In randomised controlled trials (RCTs) exposure reduced fear more than did relaxation, and clinician-accompanied exposure appeared redundant (Reference MarksMarks, 1987; Reference Al-Kubaisy, Marks and LogsdailAl-Kubaisy et al, 1992). An important question is whether gains continue for years after treatment has ended, because the patients in the RCTs usually have been very chronic (Reference Noyes, Holt, Woodman, Mavissakalian and PrienNoyes et al, 1996). In several studies improvement did continue for years after clinician- accompanied exposure and/or exposure plus cognitive therapy (panic disorder: Reference O'Rourke, Fahy and BrophyO'Rourke et al, 1996; agoraphobia: Reference Lelliott, Marks and MonteiroLelliott et al, 1987; Reference Fava, Rafanelli and GrandiFava et al, 2001a ; social phobia: Reference Juster and HeimbergJuster & Heimberg, 1995; Reference Fava, Grandi and RafanelliFava et al, 2001b ; specific phobia: Reference ÖstÖst, 1989; obsessive—compulsive disorder: Reference O'Sullivan, Noshirvani and MarksO'Sullivan et al, 1991). Only Fava et al examined self-exposure alone. We report the status of Al-Kubaisy et al's (Reference Al-Kubaisy, Marks and Logsdail1992) patients 2 years after the end of the original RCT to determine how outcome at 2 years after self-exposure compared with that after clinician-accompanied self-exposure.
METHOD
Patient sample
Two-year post-treatment follow-up was achieved in 68 (85%) out of 80 psychiatric out-patients who had completed a 14-week RCT (Reference Al-Kubaisy, Marks and LogsdailAl-Kubaisy et al, 1992). Before treatment, all had a disabling (target phobia total score > 20 on a 0-32 scale) phobic disorder by ICD-10 (World Health Organization, 1992) criteria (16 with agoraphobia, 22 social phobia, 30 specific phobias) for at least 1 year (mean duration=18 years; s.d.=11). Mean age was 35 years (s.d.=11) and 25 (37%) were men.
Design
Details of the RCT are reported by Al-Kubaisy et al (Reference Al-Kubaisy, Marks and Logsdail1992). Patients were randomised to one of three treatment conditions: clinician-accompanied self-exposure (Ee); self-exposure only (e); and self-relaxation (r). During weeks 0-8, all patients had six 60-min sessions with a clinician. The Ee sessions totalled 150 min to include an extra 90 min doing clinician-accompanied live exposure. At week 14, exposure therapy was offered to patients who had not improved (mean target fear reduction <2 on 0-8 scale) after self-relaxation; acceptors were crossed over to have Ee or e (r→Ee/r→e). The r patients who did not cross over are called r-only hereafter.
Two years after the end of treatment, patients were invited by letter to attend for assessment; those who did not attend were posted outcome scales to rate and return.
Measures
At weeks 0, 8, 14 and 26 after study entry, patients had self- and independent assessor ratings (higher scores=more severe symptoms) using the following measures: the target phobias (Reference Watson and MarksWatson & Marks, 1971) (each patient negotiated with the therapist individualised targets (usually three or four) of exposure homework): fear and avoidance (each with mean range 0-8); the Fear Questionnaire (FQ; Marks & Mathews, 1979), containing 15-item total phobia (FQT; total score range 0-120), single-item global phobia severity (0-8) and single-item depression (0-8) subscores (Reference McKenzie and MarksMcKenzie & Marks, 1999); the Beck Depression Inventory (BDI: 0-52; Reference Beck, Rial and RickelsBeck et al, 1974); and the Work, Home Management, Social and Private Leisure Adjustment scale (four-item WSA: 0-32; Reference MarksMarks, 1986).
At 2 years' post-treatment, patients were asked to rate the above according to satisfaction with treatment during weeks 0-14 and any subsequent treatment, and treatment success: ‘Success’ (0-8: 0-2 failure, 3-5 moderate success, 6-8 marked success); ‘Improved as much as expected?’ (0-8: 0-2 less than expected, 3-5 about what was expected, 6-8 more than expected); ‘Needed further treatment (and which) for your phobia and/or other psychological problems?’; and ‘Choose same treatment again if need further help?’
Statistical analysis
Only self-rated measures were analysed because assessor-rated measures were unavailable for patients who did not attend follow-up and so could be biased. Self- and assessor-rated measures had correlated highly at baseline and week 14. Pearson's correlation coefficients were 0.65-0.93 (n=66-75, P<0.001) on the target phobias and on the WSA, and for the self-rated BDI v. assessor-rated Hamilton Rating Scale for Depression (Reference HamiltonHamilton, 1960). Because at weeks 8 and 14 the three treatment conditions had differed similarly regardless of type of phobia (Reference Al-Kubaisy, Marks and LogsdailAl-Kubaisy et al, 1992), the three types of phobia were pooled for analysis of inter-treatment differences at 2 years. Data from r→Ee/r→e patients were pooled to boost cell size, a further rationale being the absence of significant differences between Ee and e at 2 years (see below).
Clinical ratings were tested by repeated-measures analysis of variance (ANOVAs) in each treatment group. Paired t-tests were used as a post hoc analysis with reference points of weeks 0, 8 and 14. Group comparison on symptom severity is valid for Ee v. e because r patients were not assigned randomly to r-only or r→Ee/r→e after week 14. Two-way ANOVAs were used to test the influence of compliance or co-therapist on the outcome of Ee and e. The χ2 and Fisher's exact test were used for categorical data. All statistical tests were two-tailed and the significance level was set at P<0.05.
RESULTS
Patients followed up (rated) at 2 years v. non-followed-up (unrated) patients
At pretreatment, the 68 patients with 2-year ratings, compared with the unrated 12 patients, had similar demographic and clinical features, including symptom severity, but more rated patients had been employed (82% v. 50%; χ2 (1)=5.96, P=0.015).
At 2 years, numbers from each of the original treatment conditions were (numbers at week 14 in italic): Ee 25 (27); e 23 (26); r-only 10 (15). Numbers from the crossover conditions were r→Ee 3 (4) and r→e 7 (8); more r-only patients had been followed up (33% v. 11%, P=0.043).
Patients with follow-up had improved more than the non-followed-up patients during weeks 0-8 on all measures except FQT, with a week 0-8 mean fall in: target fear, 2.8 v. 1.1 (t(78)=2.48, P=0.015); target avoidance, 3.4 v. 0.9 (t(78)=3.56, P=0.001); global phobia severity, 2.3 v. 0.4 (t(78)=2.87, P=0.005); WSA total, 5.4 v. 1.2 (t(74)=2.10, P=0.039); single-item depression, 4.7 v. ‒2.1 (t(78)=2.87, P=0.017); and BDI, 1.9 v. ‒0.9 (t(77)=2.28, P=0.025).
Outcome on clinical ratings over 2 years
Of all the patients, 91% identified three (26%) or four (65%) most fearful situations or activities as treatment targets (9% had very specific phobias). The mean total amount of self-exposure homework set was 75 h in Ee and 79 h in e; the mean total amount actually done by patients was 59 h in Ee and 52 h in e. Clinical ratings at weeks 0, 8 and 14 post-entry and 2 years after treatment ended appear in Fig. 1 and Table 1.
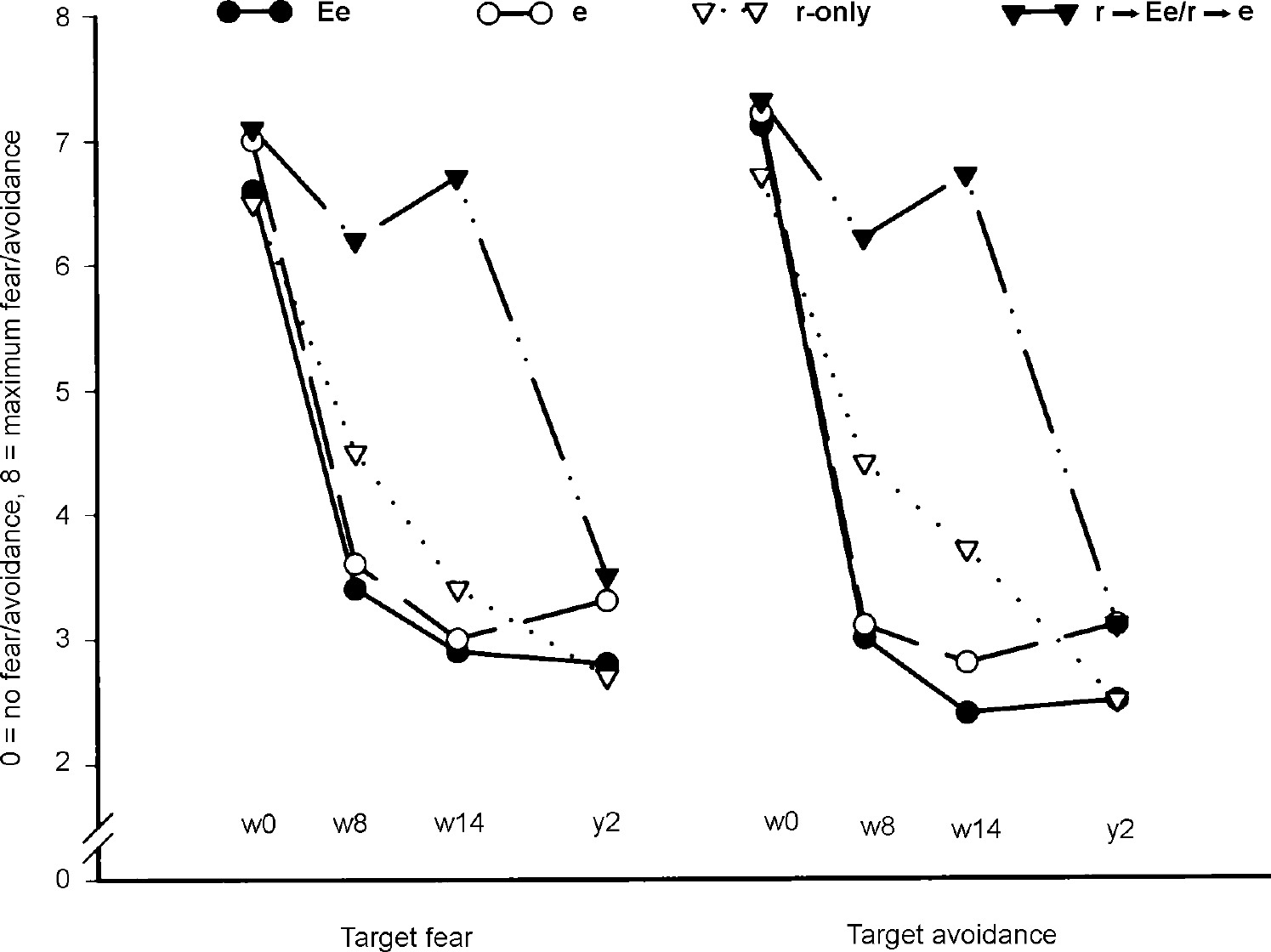
Fig. 1 Outcomes on target fear and avoidance raw scores: Ee, clinician-accompanied self-exposure; e, self-exposure; r-only, self-relaxation; r→Ee/r→d, self-relaxation then crossed over to Ee or e at week 14.
Table 1 Overall outcomes on clinical measures: raw scores
| Week 0 | Week 8 | Week 14 | Two years | Repeated measures ANOVA for each group | ||||
|---|---|---|---|---|---|---|---|---|
| n | n (s.d.) | n (s.d.) | n (s.d.) | n (s.d.) | d.f. | F | P | |
| Mean target fear | ||||||||
| Ee | 25 | 6.6 (1.0) | 3.4 (2.0)* | 2.9 (2.0)* | 2.8 (1.9)* | 3,72 | 55.45 | <0.001 |
| e | 23 | 7.0 (0.8) | 3.6 (2.2)* | 3.0 (2.3)* | 3.3 (2.4)* | 3,66 | 30.98 | <0.001 |
| r-only | 10 | 6.5 (0.9) | 4.5 (2.0)* | 3.4 (1.7)* | 2.7 (1.8)* | 3,27 | 10.99 | <0.001 |
| r→Er/r→e | 10 | 7.1 (0.7) | 6.2 (1.5)* | 6.7 (1.2) | 3.5 (2.3)*,†,‡ | 3,27 | 13.79 | <0.001 |
| Mean target avoidance | ||||||||
| EE | 25 | 7.1 (0.9) | 3.0 (2.3)* | 2.4 (1.8)* | 2.5 (1.8)* | 3,72 | 68.70 | <0.001 |
| e | 23 | 7.2 (0.6) | 3.1 (2.4)* | 2.8 (2.3)* | 3.1 (2.4)* | 3,66 | 44.01 | <0.001 |
| r-only | 10 | 6.7 (1.1) | 4.4 (1.8)* | 3.7 (1.8)* | 2.5 (1.6)*,† | 3,27 | 16.78 | <0.001 |
| r→ee/r→e | 10 | 7.3 (0.8) | 6.2 (1.7) | 6.7 (1.1)* | 3.1 (2.2)*,†,‡ | 3,27 | 21.00 | <0.001 |
| FQ total | ||||||||
| Ee | 22 | 42.5 (23.4) | 24.1 (16.2)* | 21.8 (18.6)* | 21.9 (23.2)* | 3,63 | 17.62 | <0.001 |
| e | 20 | 34.1 (23.2) | 26.1 (23.7)* | 22.7 (22.3)* | 22.9 (21.7)* | 3,57 | 7.42 | <0.001 |
| r-only | 9 | 49.9 (21.2) | 38.6 (22.1) | 29.8 (19.2)* | 29.9 (18.1)*,† | 3,24 | 8.17 | 0.001 |
| r→Ee/r→e | 9 | 30.9 (21.1) | 29.8 (21.8) | 29.4 (25.3) | 29.4 (20.2) | 3,24 | 0.026 | 0.994 |
| FQ depression | ||||||||
| Ee | 22 | 16.9 (10.0) | 10.4 (7.1)* | 9.3 (6.7)* | 8.9 (9.3)* | 3,63 | 9.85 | <0.001 |
| e | 20 | 15.0 (11.7) | 12.3 (11.3)* | 9.7 (11.2)*,† | 8.5 (9.8)*,† | 3,57 | 10.57 | <0.001 |
| r-only | 8 | 21.0 (9.3) | 12.1 (9.5)* | 10.6 (4.9)* | 10.1 (6.4)* | 3,21 | 9.87 | <0.001 |
| r→Ee/r→e | 9 | 15.3 (11.5) | 14.9 (13.0) | 13.2 (12.4) | 14.6 (11.5) | 3,24 | 0.185 | 0.905 |
| FQ global phobia severity | ||||||||
| Ee | 24 | 6.2 (2.2) | 3.2 (1.6)* | 2.8 (1.6)* | 2.6 (1.8)* | 3,69 | 24.03 | <0.001 |
| e | 23 | 6.6 (1.3) | 4.1 (2.3)* | 3.5 (2.3)*,† | 3.4 (2.2)* | 3,66 | 21.15 | <0.001 |
| r-only | 9 | 6.2 (1.3) | 4.6 (2.1)* | 3.3 (2.2)*,† | 2.7 (2.7)* | 3,24 | 9.10 | 0.001 |
| r→Ee/r→e | 9 | 5.8 (2.2) | 4.4 (1.9)* | 5.4 (1.7)† | 3.1 (1.8)*,†,‡ | 3,24 | 8.73 | <0.001 |
| WSA total | ||||||||
| Ee | 25 | 12.9 (6.7) | 4.8 (3.2)* | 5.5 (6.3)* | 4.4 (4.5)* | 3,72 | 21.08 | <0.001 |
| e | 20 | 10.6 (6.4) | 7.1 (8.3)* | 5.4 (7.8)*,† | 5.1 (5.9)* | 3,57 | 9.95 | <0.001 |
| r-only | 10 | 13.5 (7.9) | 8.9 (6.7)* | 8.5 (5.3)* | 6.1 (6.4)* | 3,27 | 4.98 | 0.007 |
| r→Ee/r→e | 10 | 12.1 (6.2) | 8.9 (4.4) | 11.4 (8.1) | 6.7 (5.4)*,‡ | 3,27 | 2.58 | 0.075 |
| BDI | ||||||||
| Ee | 25 | 7.9 (6.3) | 5.1 (5.4)* | 5.0 (5.8)* | 5.7 (5.8) | 3,72 | 3.64 | 0.017 |
| e | 22 | 7.4 (7.5) | 6.0 (7.0)* | 6.0 (7.8) | 4.8 (5.4)* | 3,63 | 2.79 | 0.048 |
| r-only | 9 | 10.1 (4.3) | 7.9 (3.5)* | 6.2 (3.5)* | 5.6 (4.7)* | 3,24 | 5.51 | 0.005 |
| r→Ee/r→e | 10 | 6.6 (6.2) | 6.6 (5.7) | 9.4 (8.9)* | 8.2 (9.5) | 3,27 | 1.03 | 0.395 |
Six 90-min sessions of clinician-accompanied exposure during weeks 0-8 did not affect the 2-year ratings — interaction between Ee or e and time was not significant on any measure (Table 1). Both Ee and e improved significantly and then remained stable up to 2 years on nearly all measures. The great bulk of improvement had occurred between weeks 0 and 14 (see Table 1) rather than thereafter. From week 0 to 2 years, Ee patients improved by a mean of 58% (s.d.=27) on their target fear, nearly all of this (57%, s.d.=26) having been achieved during weeks 0-14 and almost none thereafter during follow-up. From week 0 to 2 years, e patients improved by a mean of 53% (s.d.=33), all of this having been attained during weeks 0-14 (57%, s.d.=33), with a tiny loss of gain thereafter.
The r-only patients had improved mostly by week 14 (46%, s.d.=29), with slight further gain over the next 2 years (10%, s.d.=28), and overall improvement from week 0 to 2 years was 56% (s.d.=31).
The r→Ee/r→e patients improved on target fear by a mean of merely 7% (s.d.=16) during weeks 0-14 but by 45% (s.d.=43) between week 14 and 2 years; the latter was significant, as was improvement between week 14 and 2 years for target avoidance, global phobia and WSA (see Table 1).
On target avoidance, the Ee patients improved by 65% (s.d.=25) from week 0 to 2 years; 67% (s.d.=23) of the gains had been during weeks 0-14, with little change thereafter. Improvement for e patients was 57% (s.d.=31) from week 0 to 2 years; 60% (s.d.=32) of these gains had been during weeks 0-14 and almost none thereafter. Analysis of variance revealed no difference between Ee and e. Improvement for r-only was 61% (s.d.=28) from week 0 to 2 years, of which 45% (s.d.=24) was during weeks 0-14 and 16% (s.d.=25) thereafter. Group r→Ee/r→e improved by 59% (s.d.=29) from week 0 to 2 years, of which just 10% (s.d.=11) was during relaxation in weeks 0-14 and 49% (s.d.=32) after crossing over to exposure at week 14.
Week 0-8 compliance predicted outcome
The therapist had rated Ee and e patients for between-session compliance with the exposure-homework tasks negotiated during week 0-8 sessions (≥85% of negotiated tasks carried out=complaint, n=15; ≤ 50%=non-compliant, n=12). As in past studies (e.g. Reference de Araujo, Ito and Marksde Araujo et al, 1996), compliant patients improved significantly more than non-compliant patients on target phobia avoidance and fear at week 26 and 2 years.
Ee and e patients' use of a co-therapist
A relative or friend as co-therapist had been recruited during weeks 0-14 by 11 (44%) patients in Ee and by 8 (35%) in e. The presence of a co-therapist did not relate significantly to overall improvement of target fear or target avoidance from week 0 to 2 years in either Ee or e, despite Ee and e patients having improved slightly more in weeks 0-14 on target fear if they had a co-therapist (F(1,44)=3.63; P=0.063); by including the five patients who had no 2-year rating in this analysis, the difference became significant (F(1,49)=4.67; P=0.036). On target avoidance, e patients with a co-therapist tended to improve more during weeks 0-14 (F(1,44)=2.97; P=0.092). At 2 years, however, e patients who had a co-therapist lost 22% of their former improvement, a loss that was significantly greater than in e patients who had no co-therapist (6% further improvement) or in Ee patients (5% further improvement with and ‒8% without a co-therapist; F(1,44)=5.90; P=0.019).
Retrospective self-evaluations of treatment
Treatment success
Ratings were similar across treatment groups: 29 patients (43%) rated treatment as markedly successful, 19 (29%) as moderately successful and 19 (29%) as a failure. Success ratings were strongly predicted by the percentage improvement on target fear from week 0 to 2 years (adjusted R 2=0.464, β=0.688, t=7.36 and P=0.0001 on stepwise multiple regression) but not by the following variables: age; gender; education; illness duration; total time spent by therapist or patient during weeks 0-8; 2-year BDI score.
Improvement expectancy
Thirty-five patients (52%) rated improvement as more than expected, nine (14%) about what they had expected and twenty-two (33%) as less than expected. More Ee than e and r patients felt that they had improved more than expected (linear-by-linear association: χ2 (1)=6.29, P=0.012; ANOVA on expectancy scores: F(2,63)=4.28, P=0.018).
Other treatments from week 26 to 2 years
From week 26 to 2 years, of 67 patients who had been followed up, 18 (27%) had had other treatment for their phobia. Their frequency did not differ significantly across diagnosis (seven with agoraphobia, three with social phobia and eight with specific phobias) or type of treatment during weeks 0-14 or crossover from r at week 14 (five Ee, six e, three r-only and four r→Ee/r→e). Six (9%) patients had had tranquillisers, two had antidepressants, one had both types of medication, one had counselling and eight (12%) had other treatments.
On almost all pretreatment clinical measures, patients who had had other treatments after week 26 had not differed from those who had not, but had been significantly worse than patients who had not at week 14 and 2 years. It is unlikely that they had further gains from other treatments after week 26 because week 14 and 2-year scores did not differ on repeated-measures ANOVA.
Perceived need for further treatment at 2 years
Of 67 patients who had been followed up 33 (49%) felt that they needed more treatment for their phobia at 2 years (8/24 Ee; 14/23 e; 5/10 r-only; 6/10 r→Ee/r→e; 67% for agoraphobia, 43% for social phobia and 38% for specific phobias) and their distribution did not differ across the type of treatment. When asked if they would choose the same type of treatment they had had before week 26, 32 (97%) replied, of whom 13 (41%) said ‘yes’ (6/8 Ee, 5/14 e, 1/5 r-only, 1/5 r→Ee/r→e) and 19 (59%) said ‘no’ (2/8 Ee, 9/14 e, 4/5 r-only, 4/5 r→Ee/r→e). If this is a proxy for treatment preference, this was significantly greatest for Ee, next for e and least for r (linear-by-linear association: χ2 (1)=4.36, P=0.043).
DISCUSSION
Neither clinician- nor co-therapist-accompanied exposure enhanced 2-year outcome
Although Ee seemed preferred to e, this did not enhance outcome in terms of self-rated symptom severity and need for further treatment, so the 9 h of clinician-accompanied exposure proved redundant up to 2 years later. Our results extend earlier similar findings in this sample at 3-6 months' follow-up (Reference Al-Kubaisy, Marks and LogsdailAl-Kubaisy et al, 1992) and in other studies (e.g. Reference Marks, Lelliott and BasogluMarks et al, 1988).
Clinician-accompanied exposure had been given in a sufficient dose to show an effect. The six 90-min sessions during weeks 0-8 were even more than is usual in National Health Service clinics. For spider phobia, one 2-h session of clinician-accompanied exposure was compared with 2-h sessions guiding self-exposure over 2 weeks (Reference Öst, Salkovskis and HellstromÖst et al, 1991); clinician-accompanied exposure was superior up to 1 year but it is unclear how much this was due to its exposure bouts having been more prolonged and having included systematic modelling by a therapist. In present patients an effect of clinician-accompanied exposure sessions in Ee may have been overshadowed by the large amount of self-exposure homework.
About one-third of present e patients had recruited relatives or friends as co-therapists whose role during self-exposure might have resembled that of a clinician during Ee. Such a co-therapist in e was associated with slightly more phobia reduction in weeks 0-14 but not at 2 years, by which time some of these gains had been lost.
Contextual cues are important in learning and memory (e.g. Reference Smith, Glenberg and BjorkSmith et al, 1978). Fear spreads more easily to a neutral context than does fear reduction (Reference BoutonBouton, 1988; Bouton & Swartzentruber, 1991). A clinician or co-therapist may serve as a dual-edged contextual (safety or reminder) cue during exposure, facilitating fear reduction during active treatment but raising the risk of relapse in new phobic situations (Reference Rowe and CraskeRowe & Craske, 1998a ) or when the context changes to having no clinician or co-therapist present (Reference Rodriguez, Craske and MinekaRodriguez et al, 1999).
In Ee and e, compliance with self-exposure homework negotiated during week 0-8 sessions predicted better outcome at week 26 and 2 years. In obsessive—compulsive disorder, too, such compliance predicted more improvement up to six months (Reference de Araujo, Ito and Marksde Araujo et al, 1996). What determines compliance is largely unclear.
Compared with the 15% of patients without 2-year data, the 85% with such data had been very similar at pretreatment. By week 8 the 85% had improved more, and by week 26 more had had exposure in some form (Ee, e or r→Ee/r→e) rather than r-only. If the 15% of patients without 2-year data remained less improved at 2 years, then gains at 2 years may be overstated for the entire sample. This does not affect our main conclusions that Ee v. e did not differ significantly in outcome, that doing self-exposure homework in weeks 0-8 predicted more improvement at two years and that unimproved r patients improved after subsequent exposure.
Need for further treatment
The improvement that continued beyond week 14 to two years is in accordance with the stability of gains in other long-term follow-ups noted above. Although exposure treatments reduce phobias, they seldom abolish them completely (Reference Lelliott, Marks and MonteiroLelliott et al, 1987; reviewed by Reference MarksMarks, 1987). At 2 years, nearly half of our patients felt that they needed further treatment for their phobias; whether this should be more exposure or another approach deserves study.
Patients who fear many phobic situations may need exposure to them all in order to maximise improvement. Both Ee and e had focused on three or four main phobic targets. Patients who had more phobic situations that they were not exposed to may have remained unimproved in such situations and so felt a need for further treatment. Bearing this out, the percentage of Ee or e patients who felt the need for further treatment was two-fold greater for agoraphobia than specific phobias (with social phobias, including both focal and diffuse phobias, in between).
It is unclear whether desire for further help is reduced by adding non-exposure treatments. Almost half of those with social phobia still sought further treatment during follow-up after exposure plus cognitive therapy (Reference Mersch, Emmelkamp and LipsMersch et al, 1991). Although patients receiving such combined therapy felt less need for further therapy, at 18-month follow-up exposure plus cognitive therapy had no better outcome than exposure alone (Scholing & Emmelkamp, Reference Scholing and Emmelkamp1996a ,Reference Scholing and Emmelkamp b ). A liking of more therapist contact is common even when that does not enhance improvement.
Did relaxation have an effect?
Of the 27 original r patients, 10 had improved by week 14 and their gains continued to 2 years. This non-random r-only subgroup, however, was not comparable to the originally randomised Ee and r groups. Of the ten r-only patients, four did a mean of 17 h of uninstructed ‘self-exposure’ during weeks 0-14, so it is unclear as to what to attribute r-only's continuing gains at 2 years. The non-follow-up rate for r-only was higher and their improvement was greater than that of the total original r group. Our ten r patients who did not benefit from self-relaxation but went on to improve with Ee or e remained improved at 2 years.
Although r had been far less effective than Ee or e over weeks 0-14, at 2 years patients from all groups rated their treatments as having been similarly successful. However, the treatment that the original r patients rated as successful at 2 years had by then included self-exposure at some point in at least half of them. Satisfaction can be an unreliable guide to actual improvement.
Patients with post-traumatic stress disorder improved somewhat with therapist-accompanied plus self-relaxation, albeit less than with exposure or cognitive restructuring (Reference Marks, Lovell and NoshirvaniMarks et al, 1998), in an RCT that did not test whether such improvement was a placebo or a relaxation effect.
Clinical Implications and Limitations
CLINICAL IMPLICATIONS
-
▪ Improvement in phobias after self-exposure continued up to 2 years post-treatment, although nearly half of the patients still felt that they needed further treatment.
-
▪ Clinician-accompanied exposure proved redundant up to the 2-year follow-up.
-
▪ Patients who failed to improve with relaxation improved after subsequent exposure.
LIMITATIONS
-
▪ The three types of phobia had to be pooled because there were too few patients to analyse each phobia type separately.
-
▪ Patients who were followed up had only self-ratings at 2 years and they had been more improved at week 14 than the patients not followed up.
-
▪ Conclusions about the long-term effects of relaxation are unsafe because ten of the original relaxation patients had crossover exposure therapy after week 14.
ACKNOWLEDGEMENTS
David Mataix-Cols was funded by the Spanish Ministerio de Educación y Cultura and Je-Min Park by Pusan National University, Korea. Valuable comments on the manuscript were made by Drs Michael McDonough and Homa Noshirvani.





eLetters
No eLetters have been published for this article.