INTRODUCTION
Respiratory distress secondary to acute cardiogenic pulmonary edema (ACPE) and acute exacerbations of chronic obstructive pulmonary disease (AECOPD) are common presenting complaints for emergency medical services (EMS). Until recently, the main prehospital interventions that have specifically targeted these disease processes are supplemental oxygen, bronchodilators, nitrates, and, in severe cases, assisted ventilation with bag valve mask (BVM) or endotracheal intubation.Reference Bruge, Jabre and Dru 1 , Reference Thompson, Petrie and Ackroyd-Stolarz 2 Some services use furosemide as a diuretic and morphine at low doses as an anxiolytic, but these are controversial and have been removed from many protocols.Reference Peacock, De Marco and Fonarow 3
Continuous positive airway pressure (CPAP) is a form of non-invasive ventilation (NIV) that has been demonstrated to be a useful adjunct in the management of ACPE and various forms of respiratory failure in the hospital setting.Reference Plant, Owen and Elliott 4 - Reference Vital, Saconato and Ladeira 6 As with other forms of NIV, CPAP results in faster clinical improvement and can reduce the requirement for invasive ventilation that increases the risk of complications, including nosocomial infections (pneumonia, sinusitis) and tracheal injury, which prolong intensive care unit (ICU) stay and hospital stay.Reference Thompson, Petrie and Ackroyd-Stolarz 2 , Reference Girou, Brun-Buisson and Taille 7 , Reference Levitt 8 A growing body of research has recently explored the application of this intervention in the prehospital setting, and there is some evidence to support a benefit in regard to morbidity, mortality, and cost.Reference Thompson, Petrie and Ackroyd-Stolarz 2 , Reference Vital, Saconato and Ladeira 6 , Reference Hubble, Richards and Wilfong 9 Barriers to the early adoption of prehospital CPAP were largely due to limitations in technology, money, and training. Although the adoption of this modality has increased to include most systems, the overwhelming management for these diseases has been the use of symptom relief drugs and traditional ventilatory support using high-flow demand oxygen devices (non-rebreather) and ventilatory assistance using BVM. There have been significant advances in producing cost-effective portable CPAP devices, but the implementation of this technology still requires a significant allocation of resources. As such, ongoing research is needed to determine the effectiveness and safety of this prehospital intervention on patient outcomes.
The objectives of this study were to 1) determine the effectiveness of appropriately administered prehospital CPAP on specific patient outcomes of morbidity and mortality, and 2) determine the ability of paramedics to adequately identify and safely treat patients with CPAP in a newly implemented prehospital protocol.
METHODS
Design and setting
A before-and-after study was conducted from August 1 to October 31 in 2010 and in 2011, before and after the implementation of prehospital CPAP in a city of one million people with large rural areas. The study size and period were chosen due to pragmatic constraints of budget and time. We compared the same 3-month period in 2 successive years to minimize bias from seasonal variations in disease prevalence. Almost all ambulances in this region are assigned one primary (i.e., basic life support) and one advanced care (i.e., advanced life support) paramedic. This study was approved by the Research Ethics Board of The Ottawa Hospital.
Study population
The study population was composed of persons ages 12 years and older and at least 40 kg of body weight with onset of respiratory distress assessed as ACPE or AECOPD by paramedics. All participants were transported by ambulance and treated in two emergency departments (EDs) in eastern Ontario.
Study intervention
Paramedics were trained to apply CPAP to patients with respiratory distress and a presumed diagnosis of ACPE or AECOPD prior to the commencement of the after period. Paramedics were trained with a 2-hour classroom module that included hands-on training in the ambulance. There was a follow-up video presentation (online) and continuing medical education review module. The device used was the Pulmodyne O2-RESQ System, which delivers 30% FiO2. CPAP could be applied at 5 cm H2O to 15 cm H2O.
We allotted a 3-month run-in period to allow for initial adoption issues to be sorted out before collecting data. Criteria for CPAP application were 1) at least two of the following: respiratory rate ≥24 breaths per minute, oxygen saturation <90%, and accessory muscle use; 2) paramedic impression of AECOPD or acute pulmonary edema; and 3) ≥12 years old and ≥40 kg body weight. Contraindications to CPAP application were defined as Glasgow Coma Scale <14, facial anomalies, airway compromise, intubation/tracheostomy, respiratory rate <8 breaths per minute, blood pressure <90 mm Hg, cardiac arrest, major trauma, or burns.
Data collection
Patient records were identified from the prehospital electronic database using the search criteria of presenting the complaint of “shortness of breath” and hospital return code “emergent.” In addition to these criteria, all patients receiving prehospital CPAP in the after group were captured. An electronic copy of the prehospital patient record was obtained for each patient and was then linked to in-hospital records using name and date of birth as identifiers. Prehospital and in-hospital patient records were manually screened, and data were abstracted by the primary author. Those patients missing in-hospital data were not included in the analysis (Figure 1). Data points included patient demographics, times for EMS arrival and departure, time of CPAP application, criteria for CPAP application, ED and hospital lengths of stay, paramedic impression of diagnosis, prehospital intubation, ED intubation, final ED diagnoses, and survival to ED/hospital discharge.

Figure 1 Patient Flow Diagram.
The use of “shortness of breath” as our initial search strategy was overly inclusive in our context, and the authors are confident that this captured all relevant patients. All use of CPAP was strictly documented, and the paramedic service assured 100% compliance.
Outcome measures
There were two main objectives in this study: 1) effectiveness and 2) safety. Each of these was defined with different suboutcomes, which will be explained here.
The primary effectiveness outcome was overall mortality. Secondary effectiveness outcomes were rates of intubation in the prehospital setting and the ED, rates of NIV in the ED, disposition from the ED, and length of stay.
For patient safety, the primary outcome was appropriateness of CPAP application based on the protocols to which the paramedics were trained. The secondary safety outcomes were rates of adverse events (paramedic reported adverse events as well as application of CPAP when contraindications were present) and the effect of CPAP on transport times. We included transport times in the safety arm of the study as a quality-control measure. We hypothesized that CPAP application would increase transport times and wanted to measure this to see whether it created an unreasonable delay.
There were no new co-interventions initiated during the study period. The use of symptom relief drugs was similar between groups.
Data analyses
Based on existing historical data, we predicted approximately 200 patients in the before and after groups. Sample size was primarily guided by feasibility in this unfunded study where we believed that two 3-month periods would provide sufficient patients to address the objectives. The association between the outcome measures and clinical variables was assessed by the appropriate univariate analyses according to the type of data: for nominal data, the χ2-test with continuity correction was used; for ordinal variables, the Mann-Whitney U-test was used; and, for continuous variables, the unpaired two-tailed t-test, using pooled or separate variance estimates as appropriate, was used.
RESULTS
We enrolled 341 patients from 383 charts reviewed, including 177 in the before CPAP group and 164 in the after CPAP group (see Figure 1). Ten patients in the before group and 22 in the after group had missing data, and thus were excluded from the analysis.
The mean age of patients was 71.5 years, with females comprising 51.4%. Final diagnoses included ACPE (18.9%) and acute exacerbation of COPD (AECOPD) (21.9%) (Table 1). Prehospital patient characteristics and transport times were similar between groups. Rates of EMS intubation were uniformly low, with only one intubation in the after group. There were a total of 36 CPAP applications in the after group. Paramedic diagnosis impressions differed between groups, with a higher rate of ACPE in the after group (34.6% v. 18.2%).
Table 1 Prehospital Characteristics of the 341 Dyspnea Patients in the Before and After Groups

In-hospital patient characteristics for the before and after groups were similar, with lower oxygen saturations on presentation to the ED in the after group (93.4% v. 99%) (Table 2). Final ED diagnoses of ACPE and AECOPD were similar between groups. There was a higher incidence of pneumonia in the before group. Rates of NIV in the ED were higher in the after group (20% v. 13.4%, p<0.0001), and there was no difference in the rates of intubation (2.1% v. 2.3%, p<0.001). There was no statistically significant difference in length of stay (6.8 v. 8.7 days, p=0.24). Disposition from the ED was similar between groups.
Table 2 In-hospital Characteristics of the 341 Dyspnea Patients in the Before and After Groups

Analysis of the prehospital characteristics of only those patients meeting CPAP criteria (n=112) yielded similar patient characteristics, although there were more female patients in the after group (54.5% v. 45.6%) (Table 3). Paramedic impressions varied between groups, with a greater proportion of AECOPD in the before group (52.2% v. 33.3%) and a greater proportion of ACPE in the after group (65.2% v. 43.5%) (Tables 3 and 4).
Table 3 Prehospital Characteristics of the 112 Dyspnea Patients Meeting CPAP Criteria in the Before and After Groups
Table 4 In-hospital Characteristics of the 112 Dyspnea Patients Meeting CPAP Criteria in the Before and After Groups

There were a total of 31 EMS CPAP applications out of the 66 patients meeting application criteria in the after group (i.e., 53% of patients meeting CPAP criteria did not receive the intervention). Of the 98 patients not meeting CPAP criteria in the after group, 5 patients received the intervention (i.e., 5.4% of patients not meeting criteria received the intervention anyway) (Table 5). There were 12 minor adverse events in 36 applications (33.3%), but none of these represented a patient safety issue (these patients did not tolerate CPAP in the prehospital setting).
Table 5 Number of Patients Meeting Criteria versus Actual Application of CPAP in the After Group

Footnote: 53% of patients meeting criteria did not receive CPAP. 5.4% of patients not meeting criteria received CPAP.
In-hospital characteristics of only those patients meeting CPAP criteria were similar between groups. Rates of NIV in the ED were higher in the after group, but this was not statistically significant (31.8% v. 21.7%, p=0.33) (see Table 4). Of the patients who received prehospital CPAP, six of them had the intervention discontinued on arrival to the ED and did not receive NIV for the duration of their stay. Eleven patients had their NIV continued in-hospital. Twenty patients who received NIV in the ED had not received prehospital CPAP. We did not include this in the analysis because the delay in the latter group of patients receiving NIV was up to 20 hours, so their condition may have deteriorated and would not reflect what the paramedics assessed in the field. There was no statistically significant difference in intubation rates (4.4% v. 1.5%, p=0.47).
There were significantly more patients discharged home from the ED in the before group (28.2% v. 10.6%, p<0.05). Mortality in the ED was greater in the after group (7.6% v. 0%, p<0.05). Length of stay in the ED was similar between groups, but the average length of admission was greater in the after group (12.2 days v. 6.6 days).
Overall mortality was greater in the after group (Figure 2, 18.8% v. 14.9%, p<0.0001). When looking at only those patients meeting CPAP criteria in each group, no statistically significant difference in mortality was observed (Figure 3, 19.7% v. 10.9%, p=0.21). There was one “do not resuscitate” (DNR) patient captured in the after group for those patients not surviving to hospital discharge. There were no DNR patients in the pre group for those patients not surviving to hospital discharge.
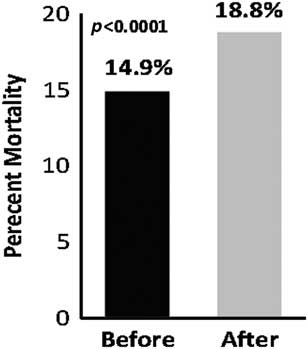
Figure 2 Overall Mortality Amongst the 321 Dyspnea Patients in the Before and After Groups.
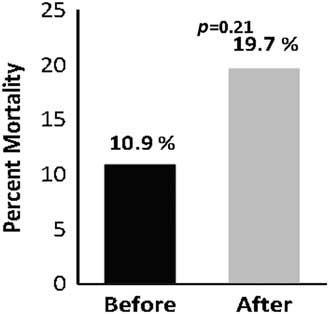
Figure 3 Mortality Amongst the 112 Patients Meeting CPAP Criteria in the Before and After Groups.
DISCUSSION
This before-and-after study was designed to assess the effectiveness of prehospital CPAP on patient mortality, morbidity, and length of stay. It was also designed to audit the safety and appropriateness of the application of this device by paramedics. We found the before and after groups to have similar patient characteristics, both prehospital and on presentation to the ED. CPAP did not show benefit with respect to rates of NIV in the ED, length of stay, or mortality. With respect to patient safety, there were very few applications of CPAP given the number of eligible patients, but no serious adverse events were reported as per protocol. It is unclear as to why there were so few applications of CPAP on patients who met clinical criteria. We did not include a questionnaire or debriefing tool for medics during this study, but, in speaking with paramedics and training staff, it would seem that the main barrier to CPAP application was the perception by paramedics that a patient had to be sick enough to warrant the device.
As in our study, not all published reports have shown benefit. In a recent observational study by Cheskes et al., researchers were unable to demonstrate a decrease in intubation or mortality related to the use of prehospital CPAP.Reference Cheskes, Turner and Thomson 10 A recent historical cohort analysis by Aguilar et al. failed to show a decrease in intubation, ICU admission, length of stay, or mortality.Reference Aguilar, Lee and Dunford 11
The results of this study are not consistent with several previous publications. Studies of this technology in the hospital setting have provided robust support for the routine use of NIV in patients with cardiogenic pulmonary edema and respiratory failure due to AECOPD.Reference Gray, Goodacre and Newby 5 , Reference Tsai, Clark and Cydulka 12 NIV has been shown to decrease rates of intubation, improve physiologic parameters, and even decrease mortality in hospital.Reference Vital, Saconato and Ladeira 6 Barriers to the widespread adoption of this treatment modality in the prehospital setting were largely due to the size, weight, and cost of older models; however, recent technological advances have led to increasing use. Furthermore, prehospital NIV has been shown to be an efficacious and cost-effective intervention for ACPE and AECOPD in several small prehospital studies.Reference Thompson, Petrie and Ackroyd-Stolarz 2 , Reference Hubble, Richards and Wilfong 9 In a recent systematic review of randomized control trials by Mal et al., a significant reduction in mortality and need for invasive ventilation both in and out of the hospital was found.Reference Mal, McLeod and Iansavichene 13 Williams et al. came to the same conclusion in their meta-analysis that included non-randomized and observational studies.Reference Williams, Finn and Perkins 14 Both of these reviews included primarily small studies, which presents a challenge to applicability to varied health care contexts. Because of these positive findings, adoption of NIV is increasing exponentially, allowing for a growing body of prehospital evidence. As discussed by Williams et al. in their literature review, there is a significant deficit in high-quality research pertaining to non-invasive management of respiratory distress in the prehospital setting.Reference Williams, Finn and Perkins 14 , Reference Williams, Boyme, Robertson and Giddings 15 NIV has been shown to be beneficial to patient care as a whole, but the question remains: Is the actual clinical impact of widespread prehospital CPAP worth the cost and training? How does it compare to other existing treatment modalities, such as nitrates, diuretics, and steroids?
This study has several strengths. First, it was a before-and-after study that measured the impact of this treatment modality in a real working environment, and there were no competing interventions during the study period. We conducted a comprehensive search of the database to capture all relevant patients and had balanced groups with respect to baseline patient characteristics. In order to minimize potential confounders, we allowed for a 3-month run-in period. We also selected identical months in 2 consecutive years to control for seasonal disease variations.
There were limitations to our study. The study was not blinded but this would be very difficult to accomplish. The study was neither multicentre nor randomized. We were missing some in-hospital data, and thus had to exclude a few patients in each group. Due to practical considerations, we limited our study to two EDs of one hospital, and thus limited our patient sample size. Data were collected by a single investigator, and, as such, we were not able to provide inter-rater reliability scoring (although the data extracted were objective). We also had a study population that was arguably less sick than in other studies; rates of intubation and use of NIV were low, which makes it difficult to draw conclusions from the data. Last, our centre is primarily urban with some rural areas, and thus our findings may not be generalizable to primarily rural populations.
CONCLUSION
Despite the robust in-hospital data supporting its use, we could not find benefit from CPAP in our prehospital setting with respect to morbidity, mortality, and length of stay. EMS must exercise caution in making the decision to invest in the equipment and training required to implement prehospital CPAP.
Acknowledgements
We would like to thank the Ottawa Paramedic Service, Julie Sinclair (Regional Paramedic Program for Eastern Ontario), Dr. Michael Austin (The Ottawa Hospital), My-Linh Tran and Angela Marcantonio (Ottawa Hospital Research Institute).
Competing interests: None declared.










