Background
Nonconvulsive status epilepticus (NCSE) is common in critically ill patientsReference Dunne, Summers and Stewart-Wynne 1 and increases morbidity and mortality.Reference Shneker and Fountain 2 In patients admitted to intensive care units (ICU) continuous electroencephalogram (EEG) monitoring detected seizure activity in 19%, and almost all episodes were nonconvulsive.Reference Claassen, Mayer, Kowalski, Emerson and Hirsch 3 At the emergency department (ED), NCSE was shown to occur in more than 30% of patients with unexplained alteration of mental status.Reference Privitera and Strawsburg 4 Given the subtlety of clinical signs, the diagnosis can be missed without an EEG.Reference Alroughani, Javidan, Qasem and Alotaibi 5
Routine use of hairline EEG as a screening tool for NCSE in the ICU has not been as promising, with sensitivity of 54%Reference Tanner, Särkelä and Virtanen 6 to 72%Reference Kolls and Husain 7 for seizures and 54% for periodic lateralized epileptiform discharges with the potential to overinterpret benign patterns.Reference Kolls and Husain 7 Hence, obtaining an urgent EEG for the diagnosis of NCSE in the ICU and ED is crucial in the management. Unfortunately, it raises logistic difficulties in some hospitals. First of all, the standard procedure for application of electrodes and performing EEG recordings requires substantial training, including complex head measurement for accurate electrode placement, specific skin preparation, and application of conductive paste or glue.Reference Teplan 8 Consequently, a qualified EEG technologist must be available, even if the study is requested after day shift hours.Reference Kolls and Husain 7 This entire process takes a considerable amount of time and, in some centers, there are no EEG technologists on call. In fact, many facilities lack immediate and continuous access to EEG testing and its interpretation even during working hours, which directly affects timely treatment of NCSE. Current statistics indicate that the waiting time for a conventional EEG may be several hours to even days, especially on weekends.Reference Ganesan, Appleton and Tedman 9 , Reference Keenan and Sadlier 10 Furthermore, EEG interpretation by qualified electroencephalographers lags behind the real-time recordings by hours or days, which contribute to further delays in diagnosis and treatment.Reference Trevathan and Ellen 11
Given that NCSE treatment delay is associated with poor outcomes,Reference Shneker and Fountain 2 performing an EEG as early as possible is important. We present a simplified single-use disposable EEG headpiece system called StatNet (HydroDot, Inc., Westford, MA, USA). This is a peel-and-stick device that can be applied fast with no preparation of the scalp by a non-EEG technologist after minimal training. We compared the quality of the recordings and the ability to detect abnormal findings between the StatNet stat EEG and conventional EEG in the same group of patients. In addition, setup duration and time delay from EEG request to start of acquisition during working hours were compared. We hypothesized that StatNet EEG will be reliable and significantly faster to obtain compared with conventional EEG, without significant compromise of study quality. This method is not intended to replace the current conventional EEG; instead, it supports use after hours when there is no EEG technologist on call. In addition, StatNet can prove very beneficial in remote hospitals where services are not available.
Methods
Between September 2013 and August 2014, consecutively referred adult patients with clinical suspicion of NCSE from the ED, ICU, or hospital wards were included. This was a prospective cohort study carried out by the Saskatchewan Epilepsy Program in the Royal University Hospital, a tertiary care center in Saskatoon, Saskatchewan, Canada. Patient guardians provided written informed consent. In the majority of cases, it was not possible to obtain consent directly from patients because they were either critically ill for many days, did not have or regain an adequate level of awareness, and, in one case, the patient passed away. The study was approved by Health Canada and the Research Ethics Board at the University of Saskatchewan.
Patient Selection
Patients with the following criteria were included: 1) adults at 18 years of age or older; 2) any unexplained change or variation in behavior or level of awareness; 3) coma or significantly impaired mental status; and 4) one of the following conditions: sepsis, metabolic or toxic abnormalities including drug intoxication with stimulants (cocaine or amphetamines) and lithium, history of epilepsy, witnessed seizures without regaining baseline mental status within 30 minutes, cardiac arrest, clinical features suspicious for status epilepticus such as gaze deviation or nystagmus, mini-myoclonus of fingers, ischemic or hemorrhagic stroke, traumatic brain injury, brain tumor, and central nervous system infection. Neurologists, neurology residents, and emergency physicians received a practical training session for identifying the appropriate patients. They informed the epilepsy fellow during the day shift hours about the patients’ clinical history and possible inclusion criteria by a telephone call, without neurologic consultation. They also sent a simultaneous request for a conventional EEG to the Neurophysiology Department. After the call, the epilepsy fellow would attend the patient’s bedside as soon as possible to perform the StatNet EEG. Every patient also underwent a routine conventional EEG during the same day.
StatNet and Conventional EEG Setup
The epilepsy research fellow placed the StatNet electrodes on the patient’s head. The fellow received 3 hours of training on how to apply the StatNet EEG electrode set on a dummy’s head with hair and how to set up the portable EEG amplifier and the laptop computer for rapid acquisition. The StatNet EEG montage consisted of a longitudinal and transverse bipolar montage without F3, F4, P3, P4, and Pz electrodes. To provide adequate coverage of the parietal region, the lowest posterior electrode line (T5, T6, O1, and O2) is slightly shifted anteriorly (Figure 1A).

Figure 1 (A) StatNet electrode positions. The StatNet headpiece has fewer electrodes compared with that of a conventional EEG (18 instead of 23); however, it has adequate coverage of all the major areas of the brain. It uses a modified international 10-20 system placement: FP1, FP2, F7, F8, T3, T4, T5, T6, O1, O2, C3, C4, FZ, CZ, A1, A2, REF, and GND. The electrode positions are at approximately 5% to 10% of each 10-20 location and are homologous. The posterior electrodes are slightly higher to make it easier to apply to patients in the supine position (www.biosignalgroup.com). Permission has been obtained for use of the submitted figure. (B) Two-piece design StatNet set. The StatNet “peel and stick” EEG disposable headpiece is a pregelled, two-piece, soft-layered integrated circuit connected with a single integrated cable (www.biosignalgroup.com). Permission has been obtained for use of the submitted figure.
After obtaining informed consent, the patient’s largest head circumference (HC) was measured at the level of the nasion and inion to choose the appropriate electrode set size. StatNet electrode sets come in medium and large sizes. Based on manufacturer recommendation, for HC ≤56 cm, a medium set was used; for HC >56 cm, a large set was used. The fellow then applied the two-piece designed set (Figure 1B) of disposable single-use electrodes by peeling and sticking it on the patient’s scalp. Each electrode was housed under foam padding soaked with conducting gel, thus eliminating the need for cumbersome scalp preparation and application of conducting paste. The silver chloride electrodes are integrated with lead wires, resulting in low ambient noise. The wires were connected to Xltek Trex ambulatory EEG system (Natus Medical Inc, San Carlos, CA, USA), which was then hooked up to a laptop. Although StatNet EEG can provide quality recordings for 4 hours before the conductive gel dries, each recording was conducted for 20 minutes. After the procedure, the epilepsy fellow removed and discarded the electrode set. The EEG traces were potentially uploadable to a central secure EEG server, which could then be accessed remotely by an on-call electroencephalographer. Results could potentially be communicated via telephone to the requesting physician to guide clinical care. However, for the proof of concept stage, the StatNet EEGs were stored on the recording laptop for future comparison with the conventional EEGs; clinical guidance was provided after the interpretation of the conventional EEG by an electroencephalographer.
Trained and board-certified EEG technologists applied electrodes according to the conventional method for EEG in the same group of patients on the same day. All recordings were carried out on a 32-channel digital EEG acquisition system (Xltek, Natus Medical Inc). The scalp electrodes were placed according to the International 10-20 measurement system using standard gold-plated cup electrodes with conductive paste secured in place with Hypafix and wrapped to conform. Anteroposterior longitudinal bipolar montage was displayed during these digital recordings. Standard activation procedures were employed whenever possible. Each EEG recording was conducted for 30 minutes per Canadian standards. Technologists and the epilepsy fellow documented the setup time in minutes. In addition, the time delay from order to execution of StatNet EEG and the conventional EEG were documented. Chart review of each case was carried out to obtain clinical data including the indication for EEG order and the referring diagnosis. The fellow who performed the StatNet test reassessed the physical examination at the time of the conventional EEG to ensure the clinical possibility of NCSE at the beginning of every test (looking for minimal clinical findings such as nystagmoid eye movements and finger mini-myoclonus).
EEG Interpretation
Two independent board-certified electroencephalographers (FM-A and JFT-Z) reviewed the conventional EEGs and StatNet EEGs in a blinded fashion. The process of blinding was undertaken by the epilepsy fellow, who converted all EEG montages to the StatNet montage (Figure 2A-D). The tests were randomly coded, and all names, information, and annotations inserted by the technologist were removed. In addition, the duration of all studies was adjusted to the first 20 minutes. The fellow included a short sentence summarizing patients’ information including age, sex, and the reason for the study. To keep the studies blinded, the electroencephalographers were not allowed to change the settings or the montage during the reading. The EEG readers were asked to assess each study in four aspects: 1) whether the study was interpretable; 2), the presence of artifact in percentage during the recording; and 3) the presence of epileptiform discharges and slowing and, if present, whether they were focal or generalized—if focal, the location, side, and specific patterns such as periodic lateralized epileptiform discharges, frontal intermittent rhythmic delta activity, or temporal intermittent rhythmic delta activity were noted. Triphasic waves and coma patterns (e.g. spindle coma, alpha coma, theta coma, delta coma, burst-suppression) were also identified. Finally, each EEG reader decided whether the EEG was positive for NCSE. The definition of NCSE proposed by Walker et al in 2005 was used.Reference Walker, Cross and Smith 12 Electrographic seizure was defined as repetitive generalized or focal spikes, sharp waves, spike-and-slow wave, or sharp-and-slow wave complexes at frequency greater than 3 Hz or sequential rhythmic, periodic, or quasi-periodic waves at frequency greater than 1 Hz with definite evolution in frequency, morphology, or location lasting at least 10 seconds.Reference Chong and Kirsch 13 Their interpretations were then compared with the known diagnosis.

Figure 2 NCSE in two patients. EEG set up on a longitudinal and transverse bipolar montage. Scale represents 1 s and 50 μV. (A, B) A continuous left frontotemporal 0.5- to 2-Hz sharp wave activity without clinical manifestations in the patient 1 in a conventional and StatNet EEG, respectively. (C-D) A diffuse sharp wave periodic pattern at a frequency of 0.5 to 1 Hz with maximum activity over the right frontal area in the patient 2 in a conventional and StatNet EEG, respectively.
Analysis
We calculated the agreement between two readers using the kappa coefficient. The interpretation of the kappa values was done according by Landis and Koch.Reference Landis and Koch 14 We compared the time from EEG order request to start of the EEG acquisition and the setup time between both tests (StatNet and conventional) as well as the amount of artifact and ability to detect abnormal findings. Nonparametric Mann-Whitney t test was used for comparison. Results are expressed in median minutes ± standard error of the median. The statistical analysis of the data was performed using commercially available software (SPSS 20; Chicago, IL, USA). The level of significance was set to p<0.05.
Results
Over 10 months, 19 patients were evaluated. The mean age was 61±16.3 (25 to 93) years and 63% of the patients were female. The clinical characteristics of the sample are displayed in Table 1. The majority of the EEG requests came from the ICU and ED; clinical histories were predominantly consistent with an underlying neurological condition (84%). Non-neurological cases accounted for 16% of the total: drug intoxication (11%) and sepsis (5%). Six (32%) patients carried a long-standing epilepsy diagnosis and half of them (16%) had a history of convulsive status epilepticus. These six patients with known epilepsy diagnosis had witnessed tonic-clonic seizure activity lasting more than 5 minutes, five (83%) of them had also witnessed seizure without return of mental status to baseline, and three (50%) had positive semiologic findings in the neurological examination suggestive of NCSE. In general, the mean time of mental status depression before the admission was 22±15 (1 to 48) hours. The neurological examination was similar between the two studies.
Table 1 General characteristics of the patients

CNS = central nervous system; ED = emergency department; ICU = intensive care unit; NCSE = nonconvulsive status epilepticus.
* Patients highly suspected of having NCSE (convulsive seizures followed by unconsciousness)
~ The patient has a stable intracranial hemorrhage or ischemic stroke but declines from a Glasgow Coma Score of 12 to 7
EEG Validity and Utility
The inter-observer agreement for the decision of interpretability was almost perfect for StatNet (kappa=1.0, p<0.0001) and moderate for the conventional group (kappa=0.76, p<0.002). The concordance for the detection of abnormal findings was almost perfect for StatNet EEG (0.83) and moderate for conventional EEG (0.75, p<0.0001). The inter-observer agreement in regard to the final diagnosis (normal, encephalopathy, and epileptiform activity) was moderate for StatNet (kappa=0.7, p<0.0001) and conventional EEG (kappa=0.6, p<0.0001).
There was no difference between the two interpreters in regard to the presence of epileptiform activity. NCSE was detected in 10% (two of 19 patients) with both studies (Figure 2). Both patients were treated and improved with antiepileptic drugs in the ICU. EEG was normal in 10% of patients; showed interictal epileptiform discharges that did not evolve into seizures in 10% (one was a pattern of generalized discharges in a patient with idiopathic epilepsy and suspicion of absence status; the other was a left temporal epileptogenic focus in a patient with a brain tumor); indicated NCSE with periodic discharges in 10%; generalized slowing suggestive of underlying encephalopathy in 60%, and noninterpretable study in 10%, with both StatNet EEG and conventional EEG. There were no patients with clinical seizures during the tests.
EEG Timing and Quality
The mean delay time from EEG order to EEG acquisition was 22.42±2.53 minutes for the StatNet group and 217.74±44.60 minutes for the conventional group; the difference was significant (p<0.0001, Mann-Whitney U=23) (Figure 3). The mean setup time was 9.98±0.86 minutes for the StatNet group and 17.88±0.81 minutes for the conventional group; the difference was significant (p<0.0001, Mann Whitney U=7) (Figure 4).
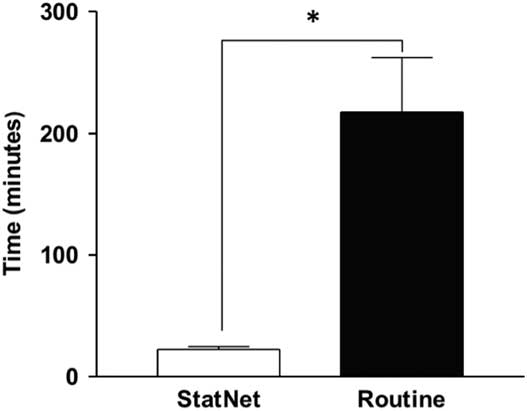
Figure 3 Delay from EEG order to EEG recording.

Figure 4 Comparison of setup time between StatNet and conventional EEG.
No difference was noted in the quality of the recordings or the duration of artifacts between the StatNet EEG and the conventional EEG groups. The first EEG reader reported a similar percentage of artifacts in the StatNet and the conventional groups (61±37% vs. 52±42%, p>0.05). The second electroencephalographer reported fewer artifacts in both tests, but there was no difference between the StatNet and the conventional groups (23±26 vs. 27±34, p>0.05). Overall, there was no difference in the percentage of artifacts during the recording between StatNet and conventional EEG, respectively (42% vs 39%, p>0.05).
Discussion
To the best of our knowledge, there is no prospective study to date that compares the value of StatNet EEG and conventional EEG performed in the same group of patients with suspected NCSE. Our study suggests that StatNet EEG electrode set performs similarly to conventional electrodes in the urgent setting for patients suspected of having NCSE. At the same time, we demonstrated that StatNet EEG has the advantages of being readily available and reliable. In our study, the disposable StatNet EEG electrode set allowed medical staff to fit it to the patient’s scalp in less than 10 minutes on average and obtain an acceptable recording.
NCSE can occur after clinically treated convulsive status epilepticusReference DeLorenzo, Waterhouse and Towne 15 , Reference Drislane, Lopez, Blum and Schomer 16 ; nevertheless, only in 25% of the cases did noticeable clinical seizures precede EEG diagnosis of NCSE.Reference Laccheo, Sonmezturk and Bhatt 17 Critically ill patients with unexplained alteration of mental status in ICU and ED might also suffer this condition. Epileptic activity was recently found in the EEG of almost half of patients with acute impairment of consciousness,Reference Ricardo, França, Lima, Yassuda and Cendes 18 and it has been demonstrated that delayed diagnosis and treatment of NCSE may lead to increased neurological complications and mortality.Reference Drislane, Lopez, Blum and Schomer 16 , Reference Firosh Khan, Ashalatha, Thomas and Sarma 19 There is currently no standardized protocol for identifying the patients with suspected NCSE, and no after-hours urgent EEG availability even in some tertiary care centers.Reference Abend, Dlugos, Hahn, Hirsch and Herman 20 StatNet EEG could be a solution to this problem, and a more universal use of handy full-montage quick electrode sets may help lower morbidity and mortality in this population. This could potentially save health care dollars while increasing availability of testing allowing for earlier treatment of NCSE. However, more prospective studies are required to assess this possibility.
Our study detected NCSE on stat EEG in 10% of patients, similar to earlier reports. Varelas et alReference Varelas, Spanaki, Hacein-Bey, Hether and Terranova 21 executed a retrospective study in patients with change in mental status or coma. They reported that 11% of stat EEGs showed NCSE. With similar findings, AlroughaniReference Alroughani, Javidan, Qasem and Alotaibi 5 described a rate of 9% in patients with unknown cause of impaired level of consciousness, and Bastani et alReference Bastani, Young and Shaqiri 22 described subclinical epileptiform activity in 12% of patients studied with a screening EEG device in the ED. More recently, Brenner et alReference Brenner, Kent, Wojcik and Grant 23 found nonconvulsive seizure activity in 8% of patients when comparing a portable six-lead Brainmaster EEG device with conventional EEG. However, the detection of NCSE in stat EEG varies widely between studies. It has been as low as the study published by Seidel et al,Reference Seidel, Aull-Watschinger and Pataraia 24 who found an incidence of 0.8% among 2514 consecutive patients in a tertiary center, and the series by LorenzlReference Lorenzl, Mayer, Feddersen, Jox, Noachtar and Borasio 25 and Zehtabachi,Reference Zehtabchi, Abdel Baki and Omurtag 26 which confirmed NCSE in only 5% of patients with altered consciousness at a palliative care center and ED, respectively. On the contrary, Privitera and StrawsburgReference Privitera and Strawsburg 4 found NCSE in 34% of patients who presented with altered consciousness and Praline et alReference Praline, Grujic and Corcia 27 reported that 20% of stat EEG in emergency situations confirmed the presence of NCSE. The low rates of some studies could be due to using only 20 minutes or shorter stat EEGs and not continuous EEGs. It has been well described that electrographic seizures or NCSE in critically ill patients can be better detected using continuous EEG monitoring. In fact, the sensitivity increased to 80%–90% by extending the recording time to 24–48 hours.Reference Claassen, Mayer, Kowalski, Emerson and Hirsch 3 , Reference Alroughani, Javidan, Qasem and Alotaibi 5 , Reference Claassen, Jette and Chum 28 , Reference Narayanan and Murthy 29 Other bias to take into account is the selection of patients; in more acutely complicated and elderly patients, the possibility of diagnosis is higher.Reference Seidel, Aull-Watschinger and Pataraia 24 , Reference Zehtabchi, Abdel Baki and Omurtag 26 , Reference Praline, Grujic and Corcia 27
As was expected, in our series, StatNet EEG was frequently requested in patients older than age 50 years (84%) and often located in the ICU and ED (90%). Both findings are quite similar to another prospective study done on 111 consecutive stat EEG recordings in which 60% of patients were between the ages of 50 and 70 years and two-thirds of them came from the ICU and ED, possibly because this group of patients is especially exposed to acute medical problems and neurological disorders.Reference Praline, Grujic and Corcia 27
Finally, the majority of patients in our study (60%) showed a diffuse polymorphic slowing. This finding is comparable with earlier reports in which diffuse slowing was seen in half of the ICU-ordered stat EEGsReference Zehtabchi, Abdel Baki and Omurtag 26 , Reference Varelas, Hacein-Bey, Hether, Terranova and Spanaki 30 and up to 70%Reference Lepola, Myllymaa and Töyräs 31 of ED patients with alteration of mental status. Although slowing is a nonspecific manifestation of cerebral dysfunction, its magnitude may correlate with the functional severity of clinical encephalopathy.
Each StatNet electrode set costs $100. Because StatNet is performed by a physician and not a technologist, it could potentially save costs associated with calling back a technologist after hours. In addition, StatNet EEG may potentially save money by earlier patient discharge from the ED or an overall shorter duration of hospital stay; however, our study was not designed to assess such parameters. In the future, if this device achieves approval from Health Canada, more studies could be designed to look at cost effectiveness of using StatNet EEG in the ED or in remote areas.
Limitations
This study has a few limitations. The main limitation is the small sample size, although the sample size is reasonable for a pilot study designed to assess feasibility and validity of StatNet EEG compared with conventional EEG. We believe that this objective was accomplished in our study. We did not identify patients who received anticonvulsant medications before the recording or in between StatNet and conventional EEG, which could potentially change the electrical findings. We did not study the clinical benefits of stat EEGs in this study because it was a feasibility study only. The potential therapeutic benefit of StatNet EEG could be assessed in a prospective study. StatNet EEG and conventional EEG were not recorded at the same time and, potentially, some patients in NCSE on one test may not be in NCSE later. Fortunately, in our study, all patients with NCSE were correctly diagnosed with both tests. Finally, it is likely that emergency physicians referred patients with higher pretest probability of NCSE for enrollment and not every patient with alteration of mental status was referred; subjecting the study to a sampling bias. However, this will not affect the comparison between the two studies.
Conclusion
StatNet EEG is a practical and reliable test when compared with conventional EEG for detection of NCSE. It reduces the delay in testing and treatment in patients suspected of having NCSE, in particular, after hours when there is limited or no access to EEG services. The StatNet method does not replace conventional EEG; however, it can be beneficial by providing earlier assessment. Future studies with larger patient populations may assess the clinical outcomes of patients assessed with StatNet and the use of this device in remote hospital settings.
Acknowledgments
We thank the physicians, nurses, and electroencephalogram (EEG) technologists of the Royal University Hospital emergency department and intensive care unit for their cooperation in this study, particularly the EEG technologists who performed the conventional EEGs.
Disclosures
FM-A has served as a researcher and has received research grants from the College of Medicine of the University of Saskatchewan, the Saskatchewan Health Research Foundation (SHRF), and Ralston Brothers Research Trust. JFT-Z has served as a researcher and has received research grants from the University of Saskatchewan and the Royal University Hospital Foundation. AV,DD, LDL, WS, and LH-R do not have anything to disclose.







