INTRODUCTION
Levothyroxine is a commonly used medication for hypothyroidism. Despite the large numbers of patients on levothyroxine, there is a surprising paucity of cases of overdose reported in the literature suggesting infrequent overdose with this medication, low toxicity, under-reporting, under-recognition of levothyroxine overdose, or a combination of one or more of these factors.
Chronic thyrotoxicosis is associated with significant morbidity and premature mortality.Reference Brandt, Green and Hegedus 1 A patient who takes an overdose of levothyroxine may be relatively asymptomaticReference Gorman, Chamberlain and Rose 2 or may develop the following symptoms: hyperthermia,Reference Loos, Das and Maury 3 cardiac arrhythmias, seizures,Reference Kulig, Golightly and Rumack 4 thyroid storm,Reference Majlesi, Greller and McGuigan 5 and even death.Reference Loos, Das and Maury 3 , Reference Levine 6 In the 2012 report from the American Association of Poison Control Centers (AAPCC), levothyroxine was one of the drugs ingested in nine fatal overdoses.Reference Mowry, Spyker and Cantilena 7 All of these fatal overdoses occurred in adults as part of a polydrug overdose.Reference Mowry, Spyker and Cantilena 7 Outside of the AAPCC data, most published cases are in the pediatric literature and relate to accidental overdose.Reference Gorman, Chamberlain and Rose 2 , Reference Kulig, Golightly and Rumack 4 , Reference Majlesi, Greller and McGuigan 5 , Reference Berkner, Starkman and Person 8 - Reference Singh and Winterborn 11 Adult cases have been reported only rarely and may be accidental, for example, due to ingestion of veterinary tablets.Reference Narula 12 In the small group of cases reported, the diagnosis is typically evident at presentation, that is, the patient arrives at the hospital already known to have taken an overdose.Reference Matthews 13 - Reference Hack, Leviss and Nelson 16 When there is no information at presentation to support an overdose, diagnostic confusion can occur. This may result in a missed opportunity to identify and initiate treatment for a polydrug overdose and/or result in the administration of unhelpful and potentially harmful therapies if, for example, specific therapy for Graves disease is initiated.
The aims of this case were to describe the biochemical findings diagnostic of exogenous thyroid hormone overdose, as compared to endogenous causes of thyrotoxicosis, and briefly summarize the management of levothyroxine overdose and where it differs to that of Graves disease.
CASE DESCRIPTION
A 55-year-old woman presented to the emergency department with confusion, dizziness, and vomiting. Shortly after arrival, the patient had a tonic-clonic seizure lasting less than 1 minute. Due to the reduced level of consciousness, no history was available from the patient, but the medication brought in with her by the ambulance staff included levothyroxine and citalopram. From the hospital chart, it was noted that the patient had a past history of Graves disease treated with radioactive iodine in 1993 and had been receiving levothyroxine (900 mcg per week). Thyroid function tests were normal 10 months earlier. Family members present at the initial assessment denied that she would ever consider overdose. There was no history of recent weight loss or thyrotoxic symptoms noted by the family members.
On examination, she was afebrile and normotensive with a pulse of 100 beats per minute. A neurological exam revealed a Glasgow Coma Scale (GCS) of 9/15, pupils were equal and reactive to light, but nystagmus was present in all directions. She was hyperreflexive with ankle clonus present. She had no meningism. There was no goiter or thyroid bruit.
A complete blood count, urea and electrolytes, and calcium and glucose were unremarkable. A computed tomography (CT) brain was normal. Thyroid function tests were markedly abnormal (Table 1).
Table 1 Relevant blood results from admission to day 14

D=day; FT3=free triiodothyronine; FT4=free thyroxine; RR=reference range; SHBG=sex hormone-binding globulin; TSH=thyroid-stimulating hormone.
* SHBG levels are raised in all forms of thyrotoxicosis, and the normal levels at presentation, despite very high thyroid hormone levels, suggested that the elevation of thyroid hormone was of recent onset.
The initial working diagnosis was a suspected thyroid storm due to recurrent Graves disease, and she was referred to the endocrine team.
Given the biochemical severity of thyrotoxicosis, despite an incompletely suppressed TSH, long duration of hypothyroidism, lack of recent symptoms and absence of a goiter, a polydrug (including levothyroxine) overdose was suspected. An urgent sex hormone-binding globulin (SHBG) level was within the reference range (see Table 1), and thyroglobulin was undetectable, confirming the clinical suspicion of excess exogenous thyroid hormone ingestion. Treatment was commenced with dexamethasone 8 mg daily and cholestyramine 1 g qid. Cardiac monitoring was performed. Beta-blockade was not given due to a history of asthma.
The patient’s GCS normalized within the next 4 hours, and she remained hemodynamically stable with no dysrhythmias. When alert, she admitted an intentional overdose of levothyroxine (15,800 mcg) and citalopram (2,460 mg) approximately 18 hours prior to presentation due to recent severe social stressors.
Cholestyramine was continued until FT4 levels were <50 pmol/L with regular monitoring of thyroid tests until the free thyroid hormone levels normalized. TSH receptor antibodies (TRAb) were positive at 4.4 U/L (normal <1.3 U/L). Following psychiatric assessment, the patient was discharged well on day 5.
DISCUSSION
We describe a case of massive levothyroxine overdose associated with co-ingestion of citalopram. Both citalopram and levothyroxine can produce hyperreflexia and clonus. The citalopram was most likely responsible for the seizure because this agent is known to increase seizure risk in doses >600 mg.Reference Personne, Persson and Sjöberg 17 Attributing the seizure to her thyroid dysfunction potentially risked missing the diagnosis of overdose.
Thyroid endocrinology
Common symptoms and signs of thyrotoxicosis include weight loss, palpitations, nervousness, tremor, tachycardia, goiter, sweating, and thyroid eye signs.Reference Sternlicht and Wogan 18 However, elderly patients may present with minimal symptoms (apathetic thyrotoxicosis).Reference Sternlicht and Wogan 18 The typical laboratory findings in thyrotoxicosis are of elevated FT4 and FT3 levels with a suppressed TSH due to the negative feedback of free thyroid hormones on the pituitary. This is true for any cause of thyrotoxicosis, including that of excess exogenous thyroid hormone administration with only rare exceptions, for example, secondary hyperthyroidism from a TSH-secreting pituitary tumour. T3 is the active hormone and, in addition to its secretion from the thyroid, is also produced from peripheral conversion of T4. Levothyroxine is a synthetic preparation of T4, which is also converted to T3 within the body. Patients receiving adequate levothyroxine replacement should have normal levels of FT4, FT3, and TSH. Levothyroxine (T4) overdose may result in delayed symptoms for several days after overdose because FT4 needs to be converted to the active FT3.Reference Bouchard 19
Diagnosis of levothyroxine overdose
At initial presentation, this patient had extremely high FT4 levels with an incompletely suppressed TSH level. Although this patient may have had endogenous thyrotoxicosis, such as from a late relapse of her Graves disease, there are a number of factors pointing toward the cause being due to the exogenous thyroid hormone. The most common causes of thyrotoxicosis are Graves disease, toxic multinodular goiter (TMNG), thyroiditis, and excess levothyroxine replacement (acute or chronic). There are key biochemical findings, which can help emergency physicians differentiate between the various diagnoses of thyrotoxicosis, in particular, levothyroxine overdose. Overdose is particularly important to recognize because this may be part of a polydrug overdose requiring specific treatment.
The clinical factors suggestive of exogenous thyroxine being the source of the thyrotoxicosis in this case included the long history of thyroxine use for previously treated Graves disease, the lack of thyrotoxic symptoms or signs noted by the family members, and the lack of a goiter.
The pattern of initial thyroid function tests suggested that an acute levothyroxine overdose was likely. In particular, despite the very high FT4 value (above the upper limit of the assay), the TSH was incompletely suppressed. The incomplete TSH suppression suggested that the overdose of levothyroxine was likely recent rather than chronic. This was supported by the normal SHBG level that peaked at only day 7 following admission (see Table 1). An urgent thyroglobulin was also performed at admission and was undetectable. Thyroglobulin is a protein specific to thyroid tissue, which can be measured from a peripheral blood sample. An undetectable thyroglobulin (in the absence of interfering antithyroglobulin antibodies) is confirmation that the cause is not due to endogenous thyrotoxicosis. Thyroglobulin levels will also be undetectable in surreptitious chronic thyroid hormone ingestion (thyrotoxicosis factitia). TRAb are not useful to help differentiate recurrent Graves disease from levothyroxine overdose because these may be elevated for many years following radioactive iodine therapy,Reference Laurberg, Wallin and Tallstedt 20 as demonstrated in this case.
Thyroid storm is a rare but important condition associated with a high mortality and requires urgent, aggressive therapy.Reference Burch and Wartofsky 21 A scoring system, developed by Burch and Wartofsky, based on abnormalities in the thermoregulatory, central nervous, gastrointestinal, and cardiovascular systems, can be used to help determine whether a patient is likely to have a thyroid storm (Table 2).Reference Burch and Wartofsky 21 This patient did not meet the criteria for the diagnosis due to the absence of fever, significant tachycardia, or other organ involvement. The only potential supporting feature other than thyrotoxicosis was the seizure (likely citalopram-related) and reduced GCS when postictal.
Table 2 Diagnostic criteria for thyroid storm (modified from 21)
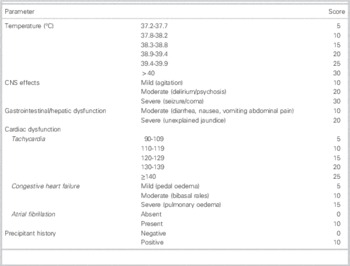
A score of ≥45 points is highly suggestive of thyroid storm; 25–44 is suggestive of impending storm; <25 points thyroid storm unlikely.
Thyroxine overdose management
Treatment of levothyroxine overdose should be considered as the following:
-
1. Decontamination
-
2. Symptomatic for life-threatening/hemodynamic complications or sympathetic overload
-
3. Blockade of peripheral conversion
-
4. Monitoring
Decontamination
Criteria are available as to when decontamination and medical treatment following excess thyroxine ingestion are appropriate.Reference Bouchard 19 Adults who present with acute ingestion >5,000 mcg should receive activated charcoal.Reference Bouchard 19 There is a limited role for gastric lavage in this setting, except in a very early massive overdose (e.g., >10,000 mcg).Reference Bouchard 19 In this case, the patient presented approximately 18 hours after an overdose, and so decontamination was not performed.
Symptomatic treatment
Symptomatic treatment for sympathetic overstimulation (tachycardia, systolic hypertension, widened pulse pressure, or a high cardiac output) with beta-blockade (or diltiazem if beta-blockade is contraindicated) is recommended.Reference Bouchard 19 In addition to the cardiac benefits, propranolol also reduces peripheral conversion of FT4 to the active FT3, which does not occur with selective beta-blockers. Given the history of asthma and the hemodynamic stability, beta-blockade was not given in this case. Beta-blockade can be started at any time point after presentation and the dose tailored to the clinical situation. Hyperthermia should be treated with acetaminophen and cooling cares.Reference Bouchard 19 Aspirin should be avoided due to the theoretical risk of increasing free thyroid hormone levels due to displacement from the thyroid hormone-binding proteins.Reference Bouchard 19 Use of benzodiazepines can be considered if the patient is severely agitated.Reference Bouchard 19
Blockade of peripheral conversion and increasing thyroid hormone clearance
Dexamethasone can be useful in severe thyrotoxicosisReference Jude, Dale, Kumar and Dodson 22 because it reduces peripheral FT4 to FT3 conversion. Dexamethasone was given, in this case, as the amount of levothyroxine taken was initially unknown, the FT3 was over three times the upper limit of normal, and it was thought that the FT3 level could further increase with the potential for cardiac instability. We would recommend considering corticosteroids in the setting of a massive levothyroxine overdose (>10,000 mcg), especially if the initial FT4 level is above the limit of quantification of the assay or in any patient with associated adrenal insufficiency. Bile acid sequestrants, such as cholestyramine, reduce enterohepatic recycling of thyroxine and have been demonstrated to lower thyroid hormone levels in thyrotoxicosis,Reference Tsai, Pei and Wang 23 , Reference Kaykhaei, Shams and Sadegholvad 24 including levothyroxine overdose.Reference de Luis, Duenas and Martin 25 Use of these agents in thyrotoxicosis is usually well tolerated and of low toxicity,Reference Kaykhaei, Shams and Sadegholvad 24 so they could be considered in patients who have taken a large overdose, to increase fecal thyroid hormone clearance.
Iopanoic acid and sodium ipodate reduce peripheral conversion of FT4 to FT3.Reference Laurberg and Boye 26 These agents can be useful for the short-term management of endogenous thyrotoxicosis because they also prevent thyroid hormone secretion acutely. Data on their use in acute levothyroxine overdose are limited to two pediatric case reports where they appeared to be successful.Reference Berkner, Starkman and Person 8 Routine use of these agents in levothyroxine overdose cannot be recommended due to the limited data available but should be considered in the setting of a thyroid storm.Reference Nayak and Burman 27
Hemoperfusion and plasmapheresis have been reported to be successful in removing levothyroxine from the serum.Reference Binimelis, Bassas and Marruecos 28 These methods are not likely to be necessary for most cases of levothyroxine overdose but could be considered in critically ill patients. However, data on the use of these therapies are limited, and not all groups have reported plasmapheresis to be efficacious in this setting.Reference May, Mintz and Lowry 14 , Reference Henderson, Hickman and Ward 29
Monitoring
Depending on the amount ingested, medical observation for at least 3–4 days following overdose should be considered. It is known that the peak thyroxine plasma concentration can occur 2–4 days post-ingestion (due to the long t1/2 of levothyroxine, approximately 7 days and the need for T4 to be converted to the active FT3).Reference Bouchard 19 For this reason, close monitoring of vitals (blood pressure, heart rate, respiratory rate, and temperature) is important. Hospital admission may not always be necessary if the patient is stable and psychiatric assessment advises that the patient can be safely discharged, but the amount of levothyroxine ingestion, comorbidities, particularly underlying cardiac disease, and clinical judgment should be used as markers for safe discharge.
Differences in management from endogenous thyrotoxicosis
Antithyroid drugs, such as methimazole, are usually the mainstay of treatment for Graves disease or TMNG but carry a small but significant risk of life-threatening side effects, such as agranulocytosis and liver dysfunction.Reference Nakamura, Miyauchi and Miyawaki 30 , Reference Malozowski and Chiesa 31 Antithyroid drugs are not effective in reducing thyroid hormone levels in exogenous thyroid hormone ingestion because endogenous thyroid hormone production is already suppressed. While propylthiouracil also reduces peripheral conversion of free thyroxine (T4) to free triiodothyronine (T3), there are other therapeutic alternatives for this, as described previously. Antithyroid drugs should not be given in the setting of excess exogenous thyroid hormone ingestion. Symptomatic treatment with beta-blockade and consideration of therapies to reduce peripheral conversion and to increase clearance of thyroid hormone are similar for both situations.
TAKE-HOME CLINICAL MESSAGES
Recognition of levothyroxine overdose is critical for appropriate management.
The diagnosis of levothyroxine overdose may be suggested by the history and examination findings. Biochemical features, such as the pattern of thyroid hormone elevation, SHBG, and thyroglobulin levels, help differentiating exogenous thyroid hormone overdose from endogenous causes of thyrotoxicosis. These tests are readily available from most hospital laboratories.
The ideal management of levothyroxine overdose is patient-dependent. Clinical signs and symptoms are the best indicator for the level of intervention required. Antithyroid drugs should not be given in the setting of exogenous thyroid hormone ingestion.
Competing interests: None declared.