Dispersion of volatile toxic industrial compounds (TICs) may occur due to an industrial accident or as a result of an act of terrorism, presenting a major threat to nearby residents.Reference Hughart and Bashor 1 - 11 Standard issue gas masks provide respiratory protection against TICs by filtering inspired air through a chemical-biological-radio-nuclear (CBRN) activated charcoal filter.Reference Rimpel, Boehm, O’Hern, Dashiell and Tracy 12 , Reference Martyny, Glazer and Newman 13 Patients on home mechanical ventilation, however, are a subgroup for whom standard CBRN gas masks worn on the face would not provide protection from TICs, because in an environment contaminated with TICs an exposed ventilator would intake contaminated air and transmit it directly to the patient via the ventilation circuit and patient interface, without flowing through the CBRN filter in the patient’s gas masks. This subgroup has been steadily growing in size in recent years.Reference Carson, Cox, Holmes, Howard and Carey 14 - 17 Although a limited number of home ventilators have been custom designed to enable attachment of a CBRN filter to the ventilator’s air intake port for filtering of TICs,Reference Roberts, Bell and Wong 18 the majority of home ventilators currently in use do not have this design feature.
We have previously reportedReference Be’eri, Owen, Shachar, Barlavie and Eisenkraft 19 that although many potential solutions are impractical (such as attaching a CBRN filter to the air intake port of the ventilator, enclosing the patient and the ventilator in a gas-proof tent, or attaching the ventilator air intake port to a cylinder of compressed air or oxygen), in-line addition of a CBRN filter to the air-outflow port of a patient’s ventilator could be a realistic and effective strategy for affording CBRN protection to these patients. In that study, an animal model was used to study the physiological impact of a CBRN filter attached to the air-outflow port of a ventilator. We chose this strategy because it offers several advantages over the potential alternatives:
(1) Because the diameter of the air-outflow port of all home ventilators conforms to a universal 22 mm standard, a 1-size-fits-all CBRN filter designed to fit on an air-outflow port in an airtight manner would be a universal solution for TIC protection for all ventilator-dependent individuals, regardless of their ventilator type or design, and could be mass-produced without great expense.
(2) Even if the ventilator itself became contaminated by TICs, all air reaching the patient would still be adequately filtered of contaminants. This would obviate the need to immediately replace ventilators in a contaminated environment.
(3) The period of time during which a ventilator could operate during suspected exposure to TICs would be practically unlimited, thus facilitating emergency evacuation and management of ventilated individuals in mass-casualty scenarios.
(4) Caregivers would have unhindered access to the ventilated patient at all times, thus enabling life-support treatment whenever needed.
A concern of a possible exothermic reaction between the charcoal of the CBRN filter and enriched oxygen was tested separately in a study that showed there is no such reaction, and that oxygen flow through the CBRN filter is safe.Reference Krivoy, Luria, Gafnit, Sukhotnikovt and Yehezkelli 20
To the best of our knowledge, however, the impact of attaching a CBRN filter to the air-outflow port of a home ventilator has never been described in human beings. The current study was therefore carried out to test the physiological impact of this potential solution on a cohort of patients on chronic home ventilation.
Methods
Adult patients on stable, long-term mechanical ventilation at a chronic ventilation facility (Alyn Hospital, Jerusalem, Israel) volunteered to participate in the study. The study was performed with the approval of the Institutional Review Board of Hadassah Medical Center, Jerusalem, Israel, and written informed consent was obtained from all participants.
For each patient, baseline physiological indices (blood O2 saturation, inspired CO2, end tidal CO2, inspired O2, respiratory rate, and heart rate) and ventilation airflow parameters (peak inspiratory pressure [PIP], peak end expiratory pressure [PEEP], and tidal volume) were recorded. Then, a standard-issue model M-80 CBRN filter was added to the air-outflow port of the ventilator in-line with the ventilation circuit, using a specially designed adaptor (Figures 1 and 2). Ventilation was continued for 60 minutes, without change to the ventilation parameters. During this period of CBRN-filtered ventilation, physiological indices were measured every 15 minutes, airflow parameters were measured every 30 minutes, and the subjects reported their subjective sensation of breathing on an ongoing basis.
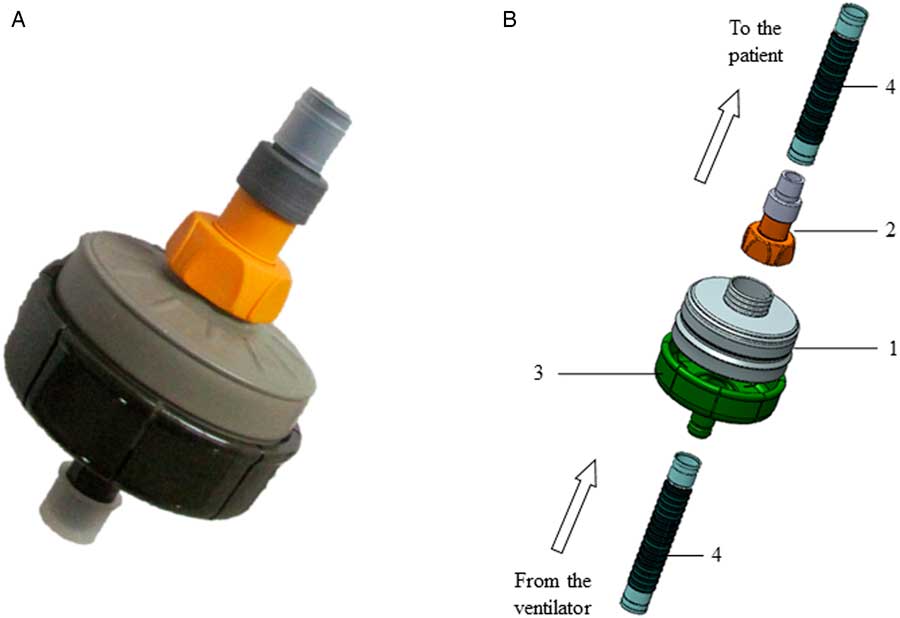
Figure 1 The Universal Chemical-Biological-Radio-Nuclear (CBRN) Filter Canister Adaptor for Ventilators. (A) Assembled filter-adaptor complex. (B) Components of the device: 1.—standard CBRN filter; 2.—specially designed connector between the CBRN filter and the ventilation tubing; 3.—standard-issue CBRN filter canister adaptor; 4.—standard ventilation tubing.

Figure 2 The Adaptor With a Standard-Issue Chemical-Biological-Radio-Nuclear Filter Canister Connected to a Ventilated Patient. Measurements were taken proximal and distal to the filter.
Respiratory physiological parameters were measured using a Capnomac Ultima ventilation monitor (Datex-Ohmeda Inc., Madison, WI) and a Nellcor pulse-oximeter (Tyco International Inc., Princeton, NJ). Ventilation airflow parameters were measured using a Ventcheck respiratory mechanics monitor (Novametrix Medical Systems Inc., Wallingford, CT).
Data analysis was performed with the Wilcoxon signed-rank test, in which exact P values are calculated, based on the permutation distribution of the test statistic. Standard asymptotic P values were not used because the data set was small, and asymptotic P values are valid only if sample sizes are reasonably large. StatXact 5 statistical software was used.
Results
Eight subjects participated in the study. All were ventilated via tracheostomy, using a volume-cycled assist-control mode of ventilation with no oxygen requirement. Diagnoses included Duchenne muscular dystrophy (n=6), congenital myopathy (n=1), and severe peripheral neuropathy (n=1). All subjects had been in stable condition with no adjustments made to their respiratory parameters and no episodes of acute illness during the 3 months before the trial. Seven of the ventilators used were LP-10 or LP-6 (Aequitron Medical Inc., Plymouth, MN) machines, and 1 was an LTV-950 (Pulmonetic Systems Inc., Minneapolis, MN) device. The ages of the subjects ranged from 18 to 39 years (mean: 28) and their mean duration of ventilation was 10.4 years (range: 4 months to 23 years).
All patients reported no subjective discomfort associated with addition of the CBRN filter to their ventilation tubing. This was true even for those patients who were breathing spontaneously and thus activating the ventilator’s trigger/sensitivity function. Table 1 shows the measured physiological parameters for the 8 subjects before and after 60 minutes of ventilation through a CBRN filter. Although mean saturation decreased from 98% to 97%, mean pulse rate increased from 90 to 94, and mean end tidal CO2 increased from 3.5 to 3.6 mg% during the 1 hour of CBRN-filtered ventilation, none of these changes were found to have statistical significance (Table 2). No changes in airflow parameters were detected (Table 3), and there was no evidence of rebreathing (inspired oxygen [FiO2] and inspired CO2 remained stable—Table 4).
Table 1 Measured Physiological Parameters for 8 Subjects Before (Pre) and After (Post) 60 Minutes of Ventilation Through a Chemical-Biological-Radio-Nuclear Filter

Abbreviations: O2 sat, oxygen saturation (%); etCO2, end tidal CO2 (cmH2O).
Table 2 Statistical Comparison of Measured Physiological Parameters Before (Pre) and After (Post) 60 Minutes of Ventilation Through a Chemical-Biological-Radio-Nuclear Filter

Abbreviations: O2 sat, oxygen saturation (%); etCO2, end tidal CO2 (cmH2O).
Table 3 Statistical Comparison of Airflow Parameters Before (Pre) and After (Post) 60 Minutes of Ventilation Through a Chemical-Biological-Radio-Nuclear Filter

Abbreviations: Vt, tidal volume (ml); PIP, peak inspiratory pressure (cmH2O); PEEP, positive end expiratory pressure (cmH2O).
Table 4 Statistical Comparison of Indices of Rebreathing Before (Pre) and After (Post) 60 Minutes of Ventilation Through a Chemical-Biological-Radio-Nuclear Filter

Abbreviations: FiO2, fraction of inspired oxygen (%); FiCO2, fraction of inspired CO2 (mg%).
No technical malfunctions of the ventilators occurred after addition of the CBRN filter to the air-outflow ports of the ventilators.
Discussion
We have previously reported the feasibility of adding a CBRN filter to the air-outflow port of a ventilator in an animal model, and proposed this as a strategy for providing ventilator-dependent individuals with protection from TICs.Reference Be’eri, Owen, Shachar, Barlavie and Eisenkraft 19 We now report the first application of this technique in human beings. We found that addition of the CBRN filter to the patient’s ventilation circuit was well tolerated subjectively by the patients, and found no evidence that the added resistance and dead space of the filter caused a significant change in the patient’s respiratory physiology or airflow parameters.
We previously reportedReference Be’eri, Owen, Shachar, Barlavie and Eisenkraft 19 that when ventilating through a CBRN filter with a ventilator that measures tidal volume at a sensor located proximal to (ie, “upstream” to) the CBRN filter (as is the case in LP-6 and LP-10 home ventilators), a 5% drop off in tidal volume delivered to the patient could be expected (possibly reflecting the additional dead space represented by the filter). The current study did not confirm this finding, although this may be due to the very small size of the study population. It would therefore be prudent to monitor both oxygen saturation and the patient’s subjective feeling of dyspnea after addition of a CBRN filter to any ventilator, and adjust the delivered tidal volume or peak pressure accordingly if needed.
All the ventilators used in this study sensed pressure at a point distal to (ie, “downstream” from) the CBRN filter, in proximity to the patients’ tracheostomy cannulae. In our previous studyReference Be’eri, Owen, Shachar, Barlavie and Eisenkraft 19 we postulated that in such circumstances addition of a CBRN filter to the ventilation circuit would not change the subjective effort experienced by a patient when pressure-triggering mechanical breaths. The current study confirms this hypothesis, with all patients reporting no subjective difficulty triggering breaths after addition of the CBRN filter as compared to before. It should be emphasized, however, that when using ventilators that sense pressure or flow triggering at a point proximal to the CBRN filter (such as most Bilevel Positive Airway Pressure [BiPAP] and Continuous Positive Airway Pressure [CPAP] ventilators), patients may experience decreased ventilator sensitivity to their inspiratory effort after addition of a CBRN filter to the ventilation circuit.
Based on the combined findings of our previously reported animal and in-vitro studyReference Be’eri, Owen, Shachar, Barlavie and Eisenkraft 19 and this human study, our recommendations for providing TIC protection to ventilator-dependent individuals can be summarized as follows:
(1) A CBRN filter should be placed on the air-outflow port of the ventilator. Ensure that patients and caregivers do not mistakenly attach the CBRN filter to the patient’s tracheostomy, endotracheal tube, or facemask instead.
(2) Tracheostomized patients should wear a standard-issue gas mask in addition, so as to protect the mucous membranes of their eyes, nose, and mouth. This is desirable, but probably unfeasible, also for patients with endotracheal tubes and non-invasive facemasks.
(3) For patients using BiPAP or CPAP ventilators, or any other ventilator that senses flow internally and not at a point downstream from the added CBRN filter, consider making the following adjustments to the ventilation parameters:
(a) If “time cycled pressure limited” (pressure controlled) or “flow cycled” (pressure support) ventilation is being used, increase the PIP or inspiratory positive airway pressure by 2 cmH2O.
(b) Check if the patient experiences difficulty triggering spontaneous breaths after addition of the CBRN filter. This may be mitigated by adjusting the trigger (sensitivity) setting, increasing the mandatory breath rate in compensation and/or increasing the PEEP setting.
(c) If “volume cycled” (volume controlled) ventilation is being used, consider increasing the tidal volume by 5% if the patient experiences discomfort.
(4) If parameter adjustments are needed, consider whether this is best done by professional health care providers as opposed to the patient/home aide. Ensure that parameters are reset to their prior values after the CBRN filter is removed.
(5) After addition of a CBRN filter to any ventilator, monitor both oxygen saturation and the patient’s subjective feeling of dyspnea and adjust the delivered tidal volume or peak pressure accordingly only if needed.
(6) Do not change the FiO2 because of addition of a CBRN filter.
(7) Replace the CBRN filter after 8 hours of continuous use, or, if opened but not used, after 12 months of storage.
CONCLUSIONS
A CBRN filter can be added to the air-outflow port of chronically ventilated patients, without causing an objective or subjective deterioration in the quality of the patient’s mechanical ventilation. This may serve as a simple and inexpensive solution for chronically ventilated patients in the setting of a chemical incident.
Authors’ Contribution
E.B. and A.E. conceived the study. E.B., A.E., M.B. and S.O. participated in the design of the study and in the data collection. S.R.M. performed the statistical analysis. E.B. and A.E. drafted the manuscript. All authors read and approved the final manuscript.
Conflicts of Interest
The authors declare that they have no competing interests.








