Introduction
It is estimated that 38% of all ambulance transports are for adults aged 65 or older, despite only comprising 13% of the population.Reference Jones, Wasserman, Li, Amidon, Abbott and Shah 1 , Reference Shah, Bazarian and Lerner 2 The size of the older adult population is growing. By the year 2050, it is estimated that there will be over 84 million adults 65 years of age and older in the United States. 3 This increase in the older adult population has the potential to place strains on the ambulance-based Emergency Medical Services (EMS) system as the rate of EMS utilization among older adults is nearly four-times higher than adults less than age 65 (167 per 1,000 versus 39 per 1,000).Reference Jones, Wasserman, Li, Amidon, Abbott and Shah 1
The association between older age and increased frequency of EMS use as a mode of transportation to the emergency department (ED) compared to younger adults is well-documented. 4 - Reference McConnel and Wilson 15 Among ED patients, older age has been associated with an increase in perceived medical necessity,Reference Dickinson, Verdile, Kostyun and Salluzzo 16 injury or illness severity,Reference Wofford, Moran, Heuser, Schwartz, Velez and Mittelmark 12 , Reference Dickinson, Verdile, Kostyun and Salluzzo 16 poor social and physical function,Reference Dickinson, Verdile, Kostyun and Salluzzo 16 comorbidities,Reference Gerson and Shvarch 8 and insurance status, all of which may lead to increased EMS use. 4 , Reference Wofford, Moran, Heuser, Schwartz, Velez and Mittelmark 12 , Reference Ruger, Richter and Lewis 13 Previous research studies evaluating the effect of older age on transportation to an ED via an ambulance have been retrospective, have not collected the breadth of information necessary for a complete analysis, have not used statistical methods to control for potential confounding variables, or have been performed in unique sub-populations. Thus, these factors may confound the association between older age and EMS use, potentially leading to false conclusions about the extent of EMS use among older adults compared to younger adults. Elucidating the relationship between increased age and mode of ED arrival is important, as this information may help inform the development of targeted community strategies designed to provide efficient provision of timely EMS care.
The purpose of this study was to test the association between age and mode of ED arrival while controlling for confounders in a cross-sectional sample of patients who presented to the ED. Additionally, common reasons for using EMS reported by both younger and older adults were identified.
Methods
A cross-sectional survey study was conducted in the University of Rochester Medical Center’s Strong Memorial Hospital ED (Rochester, New York USA) from September 2010 through June 2011. Strong Memorial Hospital is a 900-bed academic medical center. The 2014 population of the greater Rochester metropolitan area was approximately 1.5 million people, consisting of six counties, and the following demographic characteristics: 16% aged greater than 65; 51% female; 77% white; and 14% living below the poverty line.Reference Shah, Glushak and Karrison 17 The Strong Memorial Hospital ED serves as the region’s primary tertiary care center and Level I trauma center. The ED serves a nine-county catchment area, including rural, suburban, and urban communities and provides care to patients with a broad range of acuities and chief complaints. The ED treats over 100,000 patients annually with approximately 85% of patients being adult (age ≥18), nine percent Hispanic, and 41% non-white. The University of Rochester’s Research Subjects Review Board approved the conduct of this study.
Eligibility criteria included being an ED patient, age ≥19 years, presence of decisional capacity, and an ability to read and understand English. Prisoners, psychiatric patients, sedated patients, and critically ill patients, as defined by an Emergency Severity Index (ESI) of one, were excluded from participation. Patients residing in institutional settings, such as skilled nursing facilities and assisted living centers, were excluded from the present analysis as these patients are not consulted during the decision-making process regarding emergency transport modes due to facility policies.
During the study period, research assistants screened all ED patients for eligibility and completed a subject log which recorded basic demographic and clinical information of all patients screened for eligibility. Eligible patients were approached for participation and an information letter was distributed. After gauging participant interest, decisional capacity was evaluated using a standardized instrument that was developed by the principal investigators (CMCJ and MNS).
Eligible and consenting participants were interviewed using a cross-sectional survey that was designed by members of the study team and expanded upon a similar previously conducted study in the pediatric population. 18 The survey was adapted for use in the adult population, with specific questions relevant to the older adult population. The survey was interviewer-administered and contained detailed questions about the subject’s medical history, chief complaint, self-perceived illness severity, demographics, and mode of arrival to the ED (ambulance versus other means). All variables were based on patient self-report, including comorbid medical conditions and history of depression and anxiety. Subjects who arrived to the ED via EMS also were asked specific questions regarding reasons why they opted to call an ambulance for their current illness/injury. The survey was pre-tested and pilot-tested prior to administration. A standardized medical record review process was developed and research assistants abstracted patient acuity levels as well as other clinical information from each patient’s electronic medical record.
Data were analyzed using SAS 9.3 (SAS Institute, Inc.; Cary, North Carolina USA). To capture a wider range of an aged population, age was classified into three categories:<55, 55-79, and ≥80. There is no gold standard for classifying subjects into age-based categories. Three age strata were selected to improve interpretability of the results versus evaluating age as a continuous variable. Further, the three categories allowed for evaluation of linear effects versus simply dichotomizing age. The oldest category of ≥80 years was selected based on previous EMS researchReference Shah, Davis, Bauer and Arnold 19 and limitations of the sample size. A Cochrane Armitage test for linear trend was used to assess the crude relationship between increasing age and arrival to the ED via EMS. Bivariate analyses were conducted with all relevant subject characteristics and the outcome variable (mode of ED arrival) and are presented in Table 1. All covariates associated with the outcome (P<.20) were evaluated for confounding effects in a multivariable regression model. Logistic regression modeling was deemed inappropriate due to the large proportion of subjects who arrived to the ED via EMS, as the odds ratio will overestimate the true association when the outcome is common.Reference Munjal, Shastry and Loo 20 , Reference Greenland 21 To address this, a multivariable Cox regression model was developed and specified a constant time at risk. Although Cox regression is traditionally used to model time-to-event data, if the time at risk is constant for all subjects, the hazard ratio will closely approximate the prevalence ratio in cross-sectional studies.Reference McNutt, Wu, Xue and Hafner 22 A manual change-in-estimate model building approach was used to evaluate the effect of confounding variables.Reference Barros and Hirakata 23 Covariates that changed the beta coefficient appreciably (≥10%) for any level of the primary exposure variable (age category) were retained in the final model.Reference Greenland 24 To increase model precision, all statistically significant (P<.05) predictors of mode of ED arrival were included in the final regression model. Reasons for using an ambulance for transportation to the ED were quantified using proportions. Associations between reasons for arriving via EMS and age were evaluated using chi-square tests, using Fisher’s exact test where appropriate.
Table 1 Subject Characteristics Stratified by Mode of ED Arrival (n=1,058)

Note: All variables from Table 1 were evaluated in bivariate analysis for inclusion in the multivariable model.
Abbreviations: ED, emergency department; EMS, Emergency Medical Services; ESI, Emergency Severity Index.
a Cochran-Armitage Test for Trend.
b P value <.20; evaluated as a confounder in multivariable Cox regression model.
c Chief complaint categories were collapsed into a composite variable indicating high- and low-risk for ambulance transport. High-risk chief complaints included: cardiac, injury, neurologic, syncope/near syncope, and low-risk chief complaints included: anemia, gastrointestinal, genitourinary, infection, metabolic, pain, and other non-life threatening conditions.
Results
Data from 1,058 subjects were analyzed (Figure 1). Characteristics of the study sample are presented in Table 1. The median age of the sample was 61 years. Of those included in the analysis, 42% (n=449) arrived to the ED via EMS. Characteristics of those included in the analysis did not differ significantly from characteristics of individuals who refused participation (data not shown).

Figure 1 Subject Enrollment Abbreviations: ED, emergency department; EMS, Emergency Medical Services.
There was a statistically significant linear trend in the proportion of subjects who arrived via EMS by increasing age (Cochran-Armitage Test; P<.001); among individuals aged<55, 55-79, and ≥80 years, 36.7%, 43.3%, and 56.6% arrived to the ED via EMS, respectively. Compared to adults<55 years, the unadjusted prevalence ratio associating age and EMS use was 1.18 (95% CI, 0.96-1.45) for subjects 55-79 years and 1.54 (95% CI, 1.18-2.02) for subjects ≥80 years (Table 2).
Table 2 Evaluation of Confounding Variables in the Association between Age and Mode of ED Arrival (n=1,058)

Abbreviations: APR, adjusted prevalence ratio; ED, emergency department; PR, prevalence ratio.
a Chief Complaint and self-perceived illness severity were not identified as confounders, but were statistically significantly (P<.05) associated with mode of ED arrival and were included in the final model (Model 4) as they were statistically significantly associated with the outcome.
On bivariate analyses, subjects who arrived to the ED via EMS tended to be of older age, high-acuity, high-risk chief complaints, lower education, resided alone, did not reside in a single-family home, had more chronic medical conditions, higher self-perceived illness severity, worse self-rated health, sought medical attention when ill, and had a history of depression (P<.20). Statistically significant effect measure modifiers were not identified. The effect of these potentially confounding variables on the association between age and mode of ED arrival was assessed using multivariable regression modeling (Table 2). Number of chronic medical conditions and history of depression confounded the association between age and mode of ED arrival. As shown in Model 1, after adjustment for number of chronic medical conditions, the association between age and mode of ED arrival was attenuated with subjects aged 55-79 having a prevalence ratio of 1.10 (95% CI, 0.89-1.36) and subjects aged ≥80 having a prevalence ratio of 1.43 (95% CI, 1.09-1.88) compared to adults less than age 55. History of depression also was identified as a confounder; however, after its inclusion in Model 2, the effect estimates for age increased, especially for subjects age 80 or older (adjusted prevalence ratio: 1.62; 95% CI, 1.23-2.13). Model 3 included age, number of chronic medical conditions, and history of depression. The fully adjusted model, Model 4, included age, the identified confounders, as well as chief complaint and self-perceived illness severity, which were statistically significantly associated with mode of ED arrival. The final model showed that the effect of age on mode of ED arrival was attenuated but remained statistically significant after adjustment for these covariates with subjects aged 55-79 having a prevalence ratio of 1.14 (95% CI, 0.92-1.41) and subjects aged ≥80 having a prevalence ratio of 1.44 (95% CI, 1.09-1.90) compared to adults less than age 55.
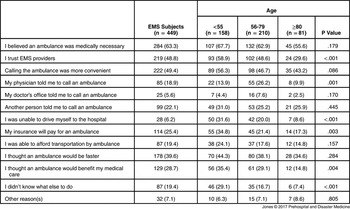
Reasons for arriving to the ED via EMS were stratified by age group (Table 3). The most commonly endorsed reasons for arriving to the ED via ambulance among the entire sample included belief that an ambulance was medically necessary (63%), trust in EMS providers (49%), and convenience (49%). There were statistically significant differences in reasons for arriving to the ED via ambulance among younger and older adults. Compared to older adults, younger adults were significantly more likely to endorse the following reasons for EMS transport: trust in EMS providers, unable to identify other means of transportation, insurance provides coverage for ambulance transportation, belief that EMS would benefit their medical care, and not knowing what else to do (P<.05). There also was a statistically significant difference in the proportion of subjects reporting his/her physician instructed him/her to call for an ambulance, with 26% of subjects aged 55-79 answering affirmatively compared to only 14% and 10% of subjects aged<55 and ≥80, respectively.
Table 3 Reasons for Calling EMS, Stratified by Age group (EMS Subjects Only, n=449) [n (%)]
Abbreviation: EMS, Emergency Medical Services.
Discussion
This study aimed to determine the independent effect of older age on EMS use for transport to the ED by controlling for confounders in a large sample of ED patients. The results of this study showed the proportion of subjects arriving via EMS increased linearly with age, consistent with previous literature which has consistently demonstrated increased frequency of EMS use among the older adult population in unadjusted analyses.
In the multivariable analysis, the effect of older age on EMS transportation to an ED remained statistically significant, with the proportion of subjects arriving to the ED via EMS in the oldest age category (≥80 years) being 44% higher compared to subjects less than age 55. It was hypothesized that, after adjustment for patient-level factors, the association between age and mode of ED arrival would no longer be statistically significant; however, this was not supported by the results of the present study. The effect of increasing age on mode of ED arrival was confounded by number of chronic medical conditions and history of depression. However, adjustment for these variables did not eliminate the effect of age on mode of ED arrival. Both number of chronic medical conditions and history of depression have been identified as predictors of increased ED use in previous studies, providing face validity to these findings. 4 , Reference Gerson and Shvarch 8 , Reference Dickinson, Verdile, Kostyun and Salluzzo 16 The confounding effects of these patient characteristics have important implications for research related to emergency care of the older adult population and the perceived burden older adults place on EMS care.
As hypothesized, the results demonstrated that the effect of older age on EMS transport to an ED was attenuated after adjustment for number of chronic medical conditions. Thus, failure to adjust for chronic medical conditions in previous studies likely provided an overestimate of the effect of older age on mode of ED arrival. Conversely, the magnitude of the effect of older age on mode of ED arrival increased after adjustment for history of depression; thus, indicating the effect of older age would likely be an underestimate in studies that fail to adjust for depression. These two variables confounded the association in different directions, ultimately yielding similar results in the fully adjusted analysis and the unadjusted model. This suggests that while previous studies did not control for these factors, the combined effect of these two factors provides an adjusted effect estimate similar to the crude effect estimate.
Numerous other patient characteristics were explored for confounding effects and no other variables were found to appreciably influence the effect of age on mode of ED arrival. Although an attempt was made to evaluate the potential confounding effect of many patient characteristics, the possibility of residual confounding remains a concern. Insurance status, functional status, and availability of transportation are three important potential confounders that were not evaluated in the present analyses. Data were not collected on these variables and thus, were unable to determine the effect of these variables on mode of ED arrival. An indicator variable was created for subjects aged 65 or older, as these individuals would be eligible for Medicare, and it did not influence the effect of age on mode of ED arrival. Adjustment for availability of primary care and other transportation means could further attenuate the effect of age on mode of ED arrival; however, among subjects who arrived to the ED via EMS, lack of transportation was not commonly endorsed as a reason for opting for ambulance transportation.
Since the older adult population is growing rapidly, it is essential to understand the reasons why older adults more frequently use EMS for transportation to an ED as compared to their younger counterparts. Identification of such factors may provide insight into resource allocation and staffing for local EMS agencies with a high proportion of community-dwelling older adults residing in their jurisdiction. It was hypothesized that factors such as lack of transportation and medical necessity would be more commonly endorsed among older adults compared to younger adults. Among all subjects, the most commonly cited reasons for arrival to the ED via ambulance included perceived medical necessity, trust in EMS, and convenience. These are reasons that are not traditionally measured or collected but were endorsed by approximately one-half of the study sample and are an area in which future research is warranted. Interestingly, the only variable in which older adults were more likely to answer affirmatively than younger adults was the patient’s physician instructed him/her to call an ambulance, with 26% of subjects aged 55-79 answering affirmatively compared to only 14% of subjects aged less than 55. Primary care physicians (PCPs) may instruct a patient to go to the ED for many reasons, such as patient complexity, lack of available appointments, practice policy, and the relative ease of sending patients to the ED.Reference Mickey and Greenland 25 However, reasons for PCP recommendation for EMS transportation to the ED are largely unknown and may be a function of ensuring safe transport for acutely ill patients or miscommunication between the patient and PCP regarding the immediacy of their medical condition.
There were statistically significant differences in other reasons for EMS use between younger and older adults; however, younger adults were more likely to answer affirmatively to these questions as compared to older adults, thus limiting the ability to identify potential reasons for higher rates of EMS utilization among older adults. Previous research has identified personality traits, including agreeableness and higher extroversion, to be associated with increased odds of ED use among older adults.Reference Cunningham 26 Further, research of Medicare enrollees indicated that inadequate health literacy is associated with increased ED use. 4 , Reference Wofford, Moran, Heuser, Schwartz, Velez and Mittelmark 12 , Reference Ruger, Richter and Lewis 13 It is possible that differences in generational intrinsic qualities not assessed via the survey instrument may be driving the higher rates of EMS use for transportation to an ED among the older adult population. Qualitative research may be useful for hypothesis generation to better identify potential reasons for this association, which can then be examined in future quantitative studies.
Limitations
There are important limitations to the study. This study used a convenience sample from an urban academic medical center’s ED, which may affect the generalizability of results. This is likely somewhat mitigated due to the large catchment area and diverse patient population of the ED in which subject recruitment occurred. Furthermore, although this ED is the region’s tertiary care and specialty center, the ED serves patients of all acuities and chief complaints. Second, there are potentially important confounders that could not be considered in the present analysis due to lack of data. Future research should explore the effect of other patient- and system-level characteristics on this association. Additionally, due to the self-reported nature of the data collection, there is potential for bias with respect to some of the covariates used in the present analysis. The primary independent and dependent variables in the present analysis were collected via self-report and confirmed in the ED electronic medical record. Lastly, there is no accepted gold standard for age to classify patients as older adults. As such, three age strata were used that represented a spectrum of an aged population which allowed the evaluation of linear effects with increasing age. Age greater than 80 years was used to classify subjects as oldest-old based on the available sample size and previous EMS research.Reference Shah, Davis, Bauer and Arnold 19 Simply dichotomizing age based on the traditional cutoff of 65 years would not allow for such comparisons. However, the sample size limited the ability to use smaller age strata and still have the ability to adjust for relevant covariates.
Conclusion
Among participants in this sample, older age was a statistically significant and independent risk factor for mode of ED arrival, even after controlling for confounding effects of number of medical comorbidities and history of depression. Common reasons for arrival to the ED via EMS included perceived medical necessity, trust in EMS, and convenience; however, these reasons do not explain higher rates of EMS use among older adults, as they were more commonly endorsed by younger adults. Future research is needed to further explore reasons for higher rates of EMS use among the older adult population.






