Introduction
People with mental illness often suffer from long-lasting psychiatric symptoms, despite treatment with medication or psychotherapy, resulting in lower social functioning and lower quality of life [Reference Patel, Saxena, Lund, Thornicroft, Baingana and Bolton1, 2]. They also experience impaired physical health since they have a 1.4–2 times higher risk to develop cardiometabolic diseases and have a lower life expectancy, which is partly caused by unhealthy lifestyle habits [Reference Plana-Ripoll, Weye, Momen, Christensen, Iburg and Laursen3–Reference Firth, Siddiqi, Koyanagi, Siskind, Rosenbaum and Galletly5]. People with mental illness are less physical active, tend to smoke more, and eat less healthy [Reference Firth, Siddiqi, Koyanagi, Siskind, Rosenbaum and Galletly5]. Interventions aiming to improve lifestyle habits, for example, increasing physical activity and smoking cessation, can improve mental and physical health across a range of diagnoses [Reference Firth, Siddiqi, Koyanagi, Siskind, Rosenbaum and Galletly5, Reference Firth, Solmi, Wootton, Vancampfort, Schuch and Gilbody6]. Therefore, international guidelines, including from the World Health Organization and the European Psychiatric Association advice lifestyle interventions in the treatment for mental illness [Reference Stubbs, Vancampfort, Hallgren, Firth, Veronese and Solmi7–10]. For mild–moderate depression, physical activity interventions are even recommended as first-line treatment [Reference Stubbs, Vancampfort, Hallgren, Firth, Veronese and Solmi7], and a meta-review on lifestyle psychiatry stated that physical activity interventions can be used as prevention and treatment for mental illness [Reference Firth, Solmi, Wootton, Vancampfort, Schuch and Gilbody6]. Moreover, The Lancet Psychiatry commission on protecting physical health in people with mental illness advised that lifestyle interventions should be available from patient’s first presentation to protect the physical health of people with mental illness [Reference Firth, Siddiqi, Koyanagi, Siskind, Rosenbaum and Galletly5].
However, it is still not common practice to refer patients with mental illness to lifestyle interventions to improve their disadvantaged health status. An Australian study found that 70% of the mental healthcare professionals (MHCPs) prescribed exercise daily or weekly for depression, anxiety, or stress, but only 11% for schizophrenia or bipolar disorder [Reference Fibbins, Czosnek, Stanton, Davison, Lederman and Morell11]. A Dutch study found that 80% of referring MHCPs had ever referred a patient to an exercise program. Some studies suggest that HCPs’ own lifestyle habits impact their clinical lifestyle practices [Reference Carlos, Carlos, Rico-Campà, Rico-Campà, Rico-Campà and De La Fuente-Arrillaga12–Reference Deenik, Koomen, Scheewe, van Deursen and Cahn20]. The Dutch study found that referral to physical activity interventions was associated with MHCPs’ physical activity levels [Reference Deenik, Koomen, Scheewe, van Deursen and Cahn20]. These findings are in line with previous research on lifestyle habits of the HCP and their counsel and referral practices in general healthcare. HCPs who practice healthy lifestyle habits are more likely to counsel on these lifestyle habits and non-smoking HCPs are more likely to advice their patients to quit smoking [Reference Carlos, Carlos, Rico-Campà, Rico-Campà, Rico-Campà and De La Fuente-Arrillaga12–Reference Lewis, Clancy, Leake and Schwartz19].
Although previous studies investigated the personal physical activity habits of psychiatrists and their referral practices to physical activity interventions [Reference Fibbins, Czosnek, Stanton, Davison, Lederman and Morell11, Reference Deenik, Koomen, Scheewe, van Deursen and Cahn20], it is unknown whether such associations also apply to a broader spectrum of lifestyle habits and referring professions in mental healthcare. Therefore, the aim of this study was to identify MHCPs’ lifestyle habits and their clinical practices on taking a lifestyle history, and referral regarding physical activity, dietary habits, sleep, tobacco, and alcohol use, and to investigate whether these practices are associated with their personal lifestyle habits.
Methods
Study design
This cross-sectional study was conducted between May 2022 and January 2023. All mental healthcare institutions, psychiatry departments of hospitals, organizations for nurse specialists, and organizations for independent working psychiatrists in The Netherlands were asked to distribute the link to the online questionnaire to referring MHCPs. In addition, invitations to the online questionnaire were distributed at the Dutch Association for Psychiatry (NVvP) 2022 congress, which is the main psychiatry congress in The Netherlands. To minimize selection bias, the invitation to the online questionnaire invited referring MHCPs to give their opinion about lifestyle psychiatry, also when they believed healthy lifestyle should not play a role in psychiatry.
Participants
We included the following groups of referring MHCPs based on informed consent: residents in psychiatry, nurse specialists working at a general practitioner practice (GP-based nurse specialists), specialized nurses and physician assistants (category referring MHCP with a nursing background), healthcare psychologists and remedial educationalists (category referring MHCP with scientific background), clinical psychologists and psychiatrists. Although the questionnaire was aimed for referring MHCPs, also MHCPs who cannot refer patients filled in the questionnaire. They were divided into the categories psychologists and “other.” The division of profession groups was based on educational level and clinical responsibilities. Participants were included in the study when they at least completed the first two parts of the questionnaire.
Under Dutch law, medical ethical approval is not required for non-medical research with anonymous data. The rules of conduct as outlined in the Declaration of Helsinki of 1975, as revised in 2008, were followed, and participants were asked for written consent.
Questionnaire
The questionnaire consisted of three parts. Participants were first asked about age, gender, height, weight, profession, work setting, main patient population they work with, and if lifestyle interventions were available within their work setting.
Then, questions about their own lifestyle were asked. Participants were asked how important their lifestyle is on a scale from 0 to 10. Questions on tobacco use, drinking habits, and drug use were based on the FANTASTIC instrument [Reference Wilson, Nielsen and Ciliska21]. Questions regarding physical activity were based on international physical activity guidelines, namely ≥2x bone and muscle strengthening exercises per week, and ≥150 min moderate to vigorous physical activity (MVPA) per week [Reference Bull, Al-Ansari, Biddle, Borodulin, Buman and Cardon22]. For analysis, we calculated if participants adhered to these guidelines. Questions on eating pattern were based on the FANTASTIC instrument and WHO steps [Reference Wilson, Nielsen and Ciliska21, 23]. Participants were asked on sleep satisfaction, and stress related to their work and their private life on a scale from 0 to 10.
The third part of the questionnaire consisted of questions on lifestyle within psychiatric treatment. Participants were first asked if lifestyle should be part of psychiatric treatment, and who is responsible for the lifestyle treatment of a psychiatric patient. Then, participants were questioned what proportion of their patients they ask about: physical activity, dietary habits, sleep, tobacco, and alcohol use. What proportion of their patients they advise to quit smoking if they smoke, and what proportion of their patients they refer to: lifestyle interventions to improve mental health, lifestyle interventions to improve physical health, and insomnia cognitive behavioral therapy (CBT). These questions were stated as follows: What proportion of your patients do you refer to “an intervention aimed at improving or maintaining someone’s lifestyle” to improve their mental health, if you believe there is something to gain for the patient in terms of lifestyle? Answer options were: 0%, 0–10%, 10–20%, 20–30%, 30–40%, 40–50%, 50–60%, 60–70%, 70–80%, 80–90%, 90–100%, and not applicable. For analysis, we recoded these answer options into mean percentages.
See the Supplementary Material for the full questionnaire.
Analyses
Answers were presented using numbers, percentages, means, and standard deviations. Differences between profession groups were calculated using ANOVA for continuous variables and chi-square tests for categorical variables. To analyze if MHCPs own lifestyle habits, gender, and profession were associated with taking a history on lifestyle habits and referral practices, an ordinal regression was done with the use of the following independent variables: age per 10 years, gender (female, male), BMI per 5 units, question “how important their own lifestyle is” (0–10), smoking status (smoked in past, never smoked, current smoker), alcohol use (no, yes), physical activity level (meets the physical activity criteria, meets 1 physical activity criterium, meets 0 criteria), dietary habits (has/has not a balanced eating pattern), sleep satisfaction (0–10), and profession (other, psychologist, resident in psychiatry, G-based nurse specialist, referring MHCP with nursing background, referring MHCP with a scientific background, clinical psychologist, and psychiatrist). Additionally, we did a sensitivity analysis with the variable work-related stress. Results were presented using odds ratios, confidence intervals, and significance levels. For the analyses on taking a history on tobacco and alcohol use, and advice to quit smoking, only MHCPs working with adults and elderly were included. For the analyses on referral practices, only referring MHCPs were included. A Bonferroni correction was done to correct for multiple testing, such that p < 0.006 was considered statistically significant. SPSS version 27.0 was used for analyses.
Results
Participants
Table 1 presents participant characteristics, their lifestyle habits, and their practices on taking a lifestyle history and referral to lifestyle interventions. A total of 1,607 participants filled in the online questionnaire. About 78.4% of the participants were female, age ranged between 22 and 75 years, and lifestyle interventions were available in 62.9% of the work settings. Table S1 in the Supplementary Material presents all results of the questionnaire, also divided by profession category.
Table 1. Participant characteristics, lifestyle habits, and lifestyle history and referral practices
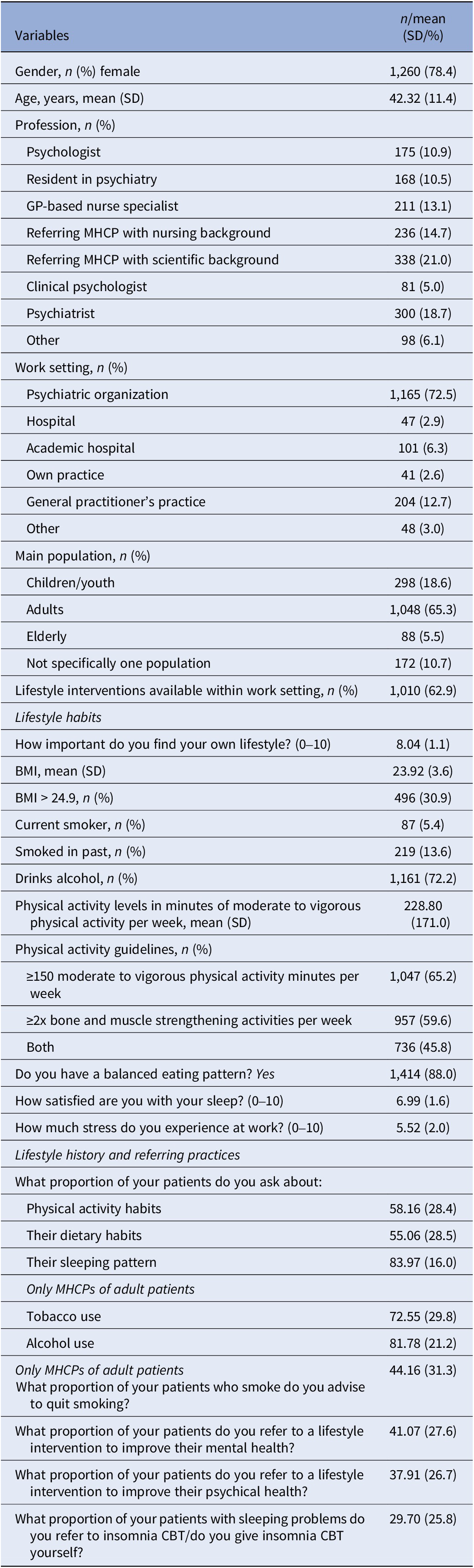
MHCP, mental healthcare professional; n, number; SD, standard deviation.
Lifestyle habits of the MHCP
On average, participants rated an 8.0 on the question if they find their own lifestyle important. BMI ranged between 15.8 and 44.4, and 30.9% of the participants were overweight. A minority (5.4%) are current smokers, and 13.6% smoked in the past. The majority of the participants (72.2%) drinks alcohol and 6.8% uses drugs. About 45.8% of the MHCPs adheres to the physical activity guidelines, 88.0% believes they have a balanced eating pattern, and the MHCPs rate their sleep on average a 7.0 out of 10. The average level of stress at work is rated a 5.5 out of 10.
Lifestyle within psychiatric treatment
MHCPs rated on average an 8.1 to how important lifestyle is in psychiatric treatment and 87.6% (totally) agreed with the statement that lifestyle should be part of every psychiatric treatment. They found that the responsibility for the lifestyle treatment of a psychiatric patient lies with every MHCP (77.0%), followed by the patient (66.0%) and the general practitioner (43.6%).
MHCPs asked patients the most about their sleeping pattern (84.0%), followed by alcohol use (81.2%), tobacco use (72.6%), physical activity (58.2%) and dietary habits (55.1%). They advised 44.2% of their patients to quit smoking if they smoke. Moreover, they referred 41.1% of their patients to lifestyle interventions to improve their mental health, and 37.9% of their patients were referred to lifestyle interventions to improve their physical health. MHCPs referred 29.7% of their patients to insomnia CBT or gave insomnia CBT themselves if patients experience sleep problems.
Association between personal lifestyle habits, gender, and profession and clinical lifestyle practices
Table 2 and Figures 1 and 2 show the results of the ordinal regression analyses on lifestyle habits, gender, profession, and lifestyle history and referral practices. MHCPs who find their own lifestyle important have higher odds to take a lifestyle history, to advice patients to quit smoking and to refer patients to lifestyle interventions. Compared to current smokers, MHCPs who smoked in the past have higher odds to take a history on physical activity, and MHCPs who smoked in the past and MHCPs who never smoked have higher odds to advice patients to quit smoking. Physically active MHCPs have higher odds to take a history on lifestyle habits, except for sleep, and higher odds to advice patients to quit smoking, and to refer to lifestyle interventions. MHCPs who have a balanced eating pattern have higher odds to ask patients about physical activity, and MHCPs who are more satisfied with their sleep have higher odds to ask patients about their sleep pattern, and to refer patients to lifestyle interventions to improve their mental health. Female MHCPs have higher odds to take a history on physical activity, dietary habits and sleep, and higher odds to refer patients to lifestyle interventions to improve their mental health and sleep.
Table 2. Results of the ordinal regression analyses on lifestyle habits, gender, profession, and lifestyle history and referral practices
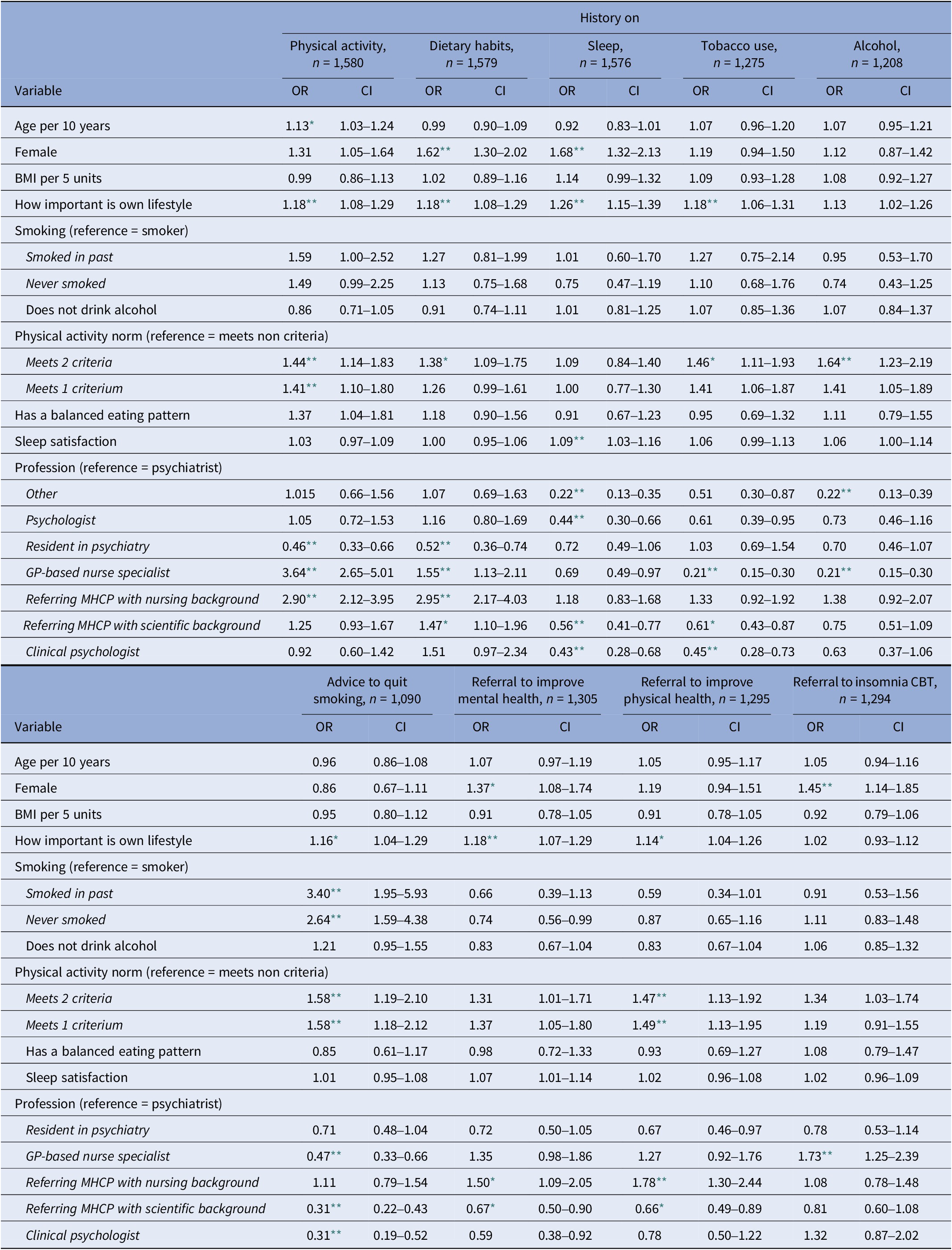
CI, confidence interval; GP, general practitioner; MHCP, mental healthcare professional; n, number; OR, odds ratio.
* p < 0.01.
** p < 0.006.
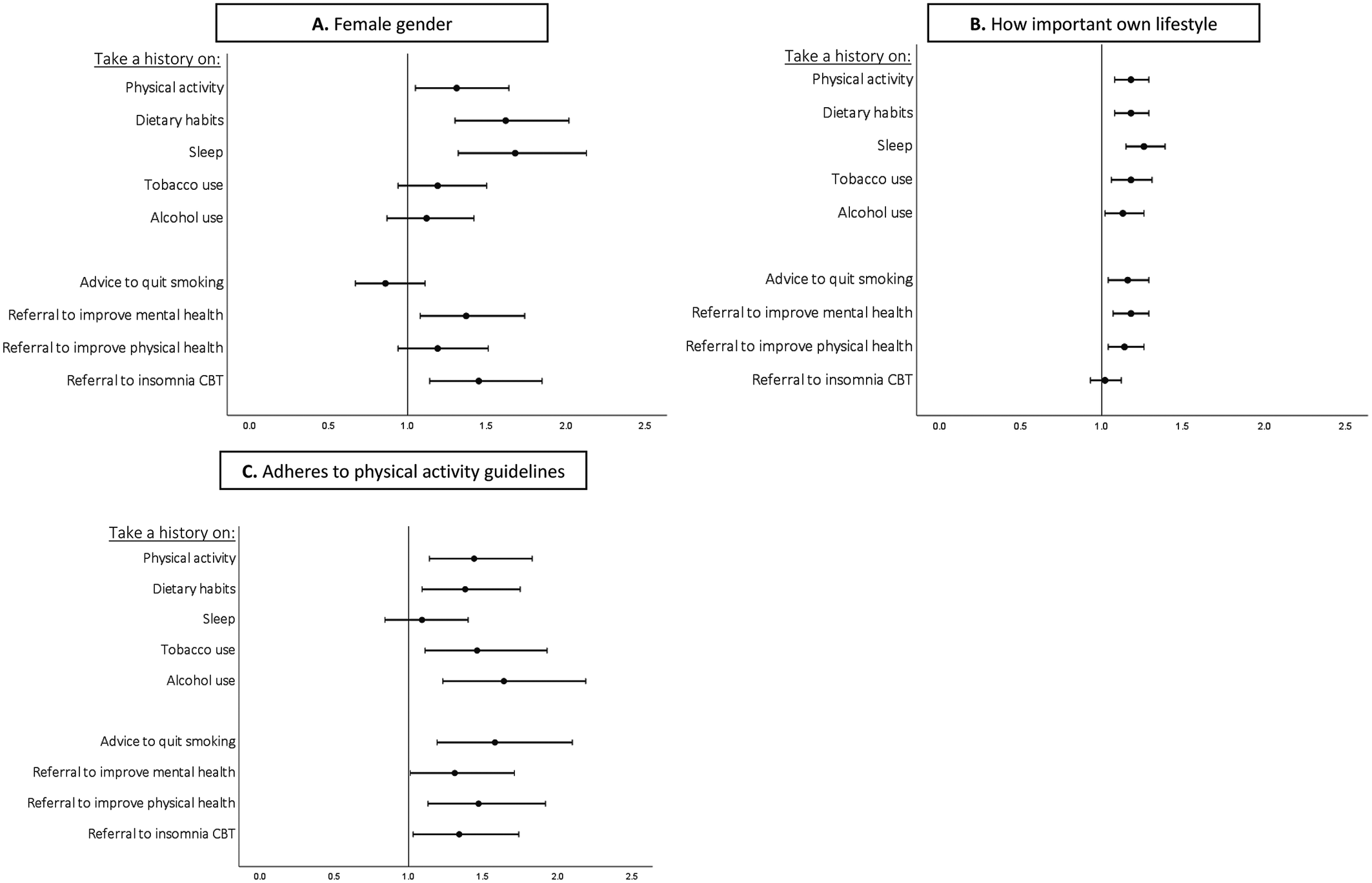
Figure 1. Forest plots of the results of ordinal regression analyses on MHCPs’ gender (A), importance of own lifestyle (B) and physical activity (C), and lifestyle history and referral practices. Odds ratio 0–1: take less history on lifestyle habits, advice less to quit smoking, and refer less to lifestyle interventions. Odds ratio >1: take more history on lifestyle factors, advice more to quit smoking, and refer more to lifestyle interventions.
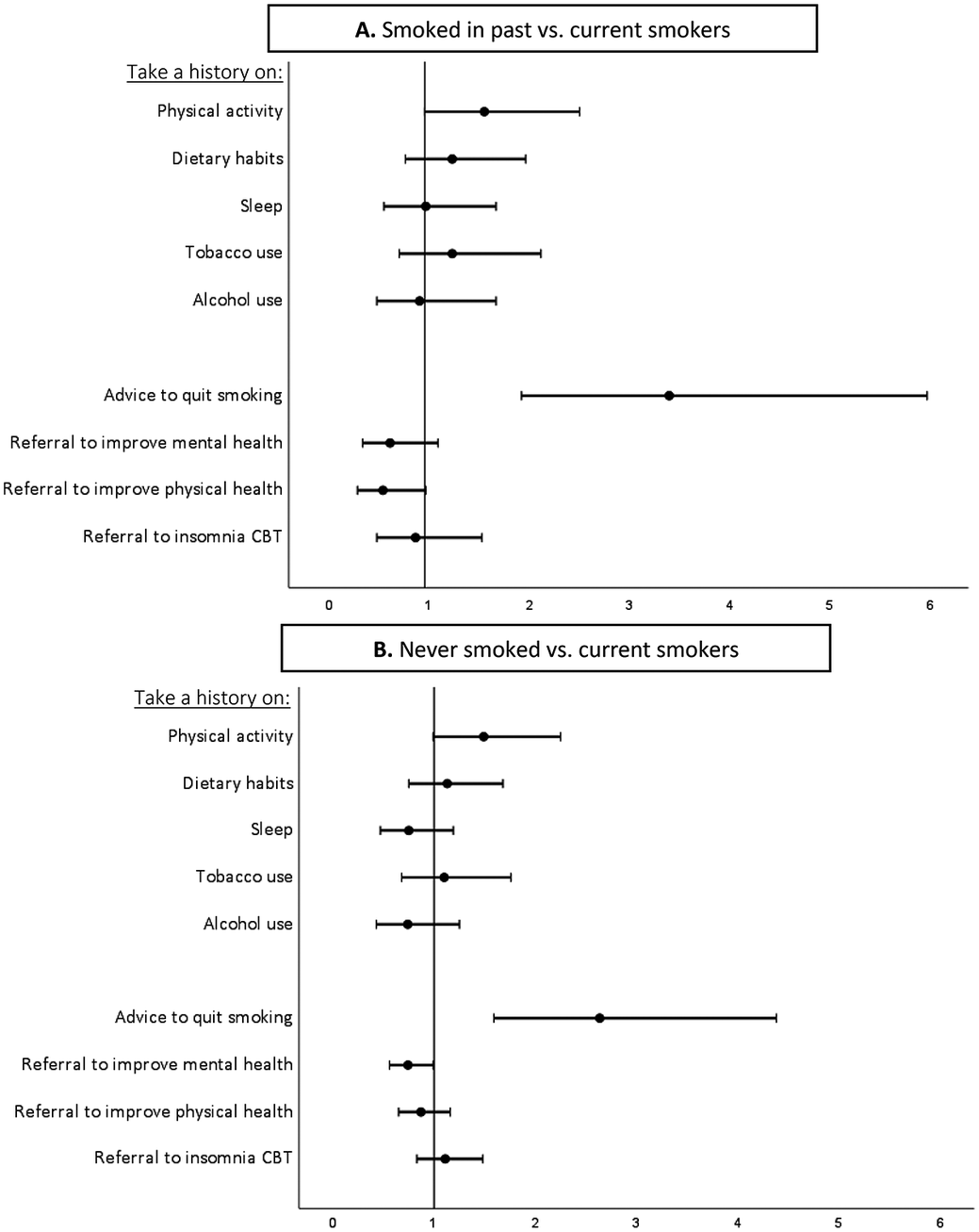
Figure 2. Forest plots of the results of ordinal regression analyses on MHCPs’ smoking status, and lifestyle history and referral practices. A: MHCPs who smoked in the past versus current smokers. B: MHCPs who never smoked versus current smokers. Odds ratio 0–1: take less history on lifestyle habits, advice less to quit smoking, and refer less to lifestyle interventions. Odds ratio >1: take more history on lifestyle factors, advice more to quit smoking, and refer more to lifestyle interventions.
Psychologists, residents in psychiatry, referring MHCPs with a scientific background, and clinical psychologists had lower odds to take a history on several lifestyle habits, and referring MHCPs with a scientific background and clinical psychologists had lower odds to refer patients to lifestyle interventions. On the contrary, MHCPs with a nursing background had higher odds to take a history on several lifestyle habits, and higher odds to refer patients to lifestyle interventions compared to psychiatrists. Interestingly, GP-based nurse practitioners had lower odds to take a history on sleep, tobacco, and alcohol use, but higher odds to take a history on physical activity and dietary habits than psychiatrists. In addition, they had lower odds to advice patients to quit smoking, but higher odds to refer patients to insomnia CBT.
The sensitivity analysis on work related stress did not change these outcomes (Table S2 in the Supplementary Material).
Discussion
We found that Dutch MHCPs are often non-smokers (94.6%), but the majority does consume alcohol (72.2%). Less than half (45.8%) adheres to the physical activity guidelines, 88.0% believes they have a balanced eating pattern, and they rate their sleep on average a 7.0 out of 10. The majority (87.6%) finds that lifestyle should be part of every psychiatric treatment, but depending on which lifestyle factor, 55.1–84.0% take a lifestyle history, 29.7–41.1% refer to interventions, and less than half (44.2%) of smoking patients are advised to quit. MHCPs who find their lifestyle important, who are physically more active, females, and MHCPs with a nursing background take more lifestyle histories and refer more often. Compared to current smokers, MHCPs who never or formerly smoked have higher odds (2.64 and 3.40, respectively, p < 0.001) to advice patients to quit smoking.
The physical activity and alcohol consumption are representative for the Dutch population [Reference Kraaykamp, André and Meuleman24]. Yet, our sample smokes less (5.4% vs. 26.1%), is less overweight (31.6% vs. 51.6%), and eats more fruit on a daily basis (56.4% vs. 26.0%) [Reference Kraaykamp, André and Meuleman24], which might also be explained by the younger age of our population. In the context of similar evaluations, the sample is more active than Australian psychiatrists [Reference Fibbins, Czosnek, Stanton, Davison, Lederman and Morell11], corresponding to previous research [Reference Deenik, Koomen, Scheewe, van Deursen and Cahn20].
Noteworthy, less than half of the patients who smoke are advised to quit, while the Very Brief Advice, an evidence-based intervention to increase quit smoking attempts, only costs 30 s of time [Reference Aveyard, Begh, Parsons and West25]. Surprisingly, MHCPs refer the least to insomnia CBT or give insomnia CBT themselves, while sleep problems occur often in patients with mental illness, and insomnia CBT is an effective treatment that also decreases psychiatric symptoms [Reference Firth, Solmi, Wootton, Vancampfort, Schuch and Gilbody6, Reference Freeman, Sheaves, Waite, Harvey and Harrison26].
In addition, we found that MHCPs who find their own lifestyle important, who are physically more active and female MHCPs more often take lifestyle histories and refer more frequently to lifestyle interventions. Compared to current smokers, MHCPs who formerly or never smoked have higher odds to advice patients to quit smoking. These findings are in line with previous research in psychiatry [Reference Deenik, Koomen, Scheewe, van Deursen and Cahn20] and general healthcare [Reference Carlos, Carlos, Rico-Campà, Rico-Campà, Rico-Campà and De La Fuente-Arrillaga12–Reference Belfrage, Grotmol, Tyssen, Moum, Finset and Rø15, Reference Fie, Norman and While17–Reference Lewis, Clancy, Leake and Schwartz19]. Interestingly, MHCPs tend to take more histories and make more referrals if they engage in the lifestyle behavior themselves. This could be explained by the fact that it is easier to talk about and advise patients on behavior that you personally consider important and engage in yourself. Regarding profession groups, it was noticeable that professionals with less clinical experience and medical training did take less lifestyle history and referred less, and MHCPs with a nursing background did more in comparison to psychiatrists.
Our findings show that taking a lifestyle history and referral depends on the lifestyle habits, gender, and profession of the MHCP. There is compelling evidence that lifestyle interventions can improve mental and physical health and these interventions are therefore recommended in the treatment for people with mental illness [Reference Firth, Siddiqi, Koyanagi, Siskind, Rosenbaum and Galletly5–10]. Therefore, taking a lifestyle history should always be done, and referral to lifestyle interventions should be considered in every psychiatric treatment, and should not depend on the personal and professional characteristics of the MHCP. Previous research on counseling of physicians in primary care suggested that physicians often struggle with counseling on health behavior that they do not practice themselves [Reference Vickers, Kircher, Smith, Petersen and Rasmussen27]. It seems therefore important to practice what you preach, also since patients see their physicians as role models for healthy lifestyle habits, and physicians who disclose information about their own lifestyle are found to be more credible and motivating [Reference Frank, Breyan and Elon28].
To improve the clinical lifestyle practices of MHCPs at a short notice, it is important to educate MHCPs on the evidence about lifestyle psychiatry, lifestyle counseling and referral. Practical training in motivational interviewing can be particularly helpful in this regard. In addition, practical guidelines and referral options should be provided. Currently, there are hardly any courses on healthy lifestyle in education and medical training [29], and lifestyle interventions are often not part of treatment guidelines. Our finding that MHCPs with less clinical experience and medical training take less lifestyle histories and refer less, underline the necessity of adequate training. Next to this, it might not only be important to look at the MHCP, but also to critically review the role of healthy lifestyle in the healthcare system and society. In most healthcare systems, just as in The Netherlands, financial incentives in healthcare are based on the treatment of diseases, and not on the prevention of diseases [Reference Varkevisser, Schut, Franken and Van Der Geest30]. Moreover, medical insurance only reimburse a few lifestyle interventions, and a mental illness is not an indication for referral to these lifestyle interventions [31]. Future research should investigate barriers and facilitators MHCPs experience in taking lifestyle histories and referring to lifestyle interventions to identify solutions to improve their clinical lifestyle practices.
Limitations
Our study has some limitations. Our main concern is that there might have been selection bias, since MHCPs who believe lifestyle is an important topic within psychiatry, and MHCPs who have a healthier lifestyle might be more likely to fill in the questionnaire. To reduce this bias, we especially stated in the invitation, that all MHCPs, also when they believe healthy lifestyle should not play a role in psychiatry, were invited to participate. That healthier and more lifestyle-focused MHCPs might have participated in this study may also indicate that the actual clinical lifestyle practices are even worse. Moreover, this limitation is inherent to questionnaire-focused research and it will be challenging to study this topic in a more objective way. After all, this is the largest sample including these data and thereby the most representative, so far. Nevertheless, this remains a cross-sectional study, thus we only examined associations and not causal relations. Another limitation is that the questionnaire was a self-reporting questionnaire, and we did not measure lifestyle habits by performing for example physical activity tracking. Therefore, the actual lifestyle habits of the MHCP might differ. Lastly, we framed the question on referral to lifestyle interventions as “if you believe there is something to gain for the patient in terms of lifestyle?” This could have caused bias because the response depends on what the participant perceives as a healthy lifestyle.
This study indicates that MHCPs’ personal lifestyle habits, gender, and profession affect their clinical lifestyle practices, and thereby the translation of compelling evidence on lifestyle psychiatry to improved healthcare for patients.
Supplementary material
The supplementary material for this article can be found at https://doi.org/10.1192/j.eurpsy.2023.2475.
Acknowledgments
We would like to thank all institutions that distributed the questionnaire and would like to thank all participants for their time and valuable answers.
Financial support
This research received no specific grant from any funding agency, commercial, or not-for-profit sectors.
Competing interest
The authors have no competing interests to declare.
Ethics statement
Under Dutch law, medical ethical approval is not required for non-medical research with anonymous data. The rules of conduct as outlined in the Declaration of Helsinki of 1975, as revised in 2008, were followed, and participants were asked for written consent.







Comments
No Comments have been published for this article.