies were carried out in different countries (i.e., Spain, Canada, Finland, and Germany) providing prospective data for a period of five years or more. Findings in these studies add to the evidence that the course of BPD is characterised by symptomatic improvement, although remission rates ranged widely from 31% to 81%, which were informed at different time points of follow-up [Reference Alvarez-Tomás, Soler, Bados, Martín-Blanco, Elices and Carmona10, Reference Links, Heslegrave and Van Reekum11, Reference Riihimäki, Vuorilehto and Isometsä12, Reference Zeitler, Bohus, Kleindienst, Knies, Ostermann and Schmahl13]. Álvarez-Tomás et al. also reported a slight improvement of psychosocial functioning in a Spanish sample followed up at 10 years, although dysfunctional levels of adjustment were maintained [Reference Alvarez-Tomás, Soler, Bados, Martín-Blanco, Elices and Carmona10]. Moreover, only one third of subjects with BPD, on average, achieved both symptomatic and functional recovery at a 14-year follow-up in a German study [Reference Zeitler, Bohus, Kleindienst, Knies, Ostermann and Schmahl13].
Further analysis of potential moderators should be required to take into account variations on the course of BPD among studies. In this regard, previous longitudinal research pointed out the following factors as predictors of long-term outcomes: demographic characteristics, childhood experiences, stressful life events, treatment history, psychopathologic comorbidity, personality traits, and premorbid psychosocial functioning [Reference Zanarini, Frankenburg, Hennen, Reich and Silk14, Reference Shea, Edelen, Pinto, Yen, Gunderson and Skodol15, Reference Gunderson, Stout, Shea, Grilo, Markowitz and Morey16, Reference Soloff and Chiappetta17, Reference Wedig, Frankenburg, Bradford Reich, Fitzmaurice and Zanarini18].
In addition to naturalistic research, clinical trials of psychotherapeutic interventions for BPD have recently shown greater interest in their long-term outcomes, reporting follow-up data for five years or more [Reference Antonsen, Kvarstein and Urnes19, Reference Bateman and Fonagy20, Reference Davidson, Tyrer, Norrie, Palmer and Tyrer21, Reference Sahin, Vinnars, Gorman, Wilczek, Åsberg and Barber22, Reference Stevenson, Meares and D’Angelo23]. This longitudinal perspective on efficacy studies underlines the relevance of treatment as a potential factor of change over time. Nevertheless, findings are controversial among studies with respect to a differential impact of specialised therapies in comparison to treatment as usual (TAU) on diagnostic change and social functioning in the long-term. Bateman and Fonagy reported significant differences on remission favouring mentalisation-based treatment (MBT) over TAU (86% vs. 13%), but this effect was not found for other specialised therapies [Reference Antonsen, Kvarstein and Urnes19, Reference Bateman and Fonagy20, Reference Davidson, Tyrer, Norrie, Palmer and Tyrer21]. Antonsen et al. reported better outcomes for the social functioning of a specialised therapy for personality disorders compared to TAU, in contrast to findings in the Boscot trial indicating a similar impact of treatment interventions [Reference Antonsen, Kvarstein and Urnes19, Reference Davidson, Tyrer, Norrie, Palmer and Tyrer21]. As far as we are aware, there are no published meta-analyses that synthesise current evidence on the long-term outcome of treatment interventions in BPD or that combine these findings with those from naturalistic prospective research. This may contribute to the study of long-term treatment effects in the context of the natural course of the disorder.
Thus, our objective was to conduct a meta-analysis of studies reporting the prospective results on the long-term course of BPD, considering both naturalistic and post-treatment follow-up research. In case of heterogeneity among studies, we were interested to study the effect of potential moderators related to the natural course (e.g., age, gender, time of follow-up, psychiatric comorbidity, and initial level of functioning) and those related to the treatment interventions received. The following questions were addressed: (1) What characterises the long-term course of BPD in adulthood, both in clinical and functional domains? (2) Are there significant moderators that influence the long-term course of the disorder?
2. Materials and methods
2.1. Search strategy
Our literature review was guided by the PRISMA standards for systematic reviews [Reference Liberati, Altman, Tetzlaff, Mulrow and Gøtzsche24]. Bibliographic searches were conducted in Medline, PsycINFO, PsycArticles, PubMed, and Scopus to identify relevant literature during the period 1990-2017. The searching strategy was a combination of the following two steps: (1) either “borderline personality disorder” or “personality disorders” were used in addition to terms indicating a temporal dimension, i.e., “follow-up”, “course”, “longitudinal”, “long-term”, or “maintenance”, in the title or abstract field; (2) the terms “borderline personality disorder” and either “treatment*”, “therap*”, “psychotherap*”, “intervention*”, or “program*” were combined in the title field and added to similar temporal terms in the abstract field to identify follow-up clinical studies in BPD samples. We examined the references of all included articles to identify other relevant publications and contacted authors to obtain additional information. Dissertations and conference papers were also reviewed.
2.2. Selection criteria
Inclusion criteria were: (1) the presence of an adult BPD sample or subsample in the study, diagnosed by a validated, semi-structured interview; (2) at least two assessments with repeated outcome measures related to the course of BPD; and (3) a follow-up period of 5 years or more.
2.3. Data collection
Data extraction of the selected studies was independently completed by two investigators using an agreed coding protocol (available upon request). The authors of three studies were contacted to request additional information. A response was obtained from a study pending publication, which was included in the meta-analyses. The level of agreement between the coders was high (average agreement percentage = 95.53; average Kappa =.91).
2.4. Outcome variables
The comparable measures reported by at least three studies were considered as the minimum measures needed to successfully perform a meta-analysis, finally resulting in four outcomes of interest: remission, completed suicide, depression, and functioning.
As a measure of remission, the percentage of subjects who achieved diagnostic remission for BPD at a specific follow-up point was used; this measure differs from the cumulative remission rate, which is defined as the percentage of subjects who achieved a particular period of remission throughout the duration of the follow-up. Completed suicide was computed as the number of subjects who completed suicide during follow-up divided by the total number of subjects included at baseline in the respective study.
Depression and functioning were studied through the means of diverse instruments used in the studies. Their comparability was determined by consensus of the authors.
2.5. Definition of moderators
The potential factors reported by at least three studies were considered as moderators; age at baseline, gender, time of follow-up, comorbidity with mood disorders at baseline, initial level of functioning, presence and type of controlled treatment and its length in months, and total hours of therapy were studied.
As a measure of the initial level of functioning, we converted the mean scores of the functioning scales at baseline into a z-score, comparing the mean values in each study with those reported for these instruments in clinical populations from the corresponding countries, which mainly consisted of outpatients with anxiety or affective disorders [Reference Bobes, González, Bascarán, Corominas, Adan and Sánchez25, Reference Greenberg and Rosenheck26, Reference Pedersen, Kvarstein and Wilberg27, Reference Suominen, Salminen, Lähteenmäki, Tupala and Isometsä28, Reference Tungström, Söderberg and Armelius29, Reference Tyrer, Nur, Crawford, Karlsen, MacLean and Rao30].
Regarding treatment, we analysed the impact of receiving a controlled treatment at the outset of the follow-up, comparing samples of naturalistic studies with those of follow-up clinical trials. Any treatment received in experimental conditions (e.g., predetermined prescription or length of treatment, attendance monitoring, etc.) was considered as a controlled treatment. Secondly, we compared those subgroups receiving specialised therapy for BPD or other personality disorders with those receiving TAU in follow-up clinical studies. Finally, we studied the length of the controlled treatment in these subgroups and, where possible, the total hours of formal therapy received, including both individual and group modalities. To this end, we calculated the total amount of hours of formal therapy, multiplying the number of therapy sessions by the hours per session.
2.6. Quality assessment
A quality assessment of studies was performed with the SAQOR, which was developed to assess quality in psychiatric research [Reference Ross, Grigoriadis, Mamisashvili, Koren, Steiner and Dennis31]. We followed the adapted guidelines used to assess both intervention and longitudinal studies in a former meta-analysis [Reference Betancourt, Borisova, Williams, Meyers-Ohki, Rubin-Smith and Annan32]. According to the purpose of the present review, quality was assessed considering the presence of BPD diagnosis as the exposure variable, regardless of the original design or aims of the studies. Gender/age, psychiatric comorbidity, type of initial treatment, amount of therapy during the follow-up, and other variables were considered among factors that might affect the association between BPD diagnosis and the long-term outcome. The control group domain was not applied, since the results of these samples were not analysed. The final SAQOR ratings were modified to maintain a similar sensitivity of the scale (see Table 1). Two of the authors completed the ratings, with an 89% average interrater agreement in domains’ scores (average Kappa =.78) and an 82% in final ratings (Kappa =.63).
2.7. Meta-analyses
2.7.1. Effect size computation
For remission and completed suicide, the event rate itself was treated as a measure of effect size; event rates were converted into percentages. In the study of depression and functioning, the effect size used was Hedges’ unbiased g standardised mean difference and was calculated by subtracting the mean scores at baseline from the mean at the follow-up, divided by the standard deviation within groups [Reference Borenstein, Hedges, Higgins and Rothstein33]. Since test-retest information is used to adjust the standard errors of the effect size estimates, we used test-retest correlation coefficients of 0.50,.60 and,.70 (presented here are those results based on a correlation of.50; the remaining analyses may be obtained upon request, but no substantial differences were found). Hedges’ g was computed in such a way that positive values indicate more of a particular outcome (i.e., more depression and more functioning).
2.7.2. Meta-analytic procedures
We ran four separate meta-analyses, one for each outcome variable of interest (i.e., remission, completed suicide, depression, and functioning). The likelihood of publication bias was tested using the Egger’s regression test [Reference Egger, Smith, Schneider and Minder34] in those meta-analyses with at least ten of the studies (i.e., remission and suicide) and the trim-and-fill procedure [Reference Duval and Tweedie35] in the remaining number [Reference Sterne, Sutton, Ioannidis, Terrin, Jones and Lau36].
To determine whether each set of independent estimates shared a common effect size, we computed the homogeneity Q statistic and the I2 index (i.e., the estimated percentage of the total amount of variability that can be attributed to heterogeneity) [Reference Hedges and Olkin37, Reference Higgins and Thompson38]. Since heterogeneity was observed in three of the four meta-analyses, effect sizes were combined under the random-effects model using the restricted maximum-likelihood estimation to estimate the amount of heterogeneity [Reference Viechtbauer39]. We obtained an estimate of the overall effect size (i.e., event rate or Hedges’ g) for each outcome of interest, which was also tested by computing a 95% confidence interval (CI) and the associated p value.
To examine the relationship between the moderators and the effect sizes, a mixed-effects model was used (i.e., random-effects model with moderators), using restricted maximum-likelihood to estimate residual heterogeneity. For quantitative moderators, we report the estimated parameter, its 95% CI, the QM (i.e., heterogeneity accounted for by the moderator), and the associated p value. For categorical variables, we report the estimated effect sizes within each level of a moderator with the corresponding 95% CI, and the QB and its statistical significance. Analyses were conducted with the Comprehensive Meta-Analysis (CMA) software [Reference Borenstein and Rothstein40].
3. Results
3.1. Description of studies
A total of 1718 records were identified through database searching and other sources. Fig. 1 describes the flow chart of the selection process. After removing duplicates, 769 records were screened that fulfilled inclusion criteria. Reasons for exclusion were: the design of the study was not prospective, the absence of a specified BPD sample, the lack of repeated outcome measures, and a follow-up period that did not course entirely through adulthood or was shorter than five years. Finally, twenty full-text articles corresponding to eleven prospective studies were selected and included in at least a meta-analysis.
Table 1 describes the studies included in the meta-analyses and the outcome variables which were analysed from each of them. There were five clinical trials with long-term post-treatment follow-ups and six naturalistic studies without a controlled treatment phase. The methodological qualities of the studies are displayed in Table 1. The time from baseline to follow-up ranged from five to fourteen years, with a median value of six years. Overall, 837 participants from nine countries completed both assessments. The majority of studies showed a retention rate of more than 60 percent, with the exception of the naturalistic study with a fourteen-year follow-up [Reference Zeitler, Bohus, Kleindienst, Knies, Ostermann and Schmahl13]. Mean ages at baseline oscillated between 27 and 35 years, and the percentages of women were between 47% and 100%. Percentages of comorbidity with mood disorders at baseline fluctuated between 37.7% and 100%; this last percentage was due to one study conducted in a sample of primary care patients diagnosed with both major depressive disorder and BPD [Reference Riihimäki, Vuorilehto and Isometsä12]. Recruitment settings in the rest of studies were outpatient or inpatient psychiatric services.
3.1.1. Measures of outcome
Selected studies reported follow-up data in several areas, i.e., the presence of BPD diagnosis and BPD symptomatic domains, dimensional personality traits, Axis II and Axis I comorbidity, general psychopathology, depression, anxiety, interpersonal problems, suicidal behaviour, psychosocial and global functioning, and quality of life. We only found comparable data for the four outcomes analysed (see Table 1).
Regarding remission, the CLPS was excluded from the meta-analysis due to its reporting of cumulative remission rates [Reference Gunderson, Stout, McGlashan, Shea, Morey and Grilo9]. Aside from this type of measure, the MSAD also reported a specific remission rate at a six-year follow-up that was considered in the analyses [Reference Zanarini, Frankenburg, Hennen and Silk49]. The presence/absence of BPD diagnosis was generally assessed by similar instruments at baseline and follow-up, with the exception of two studies [Reference Zeitler, Bohus, Kleindienst, Knies, Ostermann and Schmahl13, Reference Bateman and Fonagy20].
Table 1 Description of studies included in the meta-analyses (N = 837).

Note. CT = Controlled Treatment; TAU = Treatment as usual; DIB = Diagnostic Interview for Borderline Patients; DIB-R = Revised Diagnostic Interview for Borderlines; DIBD-R = Diagnostic Interview for DSM-III-R Personality Disorders; DIPD-IV = Diagnostic interview for DSM-IV Personality Disorders; DIP-I = DSM-IV and ICD-10 Personality Disorders Interview; SCID = Structured Clinical Interview for DSM-III-R; SCID-II = Structured Clinical Interview for DSM-IV-Axis II; ZAN-BPD = Zanarini Rating Scale for Borderline Personality Disorder; IPDE = International Personality Disorder Examination; BDI = Beck Depression Inventory; BDI-II = Beck Depression Inventory-II; 17-HDRS = 17-item Hamilton Depression Rating Scale; SFQ = Social Functioning Questionnaire; GAF = Global Assessment of Functioning; WSAS = Work and Social Adjustment Scale; SOFAS = Social and Occupational Functioning Assessment Scale; SASS = Social Adaptation Self-evaluation Scale. a SAQOR ratings: High = 5-4 Adequate domains; Moderate = 3-2 Adequate domains; Low ≤ 1 Adequate domain; b Waiting list control group was present in the original trial, although follow-up data was not reported for this group; cn = 15 for remission outcome variable; d Initial n used to intent-to-treat analyses for depression,n at follow-up used for remission; eIntent-to-treat sample; f GAF scores only reported at baseline in these studies.
Depressive symptoms were evaluated by the Beck Depression Inventory (BDI or BDI-II) and the 17-item Hamilton Rating Scale for Depression (HRSD-17). The Dysphoric Affect Scale (DAS) was used by the MSAD and was not considered comparable to the BDI/BDI-II and HRSD-17 due to the fact that this instrument identifies other dysphoric states apart from depression [Reference Reed, Fitzmaurice and Zanarini51].
A variety of instruments were used as a measure of functioning, including (a) scales rated by clinicians: the Global Assessment of Functioning (GAF) and the Social and Occupational Functioning Assessment Scale (SOFAS), and (b) self-report questionnaires: the Social Functioning Questionnaire (SFQ), the Work and Social Adjustment Scale (WSAS), and the Social Adjustment Scale-Self-Report (SASS). Results on GAF scores were partially reported by three studies and were not analysed [Reference Gunderson, Stout, McGlashan, Shea, Morey and Grilo9, Reference Bateman and Fonagy20, Reference Zanarini, Frankenburg, Hennen and Silk49]. Besides, the MSAD was also excluded due to reporting specific indexes of psychosocial functioning [Reference Zanarini, Frankenburg, Hennen, Reich and Silk8, Reference Zanarini, Frankenburg, Reich and Fitzmaurice52].
3.1.2. Treatment interventions
Table 2 illustrates the controlled treatment conditions compared in the follow-up clinical trials included in the meta-analyses. Controlled treatments lasted for one to three years and were mainly conducted in outpatient settings, with the exception of two groups who received a combination of day hospital and outpatient treatment [Reference Antonsen, Kvarstein and Urnes19, Reference Bateman and Fonagy20]. The hours of formal therapy fluctuated between 60 and over 600 h, the latter reported by the MBT trial [Reference Bateman and Fonagy20].
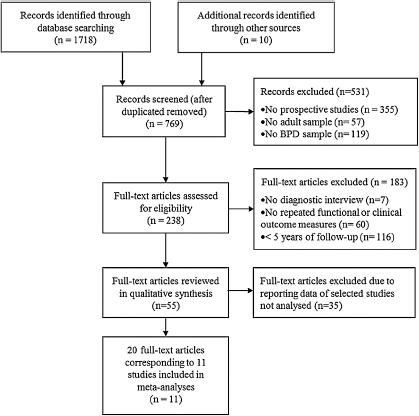
Fig. 1. Flow chart of selection process.
Among naturalistic studies, two studies followed up samples who initially participated in a clinical trial, although treatment subgroups were not individually studied at follow-up [Reference Alvarez-Tomás, Soler, Bados, Martín-Blanco, Elices and Carmona10, Reference Zeitler, Bohus, Kleindienst, Knies, Ostermann and Schmahl13]. Besides, three naturalistic studies informed of treatment use during follow-up in general terms. The CLPS and MSAD studies reported similar percentages of subjects in BPD samples who participated in individual therapy during the early years of follow-up, which tended to decrease over time (range, 85%-64% and 96%-75%, respectively) [Reference Bender, Skodol, Pagano, Dyck, Grilo and Shea53, Reference Zanarini, Frankenburg, Hennen and Silk54]. Álvarez-Tomás et al. also reported that 75% of subjects received individual therapy over the 10-year period [Reference Alvarez-Tomás, Soler, Bados, Martín-Blanco, Elices and Carmona10].
3.2. Meta-analytic results
There was no evidence for publication biases with respect to the four outcome measures studied in meta-analyses, according to the results of the Egger´s regression test (Remission, t = 0.41, df = 10, p =.69; Completed suicide, t = 1.98, df = 8, p =.08) and the trim and fill method (no study trimmed for depression and functioning).
3.2.1. Remission
Nine studies were analysed for remission, corresponding to twelve comparisons. The mean remission rate was 60% (49–71, 95% IC), although remission rates showed high heterogeneity among studies (Q = 57.9, p <.001; I2 = 80.9%). The percentages of remission in each study are displayed in Table 1.
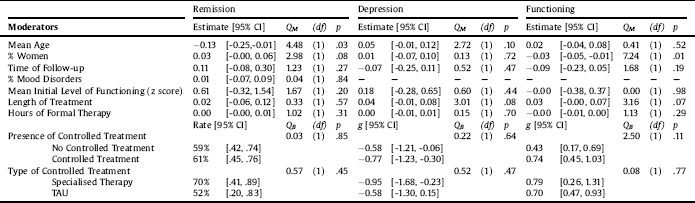
The results of the effects of moderators are summarised in Table 3. Groups with a younger mean age at baseline were more likely to show higher remission rates at follow-up (QM = 4.48, p =.03). Greater percentages of women in the samples were associated with higher remission rates in the long-term, although this tendency did not reach statistical significance (QM = 2.98, p =.08). Time of follow-up, percentage of comorbidity with mood disorders at baseline, and initial level of functioning did not demonstrate a significant influence on long-term remission. No significant differences in mean remission rates were observed between groups receiving and not receiving an initial controlled treatment, i.e., clinical trials vs naturalistic studies (61% vs. 59%). Among clinical trials, the mean remission rate in groups receiving a specialised therapy was higher than in those receiving TAU (70% vs. 52%), although this difference was not statistically significant. No relevant impact of the length of treatment or the hours of formal therapy received was found.
3.2.2. Completed suicide
Seven studies were considered for completed suicide, which represented ten comparisons. The mean suicide rate was 4% (2–5, 95% CI); the values were homogeneous among studies (Q = 8.68, p =.47; I2 =.0%). The percentages of completed suicide in the studies ranged from 0% to 8%, as shown in Table 1. Due to the low heterogeneity presented among studies, the effects of moderators were not studied on this outcome variable.
3.2.3. Depression
Four studies were studied for depression, comprising six comparisons. Meta-analytic results showed a significant reduction in depressive symptoms at follow-up, indicated by a medium mean effect size (g = -0.70, [-1.04, -0.36] 95% CI, p <.001). However, there was high heterogeneity among the studies (Q = 23.40, p <.001; I2 = 78.6%).
The percentage of comorbidity with mood disorders at baseline was not studied as a moderator on depression because there were no data from at least three studies. No relevant impact of moderators on depression was found, except for the length of treatment. Longer treatments were associated with increased improvement in depression over time, although this trend did not reach statistical significance (QM = 3.01, p =.08).
Table 2 Description of controlled treatment conditions in follow-up clinical studies.
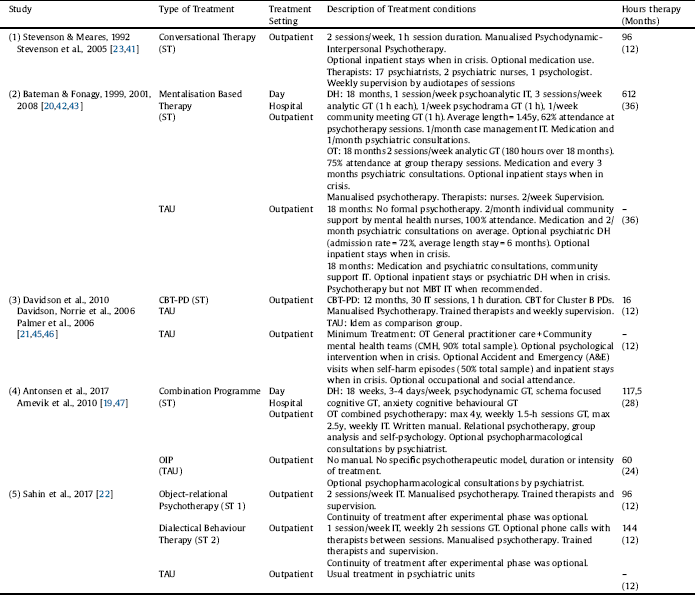
Note. ST = Specialised Therapy; TAU = Treatment as usual; CBT-PD = Cognitive Behavioural Therapy – Personality Disorders; OIP = Outpatient Individual Therapy; DH = Day Hospital; OT = Outpatient Treatment; GT = Group Therapy; IT = Individual Therapy. Community support by health professionals was not considered as formal therapy. When duration of sessions was not informed, it was computed 1 h per session. Real over planned data on use of therapy was preferred for calculations.
3.2.4. Functioning
Five studies were synthesised for functioning, which represented nine comparisons. A significant improvement in long-term functioning was also found, with a medium mean effect size (g = 0.66, [0.43, 0.89] 95% IC, p <.001). However, there was high heterogeneity among studies (Q = 25.54, p =.001; I2 = 68.7%).
Groups with a higher percentage of women were more likely to present lower improvement in functioning at follow-up (QM = 7.24, p =.007); age at baseline, time of follow-up, and initial level of functioning showed no relevant impact on long-term functioning. The initial rate of comorbidity with mood disorders was also not studied for functioning because there were no data from at least three studies. Differences in functional improvement between groups from naturalistic studies and those from clinical trials receiving a controlled treatment were not significant, although the latter showed a greater estimated effect size (g = 0.43 vs. g = 0.74, p =.11). In clinical trials, receiving specialised therapies or TAU did not show a relevant impact on functional change. There was a non-significant relationship between longer treatments and higher functional improvement (QM = 3.16, p =.07), whereas the hours of formal therapy received did not have a relevant influence on functioning.
4. Discussion
This meta-analytic study synthesised current findings from prospective research on the long-term course of BPD in adulthood. In terms of mean remission rates, it is estimated that between 50% and 70% of patients diagnosed with BPD may achieve symptomatic remission at some point between five and fifteen years of follow-up; this finding is consistent with former literature indicating that BPD diagnosis leans towards increasing proportions of remission over time. The Montreal study retrospectively reported that 75% of patients with BPD achieved remission at fifteen years and over 90% did so at 27 years of follow-up [Reference Paris2]. Both the MSAD and CLPS studies also provided evidence for an enduring symptomatic remission of BPD, despite reporting cumulative rates of remission [Reference Zanarini6]. To our knowledge, our study is the first meta-analysis reporting estimated remission rates prospectively assessed at a specific point, which may be useful in comparing the long-term effects of treatments for BPD patients over the course of the disorder.
Table 3 Results of the effects of moderators on remission, depression, and functioning.
Notably, depressive symptomatology and functioning in patients with BPD also lean towards improvement in the long-term. Findings are consistent with those reported by the CLPS and MSAD studies, indicating that the psychosocial functioning of BPD subjects may vary among individuals, but show a significant improvement over time as a group [Reference Zanarini6]. However, our results do not allow one to conclude whether individuals with BPD can reach normative functional adjustment in the long-term, although previous research indicates that a relevant proportion may suffer from persistent impairments over time [Reference Zanarini, Frankenburg, Hennen, Reich and Silk8, Reference Gunderson, Stout, McGlashan, Shea, Morey and Grilo9, Reference Alvarez-Tomás, Soler, Bados, Martín-Blanco, Elices and Carmona10, Reference Zeitler, Bohus, Kleindienst, Knies, Ostermann and Schmahl13, Reference Zanarini, Frankenburg, Reich and Fitzmaurice52]. In terms of depressive symptoms, the MSAD study also reported a significant decrease in dysphoric states in the long-term, which was more pronounced in recovered patients [Reference Reed, Fitzmaurice and Zanarini51]. Despite this favourable outcome in clinical and functional realms, we found that the rate of completed suicide in BPD subjects might be expected to be between 2% and 5% during the second half of the decade of follow-up; percentages were lower than those based on previous follow-back research at fifteen and 27 years, which were between 8% and 10%. This fact is consistent with the hypothesis that completions are more likely to occur later in the course of the illness [Reference Biskin1, Reference Paris2].
We further investigated potential moderators for those outcomes which presented high heterogeneity in the meta-analyses. Regarding patients’ age at baseline, we found that a diagnosis of BPD at a younger age was associated with higher percentages of remission in the long-term, whereas this moderator did not influence changes in depression and functioning. This is congruent with previous evidence indicating that BPD symptom severity may decline from adolescence to mid-adulthood, particularly in terms of the externalising manifestations of the disorder (i.e., impulsivity and suicidal behaviours) [Reference Blum, Franklin, Hansel, McCormick, St.John and Pfohl55, Reference Frías, Palma, Solves, Martínez and Salvador56, Reference Morgan, Chelminski, Young, Dalrymple and Zimmerman57, Reference Stepp and Pilkonis58]. Younger age has also been identified as a predictor of shorter time to remission [Reference Zanarini, Frankenburg, Hennen, Reich and Silk14]. In contrast, the CLPS informed of similar rates of improvement in BPD symptoms in younger and older subjects over six years of follow-up [Reference Shea, Edelen, Pinto, Yen, Gunderson and Skodol15]. This discrepancy in longitudinal findings suggests that age-related divergences might also be influenced by the duration of the illness, which is expected to be longer the older one becomes but with variations among subjects. Similarly, it would be useful to consider the age of onset and the duration of illness as specific moderators when studying the course of the disorder. In terms of functioning, cross-sectional research has reported, contrary to our findings, greater functional impairments in older age, when it is more likely to present worse physical health, poorer quality of life, and greater social assistance utilisation [Reference Frías, Palma, Solves, Martínez and Salvador56, Reference Morgan, Chelminski, Young, Dalrymple and Zimmerman57, Reference Stepp and Pilkonis58]. Nevertheless, this decline in functioning is more dramatically suffered in advanced age, whereas subjects comprising the study samples in our analysis were mostly in their 20 s and 30 s at baseline. Consistent with this hypothesis, the CLPS study reported that older participants only showed a higher decline in functioning midway through the follow-up [Reference Shea, Edelen, Pinto, Yen, Gunderson and Skodol15].
A striking finding was that female gender was associated with a lower improvement in functioning, whereas there were no significant differences in gender with regard to changes in BPD diagnosis and depression in the long-term. These results are consistent with those informed by the MSAD, which did not report a significant impact of gender on time to remission over ten years [Reference Zanarini, Frankenburg, Hennen, Reich and Silk14]. Unfortunately, there is scarce evidence on gender differences regarding the functional course of BPD. In this respect, our findings indicate that the long-term functional recovery in women with BPD might be hampered by other causes apart from the persistence of the disorder. A possible explanation is that psychopathological divergences between genders in symptom severity and comorbidity might deeply interfere with the long-term functional outcome of BPD women, in spite of showing similar trends of clinical improvement over time. In this line, there is evidence from cross-sectional research on gender differences that female BPD subjects present greater percentages of lifetime Axis I comorbidity and higher severity in general psychopathology, particularly in areas related to internalising patterns such as anxiety, depression, and somatisation [Reference Bayes and Parker59, Reference Silberschmidt, Lee, Zanarini and Schulz60]. Additionally, BPD women are more likely to have a history of childhood sexual abuse and experience episodes of physical and sexual aggression during adulthood, which is related to higher psychosocial impairment [Reference Bayes and Parker59, Reference de Aquino Ferreira, Queiroz Pereira and Neri Benevides61]. On the other hand, sociological studies have noted that gender roles determine different strains and benefits of normative social adaptation for men and women, which might also contribute to hindering psychosocial adjustment in female BPD subjects; for example, caregiving roles for women in the general population are associated with greater psychological distress and increased reductions in the protective benefits of employment for mental health, reporting higher rates of exposure to stressful life events involving significant others [Reference Hatch and Dohrenwend62, Reference Depression63].
Receiving an initial controlled treatment does not seem to increase the amount of clinical improvement in the long-term compared to the course of the disorder described in naturalistic studies. Besides, both specialised therapies and TAU seem to similarly improve the long-term clinical outcome, despite observing non-significant differences in mean remission rates between those groups. This contrasts with previous research indicating a higher efficacy of specialised therapies for BPD in the short-term [Reference Cristea, Gentili, Cotet, Palomba, Barbui and Cuijpers64, Reference Stoffers, Völlm, Rücker, Timmer, Huband and Lieb65], which suggests that the differential effects of psychotherapeutic interventions might be diluted by the diverse mechanisms of change over the lifespan. On the other hand, the long-term functioning of BPD patients appears to be enhanced by any kind of controlled treatment, particularly those that are implemented over a longer period of time, although these trends did not reach statistical significance in our analyses. This might indicate that common components of psychotherapies are key factors in promoting changes in psychosocial functioning in the long-term [Reference Sinnaeve, van den Bosch and van Steenbergen-Weijenburg66]. One aspect to note is that the methodological limitations of the selected studies may affect these results on treatment moderators. First, other confounding factors are likely to interfere with treatment efficacy in long-lasting post-treatment follow-ups, including the likelihood of receiving further treatment after the experimental phase. Secondly, most BPD subjects in naturalistic studies might also have received some form of uncontrolled treatment during the follow-up period [Reference Paris2, Reference Cristea, Gentili, Cotet, Palomba, Barbui and Cuijpers64].
The length of follow-up was not relevant to explain the variations in the outcomes, suggesting a low pace of change in the long-term. This differs from the early years of illness when more dramatic shifts in BPD symptoms may occur [Reference Biskin1, Reference Zanarini, Frankenburg, Hennen, Reich and Silk14]. Additionally, no significant effects of the initial level of functioning and the percentage of comorbid mood disorders were found; this contrasts with findings from the CLPS indicating that a comorbid major depressive disorder is associated with a delayed time to remission from BPD, likely due to differences in the operationalisation of remission in this study [Reference Gunderson, Stout, Shea, Grilo, Markowitz and Morey16].
There are strengths and limitations of this meta-analysis to consider. We included follow-along studies conducted in a variety of clinical settings and countries, which increases the generalisation of the findings. We also analysed the impact of several factors on the heterogeneity of the outcomes; however, the majority of selected studies reported results at follow-up lasting between five and ten years, largely restricting the scope of our findings to this time period. In general, the scarcity of selected studies and the small size of the BPD samples in most of them reduced the statistical power of the analyses and therefore may have affected the study of the effects of moderators. Additionally, the lack of data or the variability of measures used among studies restricted the analysis of other potential moderators and outcomes. Finally, we studied correlational relationships between moderators and long-term outcomes and, therefore, we cannot establish causal links based on our findings.
5. Conclusion
Our findings confirm a pattern of clinical and functional improvement over time in patients diagnosed with BPD. It is tempting to think about the beneficial effects of psychotherapeutic interventions, specialised or not, on the functional long-term course, but further research on the long-term effects of psychotherapies is required to reach consistent conclusions in this regard. Moreover, longitudinal studies in untreated samples might also enrich our knowledge of the natural course of BPD and the study of treatment efficacy. In general, the consistent use of clinical and functional measures for BPD would facilitate meta-analytic research in this field.
Our results lead to the conclusion that BPD diagnosis at a younger age corresponds to a better clinical prognosis in the long-term, whereas similar rates of functional improvement are achieved by age over time. This justifies direct efforts towards the early detection of BPD, allowing the implementation of effective treatments during patients’ youth to reduce the adverse effects of the disorder during this critical life stage. In addition, functional improvement in the long-term is hampered in women with BPD; accordingly, it is essential to incorporate a gender perspective to address psychosocial interventions for these patients, particularly due to the higher percentage of women among treatment-seekers with BPD diagnosis. Moreover, the use of study designs that allow gender comparisons would be recommended.
Financial support
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Disclosure of interest
The authors declare that they have no competing interests.







Comments
No Comments have been published for this article.