Introduction
Estimates suggest that 15% of working-age adults globally live with a mental disorder at any given time (WHO, 2022). Among these disorders, depression is the leading cause of disability worldwide (Vos et al., Reference Vos, Lim, Abbafati, Abbas, Abbasi, Abbasifard, Abbasi-Kangevari, Abbastabar, Abd-Allah, Abdelalim, Abdollahi, Abdollahpour, Abolhassani, Aboyans, Abrams, Abreu, Abrigo, Abu-Raddad, Abushouk, Acebedo, Ackerman, Adabi, Adamu, Adebayo, Adekanmbi, Adelson, Adetokunboh, Adham, Afshari, Afshin, Agardh, Agarwal, Agesa, Aghaali, Aghamir, Agrawal, Ahmad, Ahmadi, Ahmadi, Ahmadieh, Ahmadpour, Akalu, Akinyemi, Akinyemiju, Akombi, Al-Aly, Alam, Alam, Alam, Alam, Alanzi, Albertson, Alcalde-Rabanal, Alema, Ali, Ali, Alicandro, Alijanzadeh, Alinia, Alipour, Aljunid, Alla, Allebeck, Almasi-Hashiani, Alonso, Al-Raddadi, Altirkawi, Alvis-Guzman, Alvis-Zakzuk, Amini, Amini-Rarani, Aminorroaya, Amiri, Amit, Amugsi, Amul, Anderlini, Andrei, Andrei, Anjomshoa, Ansari, Ansari, Ansari-Moghaddam, Antonio, Antony, Antriyandarti, Anvari, Anwer, Arabloo, Arab-Zozani, Aravkin, Ariani, Ärnlöv, Aryal, Arzani, Asadi-Aliabadi, Asadi-Pooya, Asghari, Ashbaugh, Atnafu, Atre, Ausloos, Ausloos, Ayala Quintanilla, Ayano, Ayanore, Aynalem, Azari, Azarian, Azene, Babaee, Badawi, Bagherzadeh, Bakhshaei, Bakhtiari, Balakrishnan, Balalla, Balassyano, Banach, Banik, Bannick, Bante, Baraki, Barboza, Barker-Collo, Barthelemy, Barua, Barzegar, Basu, Baune, Bayati, Bazmandegan, Bedi, Beghi, Béjot, Bello, Bender, Bennett, Bennitt, Bensenor, Benziger, Berhe, Bernabe, Bertolacci, Bhageerathy, Bhala, Bhandari, Bhardwaj, Bhattacharyya, Bhutta, Bibi, Biehl, Bikbov, Bin Sayeed, Biondi, Birihane, Bisanzio, Bisignano, Biswas, Bohlouli, Bohluli, Bolla, Boloor, Boon-Dooley, Borges, Borzì, Bourne, Brady, Brauer, Brayne, Breitborde, Brenner, Briant, Briggs, Briko, Britton, Bryazka, Buchbinder, Bumgarner, Busse, Butt, Caetano dos Santos, Cámera, Campos-Nonato, Car, Cárdenas, Carreras, Carrero, Carvalho, Castaldelli-Maia, Castañeda-Orjuela, Castelpietra, Castle, Castro, Catalá-López, Causey, Cederroth, Cercy, Cerin, Chandan, Chang, Charlson, Chattu, Chaturvedi, Chimed-Ochir, Chin, Cho, Christensen, Chu, Chung, Cicuttini, Ciobanu, Cirillo, Collins, Compton, Conti, Cortesi, Costa, Cousin, Cowden, Cowie, Cromwell, Cross, Crowe, Cruz, Cunningham, Dahlawi, Damiani, Dandona, Dandona, Darwesh, Daryani, Das, Das Gupta, das Neves, Dávila-Cervantes, Davletov, De Leo, Dean, DeCleene, Deen, Degenhardt, Dellavalle, Demeke, Demsie, Denova-Gutiérrez, Dereje, Dervenis, Desai, Desalew, Dessie, Dharmaratne, Dhungana, Dianatinasab, Diaz, Dibaji Forooshani, Dingels, Dirac, Djalalinia, Do, Dokova, Dorostkar, Doshi, Doshmangir, Douiri, Doxey, Driscoll, Dunachie, Duncan, Duraes, Eagan, Ebrahimi Kalan, Edvardsson, Ehrlich, El Nahas, El Sayed, El Tantawi, Elbarazi, Elgendy, Elhabashy, El-Jaafary, Elyazar, Emamian, Emmons-Bell, Erskine, Eshrati, Eskandarieh, Esmaeilnejad, Esmaeilzadeh, Esteghamati, Estep, Etemadi, Etisso, Farahmand, Faraj, Fareed, Faridnia, Farinha, Farioli, Faro, Faruque, Farzadfar, Fattahi, Fazlzadeh, Feigin, Feldman, Fereshtehnejad, Fernandes, Ferrari, Ferreira, Filip, Fischer, Fisher, Fitzgerald, Flohr, Flor, Foigt, Folayan, Force, Fornari, Foroutan, Fox, Freitas, Fu, Fukumoto, Furtado, Gad, Gakidou, Galles, Gallus, Gamkrelidze, Garcia-Basteiro, Gardner, Geberemariyam, Gebrehiwot, Gebremedhin, Gebreslassie, Gershberg Hayoon, Gething, Ghadimi, Ghadiri, Ghafourifard, Ghajar, Ghamari, Ghashghaee, Ghiasvand, Ghith, Gholamian, Gilani, Gill, Gitimoghaddam, Giussani, Goli, Gomez, Gopalani, Gorini, Gorman, Gottlich, Goudarzi, Goulart, Goulart, Grada, Grivna, Grosso, Gubari, Gugnani, Guimaraes, Guimarães, Guled, Guo, Guo, Gupta, Haagsma, Haddock, Hafezi-Nejad, Hafiz, Hagins, Haile, Hall, Halvaei, Hamadeh, Hamagharib Abdullah, Hamilton, Han, Han, Hankey, Haro, Harvey, Hasaballah, Hasanzadeh, Hashemian, Hassanipour, Hassankhani, Havmoeller, Hay, Hay, Hayat, Heidari, Heidari, Heidari-Soureshjani, Hendrie, Henrikson, Henry, Herteliu, Heydarpour, Hird, Hoek, Hole, Holla, Hoogar, Hosgood, Hosseinzadeh, Hostiuc, Hostiuc, Househ, Hoy, Hsairi, Hsieh, Hu, Huda, Hugo, Huynh, Hwang, Iannucci, Ibitoye, Ikuta, Ilesanmi, Ilic, Ilic, Inbaraj, Ippolito, Irvani, Islam, Islam, Islam, Islami, Iso, Ivers, Iwu, Iyamu, Jaafari, Jacobsen, Jadidi-Niaragh, Jafari, Jafarinia, Jahagirdar, Jahani, Jahanmehr, Jakovljevic, Jalali, Jalilian, James, Janjani, Janodia, Jayatilleke, Jeemon, Jenabi, Jha, Jha, Ji, Jia, John, John-Akinola, Johnson, Johnson, Jonas, Joo, Joshi, Jozwiak, Jürisson, Kabir, Kabir, Kalani, Kalani, Kalankesh, Kalhor, Kamiab, Kanchan, Karami Matin, Karch, Karim, Karimi, Kassa, Kassebaum, Katikireddi, Kawakami, Kayode, Keddie, Keller, Kereselidze, Khafaie, Khalid, Khan, Khatab, Khater, Khatib, Khayamzadeh, Khodayari, Khundkar, Kianipour, Kieling, Kim, Kim, Kim, Kimokoti, Kisa, Kisa, Kissimova-Skarbek, Kivimäki, Kneib, Knudsen, Kocarnik, Kolola, Kopec, Kosen, Koul, Koyanagi, Kravchenko, Krishan, Krohn, Kuate Defo, Kucuk Bicer, Kumar, Kumar, Kumar, Kumar, Kumaresh, Kurmi, Kusuma, Kyu, La Vecchia, Lacey, Lal, Lalloo, Lam, Lami, Landires, Lang, Lansingh, Larson, Larsson, Lasrado, Lassi, Lau, Lavados, Lazarus, Ledesma, Lee, Lee, LeGrand, Leigh, Leonardi, Lescinsky, Leung, Levi, Lewington, Li, Lim, Lin, Lin, Linehan, Linn, Liu, Liu, Liu, Looker, Lopez, Lopukhov, Lorkowski, Lotufo, Lucas, Lugo, Lunevicius, Lyons, Ma, MacLachlan, Maddison, Maddison, Madotto, Mahasha, Mai, Majeed, Maled, Maleki, Malekzadeh, Malta, Mamun, Manafi, Manafi, Manguerra, Mansouri, Mansournia, Mantilla Herrera, Maravilla, Marks, Martins-Melo, Martopullo, Masoumi, Massano, Massenburg, Mathur, Maulik, McAlinden, McGrath, McKee, Mehndiratta, Mehri, Mehta, Meitei, Memiah, Mendoza, Menezes, Mengesha, Mengesha, Mereke, Meretoja, Meretoja, Mestrovic, Miazgowski, Miazgowski, Michalek, Mihretie, Miller, Mills, Mirica, Mirrakhimov, Mirzaei, Mirzaei, Mirzaei-Alavijeh, Misganaw, Mithra, Moazen, Moghadaszadeh, Mohamadi, Mohammad, Mohammad, Mohammad Gholi Mezerji, Mohammadian-Hafshejani, Mohammadifard, Mohammadpourhodki, Mohammed, Mokdad, Molokhia, Momen, Monasta, Mondello, Mooney, Moosazadeh, Moradi, Moradi, Moradi-Lakeh, Moradzadeh, Moraga, Morales, Morawska, Moreno Velásquez, Morgado-da-Costa, Morrison, Mosser, Mouodi, Mousavi, Mousavi Khaneghah, Mueller, Munro, Muriithi, Musa, Muthupandian, Naderi, Nagarajan, Nagel, Naghshtabrizi, Nair, Nandi, Nangia, Nansseu, Nayak, Nazari, Negoi, Negoi, Netsere, Ngunjiri, Nguyen, Nguyen, Nguyen, Nguyen, Nichols, Nigatu, Nigatu, Nikbakhsh, Nixon, Nnaji, Nomura, Norrving, Noubiap, Nowak, Nunez-Samudio, Oţoiu, Oancea, Odell, Ogbo, Oh, Okunga, Oladnabi, Olagunju, Olusanya, Olusanya, Oluwasanu, Omar Bali, Omer, Ong, Onwujekwe, Orji, Orpana, Ortiz, Ostroff, Otstavnov, Otstavnov, Øverland, Owolabi, P A, Padubidri, Pakhare, Palladino, Pana, Panda-Jonas, Pandey, Park, Parmar, Pasupula, Patel, Paternina-Caicedo, Pathak, Pathak, Patten, Patton, Paudel, Pazoki Toroudi, Peden, Pennini, Pepito, Peprah, Pereira, Pereira, Perico, Pham, Phillips, Pigott, Pilgrim, Pilz, Pirsaheb, Plana-Ripoll, Plass, Pokhrel, Polibin, Polinder, Polkinghorne, Postma, Pourjafar, Pourmalek, Pourmirza Kalhori, Pourshams, Poznańska, Prada, Prakash, Pribadi, Pupillo, Quazi Syed, Rabiee, Rabiee, Radfar, Rafiee, Rafiei, Raggi, Rahimi-Movaghar, Rahman, Rajabpour-Sanati, Rajati, Ramezanzadeh, Ranabhat, Rao, Rao, Rasella, Rastogi, Rathi, Rawaf, Rawaf, Rawal, Razo, Redford, Reiner, Reinig, Reitsma, Remuzzi, Renjith, Renzaho, Resnikoff, Rezaei, Rezai, Rezapour, Rhinehart, Riahi, Ribeiro, Ribeiro, Ribeiro, Rickard, Roberts, Roberts, Robinson, Roever, Rolfe, Ronfani, Roshandel, Roth, Rubagotti, Rumisha, Sabour, Sachdev, Saddik, Sadeghi, Sadeghi, Saeidi, Safi, Safiri, Sagar, Sahebkar, Sahraian, Sajadi, Salahshoor, Salamati, Salehi Zahabi, Salem, Salem, Salimzadeh, Salomon, Salz, Samad, Samy, Sanabria, Santomauro, Santos, Santos, Santric-Milicevic, Saraswathy, Sarmiento-Suárez, Sarrafzadegan, Sartorius, Sarveazad, Sathian, Sathish, Sattin, Sbarra, Schaeffer, Schiavolin, Schmidt, Schutte, Schwebel, Schwendicke, Senbeta, Senthilkumaran, Sepanlou, Shackelford, Shadid, Shahabi, Shaheen, Shaikh, Shalash, Shams-Beyranvand, Shamsizadeh, Shannawaz, Sharafi, Sharara, Sheena, Sheikhtaheri, Shetty, Shibuya, Shiferaw, Shigematsu, Shin, Shiri, Shirkoohi, Shrime, Shuval, Siabani, Sigfusdottir, Sigurvinsdottir, Silva, Simpson, Singh, Singh, Skiadaresi, Skou, Skryabin, Sobngwi, Sokhan, Soltani, Sorensen, Soriano, Sorrie, Soyiri, Sreeramareddy, Stanaway, Stark, Ştefan, Stein, Steiner, Steiner, Stokes, Stovner, Stubbs, Sudaryanto, Sufiyan, Sulo, Sultan, Sykes, Sylte, Szócska, Tabarés-Seisdedos, Tabb, Tadakamadla, Taherkhani, Tajdini, Takahashi, Taveira, Teagle, Teame, Tehrani-Banihashemi, Teklehaimanot, Terrason, Tessema, Thankappan, Thomson, Tohidinik, Tonelli, Topor-Madry, Torre, Touvier, Tovani-Palone, Tran, Travillian, Troeger, Truelsen, Tsai, Tsatsakis, Tudor Car, Tyrovolas, Uddin, Ullah, Undurraga, Unnikrishnan, Vacante, Vakilian, Valdez, Varughese, Vasankari, Vasseghian, Venketasubramanian, Violante, Vlassov, Vollset, Vongpradith, Vukovic, Vukovic, Waheed, Walters, Wang, Wang, Wang, Ward, Watson, Wei, Weintraub, Weiss, Weiss, Westerman, Whisnant, Whiteford, Wiangkham, Wiens, Wijeratne, Wilner, Wilson, Wojtyniak, Wolfe, Wool, Wu, Wulf Hanson, Wunrow, Xu, Xu, Yadgir, Yahyazadeh Jabbari, Yamagishi, Yaminfirooz, Yano, Yaya, Yazdi-Feyzabadi, Yearwood, Yeheyis, Yeshitila, Yip, Yonemoto, Yoon, Yoosefi Lebni, Younis, Younker, Yousefi, Yousefifard, Yousefinezhadi, Yousuf, Yu, Yusefzadeh, Zahirian Moghadam, Zaki, Zaman, Zamani, Zamanian, Zandian, Zangeneh, Zastrozhin, Zewdie, Zhang, Zhang, Zhao, Zhao, Zheng, Zhou, Ziapour, Zimsen, Naghavi and Murray2020). In Europe and the USA, depression is the second-most common disorder (after anxiety disorders), with a 12-month prevalence of approximately 7% (Kessler et al., Reference Kessler, Petukhova, Sampson, Zaslavsky and Wittchen2012; Wittchen et al., Reference Wittchen, Jacobi, Rehm, Gustavsson, Svensson, Jönsson, Olesen, Allgulander, Alonso, Faravelli, Fratiglioni, Jennum, Lieb, Maercker, van Os, Preisig, Salvador-Carulla, Simon and Steinhausen2011). Around 50% of those developing a depressive episode will have at least one more episode in the future (or never remit) (Eaton et al., Reference Eaton, Shao, Nestadt, Lee, Bienvenu and Zandi2008; Mattisson et al., Reference Mattisson, Bogren, Horstmann, Munk-Jörgensen and Nettelbladt2007).
Risk factors for the onset of depression include biological, psychological and social factors (Malhi and Mann, Reference Malhi and Mann2018) that may also include psychosocial factors in the work environment (WHO, 2022). Systematic reviews and meta-analyses have reported that specific psychosocial work factors are associated with the onset of depression (Theorell et al., Reference Theorell, Hammarström, Aronsson, Bendz, Grape, Hogstedt, Marteinsdottir, Skoog and Hall2015; Madsen et al., Reference Madsen, Nyberg, Magnusson Hanson, Ferrie, Ahola, Alfredsson, Batty, Bjorner, Borritz, Burr, Chastang, de Graaf, Dragano, Hamer, Jokela, Knutsson, Koskenvuo, Koskinen, Leineweber, Niedhammer, Nielsen, Nordin, Oksanen, Pejtersen, Pentti, Plaisier, Salo, Singh-Manoux, Suominen, ten Have, Theorell, Toppinen-Tanner, Vahtera, Väänänen, Westerholm, Westerlund, Fransson, Heikkilä, Virtanen, Rugulies and Kivimäki2017; Rugulies et al., Reference Rugulies, Aust and Madsen2017; Rudkjoebing et al., Reference Rudkjoebing, Bungum, Flachs, Eller, Borritz, Aust, Rugulies, Rod, Biering and Bonde2020; Mikkelsen et al., Reference Mikkelsen, Coggon, Andersen, Casey, Flachs, Kolstad, Mors and Bonde2021). These include, for example, job strain (Madsen et al., Reference Madsen, Nyberg, Magnusson Hanson, Ferrie, Ahola, Alfredsson, Batty, Bjorner, Borritz, Burr, Chastang, de Graaf, Dragano, Hamer, Jokela, Knutsson, Koskenvuo, Koskinen, Leineweber, Niedhammer, Nielsen, Nordin, Oksanen, Pejtersen, Pentti, Plaisier, Salo, Singh-Manoux, Suominen, ten Have, Theorell, Toppinen-Tanner, Vahtera, Väänänen, Westerholm, Westerlund, Fransson, Heikkilä, Virtanen, Rugulies and Kivimäki2017; Mikkelsen et al., Reference Mikkelsen, Coggon, Andersen, Casey, Flachs, Kolstad, Mors and Bonde2021), effort–reward imbalance (Mikkelsen et al., Reference Mikkelsen, Coggon, Andersen, Casey, Flachs, Kolstad, Mors and Bonde2021; Rugulies et al., Reference Rugulies, Aust and Madsen2017), low job control (Theorell et al., Reference Theorell, Hammarström, Aronsson, Bendz, Grape, Hogstedt, Marteinsdottir, Skoog and Hall2015), workplace bullying (Mikkelsen et al., Reference Mikkelsen, Coggon, Andersen, Casey, Flachs, Kolstad, Mors and Bonde2021; Theorell et al., Reference Theorell, Hammarström, Aronsson, Bendz, Grape, Hogstedt, Marteinsdottir, Skoog and Hall2015) and threats and violence at work (Rudkjoebing et al., Reference Rudkjoebing, Bungum, Flachs, Eller, Borritz, Aust, Rugulies, Rod, Biering and Bonde2020).
To our knowledge, only three small-scale studies have reported prospective associations between psychosocial work factors and recurrent episodes of depression. First, a study of 583 Canadian working adults with a history of depression found that neither job strain, effort–reward imbalance, lack of supervisor support nor lack of co-worker support was associated with the recurrence of depressive symptoms within a 1-year follow-up period (Wang et al., Reference Wang, Patten, Currie, Sareen and Schmitz2012). Second, a Japanese study of 540 employees returning to work after a leave of absence spell due to depression found that high job demands but not low job control were associated with a recurrent physician-certified episode of sickness absence due to depression (Endo et al., Reference Endo, Muto, Haruyama, Yuhara, Sairenchi and Kato2015). Third, a US-American study included 233 participants who were employed at baseline and were under treatment for depression and followed their trajectory of depression for up to 23 years. Those with the least severe life course trajectory of depression had a higher work resource index at baseline (job involvement, social cohesion and supervisor support) (Heinz et al., Reference Heinz, Meffert, Halvorson, Blonigen, Timko and Cronkite2018). Consequently, there is a paucity of large-scale studies investigating whether work factors are associated with recurrent episodes of depression.
Major life stressors, such as loss of primary relationships or onset of serious illness, have a more substantial impact on the risk of first-time depressive episodes than subsequent episodes (Kessing and Andersen, Reference Kessing and Andersen2017; Monroe et al., Reference Monroe, Anderson and Harkness2019). Nevertheless, interpersonal stress and lack of social support (outside of work), and other stressors in everyday life, including at work (so-called daily hassles), have been associated with the recurrence of depression in most but not all studies (Bockting et al., Reference Bockting, Spinhoven, Koeter, Wouters and Schene2006; Buckman et al., Reference Buckman, Underwood, Clarke, Saunders, Hollon, Fearon and Pilling2018). These findings are in accordance with the stress sensitisation theory, the dominant theory of stress in recurrent depression, which posits that non-major stressors can trigger subsequent episodes (Monroe et al., Reference Monroe, Anderson and Harkness2019). As such, it is plausible that stressors experienced at work could contribute to depression recurrence.
The potential link between psychosocial work factors and the recurrence of depression warrants further attention. Findings of associations between work factors and the recurrence of depression could inform guidelines regarding the prevention of depressive episodes in the workplace and thereby contribute to decreasing the enormous personal and societal costs of (recurrent) depression (Chisholm et al., Reference Chisholm, Sweeny, Sheehan, Rasmussen, Smit, Cuijpers and Saxena2016; Christensen et al., Reference Christensen, Lim, Saha, Plana-Ripoll, Cannon, Presley, Weye, Momen, Whiteford, Iburg and McGrath2020; Malhi and Mann, Reference Malhi and Mann2018).
Healthcare workers have been reported to face relatively adverse working conditions across several dimensions including, for example, high time pressure, high emotional work demands and more exposure to violence and threats (Aagestad et al., Reference Aagestad, Tyssen and Sterud2016; Vinckx et al., Reference Vinckx, Bossuyt and Dierckx de Casterlé2018). In this paper, we used data on several dimensions of the psychosocial work environment in a large Danish public healthcare employee cohort linked to national register data on treatment for depression. We aimed to examine whether work factors are associated with the risk of first-time and recurrent treatment for depression.
Methods
Study population
The study population consisted of participants in the 2014 wave of the Well-being in Hospital Employees (WHALE) study of all employees in the public healthcare enterprise of the Capital Region of Denmark in March 2014 (Hvidtfeldt et al., Reference Hvidtfeldt, Bjorner, Jensen, Breinegaard, Hasle, Bonde and Rod2017). Of the 37,720 participants invited to a workplace assessment survey, 31,823 (84%) responded. We excluded participants who had inconsistent data (n = 621), were trainees (n = 107), worked less than 18.5 hours per week at baseline or were working on an hourly basis (n = 612), had missing sociodemographic information (n = 474), emigrated (n = 230) or died (n = 128) during follow-up or had missing values on any of the included psychosocial work factors (n = 4086). We also excluded 1339 participants who had been treated for depression within the last 6 months before baseline to omit participants who concurrently or recently had undergone treatment for depression.
Participants treated for depression were identified through registrations of Anatomical Therapeutic Chemical (ATC) codes indicating redeeming of prescribed antidepressant medication (N06A) in the Danish National Prescription Registry (Pottegård et al., Reference Pottegård, Schmidt, Wallach-Kildemoes, Sørensen, Hallas and Schmidt2016) and through registrations of the International Statistical Classification of Diseases and Related Health Problems version 10 (ICD-10) codes indicating a hospital contact with unipolar depression (F32 and F33) in the Danish National Patient Register (Lynge et al., Reference Lynge, Sandegaard and Rebolj2011). This definition thus includes participants with a depression-related contact with the public hospital sector as well as participants treated using antidepressants in the primary and secondary care sector. Data on other forms of depression treatment were not available.
We defined two study populations based on the participants’ personal treatment histories. We used all the treatment data available in the project, dating back to 1 January 2000 (14.3 years), as recurrence of depression can occur up to 15 years or more after the recovery from an index episode (Eaton et al., Reference Eaton, Shao, Nestadt, Lee, Bienvenu and Zandi2008; Mattisson et al., Reference Mattisson, Bogren, Horstmann, Munk-Jörgensen and Nettelbladt2007). Thus, we defined 1) a population of 21,156 participants without a registered history of treatment for depression within the past 14.3 years before baseline (1 January 2000–31 March 2014) and 2) a population of 3070 participants with a registered history of treatment for depression within the past 14.3 years, excluding those registered with treatment in the 6-month washout period before baseline as described above (1 January 2000–31 August 2013). In total, the two study populations included 24,226 participants.
Psychosocial work factors
We examined ten individual work factors which we grouped into four broad dimensions: 1) Collegial relations included lack of collaboration and exposure to bullying (78% of those bullied reported the perpetrator to be a colleague or internal collaborator). 2) Job organisation included low job control, low influence over work schedule and high work demands. 3) Management and leadership concerning both the immediate supervisor (low leadership quality and low recognition) and the work unit in general (low justice and low trust). 4) Offensive behaviours by external actors included exposure to threats/violence (98% of those exposed to threats/violence reported the perpetrator to be a patient, user, relative or external collaborator, that is, persons external to the organisation). We also included three composite factors stemming from internationally recognised theoretical models within research on psychosocial work environments and health: effort–reward imbalance (high work demands in combination with low recognition and justice) (Siegrist, Reference Siegrist1996), job strain (a combination of high work demands and low job control) (Karasek, Reference Karasek1979) and low workplace social capital (a low average level of collaboration, justice and trust) (Kawachi and Berkman, Reference Kawachi, Berkman, Berkman, Kawachi and Glymour2014). Given the high number of included work factors, we dichotomised all factors to simplify their interpretation. Details of the measured work factors including item phrasing, scale construction, construction of the composite measures and exposure definitions are available in Appendix 1.
Treatment for depression
We followed the participants prospectively for registrations of treatment for depression for up to 2 years after baseline (1 April 2014–31 March 2016). We limited the follow-up period to 2 years to increase the likelihood that incident treatment for depression could be caused by the work exposures reported at baseline as changes in working conditions due to, for example, organisational changes are frequent within the Danish public hospital sector (Jensen et al., Reference Jensen, Flachs, Skakon, Rod and Bonde2018). We defined first-time treatment for depression as registrations of treatment occurring among those without a history of treatment and recurrent treatment for depression as registrations occurring among those with a history of treatment.
Covariates
We included sociodemographic and employment characteristics as covariates. The sociodemographic characteristics included age, sex, education, occupation, household income and marital status. Employment characteristics included seniority, full-time/part-time employment status and workplace (using the top-tier organisational structure in the Capital Region of Denmark). An overview of the categorisations is presented in Table 1. We obtained information regarding education, household income and marital status from national registries, while we obtained information on age, sex and occupation from employer-based administrative data. We obtained all information on covariates at or before baseline (31 March 2013). Furthermore, we also included the number of years since the last treatment registration for those with a treatment history.
Table 1. Sociodemographic and employment characteristics of the study populations with and without a history of treatment for depression. Total N = 24,226
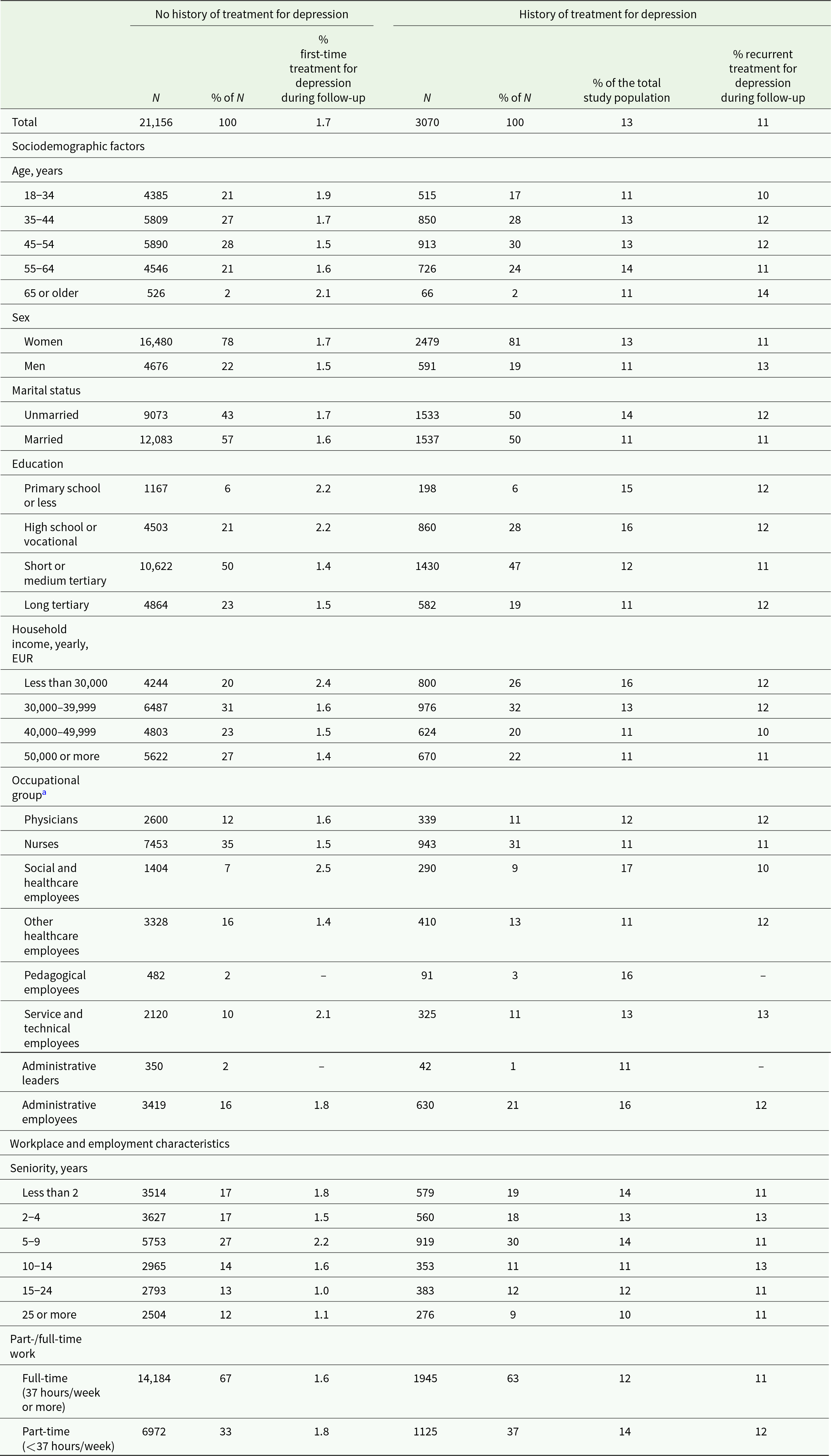
a Some data are not shown due to small cell numbers (<5 observations)
Statistical analysis
We performed the primary analyses separately in the two study populations. We applied logistic regression models to determine the associations between each psychosocial work factor and treatment for depression during follow-up. We applied Firth correction to correct a small degree of statistical separation in the logistic regression models. Furthermore, we weighted the regression models with inverse probability (IP) weights as we excluded a large number of participants due to missingness on at least one work factor (n = 4086). We constructed these weights separately in the two study populations and modelled them as the inverse of the probability of having a missing value on at least one work factor conditional on the sociodemographic factors and employment characteristics. Thereby, the IP weighting allowed the study populations to represent both those with and without missing work factor data. We report odds ratios (OR) with accompanying 95% confidence intervals (95% CI) from the logistic regression models. We adjusted all analyses for sociodemographic and employment characteristics, as mentioned above. Furthermore, we adjusted the analyses of recurrent treatment for depression for the time (years) passed since the last registered treatment.
We conducted three supplementary analyses: (1) Single-factor analyses that were not IP-weighted. (2) Mutually adjusted analyses. Mutually adjusting all work factors for each other will likely result in overadjustment due to their complex interplay, but they are reported here for completeness. (3) The washout period of 6 months may not have adequately excluded participants treated with antidepressants at baseline. Therefore, we extended the washout period to 1 and 2 years, respectively.
Results
In total, the study population included 24,226 participants, of which approximately four out of five were women. Overall, 3070 (13%) had a history of depression treatment, whereas 21,156 (87%) had not. Among those with a history, 92% were identified through redeemed prescriptions only (Supplementary Table S1). Table 1 shows the descriptive characteristics of the study populations.
Those with a history of treatment for depression were more often women and unmarried and had lower education and household income than those without a history. Also, a history of treatment was more frequent among social- and healthcare employees, pedagogical employees and administrative employees compared to other occupational groups.
In total, 703 participants (2.9%) registered with treatment for depression during the follow-up period. Of those, 95% were identified through redeemed prescriptions only (Supplementary Table S2). Among those at risk for first-time treatment, 350 (1.7%) had treatment for depression during follow-up, while among those at risk for recurrent treatment, 353 (11%) had treatment during follow-up. The crude risk of recurrent treatment was lower with more years without treatment (Supplementary Table S3).
Figure 1 shows the distributions of work factors among those with and without a treatment history at baseline. In general, participants with a treatment history reported more adverse psychosocial work environments on all factors than those without a history, most notably a higher exposure to bullying.
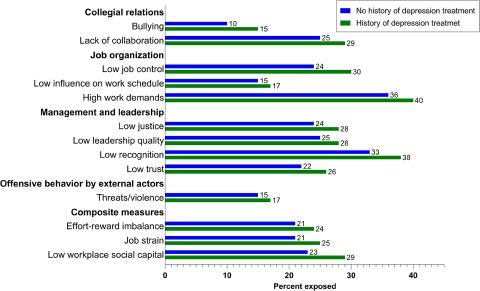
Figure 1. Distribution of work factors among those with (N = 3070) and without (N = 21,156) history of treatment for depression at baseline.
Figure 2 shows the associations between work factors and registering with first-time or recurrent treatment for depression during follow-up. Details of the estimates can be found in Supplementary Tables S4 and S5. The reference groups of all associations are those not exposed to the specific risk factor. The odds of first-time treatment were higher only in those reporting exposure to bullying (OR = 1.72, 95% CI: 1.30–2.29). However, there was also a tendency towards higher odds of first-time treatment among participants who had a low influence on their work schedule (OR = 1.27, 95% CI: 0.97–1.66) and among those exposed to job strain (OR = 1.24, 95% CI: 0.97–1.57). The odds of recurrent treatment were higher among those experiencing bullying (OR = 1.40, 95% CI: 1.04–1.88) and a lack of collaboration (OR = 1.31, 95% CI: 1.03–1.67) and among those who had low job control (OR = 1.27, 95% CI: 1.00–1.63). Most work factors, however, were neither associated with first-time nor recurrent treatment for depression.

Figure 2. Associations between psychosocial work factors and first-time (N = 21,156) and recurrent treatment for depression (N = 3070). Numerical figures are shown in Supplementary Tables S4 and S5.
The absolute risk of depression treatment during follow-up was much higher for those at risk of recurrent treatment (11%) than those at risk of first-time treatment (1.7%). Accordingly, among those under risk for first-time treatment who were bullied, the absolute risk was 2.8%, while among those under risk for recurrent treatment who were bullied, the absolute risk was 15%. Due to the substantial differences in absolute risk, the ORs from the two analyses are not directly comparable.
Supplementary analyses
The estimates in the analyses without IP-weighting were similar to the primary analysis (Supplementary Tables S6 and S7). The estimates in the mutually adjusted analyses were also similar to the primary analyses. However, all CIs overlapped unity in the analyses of recurrent treatment (Supplementary Tables S8 and S9). In analyses of recurrent treatment, where the exclusion of participants treated before baseline was extended to 1 and 2 years, respectively, the associations for exposure to bullying (OR2Y = 1.85, 95% CI: 1.30–2.63) and low job control (OR2Y = 1.37, 95% CI: 1.02–1.85) became stronger with longer exclusion time. Most other point estimates were similar to the primary analysis. However, the CIs became wider due to fewer cases (Supplementary Tables S10 and S11).
Discussion
Thirteen percent of the employees had a history of treatment for depression. Among them, more than one in ten had recurrent treatment within the 2-year follow-up period. In general, those with a history of treatment perceived their psychosocial work environment more negatively than those without depression. Overall, we found that only few work factors were associated with treatment for depression.
Exposure to bullying and, to some extent, job strain were associated with a higher risk of first-time treatment for depression. In previous studies, bullying was generally the strongest psychosocial work risk factor for the onset of depression, with a more than twofold higher risk previously reported (Mikkelsen et al., Reference Mikkelsen, Coggon, Andersen, Casey, Flachs, Kolstad, Mors and Bonde2021; Theorell et al., Reference Theorell, Hammarström, Aronsson, Bendz, Grape, Hogstedt, Marteinsdottir, Skoog and Hall2015). The association between job strain and first-time treatment for depression reported here is similar in magnitude to those reported in some analyses (Madsen et al., Reference Madsen, Nyberg, Magnusson Hanson, Ferrie, Ahola, Alfredsson, Batty, Bjorner, Borritz, Burr, Chastang, de Graaf, Dragano, Hamer, Jokela, Knutsson, Koskenvuo, Koskinen, Leineweber, Niedhammer, Nielsen, Nordin, Oksanen, Pejtersen, Pentti, Plaisier, Salo, Singh-Manoux, Suominen, ten Have, Theorell, Toppinen-Tanner, Vahtera, Väänänen, Westerholm, Westerlund, Fransson, Heikkilä, Virtanen, Rugulies and Kivimäki2017; Mikkelsen et al., Reference Mikkelsen, Coggon, Andersen, Casey, Flachs, Kolstad, Mors and Bonde2021) and lower than in other analyses (Madsen et al., Reference Madsen, Nyberg, Magnusson Hanson, Ferrie, Ahola, Alfredsson, Batty, Bjorner, Borritz, Burr, Chastang, de Graaf, Dragano, Hamer, Jokela, Knutsson, Koskenvuo, Koskinen, Leineweber, Niedhammer, Nielsen, Nordin, Oksanen, Pejtersen, Pentti, Plaisier, Salo, Singh-Manoux, Suominen, ten Have, Theorell, Toppinen-Tanner, Vahtera, Väänänen, Westerholm, Westerlund, Fransson, Heikkilä, Virtanen, Rugulies and Kivimäki2017). The CIs reported here likely overlap unity due to a low number of cases. Thus, the findings regarding bullying job strain are generally in line with previous studies.
We did not find an association between low job control and first-time treatment for depression, even though this association has previously been reported (Theorell et al., Reference Theorell, Hammarström, Aronsson, Bendz, Grape, Hogstedt, Marteinsdottir, Skoog and Hall2015; Madsen et al., Reference Madsen, Nyberg, Magnusson Hanson, Ferrie, Ahola, Alfredsson, Batty, Bjorner, Borritz, Burr, Chastang, de Graaf, Dragano, Hamer, Jokela, Knutsson, Koskenvuo, Koskinen, Leineweber, Niedhammer, Nielsen, Nordin, Oksanen, Pejtersen, Pentti, Plaisier, Salo, Singh-Manoux, Suominen, ten Have, Theorell, Toppinen-Tanner, Vahtera, Väänänen, Westerholm, Westerlund, Fransson, Heikkilä, Virtanen, Rugulies and Kivimäki2017; Mikkelsen et al., Reference Mikkelsen, Coggon, Andersen, Casey, Flachs, Kolstad, Mors and Bonde2021). The point estimate reported in this study is similar to the one reported in the systematic review by Mikkelsen et al. but had wider CIs (Mikkelsen et al., Reference Mikkelsen, Coggon, Andersen, Casey, Flachs, Kolstad, Mors and Bonde2021). The association reported by Madsen et al. was based on more cases and longer follow-up (Madsen et al., Reference Madsen, Nyberg, Magnusson Hanson, Ferrie, Ahola, Alfredsson, Batty, Bjorner, Borritz, Burr, Chastang, de Graaf, Dragano, Hamer, Jokela, Knutsson, Koskenvuo, Koskinen, Leineweber, Niedhammer, Nielsen, Nordin, Oksanen, Pejtersen, Pentti, Plaisier, Salo, Singh-Manoux, Suominen, ten Have, Theorell, Toppinen-Tanner, Vahtera, Väänänen, Westerholm, Westerlund, Fransson, Heikkilä, Virtanen, Rugulies and Kivimäki2017), while the summary estimate from the meta-analysis by Theorell et al. was based on the least adjusted models in the primary studies, which might not have been adequately controlled for confounding (Theorell et al., Reference Theorell, Hammarström, Aronsson, Bendz, Grape, Hogstedt, Marteinsdottir, Skoog and Hall2015). Thus, these discrepancies may be due to various methodological differences between this study and the previous meta-analyses. Also contrary to prior literature, we did not find an association between exposure to violence and threats and first-time treatment for depression (Rudkjoebing et al., Reference Rudkjoebing, Bungum, Flachs, Eller, Borritz, Aust, Rugulies, Rod, Biering and Bonde2020) nor between effort–reward imbalance and first-time treatment for depression (Mikkelsen et al., Reference Mikkelsen, Coggon, Andersen, Casey, Flachs, Kolstad, Mors and Bonde2021; Rugulies et al., Reference Rugulies, Aust and Madsen2017).
Regarding recurrent treatment, we found that exposure to bullying, a lack of collaboration and low job control were associated with recurrent treatment for depression. In line with our findings, a more supportive work environment at baseline was associated with a less severe life-course trajectory of depression in a US-American study of 233 working adults with depression (Heinz et al., Reference Heinz, Meffert, Halvorson, Blonigen, Timko and Cronkite2018). However, low co-worker support was not associated with depressive symptoms after 1 year in a small Canadian cohort study of 583 working adults with a history of depression (Wang et al., Reference Wang, Patten, Currie, Sareen and Schmitz2012). Endo et al. reported that high job demands but not low job control were associated with recurrent physician-certified episodes of sickness absence due to depression among 540 Japanese employees with previous registrations of such a sickness absence episode (Endo et al., Reference Endo, Muto, Haruyama, Yuhara, Sairenchi and Kato2015). In contrast, we found that low job control but not high job demands was associated with recurrent treatment for depression. None of the previous studies included exposure to bullying, which showed the strongest association with both first-time and recurrent treatment in the present study.
Interpretation and implications
The stress sensitisation theory posits that non-major stressors, which might not be strong enough to trigger an initial episode of depression, may trigger recurrent episodes of depression as individuals become sensitised to stress after a first-time depressive episode (Monroe et al., Reference Monroe, Anderson and Harkness2019). It seems reasonable to assume that workplace bullying can be considered a major stressor (Mikkelsen et al., Reference Mikkelsen, Hansen, Persson, Byrgesen, Hogh, Einarsen, Hoel, Zapf and Cooper2020). Accordingly, we found that bullying was associated with both first-time and recurrent treatment for depression. However, although results from selected analyses (on lack of collaboration and low job control) agree with the stress sensitisation theory, overall, our study does not provide strong support for this theory within a workplace setting as most work stressors were not associated with recurrent treatment for depression. Nevertheless, these findings align with studies suggesting that interpersonal stressors, lack of social support outside work and daily life stressors (including those at work) can affect the risk of recurrent episodes of depression (Bockting et al., Reference Bockting, Spinhoven, Koeter, Wouters and Schene2006; Buckman et al., Reference Buckman, Underwood, Clarke, Saunders, Hollon, Fearon and Pilling2018).
This study was conducted among predominantly female public hospital employees. Women have higher incidence of depression than men (Kessler et al., Reference Kessler, Petukhova, Sampson, Zaslavsky and Wittchen2012; Wittchen et al., Reference Wittchen, Jacobi, Rehm, Gustavsson, Svensson, Jönsson, Olesen, Allgulander, Alonso, Faravelli, Fratiglioni, Jennum, Lieb, Maercker, van Os, Preisig, Salvador-Carulla, Simon and Steinhausen2011), but there is only limited evidence for differential associations between risk factors and depression between women and men (Kuehner, Reference Kuehner2017). Healthcare employees may be less prone to seek treatment for mental health problems, due to, for example, concerns over confidentiality or negative social judgment (Clement et al., Reference Clement, Schauman, Graham, Maggioni, Evans-Lacko, Bezborodovs, Morgan, Rüsch, Brown and Thornicroft2015). This suggests that the associations between work factors and treatment for depression reported here might be slightly underestimated compared to other occupations or to, for example, a nationally representative sample of employees.
Strengths and limitations
Strengths of the study include the large study population with a very high response rate, comprehensive measurement of several psychosocial work factors and prospective linkage to national registers. Employing different data sources, we could assess the associations between several work factors and both first-time and recurrent treatment for depression while adjusting for sociodemographic and employment factors. The study adds much-needed evidence regarding the role of work factors in recurrent depression.
Several limitations are relevant to discuss. First, register-based treatment information is not optimal for identifying those who develop depressive episodes. Fewer than half of those experiencing a depressive episode are in contact with the healthcare system and even fewer are treated with antidepressant medication (Packness et al., Reference Packness, Halling, Hastrup, Simonsen, Wehberg and Waldorff2018). A recent Danish study found that among individuals who screened positive for depression using the Major Depression Inventory, 51% had redeemed a prescription of antidepressant medication within 10 years before to 2 years after the screening (Weye et al., Reference Weye, McGrath, Lasgaard, Momen, Knudsen, Musliner and Plana‐Ripoll2023). In our study, most cases were registered solely by the criteria of having redeemed prescribed antidepressant medication. Consequently, our estimates of the incidence and prevalence of treatment for depression are likely underestimated compared to the actual rates of depression. Furthermore, antidepressant medication is commonly taken for other mental disorders, such as anxiety/panic disorders or sleep disorders (Kazdin et al., Reference Kazdin, Wu, Hwang, Puac-Polanco, Sampson, Al-Hamzawi, Alonso, Andrade, Benjet, Caldas-de-almeida, de Girolamo, de Jonge, Florescu, Gureje, Haro, Harris, Karam, Karam, Kovess-Masfety, Lee, McGrath, Navarro-Mateu, Nishi, Oladeji, Posada-Villa, Stein, Üstün, Vigo, Zarkov, Zaslavsky and Kessler2023). Thus, we have likely misclassified some participants who are being treated for other disorders as being treated for depression.
Second, we were not able to account for the nature of the participants’ history of depression at baseline, which is among the strongest predictors of recurrence. This includes whether residual symptoms are present (Buckman et al., Reference Buckman, Underwood, Clarke, Saunders, Hollon, Fearon and Pilling2018), the severity of the first episode (Buckman et al., Reference Buckman, Underwood, Clarke, Saunders, Hollon, Fearon and Pilling2018) and the number of previous episodes (Buckman et al., Reference Buckman, Underwood, Clarke, Saunders, Hollon, Fearon and Pilling2018; Kessing and Andersen, Reference Kessing and Andersen2017). Concurrent depression or depressive symptoms at baseline may have negatively influenced the appraisal of the work environment and increased the risk of being treated for depression during follow-up. Thereby, this source of confounding could have biased the results away from the null. However, the associations with recurrent treatment were similar (or stronger) when we extended the exclusion period before baseline for up to 2 years, excluding those with the highest risk of recurrence.
Third, the study population with a depression treatment history is likely a selected sample of all working-age individuals with a depression history. Mental health issues such as depression are associated with involuntary exit from the workplace to unemployment or disability pension (Rm van et al., Reference van Rijn, Robroek, Brouwer and Burdorf2014). Furthermore, those with more severe episodes of depression are perhaps less likely to enter, stay at or return to work. Similarly, those with more adverse work environments are perhaps also less likely to stay or return than those with more favourable work environments. Such selection forces likely biased the associations for recurrent treatment towards the null.
Finally, some of the work factors were measured using a limited number of items. In particular, the measure of effort–reward imbalance may have been measured inadequately as we were only able to include items covering recognition from the management and the experience of justice as rewards while monetary rewards or job security also form part of the original effort–reward imbalance construct (Siegrist, Reference Siegrist1996). A similar point can be raised about other work factors, for example, justice (often referred to as procedural justice), which originally was measured using seven items, whereas we measured it using only two items (Elovainio et al., Reference Elovainio, Kivimäki and Vahtera2002). However, one multi-cohort study has suggested that using one-item measurements of procedural justice may not differ much from using instruments with more items (Xu et al., Reference Xu, Rugulies, Vahtera, Pentti, Mathisen, Lange, Clark, Magnusson Hanson, Westerlund, Ervasti, Virtanen, Kivimäki and Rod2022).
Conclusions
Depression constitutes a substantial morbidity burden in the workplace. Thirteen percent of the participants had a history of treatment for depression, and they experienced more adverse work environments and had a much higher risk of treatment for depression during follow-up compared to those without such a history. Exposure to bullying was associated with higher odds of both first-time and recurrent treatment for depression. Furthermore, job strain and low influence over the work schedule were associated with first-time treatment for depression, while low job control and lack of collaboration were associated with recurrent treatment for depression.
Supplementary material
The supplementary material for this article can be found at https://doi.org/10.1017/S2045796024000167.
Availability of data and materials
Data used in this study and from Danish registers are not publicly available due to Danish legislation. Anonymised data from the WHALE study are available upon reasonable request through collaborative agreements. Please contact Professor Naja Hulvej Rod [[email protected]] for further details.
Financial support
The work was supported by a grant from the Danish Regions (employer organisation), the Danish Association of Local Government Employees Organizations (Forhandlingsfællesskabet; employee organisation) and the Danish Working Environment Research Fund (grant number: 14-2018-09). The sponsors had no role in the study design, the collection, analysis and interpretation of the data, the writing of the manuscript or the decision to submit it for publication.
Competing interests
JM is currently employed at Novo Nordisk A/S and affiliated as a guest researcher at the Section of Epidemiology at the University of Copenhagen. The majority of the work by JM on this manuscript was conducted during a former employment spell at the Section of Epidemiology at the University of Copenhagen, and the remaining work was conducted in the role as a guest researcher at the University of Copenhagen. Novo Nordisk A/S had no role in any part of the study including the study design, the collection, analysis and interpretation of the data, the writing of the manuscript or the decision to submit it for publication. The other authors report no conflict of interest.
Ethical standards
The authors assert that all procedures contributing to this work comply with the ethical standards of the relevant national and institutional committees on human experimentation and with the Helsinki Declaration of 1975, as revised in 2000.





