The risk of developing schizophrenia is modulated, among other factors, by the social and environmental context of where people live. Incidence rates of psychosis are different across countries,Reference Jongsma, Gayer-Anderson, Lasalvia, Quattrone, Mulè and Szöke1 possibly reflecting variations in the environment. Proposed specific factors explaining this effect have included an urban upbringing,Reference Vassos, Pedersen, Murray, Collier and Lewis2 povertyReference Kirkbride, Jones, Ullrich and Coid3 and the neighbourhood crime rate.Reference Bhavsar, Boydell, Murray and Power4 Where people live has also been related to recovery rates of schizophrenia, in the context of whether it is a low- or high-income countryReference Jablensky and Sartorius5 or experiencing periods of economic expansion or recession.Reference Warner6 Brain imaging studies have shown that many of these environmental factors are related to brain changes in healthy individuals. For example, young people raised in poverty in high-income countries show reductions in total brain grey matter.Reference Noble, Houston, Brito, Bartsch, Kan and Kuperman7 Exposure to childhood adversity and violence has also been related to differences in hippocampal and amygdala volumes.Reference Calem, Bromis, McGuire, Morgan and Kempton8 An unresolved question relates to how these environmental factors affect the biology of schizophrenia. Could brain differences typically seen in patients with schizophrenia be accounted for by these environmental factors? How will the neuropathology of schizophrenia interact with brain changes related to the environment? Is there a double-hit situation, where we see increased brain abnormalities in those vulnerable individuals becoming unwell in a harsh environment?Reference Walker, Wachs, Gardner, Lozoff, Wasserman and Pollitt9
Studies on environmental factors are particularly important for harsh settings such as those in low- and middle-income countries like Latin American countries. Few imaging studies have been done in such places, and as a result, we know little about what happens to the brain when becoming unwell with psychosis in an adverse environment. Major Latin American cities have high levels of violence (with one of the highest homicide rates in non-war zones) and poverty.Reference Muggah and Aguirre10,Reference Cepal11 However, not everyone is equally exposed to these factors, with high levels of inequality where some have the living standards of high-income countries.Reference Amarante, Galván and Mancero12 We used the opportunity provided by this strong environmental-factor exposure and the large variance owing to the existing inequality,Reference Crossley, Alliende, Ossandon, Castañeda, González-Valderrama and Undurraga13 and explored the structural brain changes related to living among violence and poverty in health and schizophrenia. Considering the existing literature in healthy individuals, we predicted we would find localised changes related to environmental violence in the hippocampus,Reference Logue, van Rooij, Dennis, Davis, Hayes and Stevens14 whereas poverty would be related to global changes.Reference Noble, Houston, Brito, Bartsch, Kan and Kuperman7 In terms of the direction of this relationship, we hypothesised that we would see a stronger association between environmental factors and grey matter in patients with schizophrenia because of the potential cumulative effect of damaging factors on the brain.Reference Walker, Wachs, Gardner, Lozoff, Wasserman and Pollitt9
Method
Participants
The study is part of the Latin American Network for the Study of Early Psychosis (ANDES; www.cyted.org/redes/ANDES), a consortium of research groups from six Latin American countries: Argentina, Bolivia, Brazil, Chile, Colombia and Mexico. Six imaging groups participated in this study, totalling seven different samples acquired in different scanners located in Buenos Aires, Porto Alegre, São Paulo, Santiago, Medellin and Mexico City (the latter contributing two different samples). Participants with a diagnosis of schizophrenia or schizophreniform disorder under the age of 50 years were included in the analysis, as well as healthy controls. Further site-specific details about recruitment, assessment and inclusion criteria are described in Supplementary Table 1 available at https://doi.org/10.1192/bjp.2020.143. All participants provided written informed consent to participate, and studies were approved by their local ethics committee (Buenos Aires, Bioethics Committee Fundación para la lucha contra las Enfermedades Neurológicas de la Infancia (FLENI), approval number 1612; Medellin, Bioethics Committee, School of Medicine, Universidad de Antioquia, approval number N.013; Mexico City, Ethics and Scientific Committees of the Instituto Nacional de Neurología y Neurocirugía, approval number 98/12; Porto Alegre, Ethics Committee of Hospital de Clínicas de Porto Alegre, approval number 2010-0348; Santiago, Ethic and Scientific Committee Comité Ético y Científico Ciencias de la Salud Pontificia Universidad Católica (CEC MED UC), approval number 14-442; Sao Paulo, Research Ethics Committee of Universidade Federal de São Paulo (UNIFESP), approval number 1737/06).
Environmental exposure
For each participant, we obtained a measure of exposure to environmental violence and poverty. As a proxy for environmental violence, we used the homicide rate reported for the area where the participant was living at the time of the study. For poverty, average household income of the neighbourhood where the participant lived, according to official open-access government data, was used. In one centre (Mexico), family income was obtained directly from the participants. As addressed later in the discussion, both characteristics are therefore about the environment where the participant was living at the time of the study, rather than the participant's characterisation. Table S1 details the sources of the data used. To account for differences in how the metrics were obtained, particularly when measuring income, we used standardised z-scores normalised for each participating site. The correlation between environmental violence and income was −0.33 (P < 10−16). Potential effect of this shared variance is explored further in Supplementary file 1, which shows that our main results are unchanged when considering only one of these environmental variables at the time.
Preprocessing of images
T1-weighted images were acquired in the different centres, using different scanners and protocols (see Supplementary Table 1), but were all preprocessed equally. This involved using SPM12 (www.fil.ion.ucl.ac.uk/spm/) running on MATLAB (Mathworks) for tissue segmentation, creation of a cohort-specific template with DARTEL,Reference Ashburner15 normalisation to Montreal Neurological Institute (MNI)Reference Fonov, Evans, Botteron, Almli, McKinstry and Collins16 and extraction of voxel-level modulated grey matter volumes. To account for differences in MRI scanners and acquisition protocols, grey matter volumes were corrected by ComBat (https://github.com/Jfortin1/ComBatHarmonization) running on MATLAB.Reference Fortin, Cullen, Sheline, Taylor, Aselcioglu and Cook17 Briefly, this algorithm treats the scanner effect as additive and multiplicative, assuming that the voxel-level values can be modelled as a linear combination of the biological variable and the site effects, with the error term being modulated by additional site-specific scaling factors. It uses empirical Bayes to improve the estimation of the model with small sample sizes. To explore the potential effect of ComBat on our results, a confirmatory analysis of our main result, using a mixed-model approach to deal with the interscan variance, is included in Supplementary file 1.
Statistical analysis
Harmonised, intersite grey matter volumes were then analysed with a single general linear model that included being a case (patients, 1; controls, −1), our two variables of interest (poverty and violence) and their interaction with case. Age and gender were included as covariates of no interest. Following the recent, large Enhancing Neuro Imaging Genetics through Meta-Analysis study,Reference van Erp, Walton, Hibar, Schmaal, Jiang and Glahn18 we looked for possible regional specificity of changes by normalising the voxel-level data by the total grey matter volume of the individual. As described in the Results, we also performed a case–control comparison between selected subgroups according to income (top 20th percentile compared with bottom 20th percentile), balanced across sites and correcting for age and gender.
Data were analysed with SPM12 (www.fil.ion.ucl.ac.uk/spm/) and custom-built scripts both running on MATLAB 2016 (Mathworks, USA, www.mathworks.com). Code is available from the authors upon request. All P-values are reported as significant when <0.05, corrected with false discovery rate when presenting voxel-level results.
Results
A total of 334 patients with schizophrenia and 262 healthy controls were included in the analysis. Table 1 describes the characteristics of the participants, including their demographics, clinical characteristics and exposure to environmental factors.
Table 1 Demographics of the sample

a. To allow for intercountry comparisons in this table of income measured in different ways across sites, the site-specific income distributions were centred and scaled to the World Bank's Adjusted Net National Income per Capita for that country, which is in years (https://data.worldbank.org/indicator/NY.ADJ.NNTY.PC.CD). Equivalent doses calculated according to.Reference Mani, Mullainathan, Shafir and Zhao19
b. Participants assessed with the Scale for the Assessment of Positive Symptoms (SAPS) and the Scale for the Assessment of Negative Symptoms (SANS), which corresponds to a positive scale of 13.6 and negative scale of 18.8 of the Positive and Negative Syndrome Scale (PANSS).Reference Lungo and Baires20 Note that data from this cohort was not used for the assessment of the overall symptoms calculated below.
Grey matter volume and income
Median annual income for patients with schizophrenia and controls were $7133 and $8848, respectively, as detailed in Table 1. This corresponds to 14% and 17%, respectively, of the equivalent USA figure. There was a significant interaction between income and case in whole-brain grey matter volumes (ß = −563.8 ± 204.3, P = 0.006). Controls showed a positive correlation with income, which was significant when they were considered independently (Fig. 1(a); R = 0.14, P = 0.021). This positive correlation was not present in patients with schizophrenia. If anything, income was negatively correlated with grey matter volume in that group, albeit non-significantly (Fig. 1(b); R = −0.076, P = 0.17). The direction of this differential relationship of income on cases and controls was seen in sites exclusively recruiting first-episode patients (Mexico and Chile), as well as in other sites recruiting chronic patients (Supplementary Fig. 1A). It was also seen in both men and women (Supplementary Fig. 1B). As shown in Supplementary file 1, interaction analyses exploring whether this differential relationship varied according to chronicity or gender were not significant. Furthermore, the direction of the relationship between income and total grey matter volume was consistent across the participating sites (Supplementary Fig. 2), albeit not always significant considering the smaller sample size.
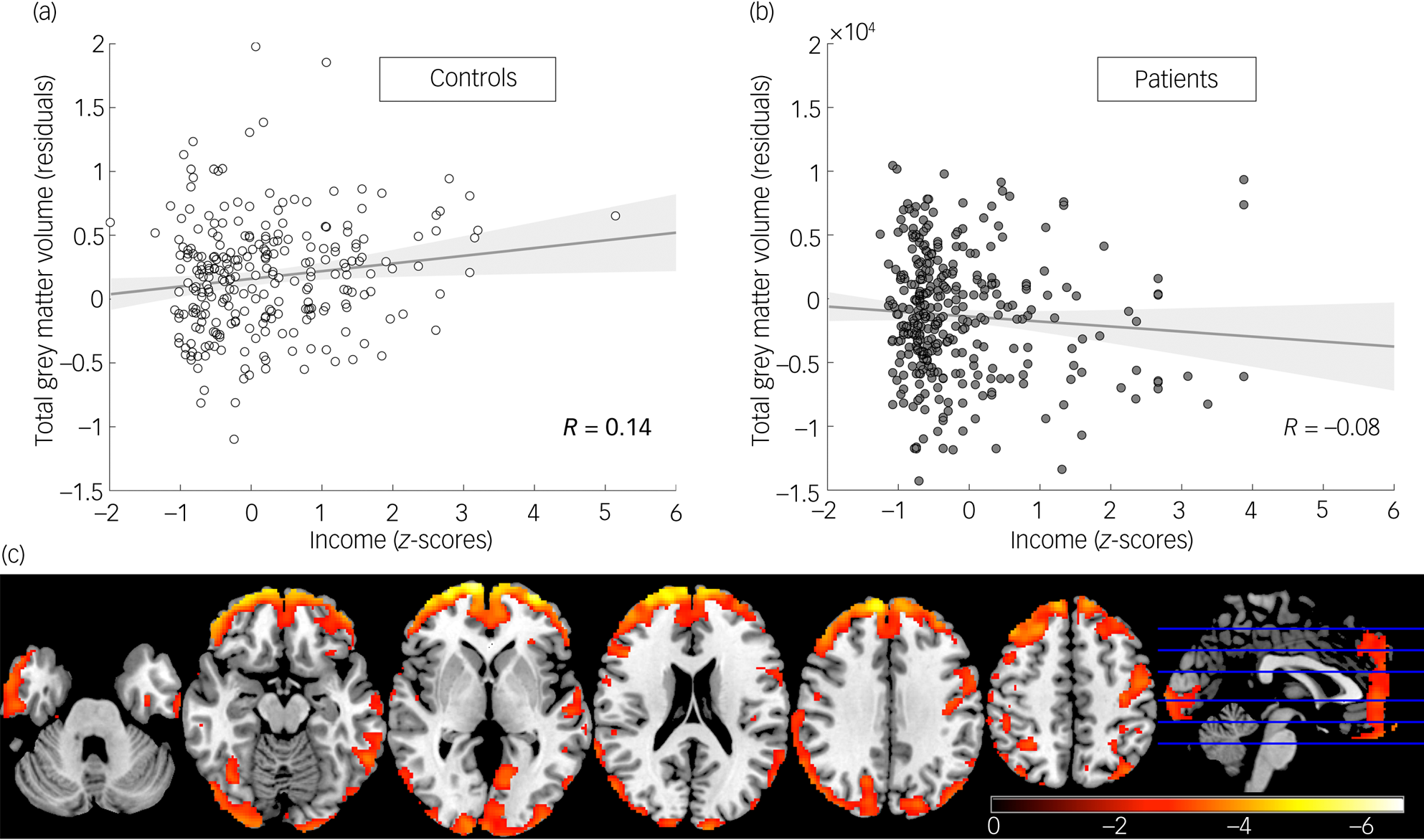
Fig. 1 Total grey matter volumes are differentially related to income in patients with schizophrenia and controls. Relationship between income and total grey matter volumes in (a) controls and (b) patients with schizophrenia (note the different direction of the relationship). (c) Voxel-level analysis of the relationship between income and grey matter volume showing that the significant interaction was widespread across the cortex (t-values from highlighted voxels are significant at P < 0.05 corrected with false discovery rate).
Exploring the relationship between income and grey matter volume at the voxel level (correcting for multiple comparisons) highlighted that the significant interaction between income and case was distributed across the whole cortex (Fig. 1(c)). All significant voxels showed the same direction of the interaction, showing a positive correlation with income for healthy controls and a negative correlation for patients with schizophrenia. We then explored how specific brain regions were related to income after accounting for changes in whole-brain grey matter. An initial pattern emerged of voxels located in the prefrontal region showing a negative interaction between case status and income after accounting for total grey matter volumes (Fig. 2(a)). In this region, income was positively related with higher grey matter volume in healthy controls (coded −1 in our model), with the correlation being stronger than the one observed in the rest of the brain. In patients with schizophrenia (coded 1 in our model), this region behaved like the rest of the brain (Fig. 2(b)). The second pattern observed was a positive interaction between grey matter volume and case status in the right hippocampus, as well as a few voxels in the frontal insula and putamen (Fig. 2(c)). In these regions, patients with schizophrenia showed a positive correlation with income, after accounting for global brain changes, whereas healthy controls showed a negative correlation (Fig. 2(d)).
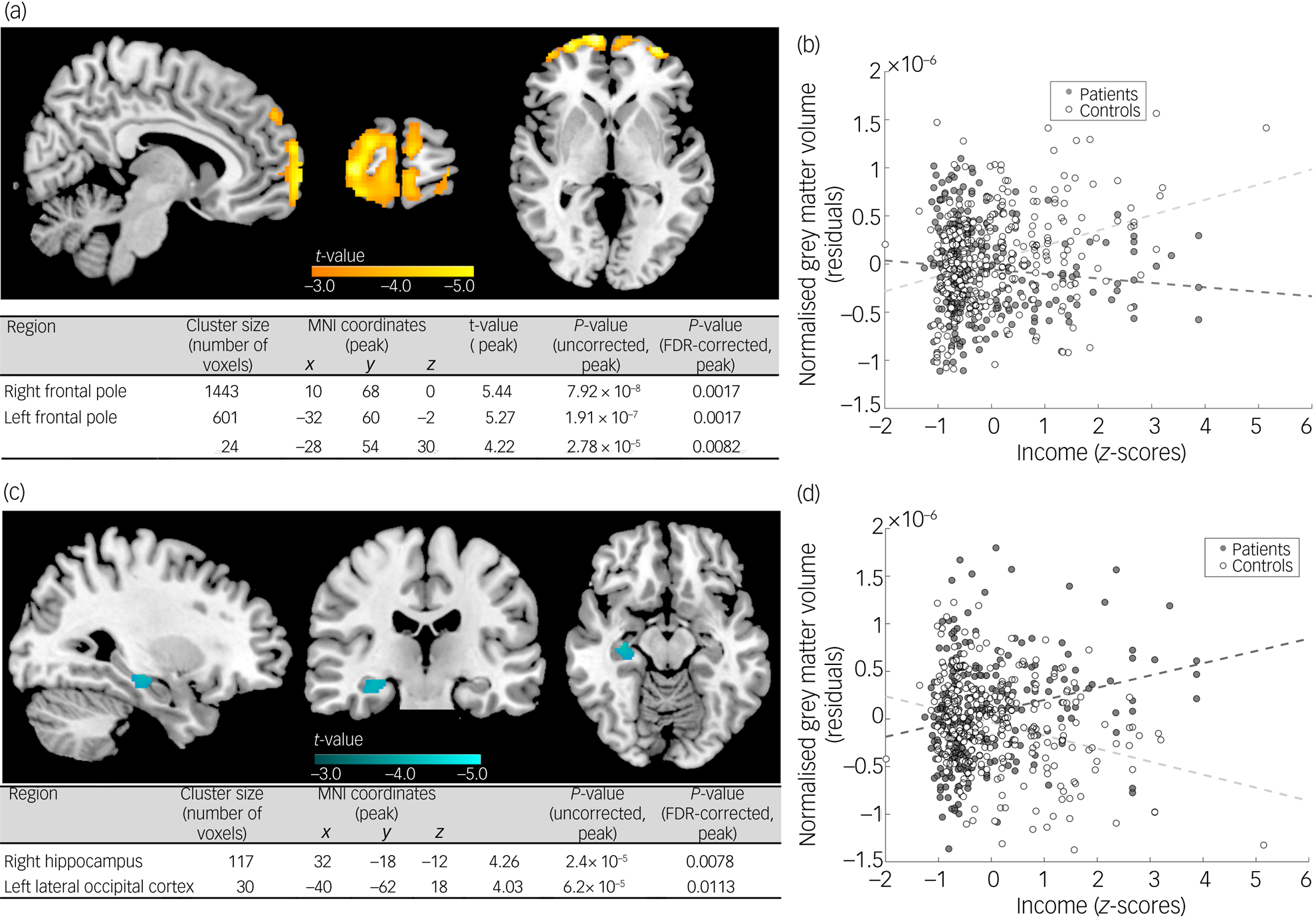
Fig. 2 Differential relationship between income and grey matter volume in cases and controls after accounting for global brain differences. Significant interactions between case and income assessed at P < 0.05 false discovery rate (FDR) were observed in two directions (cluster size >15 voxels presented). A first pattern is displayed in panel (a), covering mostly frontal regions. Panel (b) displays a scatterplot showing the mean volume of all the significant voxels highlighted in (a) for each group, and its relationship with income, controlling for age and gender. As can be seen, frontal regions in controls showed a significant positive correlation with income, beyond the one observed in the rest of the brain, with patients with schizophrenia not differing much from the effect on the rest of the brain. A second pattern is highlighted in (c), present in the right hippocampus. The scatterplot in (d) depicts the direction of this interaction showing the mean volume of all the significant voxels according to case and income, controlling for age and gender. Patients with schizophrenia showed a more significant relationship with income in their right hippocampus (relative to the rest of the brain), whereas controls showed a negative one.
MNI, Montreal Neurological Institute.
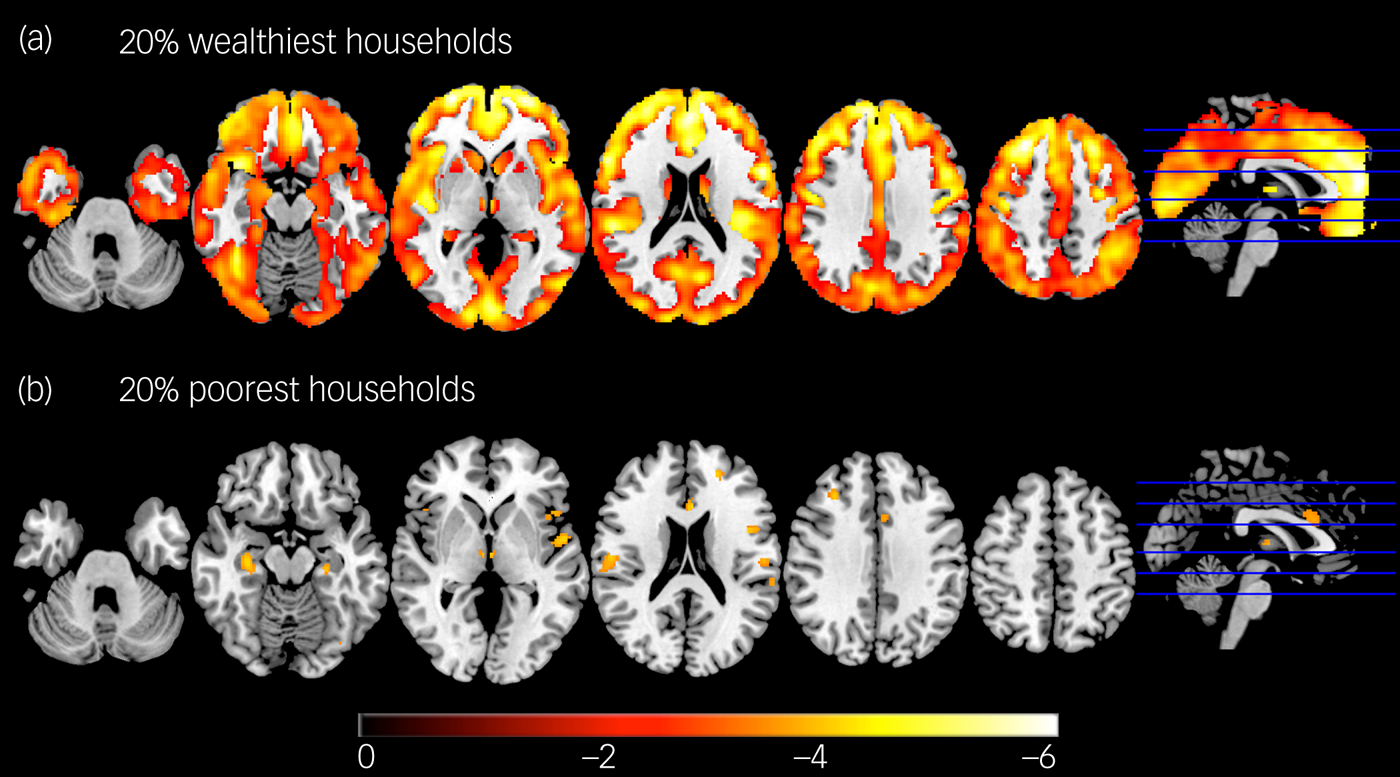
The observed relationship between income and grey matter volume implied that case–control differences varied according to whether the sample was obtained from high earners or low earners. Figure 3(a) shows the case–control comparison of 63 patients with schizophrenia and 55 controls who were within the top 20th percentile for household income from all the included cities, with widespread significant differences (all volume reductions observed in patients with schizophrenia) echoing results from a recent large case–control study.Reference van Erp, Walton, Hibar, Schmaal, Jiang and Glahn18 Figure 3(b) shows the same analysis performed with the same number of participants, but from the bottom 20th percentile for household income. Differences are only restricted to a few areas (bilateral insula, hippocampi, superior temporal regions and prefrontal cortex).

Fig. 3 Case–control analysis for the wealthiest and poorest households. Decreases in grey matter volume in 66 patients with schizophrenia compared with 53 controls, corresponding to (a) the top 20th percentile and (b) bottom 20th percentile for household income across the sample. Patients with schizophrenia did not show any areas that were larger than healthy controls in either comparison. Results are balanced for the different centres and controlled for gender and age. Highlighted voxels are significant at P < 0.05 corrected with false discovery rate, and colour-coded according to the t-value. Note the widespread differences in more affluent settings, and the more restricted differences in the poorest households.
Grey matter volume and environmental violence
As described in Table 1, participants were exposed to high levels of environmental violence, living in areas with median rates of homicides for controls and patients with schizophrenia of 7.8 and 8.8 homicides per year per 100,000 inhabitants, respectively. This is equivalent to 2.5–3 times the rate reported for all of Europe. The relationship between environmental violence and total grey matter volume, as well as its interaction between case and violence, were not significant. Voxel-level analyses did not find any significant results. There was a trend toward a significant interaction between environmental violence and total grey matter volume (P = 0.064), with a decrease in grey matter volume in more violent environments observed only in patients with schizophrenia (Supplementary Fig. 3).
Discussion
Environmental and social factors are known risk factors for schizophrenia, as well as modulators of its course. Previous literature showed that these factors are associated with differences in brain structure in healthy individuals, but how they are related in patients with psychosis is still unclear. We used a relatively large sample of patients with schizophrenia living in Latin American cities to explore the structural brain correlates of living among these factors, taking advantage of the large and unequal distribution of the exposure in these populations. We found a significant relationship between income and grey matter volume: controls presented with larger total grey matter volume when living in areas with higher household incomes, but this relationship was not present in patients with schizophrenia. As such, structural brain differences in schizophrenia and healthy controls vary according to the environment the individual lives in, possibly reflecting different neuropathological mechanisms.
Lower income has been previously related to lower global grey matter in healthy individuals, but this relationship was limited to the poorest households.Reference Noble, Houston, Brito, Bartsch, Kan and Kuperman7 Considering the average income of our participants, it is not surprising to observe such a relationship across our sample of healthy controls because most of them lived in similar conditions to the most deprived participants in those studies of high-income countries. As has been discussed in the literature, it is likely that this effect is multifactorial; it might be related to better perinatal care, better nutrition and lower risk of infections at an early age, less exposure to toxic substances, better access to education and even less stress in those not exposed to poverty.Reference Lozoff, Jimenez and Smith21 It is remarkable that despite looking at the characteristics of the environment where participants were living and not their own personal exposure to poverty, we still see a significant effect. Individuals living in a poor environment are not necessarily exposed to the same state of deprivation; they could even have moved to that neighbourhood recently. Latin American cities tend to be highly segregated according to socioeconomic class, which increases the precision of this estimate.Reference Shashi, Keshavan, Kaczorowski, Schoch, Lewandowski and McConkie-Rosell22 It might also be that the level of poverty in Latin American cities is such that the relationship is significant even when using a noisy proxy measure that might dilute its effect. On the other hand, epidemiological studies have suggested that environmental poverty has an effect even after accounting for personal experience of poverty.Reference Kirkbride, Jones, Ullrich and Coid3 We might be visualising a real environmental effect rather than just a supposed proxy.
We initially hypothesised that the observed positive association between income and grey matter volume in healthy individuals would be stronger in patients with schizophrenia because we expected poverty as an adverse factor to have a bigger effect on a vulnerable brain already affected by psychosis.Reference Walker, Wachs, Gardner, Lozoff, Wasserman and Pollitt9 Surprisingly, this relationship was not present in patients with schizophrenia. This might be because of higher-income patients presenting with neurodevelopmental abnormalities that prevent them from benefiting from the environment. However, socioeconomic gradients in a variety of measures have been observed in patients with schizophrenia with other neurodevelopmental disorders.Reference Van Os, Kenis and Rutten23,Reference Farah24 An alternative explanation could be that developing schizophrenia is the result of an underlying biological vulnerability interacting with an adverse environmentReference Schobel, Lewandowski, Corcoran, Moore, Brown and Malaspina25: perhaps less grey matter damage (a proxy for biological vulnerability) is needed to develop a psychotic episode in a very poor (adverse) environment. Similarly, the disorder would only emerge when the grey matter damage (brain vulnerability) is such that the enriched environment cannot contain it. The anatomy of schizophrenia is not an independent process detached from the environment, but rather is inseparable from it. Conceptually, schizophrenia becomes inseparable from the ecological niche in which it presents.
The observed relationship with income was mostly a global whole-brain effect. However, further examination of this effect after accounting for the global changes showed interesting localised results. The prefrontal cortex seems to be a region that benefits highly from a more affluent environment in healthy individuals, but not in patients with schizophrenia. The association in the prefrontal cortex is in line with the cognitive profiles most related to income, particularly executive functions.Reference Pajonk, Wobrock, Gruber, Scherk, Berner and Kaizl26 This does not mean that a more affluent environment has no effect on patients with schizophrenia because, after accounting for the global effect, patients showed a significant correlation with income in right hippocampal volume. The hippocampus has been highlighted as a critical region in the neuropathology of schizophrenia.Reference Koutsouleris, Kambeitz-Ilankovic, Ruhrmann, Rosen, Ruef and Dwyer27 However, it is also interesting to note that plastic hippocampal volume changes have been observed with other interventions in patients with schizophrenia, such as exercise,Reference McLaughlin, Sheridan and Lambert28 suggesting that the hippocampus is a target of both schizophrenia neuropathology and a favourable environment.
The brain in patients with schizophrenia in the lower-income group was more similar to that of healthy controls than in the upper-income group. This has several implications. These differences should be considered using the multivariate approaches under development that use statistical learning methods on neuroimaging data, particularly when including populations exposed to different environments.Reference Leucht, Samara, Heres and Davis29 If these environmental factors are not accounted for, algorithms developed with data from higher-income countries will only be useful for the few wealthy people in low- and middle-income countries who have similar living standards, further increasing existing inequalities. Our findings also support a new hypothesis to explain the alleged better prognosis of patients with schizophrenia in low- and middle-income countries,Reference Jablensky and Sartorius5 where psychosis would be ‘more environmental’. Supportive measures facilitating living in harsh environments might allow the normal developmental trajectory to resume.
There was also an interesting interaction between environmental violence and case that did not reach statistical significance. Patients with schizophrenia appeared more vulnerable to a violent environment, showing reduced total grey matter. It has been proposed that exposure to deprivation and violence have different neurodevelopmental effects. Our differential results of poverty and environmental violence would fit well with this framework.Reference Van Erp, Preda, Nguyen, Faziola, Turner and Bustillo30 Future studies will need to explore further the effect of environmental violence on the brain.
There are several limitations to our study. As discussed above, we characterised the environment where the participant was living, rather than assess the personal exposure to violence or poverty. Furthermore, environmental exposure (where participants lived) was obtained at the time of scanning, not considering the existence of critical periods in their exposure. Future studies might be able to address whether the observed effect of poverty depends on personal or environmental poverty, or the exposure at a specific period of life, such as childhood. Our study also included patients with schizophrenia of a wide range of ages and at different stages of the disorder. Chronicity and medication are known to have effects on brain morphology. However, we also showed that results were consistent across sites, and this heterogeneity in our participants also increased the generalisability of our findings. Environmental measures were not orthogonal to each other either. We preferred using these metrics than the new composite variables, for ease of interpretation. As described in Supplementary file 1, we also explored the effect of analysing only one environmental parameter at a time in our lineal model, with similar results. Our environmental metrics were also heterogeneous (particularly metrics looking at income), and our normalisation procedure allowed us to examine relative rather than absolute differences. Nonetheless, our study shows original data of a population living in an unequally distributed adverse environment such as Latin America, which has been poorly represented in the literature. Taking advantage of its highly contrasting living conditions, our study provides novel evidence about the environment effect on the neurobiological bases of schizophrenia.
Supplementary material
Supplementary material for this article are available online at http://doi.org/10.1192/bjp.2020.143
Data availability
The data that support the findings of this study are available from the corresponding author (N.A.C.), subject to permission from the senior author of each site (N.A.C., R.A.B., C.F.-S., C.S.G., S.M.G. and C.L.-J.), upon reasonable request.
Acknowledgement
The authors would like to thank Isabel Valli for her thoughtful comments on the manuscript.
Author contributions
N.A.C. designed the study. N.A.C., A.Z., F.R.-M., C.F.-S., L.S.C., M.N.C., A.M.D.-Z., J.A.P.-Z. performed the analyses. N.A.C., J.U., C.L.-J., S.M.G., C.S.G., C.F.-S. and R.A.B. provided senior leadership and secured funding for data acquisition in their respective centres. N.A.C., A.Z., F.R.-M., L.S.C., M.N.C., A.M.D.-Z., J.U., C.L.-J., S.M.G., C.S.G., C.F.-S. and R.A.B. wrote the manuscript. All authors contributed to data acquisition, and critically reviewed and approved the finalised manuscript. N.A.C. had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Funding
This collaboration was made possible thanks to the Programa Iberoamericano de Ciencia y Tecnología para el Desarrollo CYTED Redes to the ANDES Network (grant 218RT0547). Funding from individual studies came from different grants. Brazil: Grants Produtividade em Pesquisa from conselho nacional de desenvolvimento científico e tecnológico (CNPq) PQ-CNPq 304587/2018-4, CNPq Universal 470326/2011-5, Fundação de Amparo à pesquisa do Estado do Rio Grande do Sul (FAPERGS) 17/2551-0001 and 1009340-06/2010, FAPERGS/ CNPq PRONEM 11/2057-2 (to C.S.G.); Pós-doutorado junior CNPq 153081/2018-0 (to L.S.C.). Chile: Comisión Nacional de Investigación Científica y Tecnológica (CONICYT) National Fund for the Development of Science and Technology (FONDECYT) regular 1160736 (to N.A.C.) and 1180358 (to J.U.), CONICYT Associative Research Program (PIA) ACT1414 and ACT192064. Colombia: COLCIENCIAS call 990 (3 August 2017), Code 111577757629, Contract 781 de from 2017, PRISMA U.T (to C.L.-J.). Mexico: Consejo Nacional de Ciencia y Tecnología (CONACyT), projects182279 and 261895 (to C.F.-S.), and CONACyT's Sistema Nacional de Investigadores (to P.L.O. and C.F.-S.). None of these funding agencies had any role in the design and conduct of the study; collection, management, analysis and interpretation of the data; preparation, review or approval of the manuscript; or decision to submit the manuscript for publication.
Declaration of interest
C.F.-S. has served as a consultant for Janssen, and F.R.-M. has served as a speaker for AstraZeneca. R.A.B. reports personal fees and non-financial support from Janssen, personal fees from Pfizer, personal fees from Sanofi-Aventis and personal fees from Torrent, outside the submitted work. The other authors report no biomedical financial interests or potential conflicts of interest.
ICMJE forms are in the supplementary material, available online at https://doi.org/10.1192/bjp.2020.143.







eLetters
No eLetters have been published for this article.