Introduction
Mycoplasma pneumoniae pneumonia (MPP), mainly caused by Mycoplasma pneumoniae, is a common respiratory disease in children, accounting for about 10–40% of community-acquired pneumonia cases in children [Reference Harris, Clark, Coote, Fletcher and Thomson5, Reference Zhu, Luo, Li, Jiang, Du, Wang, Li, Gu, Li, Tang, Qin, Xu, Liu, Zhao, Guo and Liu27]. Although M. pneumoniae pneumonia is usually a benign and self-limiting disease, some cases can become refractory or severe and life-threatening, which is defined as refractory M. pneumoniae pneumonia (RMPP) [Reference Tong, Huang, Zheng, Zhang and Chen19]. Compared with children without RMPP, those with RMPP present with cough, fever, and abnormal lung signs more frequently, and are more likely to have multiple systems and organ involvement such as nervous, digestive, blood, and mucocutaneous systems, may have sequelae [Reference Ding, Chu, Li, Li, Lei, Zhou and Chen3]. Therefore, identifying RMPP earlier and treating it promptly to prevent the progression of the disease is essential for paediatricians.
At present, the pathogenesis of RMPP is still unknown. Studies have found that excessive inflammatory response induced by M. pneumoniae plays a crucial role in the pathogenesis of RMPP [Reference Zhang, Dou, Tu, Shi, Wei, Wan, Jia, Ning, Wang, Li, Dong, Xin and Xu23, Reference Zhang, Wan, Yuan, Dou, Tu, Shi, Fu and Xin24]. Neutrophils are the first line of cellular defence against infection in the non-specific immune system, while lymphocytes play a role in adaptive immunity [Reference Tezol, Bozlu, Sagcan, Tuncel Daloglu and Citak18]. M. pneumoniae infection can aggravate the inflammatory response of the body, which may activate the apoptosis of lymphocytes, resulting in a decrease in lymphocyte count [Reference Kazama and Nakajima8]. Neutrophil to lymphocyte ratio (NLR) was reported to have an important predictive value for RMPP [Reference Ling, Ning and Xu11]. C-reactive protein (CRP) is an acute-phase protein synthesised by hepatocytes in response to pro-inflammatory cytokines during inflammatory/infectious processes [Reference Luan and Yao13]. C-NLR, which consists of both CRP and NLR, has been proposed as a promising marker to distinguish children with exacerbated asthma from healthy children [Reference Zhu, Zhou, Li, Pan, Zhang and Cui26]. Lymphocyte-CRP ratio (LCR) is another indicator of systemic inflammation and host–tumour cell interactions [Reference Nishi, Shimada, Tokunaga, Higashijima, Yoshikawa, Kashihara, Takasu, Ishikawa, Wada, Eto and Yoshimoto15], and was identified to be associated with the disease severity of COVID-19 patients [Reference Zhang, Gao, Wang, Li, Du, Tang, Lai, Chen, Yue, Wu, Kang and Zhao22].
The current predictors for RMPP often use only a single indicator, or the indicators in some studies are not readily available clinically [Reference Cheng, Lin, Zheng, Yan, Zhang, Zeng and Dai2]. More reliable and clinically available biomarkers for RMPP were still required. Previously, the prognostic significances of C-NLR and LCR have been validated in a variety of diseases and shown to be a promising reliable predictor [Reference Nishi, Shimada, Tokunaga, Higashijima, Yoshikawa, Kashihara, Takasu, Ishikawa, Wada, Eto and Yoshimoto15, Reference Zhu, Zhou, Li, Pan, Zhang and Cui26]. Thus, we suspected that C-NLR and LCR might have better predictive values for RMPP.
In the present study, the associations of C-NLR and LCR with RMPP were explored based on the data from the Department of Paediatrics, The Second Affiliated Hospital of Wenzhou Medical University. The predictive values of C-NLR and LCR for RMPP and prolonged fever were evaluated.
Methods
Study design and population
This cohort study enrolled 389 children diagnosed with MPP in the Department of Paediatrics, The Second Affiliated Hospital of Wenzhou Medical University. Participants met all of the following requirements to be enrolled: 1. Patients who meet the diagnostic criteria of MPP (M. pneumoniae anti-MP positive, antibody titre ≥1:160, nasopharyngeal secretion polymerase chain reaction test positive results of M. pneumoniae); 2. The age of the children was ≥1 month and <18 years old; 3. Complete clinical data. The exclusion criteria were: 1. People accompanied with primary or secondary immune deficiency disease; 2. Patients with respiratory diseases such as primary ciliary dystrophy, cystic fibrosis, congenital bronchopulmonary dysplasia, vascular ring malformations, bronchial foreign bodies, asthma, pulmonary tuberculosis, lung tumours, and non-infectious interstitial lung disease; 3. Patients with infection of other respiratory pathogens (blood culture, nasopharyngeal aspirate culture, nasopharyngeal aspirate virus reverse transcriptase real-time multiplex PCR, and serological test positive for common respiratory pathogens); 4. Patients who have used glucocorticoids or antibiotics before blood routine examination. This study got approval from the Ethics Committee of The Second Affiliated Hospital of Wenzhou Medical University (SZZSECHU-F-2021014). The need for written informed consent was waived by the Ethics Committee of The Second Affiliated Hospital of Wenzhou Medical University due to the retrospective nature of the study.
Potential covariates
Potential covariates include in this study were democratic data [age (≤6 years or >6 years), gender (males or females), height (cm), and weight (kg)], laboratory data [systolic blood pressure (SBP) (mmHg), diastolic blood pressure (DBP) (mmHg), temperature (°C), respiratory rate (beat/min), heart rate (beat/min), haemoglobin (HB) (g/L), red blood cell (RBC) (10/L), white blood cell (WBC) (10/L), monocyte (MONO) (10/L), eosinophils (EOS) (10/L), basophils (BAS) (10/L), mean platelet volume (MPV) (fL), red cell distribution width (RDW) (%), alanine aminotransferase (ALT) (U/L), total bilirubin (TBil) (μmol/L), total protein (TP) (g/L), albumin (ALB) (g/L), globulin (GLB) (g/L), albumin-to-globulin ratio (AGR), blood urea nitrogen (BUN) (mmol/L), and creatinine (Cr) (μmol/L)], and clinical data [pleural thickening, and signs of pulmonary (pulmonary atelectasis, pulmonary atelectasis & diminished respiration, diminished respiration, or others)].
Main variables
NLR, C-NLR, and LCR were the main variables in this study, which were evaluated on hospital admission. NLR was defined as a neutrophil to lymphocyte ratio. NLR was divided into ≤2.2 group and >2.2 group according to median. C-NLR was defined as CRP level multiplied by NLR and was divided into ≤29.9 group and >29.9 group based on median. The LCR was defined as the ratio of lymphocyte count to CRP level and was divided into ≤1584.2 group and >1584.2 group based on median.
Outcome variables
RMPP was the primary outcome, and the diagnosis as MPP patients who treated with macrolide antibiotics for 7 days or more, with prolonged fever (>38.5 C), deterioration of clinical symptoms (violent coughing, wheezing, chest pains, and trouble breathing), and progressive pulmonary radiological examination exacerbation (the scope of lung lesion expands, density increases, pleural effusion, even necrotizing pneumonia, and lung abscess pneumonia) [Reference Tamura, Matsubara, Tanaka, Nigami, Yura and Fukaya17]. Prolonged fever was another outcome analysed in the current study. Prolonged fever was defined as patients with persistent fever (>38.5°C) for >120 h after macrolide treatment [Reference Jang, Kim and Kim6]. The median follow-up time was 24.00 days.
Statistical analysis
Mean ± standard deviation (SD) was used to describe the distribution of the measurement data with normal distribution, and a t-test was used to compare the difference between the two groups. Non-normal data were described as median and quartiles [M (Q 1, Q 3)]. WilLRon rank sum test was applied for comparisons between the groups. Univariable logistic regression analysis was used to screen covariates associated with RMPP and prolonged fever. The associations of NLR, C-NLR, and LCR with RMPP, and prolonged fever were evaluated by univariable and multivariable logistic regression analysis. The predictive values of NLR, C-NLR, and LCR for RMPP, and prolonged fever were analysed. The odds ratio (OR), 95% confidence interval (CI), and area under the curve (AUC) were calculated. Alpha was set to 0.05, and the data analysis was subjected to R version 2 ucrt (2022-2106-23).
Results
Comparisons of characteristics of participants with and without RMPP
In total, 2081 RMPP patients aged ≥1 month and <18 years old with complete clinical data were enrolled. Among them, those accompanied by primary or secondary immune deficiency disease (n = 14), patients with respiratory diseases such as primary ciliary dystrophy, cystic fibrosis, congenital bronchopulmonary dysplasia, vascular ring malformations, bronchial foreign bodies, asthma, pulmonary tuberculosis, lung tumours, and non-infectious interstitial lung disease (n = 83), children with infection of other respiratory pathogens (n = 959), and participants who have used glucocorticoids or antibiotics before blood routine examination (n = 636) were excluded. Finally, 389 participants were included. The statistical power is exhibited in Supplementary Table S1. The screening process of participants is shown in Figure 1.

Figure 1. The flow chart of the participants screening process.
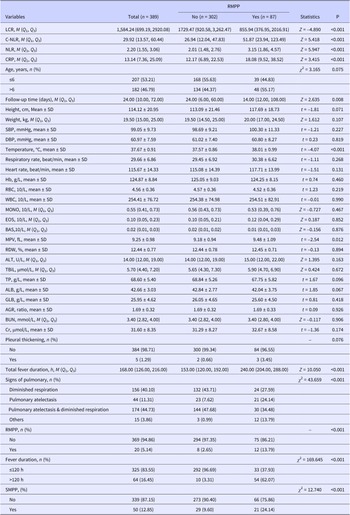
As exhibited in Table 1, there were 87 (22.37%) participants had RMPP. The median LCR in the RMPP group was lower than the non-RMPP group (855.94 vs. 1729.47). The median C-NLR in the RMPP group was higher than the non-RMPP group (51.87 vs. 26.94). The median NLR in the C-NLR in the RMPP group was higher than the non-RMPP group (3.15 vs. 2.01). There were 64 (16.45%) people with prolonged fever.
Table 1. Comparisons of characteristics of participants with and without RMPP

Abbreviations: AGR: albumin-to-globulin ratio; ALB: albumin; ALT: alanine aminotransferase; BAS: basophils; BUN: blood urea nitrogen; C-NLR: C-reactive protein-neutrophil to lymphocyte ratio; C-NLR: C-reactive protein-neutrophil to lymphocyte ratio; Cr: creatinine; CRP:C-reactive protein; CRP:C-reactive protein; DBP: diastolic blood pressure; EOS: eosinophils; GLB: globulin; Hb: haemoglobin; LCR: lymphocyte-C-reactive protein ratio; LCR: lymphocyte-C-reactive protein ratio; M: median; MONO: monocyte; MPV: mean platelet volume; NLR: neutrophil to lymphocyte ratio; NLR: neutrophil to lymphocyte ratio; Q1: 1st quartile; Q3: 3st quartile; RBC: red blood cell; RDW: red cell distribution width; RMPP: refractory M. pneumoniae pneumonia; SBP: systolic blood pressure; SD: standard deviation; TBil: total bilirubin; TP: total protein; WBC: while blood cell.
Associations of NLR, C-NLR, and LCR with RMPP in children
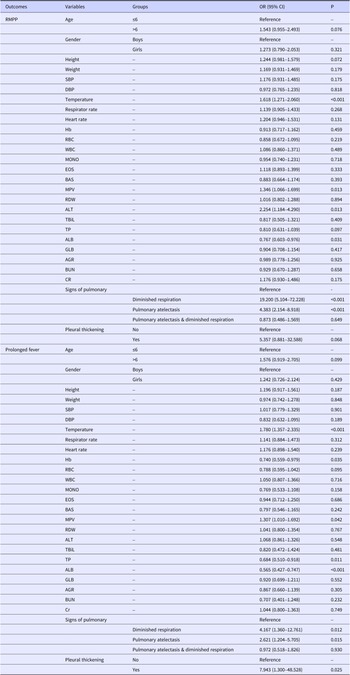
Variables with statistical association with RMPP and prolonged fever in univariable logistic regression analysis were considered to be covariates. The results depicted that temperature, Hb, TP, weight, RBC, MPV, ALT, ALB, and signs of pulmonary were covariates associated with RMPP, and prolonged fever (Table 2).
Table 2. Confounding factors associated with RMPP in children

Abbreviations: AGR: albumin-to-globulin ratio; ALB: albumin; ALT: alanine aminotransferase; BAS: basophils; BUN: blood urea nitrogen; CI: confidence interval; C-NLR: C-reactive protein-neutrophil to lymphocyte ratio; Cr: creatinine; CRP:C-reactive protein; DBP: diastolic blood pressure; EOS: eosinophils; GLB: globulin; Hb: haemoglobin; LCR: lymphocyte-C-reactive protein ratio; MONO: monocyte; MPV: mean platelet volume; NLR: neutrophil to lymphocyte ratio; OR: odds ratio; RBC: red blood cell; RDW: red cell distribution width; RMPP: refractory M. pneumoniae pneumonia; SBP: systolic blood pressure; TBil: total bilirubin; TP: total protein; WBC: while blood cell.
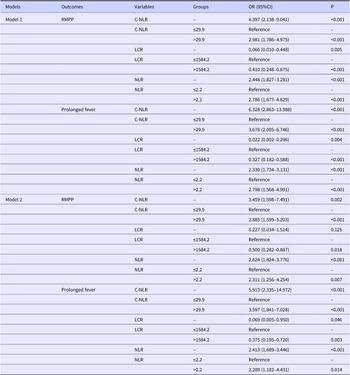
According to the data in Table 3, In the multivariable logistic regression group, the covariates were adjusted. We found that C-NLR was correlated with increased odds of RMPP in children (OR = 3.459, 95% CI: 1.598–7.491). A higher risk of RMPP was identified in the C-NLR > 29.9 group (OR = 2.885, 95% CI: 1.599–5.203). LCR >1584.2 was associated with a decreased risk of RMPP relative to children with LCR ≤1584.2 (OR = 0.500, 95% CI: 0.282–0.887). For every additional unit of NLR, the odds of RMPP were increased by 2.624 (95%CI: 1.824–3.776). In comparison to the NLR ≤ 2.2 group, children with NLR > 2.2 had a higher risk of RMPP (OR = 2.311, 95% CI: 1.256–4.254).
Table 3. Associations of NLR, C-NLR, and LCR with RMPP in children

Abbreviations: CI: confidence interval; C-NLR: C-reactive protein-neutrophil to lymphocyte ratio; CRP:C-reactive protein; LCR: lymphocyte-C-reactive protein ratio; NLR: neutrophil to lymphocyte ratio; OR: odds ratio; RMPP: refractory M. pneumoniae pneumonia.
Model 1: crude model.
Model 2: adjusted for temperature, Hb, TP, weight, RBC, MPV, ALT, ALB, and signs of pulmonary.
Associations of NLR, C-NLR, and LCR with prolonged fever in children
After adjusting for confounding factors, the increased risk of prolonged fever in children was identified with the increase of C-NLR (OR = 5.913, 95% CI: 2.335–14.972). C-NLR > 29.9 was correlated with an increased risk of prolonged fever in children (OR = 3.597, 95% CI: 1.841–7.028). Increased LCR level was correlated with reduced risk of prolonged fever in children (OR = 0.069, 95% CI: 0.005–0.950). LCR >1584.2 was related to decreased odds of prolonged fever in children (OR = 0.375, 95% CI: 0.195–0.720). Higher NLR was associated with an elevated risk of prolonged fever in children (OR = 2.413, 95% CI: 1.689–3.446). An increased risk of prolonged fever in children was observed in those with NLR > 2.2 (OR = 2.289, 95% CI: 1.182–4.431) (Table 3).
The predictive values of NLR, C-NLR, and LCR for RMPP and prolonged fever in children
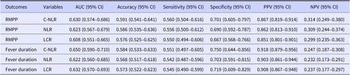
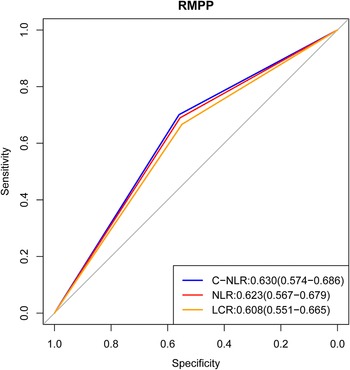
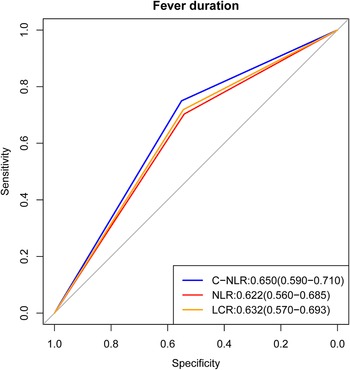
The predictive performance of NLR, C-NLR, and LCR for RMPP and prolonged fever in children was exhibited in Table 4. The AUCs of C-NLR, LCR, and NLR for predicting RMPP were 0.630 (95% CI: 0.574–0.686), 0.623 (95% CI: 0.567–0.679), and 0.608 (95% CI: 0.551–0.665), respectively (Figure 2). The AUCs of C-NLR, LCR, and NLR for prolonged fever in children were 0.650 (95% CI: 0.590–0.710), 0.622 (95% CI: 0.560–0.685), and 0.632 (95% CI: 0.570–0.693), respectively (Figure 3). Other detailed information on the predictive efficiency of NLR, C-NLR, and LCR for RMPP and prolonged fever in children is depicted in Table 4.
Table 4. The predictive values of NLR, C-NLR, and LCR for RMPP and prolonged fever in children

Abbreviations: AUC: area under the curve; CI: confidence interval; C-NLR: C-reactive protein-neutrophil to lymphocyte ratio; LCR: lymphocyte-C-reactive protein ratio; NLR: neutrophil to lymphocyte ratio; NPV: negative predictive value; PPV: positive predictive value; RMPP: refractory M. pneumoniae pneumonia.

Figure 2. The ROC curve of the predictive values of NLR, C-NLR, and LCR for RMPP in children.

Figure 3. The ROC curve of the predictive values of NLR, C-NLR, and LCR for prolonged fever in children.
Discussion
This study evaluated the associations of C-NLR and LCR with RMPP and prolonged fever as well as the predictive values of C-NLR and LCR for RMPP and prolonged fever in children. The data delineated that higher C-NLR was correlated with increased risk of RMPP, and prolonged fever in children. Higher LCR level was correlated with a reduced risk of prolonged fever in children. C-NCR presented superior predictive performance for RMPP and prolonged fever in children than LCR and NLR. The findings might offer an easy tool for quickly identifying children who were at high risk of RMPP and prolonged fever, and further guide the treatment for these children.
In our study, CRP combined with NLR exhibited superior predictive value to LCR and NLR for RMPP and prolonged fever. C-reactive protein (CRP) is a protein produced by the liver and increases significantly when there is inflammation in the body, which is one of the most investigated and widely used laboratory parameters to evaluate the body’s inflammation status [Reference Plebani16]. CRP was previously identified to exhibit statistical significance in predicting RMPP in Chinese children’s patients in the settings of paediatric emergency departments [Reference Wen, Su, Sun, Zhang and Li20]. CRP was reported to be a specific marker for diagnosing early M. pneumoniae infection in children [Reference Jiang, Wang, Zhang, Ma, Sang, Wang, Xu, Feng and Zhao7]. High ratio of CRP combined with procalcitonin could be used as a predictor for M. pneumoniae infection among adults hospitalised with community-acquired pneumonia [Reference Li, Kong, Xie, Zhang, Yan and Zhao10]. The predictive value of a high CRP combined with procalcitonin ratio for M. pneumoniae infection was also reported by Neeser et al. [Reference Neeser, Vukajlovic, Felder, Haubitz and Fux14]. High-sensitivity CRP was regarded as a vital marker for assessing the prognosis in children with mycoplasmal pneumonia [Reference Lai, Ai, Yang, Wei, Deng, Yu and Zhang9].
In the current study, increased NLR level was correlated with elevated risk of RMPP, and prolonged fever in children. In previous studies, NLR was identified to have significantly higher levels in paediatric patients with community-acquired pneumonia than those without, which showed high and moderate diagnostic value for the exclusion and indication of CAP, respectively [Reference Xu, Zhou, Zhang, Luo, Zhao and Xiong21]. Another study revealed that NLR > 3.92 might have important predictive value for RMPP in children more than 6 years old [Reference Ling, Ning and Xu11]. Fu et al. indicated that the severity of pneumonia increased proportionally with higher NLR values [Reference Che-Morales and Cortes-Telles1]. The findings in our study might be due to that NLR is a biomarker reflecting the extent of inflammation and the status of immune response [Reference Zheng, Xiang, Wang, Zhao, Fang and Dai25]. A former study demonstrated that NLR or CRP combined with lung ultrasound score can improve the accuracy of differentiating the severity and prognosis of severe pneumonia [Reference Fu, Zhang and Zhang4]. In our study, we combined CRP and NLR and established C-NLR (CRP level multiplied by NLR), and found that C-NLR level was also associated with the risk of RMPP and prolonged fever in children.
In this study, the AUC of C-NLR was higher than LCR, which indicated that C-NLR might be an essential index for quickly identifying children with high risk of RMPP and prolonged fever. LCR was an early index used for discriminating between sepsis and pneumonia in neonates in a previous study [Reference Liu and Mu12]. C-NLR is easily measurable from routine laboratory data and is a reflection of the status of the host anti-tumor immune and systemic inflammatory responses, which may be of great potential interest as a new direction for diagnosing RMPP. In the clinic, the routine detection of C-NLR might be helpful for the early identification of patients with a high risk of RMPP, and provide timely interventions to these patients might improve their prognosis. The limitation of this study was that this was a retrospective study from a single centre, the data of participants might have a recall or selection bias. Also, some features such as the lung function of participants were not considered. Large-sample and multi-centre studies are required to be conducted to gather further evidence of the value of C-NLR in the clinical use of identifying children with RMPP and prolonged fever.
Conclusions
We evaluated the associations of C-NLR and LCR with RMPP and prolonged fever as well as the predictive values of C-NLR and LCR for RMPP, and prolonged fever in children. The results showed that C-NLR was associated with increased RMPP risk in children, which might be a valuable index for predicting RMPP and prolonged fever in children. The findings might provide a reliable biomarker for early identifying children with high risk of RMPP and prolonged fever, and timely treatments might be performed on these patients.
Supplementary material
The supplementary material for this article can be found at http://doi.org/10.1017/S0950268824001134.
Acknowledgements
None.
Author contribution
Data curation: S.W., H.C.; Formal analysis: S.W., H.C.; Investigation: S.W., H.C.; Methodology: S.W., H.C.; Conceptualization: X.C., X.X.; Writing – original draft: X.C., X.X.; Writing – review & editing: X.C., X.X.
Funding statement
This research received no specific grant from any funding agency, commercial, or not-for-profit sectors.
Competing interest
None.