The concepts of equifinality and multifinality were originally derived by general systems theory (von Bertalanffy, Reference von Bertalanffy1968) and were initially formally applied to developmental psychopathology by Cicchetti and Rogosh (Reference Cicchetti and Rogosh1996) approximately 28 years ago. On the occasion of Dr Cicchetti’s retirement from the Journal, it is therefore most fitting to revisit these two critical constructs and their potential application to models for prevention of problem behavior in general, and emerging problem behavior in early childhood (0–5 years), in particular. As described by Cicchetti and Rogosh (Reference Cicchetti and Rogosh1996), equifinality pertains to how the same end state may be reached from different starting points and via multiple intervening processes. As the human condition is typically defined as an open system versus a closed one (Mayr, Reference Mayr1964, Reference Mayr1968), changes that affect the individual and their context have the potential to prevent or potentiate a pathway leading to problem behavior. Accordingly, if the conditions of the individual change or the processes influencing the pathway to problem behavior are modified, the end state also can be modified (von Bertalanffy, Reference von Bertalanffy1968). Within the field of developmental psychopathology, equifinality has been used to explain why and how a variety of pathways lead to the same problem behavior despite differences in the individual’s starting point of risk (Cicchetti & Rogosh, Reference Cicchetti and Rogosh1996).
Complementing the construct of equifinality, multifinality refers to the diversity of outcomes leading from the same adverse event (e.g., experience of childhood maltreatment, exposure to high levels of parental conflict or neighborhood violence). Much of the field of developmental psychopathology has been focused on identifying protective factors that account for positive adaptation in the context of chronic and/or acute adverse conditions that are reliably, yet not universally, associated with the development of problem behavior, commonly referred to as resilience. In fact, many selective preventive interventions have been developed based on the premise of multifinality. Specifically, by identifying children with risk reliably (but not deterministically) associated with adverse outcomes, preferably as early as possible, the delivery of intervention can prevent the development of psychopathology and promote resilience.
The concepts of equifinality and multifinality have traditionally been applied to the field of developmental psychopathology in reference to the identification of the many constellations of risk related to the same child psychopathology (i.e., equifinality) and the potential for preventive interventions to attenuate the adverse consequences of initial exposure to risk and/or lead to multiple types of positive adaptation (i.e., multifinality). The goal of the current paper is to extend the premise of equifinality and multifinality to the design and application of prevention interventions. In doing so, we question the underlying assumption of most intervention models that “one size should fit all.” First, we use the principles of equifinality and multifinality to describe the limitations of applying one intervention model to support all children (and parents) presenting with different types of risk for early problem behavior. We then describe the potential benefits of applying a tiered model, describing two applications of this approach for preventing psychopathology and promoting school readiness beginning at birth. The first of these tiered trials, Smart Beginnings, integrates the use of two evidenced-based preventive interventions, Video Interaction Project (VIP, Mendelsohn et al., Reference Mendelsohn, Dreyer, Flynn, Tomopoulos, Rovira, Tineo, Pebenito, Torres, Torres and Nixon2005), a universal parenting program, and Family Check-Up (FCU, Dishion et al., Reference Dishion, Shaw, Connell, Gardner, Weaver and Wilson2008), a selective parenting program. The second trial, the Early Childhood Collaborative of The Pittsburgh Study (TPS), also includes VIP and FCU, but also other more and less-intensive parenting programs to address the full spectrum of strengths and risks of parents of infants and toddlers.
Equifinality and multifinality applied to early childhood: infancy through preschool
The real-life application of the principle of equifinality became manifest when recruiting a sample of low-income families with boys approaching age 2 for an RCT to initially test the effectiveness of the FCU (Shaw et al., Reference Shaw, Dishion, Supplee, Gardner and Arnds2006). Eligibility criteria included having a child with clinically meaningful levels of conduct problems. It is quite unusual to see 55 consecutive cases (i.e., 55 of 60 randomly assigned to the FCU engaged in the FCU, 91.7%) where the presenting problem is a two-year old boy with emerging conduct problems. Thus, in some ways having such homogeneity in child symptoms provided a natural laboratory to examine the validity of the principle of equifinality for toddler males with conduct problems. Heavily influenced by Patterson’s (Reference Patterson1982) social learning model of parent-child coercion, we expected 50%–75% of families to show high levels of parent-child conflict accompanied by high levels of harsh and rejecting parenting. Contrary to our expectations, we were underwhelmed with the percentage of cases demonstrating profiles consistent with models of coercion. In less than 25% of cases could a case be made that the child’s current high levels of conduct problems appeared in concert with high levels of parent-child conflict, presumably fueled by individual differences in dimensions of child temperament (e.g., negative emotionality, inhibitory control, fearlessness) and/or parenting (e.g., hostility, inconsistency, neglect). Although the profile of high parent-child conflict with high levels of rejecting/hostile parenting behavior was the most commonly evident profile, other presenting contexts included having a severely depressed primary caregiver (typically biological mother), having severe economic and neighborhood deprivation, having a parent or parents with a history of trauma, and having a family environment with high levels of chaos and disorganization. Thus, at least during early childhood in reference to the development of emerging conduct problems among low-income and racially and ethnically diverse boys, the concept of equifinality appears to be operative.
The validity of multifinality in early childhood is evident based on the variability and lack of reliable prediction from children’s exposure to a variety of severe life events and subsequent socioemotional outcomes. Even for young children living in the context of poverty, which typically encompasses stressful contexts within and outside of the home (e.g., the quality of child care, availability of nutritionally sound food and nearby grocery stores, exposure to violence in the neighborhood, and greenspaces), more than two thirds of children fail to show consistently elevated levels of conduct and/or emotional problems through middle childhood and adolescence (Feng et al., Reference Feng, Shaw and Silk2008; Moilanen et al., Reference Moilanen, Shaw and Maxwell2010; Shaw et al., Reference Shaw, Gilliom, Ingoldsby and Nagin2003, Reference Shaw, Hyde and Brennan2012). These findings coupled with the typically low magnitude of “reliable” individual predictors of child problem behavior, typically ranging from correlations of .15–.30 and accounting for less than 5% of variance, suggest a lot of heterogeneity in children’s initial and later reactions to experiencing comparable levels of stressful and, even, traumatic events. These data from childhood are reinforced by the variability in adults’ reactions and subsequent outcomes after experiencing traumatic events, resulting in typically modest rates of post-traumatic stress disorder (PTSD) after experiencing such events as combat (2%), witnessing violent crimes, death or accidents (7%–11%) or being a victim of sexual assault (14%) (Norris, Reference Norris1992). Comparably modest rates of vulnerability to PTSD have been found in more recent studies of adults’ exposure to traumatic events (Lukaschek et al., Reference Lukaschek, Kruse, Emeny, Lacruz, von Eisenhart Rothe and Ladwig2013).
Applying equifinality and multifinality to the prevention of psychopathology and promotion of school readiness during early childhood
Models of developmental psychopathology have validated the principles of equifinality and multifinality in conducting basic research by demonstrating the multiple pathways leading to the same outcome and the modest to moderate magnitude of associations between “reliable” risk factors and specific types of psychopathology, respectively. Despite a strong stated interest among intervention and prevention researchers in identifying which treatments are most effective for specific populations (Ng & Weisz, Reference Ng and Weisz2016; Weisz & Hawley, Reference Weisz and Hawley2002), it is surprising that early parenting programs to prevent psychopathology and promote young children’s school readiness have not utilized a tiered approach to address the uncertainties embedded in equifinality (i.e., multiple pathways leading to problem behavior) and multifinality (lack of determinism in child outcomes despite the context of one or more serious risk factors). There are exceptions to this dearth of investment in tiered models in early childhood, but even the few existing tiered models often represent different levels of the same overarching intervention rather than the integration of independent models (e.g., Prinz et al., Reference Prinz, Sanders, Shapiro, Whitaker and Lutzker2009). Note a tiered approach has been commonly adopted in addressing children’s academic and behavioral issues at school during middle childhood and adolescence in the United States, as reflected in the popular use of multi-tiered systems of support (MTSS, Horner et al., Reference Horner, Sugai, Todd, Lewis-Palmer, Bambara and Kern2005). In fact, the FCU has been used as a component of a tier-based MTSS for addressing school-based issues for middle schoolchildren (Smolkowski et al., Reference Smolkowski, Seeley, Gau, Dishion, Stormshak, Moore, Falkenstein, Fosco and Garbacz2017). Thus, based on the successful application of tiered approaches for older children, it is even more surprising that tiered approaches have not been implemented widely for children 0–3 years based on the burgeoning interest in addressing mental health for parents and preventing mental health difficulties for children at the population level (Dodge et al., Reference Dodgein press). As discussed below, even within the context of poverty and related risk factors (e.g., exposure to toxins and violence, community resources including quality of childcare and preschools, food deserts), there is heterogeneity in levels of risk and protective factors in children’s ecologies that support the tailoring of prevention and intervention strategies to individual family’s strengths and challenges. Doing so can also address barriers to reducing poverty-related disparities that we describe below.
Barriers to reducing poverty-related disparities
A wide range of intervention programs have sought to prevent early emerging problem behavior and school readiness disparities by promoting the quality of early parent-child relationships (i.e., relational health) and attenuating effects of psychosocial stressors (Shaw et al., Reference Shaw, Mendelsohn and Morris2021). While there is significant evidence of efficacy of programs at the individual child level (e.g., HomVEE, 2020) and there have been some population-level effects on parent investment and positive parenting within metropolitan areas (Shonkoff, Reference Shonkoff2017), including ParentCorps (Brotman et al., Reference Brotman, Dawson-McClure, Kamboukos, Huang, Calzada, Goldfeld and Petkova2016), impacts at the population-level on preventing early problem behavior and promoting school readiness have been surprisingly limited despite decades of attention and investment of sizeable research dollars (Greenberg & Abenavoli, Reference Greenberg and Abenavoli2017; Isaacs & Roessel, Reference Isaacs and Roessel2008). These models face three important barriers and challenges that have severely limited impacts at the population level:
Identification and engagement of low-income parents
The identification and recruitment of parents with infants and toddlers represent a long-standing challenge for implementing early childhood interventions, especially in contexts where there are fewer universally accessed systems (i.e., schools). Family-centered interventions often struggle to identify settings that are already frequented by large numbers of families and thus where large percentages of economically challenged families can easily be reached and offered support. In addition, engaging in such programs may represent a significant challenge in terms of accessibility based on the many demands faced by families in poverty (e.g., working multiple jobs, traveling long distances for work or childcare). Further complicating the identification challenge is a prevention program’s ability to engage families, which is highly dependent on the convenience of using the program. There is likely to be considerable heterogeneity across families, with variation in preference for time and location of intervention delivery, with some families preferring clinical settings where they already will be, and others preferring delivery in their homes or other accessible locations (e.g., libraries, family support centers). Key barriers to engagement include logistical issues (e.g., time, transportation) exacerbated by work force participation and attitudes regarding preventive strategies (Spoth et al., Reference Spoth, Redmond, Hockaday and Shin1996, Reference Spoth, Clair, Greenberg, Redmond and Shin2007). Based on the presence of these barriers, it should not be surprising to learn that only approximately 40% of families invited to enroll in home visiting programs do so (Bower et al., Reference Bower, Nimer, West and Gross2020), with 80% of families receiving less than the intended number of offered visits (Sparr et al., Reference Sparr, Zaid, Filene and Denmark2017). As an example, it is estimated that only one-third of Early Head Start families complete the program (Isaacs & Roessel, Reference Isaacs and Roessel2008).
Cost and potential for scalability in existing service systems
Existing programs for infants and toddlers cannot easily utilize platforms that support population-level impact (e.g., public school systems), in large part because such universal platforms do not exist during very early childhood (Shaw et al., Reference Shaw, Mendelsohn and Morris2021). Importantly, from a prevention science standpoint, existing approaches are typically very expensive whether located in the home (e.g., $3750/family/year for ParentChild+; Levenstein et al., Reference Levenstein, Levenstein and Oliver2002; HomVEE, 2020) or center-based (e.g., $10,500/child/year for Early Head Start), making scalability fiscally challenging and population-level impact unlikely. For instance, while Early Head Start (that includes both a center-based and a home-based option) has been shown to significantly impact children’s cognitive and social-emotional development (Love et al., Reference Love, Kisker, Ross, Raikes, Constantine, Boller, Brooks-Gunn, Chazan-Cohen, Tarullo, Brady-Smith, Fuligni, Schochet, Paulsell and Vogel2005, Reference Love, Chazan-Cohen, Raikes and Brooks-Gunn2013), the program reaches only 11% of eligible families (or ∼ 160,000 children; National Head Start Association, 2021). Home visiting programs such as Nurse Family Partnership, Parents as Teachers, and Healthy Families America (Harding et al., Reference Harding, Galano, Martin, Huntington and Schellenbach2007; Olds et al., Reference Olds, Henderson, Cole, Eckenrode, Kitzman, Luckey, Pettitt, Sidora, Morris and Powers1998; Wagner et al., Reference Wagner, Spiker and Linn2002) have been widely disseminated and have favorably impacted maternal-infant health, family relational heath, and school readiness (Olds et al., Reference Olds, Henderson, Chamberlin and Tatelbaum1986, Reference Olds, Henderson, Cole, Eckenrode, Kitzman, Luckey, Pettitt, Sidora, Morris and Powers1998). Although such programs have quadrupled the number of families served recent years to reach approximately 300,000 families (including families served by the home-based version of Early Head Start that comprise about a third of Early Head Start families; National Home Visiting Resource Center, 2020), unmet need remains home visiting programs current capacity is estimated at 2% of families that could benefit, with cost a key contributor.
Heterogeneity of risk
There is substantial heterogeneity in social determinants of health (SDoH), parent assets and vulnerabilities, parent-child early relational health, and child school readiness outcomes in low-income households (Mohajer & Earnest, Reference Mohajer and Earnest2010; Young, Reference Young2014), as well as in frequency of adverse outcomes across all levels of contextual and psychosocial risk (consistent with notions of equifinality and multifinality). Such heterogeneity suggests the need for strategies that are tailored to the specific parenting issues and stressors relevant to individual families and their contexts, as well as linked to specific child outcomes. However, it is challenging to effectively identify those families who are at risk and those who can maximally benefit from various components of an integrated, tiered prevention model. While existing family-centered interventions often address parenting issues broadly and follow a regimented protocol, an emerging body of intervention work has begun to consider and address heterogeneity by addressing social determinants of health (SDoH). For example, the Family Connects postnatal home visiting model (Dodge et al., Reference Dodge, Goodman, Murphy, O’Donnell, Sato and Guptill2014; Goodman et al., Reference Goodman, Dodge, Bai, O’Donnell and Murphy2019) utilizes a variety of screening approaches to facilitate connection of families to community resources during early infancy. In the pediatric health care setting, Healthy Steps co-locates a mental health provider who facilitates practice-level screening/referral for SDoH and provides mental health services for parents (Minkovitz et al., Reference Minkovitz, Hughart, Strobino, Scharfstein, Grason, Hou, Miller, Bishai, Augustyn, McLearn and Guyer2003, Reference Minkovitz, Strobino, Mistry, Scharfstein, Grason, Hou, Ialongo and Guyer2007). Help Me Grow also facilitates provision of services for SDoH through a centralized referral and monitoring process linked to pediatric health care (Dworkin, Reference Dworkin2006).
A comprehensive reduction in disparities is most likely to be successful if it offers services prior to the emergence of risks and challenges (i.e., primary prevention) and as soon as possible following their emergence (i.e., secondary/tertiary prevention). A primary prevention approach is especially applicable for challenges in parent-child relational patterns, which theoretically could be sustained over time and lead to positive cascading impacts on multiple domains across the life course. In addition, a primary prevention approach is far less costly than treatment (Dalziel & Segal, Reference Dalziel and Segal2012; Ramos-Gomez & Shepard, Reference Ramos-Gomez and Shepard1999), as providing specialized resources for implementation for an entire low-income population would be overly costly and overkill for many low-income families at the lower end of the risk continuum. For example, in a low-income sample of 731 WIC families, half of whom were randomly assigned to FCU (secondary/tertiary preventive intervention), using latent class analysis, Pelham et al. (Reference Pelham, Dishion, Tein, Shaw and Wilson2017) found substantial differences in treatment response on later child conduct problems based on the risk status of families at child age two. For low-income families with limited family stressors (other than single parenthood), effect sizes of the FCU were negligible on child conduct problems from ages 3 to 5. However, for those low-income families with a history of parental psychopathology (i.e., depression, antisociality), large family size, history of mental health treatment, and/or a history of contact with child welfare, effects sizes ranged from .63 to .82. In short, the early childhood version of the FCU may not be an optimal intervention for reducing early child problem behavior for lower risk low-income families, whereas it may be quite effective for addressing early problem behavior among higher-risk low-income families. These results are consistent with the principles of equifinality and multifinality and reinforce the need for offering multiple preventive approaches to meet the heterogeneity of challenges faced by low-income families. However, to our knowledge no model has comprehensively integrated primary and secondary/tertiary prevention approaches, perhaps because of a dearth of predictive data on who will be at greatest risk for maladaptive outcomes and who will most benefit.
In addition to addressing the issue of heterogeneity of risk across families, it is also critical to address the fluidity of strengths and challenges families face across children’s development over time (Shaw et al., Reference Shaw, Mendelsohn and Morris2021). As an example, parents who demonstrate contingent responsivity to support infant’s needs during the first year may be less able to provide the requisite structure on children’s behavior during the transition to toddlerhood (i.e., 18 months) when children become more physically mobile and challenges in the home or community increase in the context of poverty and discrimination (Shaw & Bell, Reference Shaw and Bell1993). Based on the fluidity in both developmental and family contexts, there is a need to provide ongoing assessments of parent-child relational health during the birth to age 3 period, rather than only conducting one assessment of child functioning and only during infancy or only during the toddler period. Indeed, while it has not garnered the same attention as research on poverty, there is substantial volatility in income level for families across time (Western et al., Reference Western, Bloome, Sosnaud and Tach2016) that likely has implications for family well-being and children’s development (Hill et al., Reference Hill, Morris, Gennetian, Wolf and Tubbs2013) and further supports the case for repeated assessment and ongoing intervention (again, consistent with the notions of equifinality and multifinality).
Addressing barriers by using a tiered intervention approach: the Smart Beginnings model
Based on the principles of equifinality and multifinality and the challenges in addressing the heterogeneity of risk among families with young children living in poverty to prevent early problem behavior and promote young children’s school readiness, our initial foray in developing a tiered approach has tested the utility of combining two evidence-based approaches, Video Interaction Project (VIP) and Family Check-Up (FCU). In our tiered model, we also have capitalized on the utility of primary pediatric care, described in more detail below (Cates et al., Reference Cates, Weisleder, Dreyer, Johnson, Vlahovicova, Ledesma and Mendelsohn2016). This tiered approach, termed Smart Beginnings and outlined in Figure 1, addresses the barriers of engagement, cost, and heterogeneity and fluidity in risk by assessing risk with repeated assessments across time (Shaw et al., Reference Shaw, Mendelsohn and Morris2021).

Figure 1. Barries to population-level impact addressed by smart beginnings (SB) tiered model.
Using primary pediatric care as the platform for delivery
There were three primary reasons for locating the Smart Beginnings program in primary pediatric care.
Potential for population-level accessibility to low-income families beginning at a very young age with frequent contacts and at relatively low cost
Pediatric primary care has the potential to be a universal platform because of requirements for screening and immunizations prior to school entry, with 13 preventive visits recommended by the American Academy of Pediatrics (AAP) from birth through the age of 5 years (American Academy of Pediatrics, 2021). Improvements in access during the last 2 decades underscore this potential. Medicaid expansion and the State Children’s Health Insurance Program have resulted in ∼ 95% of children being covered and ∼ 60% of the remainder eligible for public insurance (Cohen et al., Reference Cohen, Terlizzi, Cha and Martinez2020; Kenney et al., Reference Kenney, Haley, Pan, Lynch and Buettgens2016), in turn facilitating attendance at AAP-recommended visits. Although barriers to enrollment of Medicaid may have ensued in the context of recent policy changes (Kaiser Family Foundation, 2023) and attendance is typically lower for families receiving public insurance, visit attendance is still estimated conservatively at 40%–80% across all visits through age 3 years (Wolf et al., Reference Wolf, Hochheimer, Sabo, DeVoe, Wasserman, Geissai, Opel, Warren, Puro, O’Neil, Pecsok and Krist2018). Primary care also offers early and frequent contact with families, which translates to a high number of potential “doses” of primary care interventions.
In addition to providing access to otherwise difficult to-reach population, health care interventions have potential for lower cost through leveraging of existing infrastructure and limiting need for additional caregiver/provider and family travel time. VIP, our universal intervention and delivered at preventive visits, is estimated to have a marginal cost of ∼$250/child/year (including staff, supplies, space and overhead). Although costs for FCU are somewhat higher ($480 per year in nonresearch implementations, Ridenour et al., Reference Ridenour, Murray, Hinde, Glasheen, Wilkinson, Rackers and Coyne-Beasley2021) based on the need to use interventionists with graduate-level clinical training, because of FCU’s relative brevity (i.e., average of 3–4 sessions per year), costs are still much lower than other home-based programs. Cost considerations strongly support VIP’s and FCU’s feasibility for universal and selective implementation among low-income families within pediatric primary care.
Potential for enhanced parental engagement through medical home models
Pediatrics has led the transition to a “Patient Centered Medical Home” (PCMH) model and team-based care (Asarnow et al., Reference Asarnow, Kolko, Miranda and Kazak2017; Doyle et al., Reference Doyle, Chavez, Cohen and Morrison2019; Kazak et al., Reference Kazak, Nash, Hiroto and Kaslow2017). PCMH is a multidisciplinary team approach in which psychosocial factors related to health and prevention are prioritized, accessibility, coordination and effective communication are emphasized, relationships are actively built with parents, and patient involvement in therapeutic plans is encouraged (American Academy of Pediatrics, 2021). Resulting enhancements in engagement have been shown to improve attendance and medical outcomes (Ashby et al., Reference Ashby, Ehmer and Scott2019; Dudek et al., Reference Dudek, Henschen, Finkle, Vyas, Fiszbein and Shukla2018; Justvig et al., Reference Justvig, Li, Caravella, Chen, Wang, Benz Scott and Pati2017; Limbers et al., Reference Limbers, Gutierrez and Adelyn Cohen2020).
Opportunity to build on already-existing preventive interventions and related infrastructure
More than thirty years of pediatric initiatives to enhance school readiness in low-income families have resulted in both infrastructure and stakeholder buy-in that can support layering of models such as SB. Reach Out and Read (ROR), the longest-running such program, is well-aligned with the principles described above. Specifically, ROR promotes early relational health and school readiness through provision of children’s books and guidance for parents at each pediatric health care visit. ROR’s model has been shown to have clinically important impacts on both reading aloud and on child development (Klass et al., Reference Klass, Needleman and Zuckerman1999; Mendelsohn et al., Reference Mendelsohn, Mogilner, Dreyer, Forman, Weinstein, Broderick, Cheng, Magloire, Moore and Napier2001; Needlman et al., Reference Needlman, Toker, Dreyer, Klass and Mendelsohn2005; Perlman et al., Reference Perlman, Cowan, Gewirtz, Haskett and Stokes2012; Zuckerman, Reference Zuckerman2009), and VIP was originally developed as an enhancement to ROR. ROR has been widely scaled, with 6,100 sites across the US serving 4,500,000 young children per year, representing approximately one quarter of birth to 5-year-old children living in low-income households (Reach Out and Read National Center, 2021). Most importantly for SB and other models with similar objectives, ROR has developed both central (ROR National Center) and regional infrastructure (35 regional and statewide affiliates) for delivery and training (33,000 providers/medical champions trained to date). This infrastructure has tremendous potential to support layering complementary preventive interventions such as SB to further enhance impacts in pediatric primary care in clinical sites where buy-in has already been established (High et al., Reference High, LaGasse, Becker, Ahlgren and Gardner2000; Reach Out and Read National Center, 2021).
By capitalizing on the accessibility of pediatric primary care, VIP interventionists have been quite successful in initially engaging families and maintaining engagement in VIP during children’s first year. Of six possible VIP visits in the first year that coincide with child well checkup visits, more than three-fourths of families attended five or six sessions, with less than 3% of families not having any VIP visits in this period. In addition, and consistent with the premise that VIP might be able to engage higher risk families within the context of pediatric primary care, participation in SB has been highest among mothers with lower levels of education and lower reported parenting self-efficacy – those who have been hardest to reach in the context of preventive interventions (Miller et al., Reference Miller, Canfield, Morris, Shaw, Cates and Mendelsohn2020).
The Smart Beginnings tiered approach
As displayed in Figures 2 and 3, we address challenges (and opportunities) of heterogeneity in risk within and across time that are implied through models of equifinality and multifinality through the tiered integration of healthcare based primary prevention with home-based secondary/tertiary prevention. VIP, the primary prevention program, utilizes pediatric well-child visits to build a relationship with a Bachelors’ level interventionist who facilitates self-reflection regarding interactions with the child through review of video-recordings of the parent and child made that day, and further facilitates interactions through provision of learning materials (toys and books) (Shaw et al., Reference Shaw, Mendelsohn and Morris2021). VIP’s focus throughout is on reinforcing positive parenting and strengths within the interaction. In the SB approach, VIP is offered universally at clinical practices serving low-income families regardless of their parenting assets and vulnerabilities, based on considerations related to equity, engagement (i.e., by not stigmatizing families at greatest need), and buy-in from the policy community and the public. This approach is aligned with the approach taken by ROR and AAP recommendations (Garner & Yogman, Reference Garner and Yogman2021).
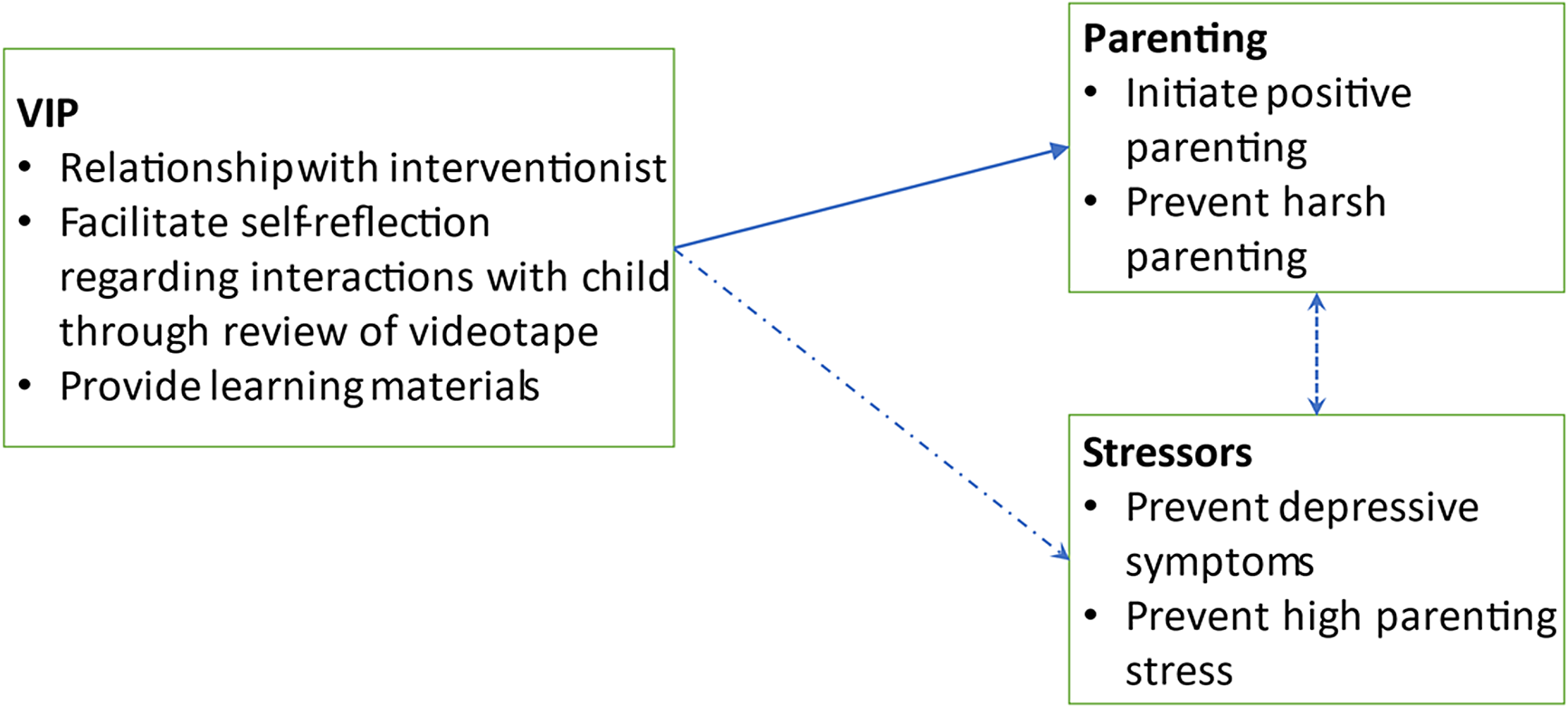
Figure 2. Video interaction project (VIP) model for primary prevention in medical home prior to onset of child problem behavior.
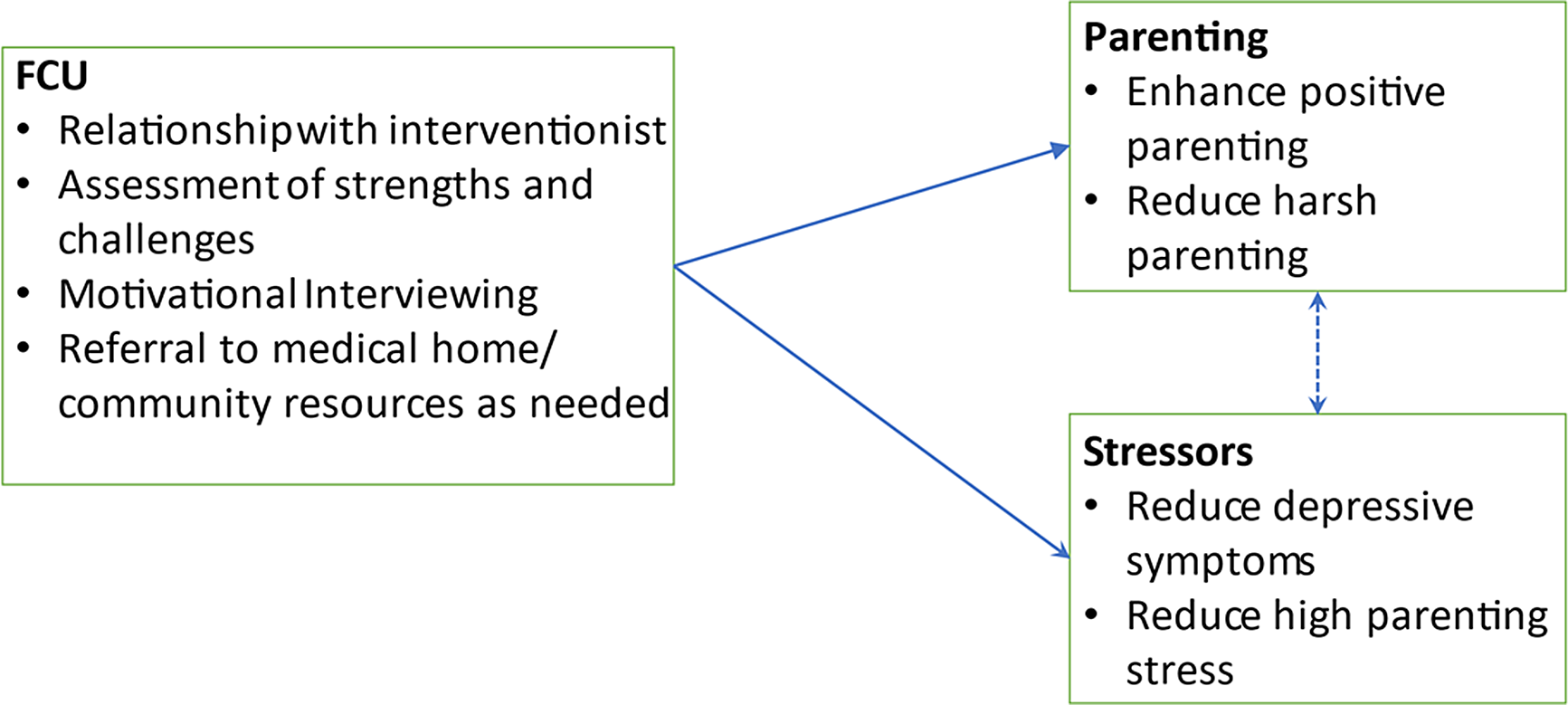
Figure 3. Family Check-Up (FCU) model for selective prevention of emerging child problems identified in VIP/medical home.
FCU (Figure 3), the secondary prevention program, utilizes home visiting to build a relationship with a clinical-level interventionist (Master’s level) who assesses family strengths and challenges and incorporates motivational interviewing and evidence-based family management strategies to support parent and child behavioral change. As with VIP, FCU’s impacts are primarily through the promotion of positive parenting and early relational health rather than the reduction of negative parenting. However, as FCU provides additional impact across a broad range of poverty-associated, and contextually derived psychosocial stressors (e.g., depression, social support, family conflict), intervention effects on emerging problem behavior and school readiness outcomes have been shown to be mediated by improvements in these stressors more broadly in addition to improved early relational health. Relatedly, targeting parent-child relationship challenges identified during the assessment process has been shown to improve satisfaction of parent social support. In the integrated model (“VIP/FCU”), VIP is provided universally for all low-income families with infants/toddlers to prevent the onset of problems by improving early parenting skills, while FCU is selectively provided to the subset of families with additional or emergent problems related to the family (parental depression, stress), the dyad (quality of parent-child interaction), and the child (language, self-regulation).
Notably, the SB framework aligns directly with AAP policy (Garner & Yogman, Reference Garner and Yogman2021), which defines primary prevention in this domain as promotion of safe, stable, nurturing relationships (SSNRs), highlighting promotion of positive parenting and including VIP as a practice-level example. In that same policy, the AAP defines secondary prevention as universal screening and addressing of barriers to SSNRs, which are core components of FCU, and further recommends working across sectors, directly aligned with SB and current initiatives for large scale implementation (i.e., see description of The Pittsburgh Study, provided below). Together, the tiered approach accounts for the principles of equifinality and multifinality by tailoring intervention to families’ specific relational health and other contextual challenges.
Alignment of Video Interaction Project and Family Check-Up within the Smart Beginnings model
In addition to VIP and FCU being complementary in their level of prevention (primary vs. secondary/tertiary as above), the two programs are well-aligned from programmatic, implementation, and cost perspectives. The programs’ ability to be complementary is critical because one of the potential challenges of an intervention espousing to the equifinality/mulitfinality framwork is its potential complexity. Indeed, as we describe below, the alignment of the two programs strengthens parent engagement across both components:
From a programmatic perspective: (1) both use videorecording with feedback as a core strategy, (2) both bring a focus on positive parenting and strengths in early relational health, (3) both consider and support interactions in the context of SDoH (informally for VIP, comprehensively for FCU), and (4) intentionally, neither has a set curriculum but instead builds on parent goals and needs, enhancing engagement, and allowing for tailoring of intervention to heterogeneity of assets and needs to meet the needs of individual families in the context of poverty. These last three components are especially important as they allow SB to align with family and cultural beliefs and values, as well as help buffer impacts of systemic racism on family functioning. VIP and FCU’s shared primary focus on early relational health (regardless of SDoH, and in the case of FCU as an opportunity to address SDoH) is relatively unique, complementing several programs with a core focus on identification and addressing SDoH (e.g., Family Connects, Help Me Grow, Healthy Steps).
From an implementation perspective: (1) both can be delivered at any time to any family without requiring that the family participate in a specific sequence of content delivery, thus facilitating participation, and (2) both work with families in the settings where they are most accessible, reducing programmatic burden, with VIP engaging families during already-attended well-child visits with trusted providers, and FCU engaging families in their homes or other locations convenient for the family (e.g., primary care, family support center, WIC, library). In addition, both models have a strong focus on fostering cultural competence in professional interactions, which may be an important factor in accounting for high levels of engagement across diverse populations (Canfield et al., Reference Canfield, Miller, Roby, Aviles, Hunter, Mendelsohn, Morris and Shaw2023c; Miller et al., Reference Miller, Canfield, Morris, Shaw, Cates and Mendelsohn2020). Furthermore, within the context of the pandemic, both VIP and FCU have been adapted for remote use with families.
From a cost perspective: (1) each individual component (VIP and FCU) is at the lower end among programs that provide 1:1 services to support self-efficacy, skills and motivation for behavior change, supporting scaling, and (2) population-level costs of the integrated SB model are also low because of the utilization of lower cost Bachelor’s level coaches providing universal prevention through VIP, while reserving higher cost clinical-level staff in FCU for families with additional risks and challenges.
Potential for additive and synergistic effects of integrating VIP and FCU
In addition to better tailoring interventions to the heterogeneous challenges facing low-income families with infants and toddlers, the Smart Beginnings tiered model also offers the potential for providing additive and synergistic effects by integrating the use of VIP and FCU, in effect demonstrating the power of tiered and fully integrated prevention/intervention approaches. Whereas all families are offered VIP, only select families are offered FCU based on the results of screening criteria. In the Smart Beginnings RCT described below, a screen was generated from select measures administered at the 6- and 18-month follow-up assessments, including parent (e.g., depression), parenting (low involvement), and child (e.g., high negative emotionality) risk domains. More specifically, credibility of the FCU parent coach is enhanced by a warm handoff from the VIP provider, including having the VIP provider introduce the parent to the FCU parent coach. Contact between VIP and FCU providers also ensures consistency and continuity in treatment, as VIP interventionists can inform FCU interventionists about the focus of their work. Continued communication and collaboration between the FCU and VIP interventionists also may be especially important in cases where the parent has engaged in FCU follow-up treatment sessions. Accordingly, the FCU interventionist can inform the VIP provider about the focus of these sessions and help reinforce parenting skills during VIP sessions.
Highly relevant from a policy perspective, the opportunity provided for coordination together with the complementarity between the two models has enhanced program engagement. This positive collateral effect is particularly important based on the potential for overwhelming parents with multiple providers and interventions, with emerging findings suggesting beneficial effects resulting from the integration. Program-specific engagement in both VIP and FCU within the SB integrated model is comparable or better than that for previous trials of each program individually during the infant and/or toddler periods. In addition to higher levels of engagement for VIP than in prior trials (described above, Miller et al., Reference Miller, Canfield, Roby, Wippick, Shaw, Mendelsohn and Morris-Perezin press), and engagement in FCU within SB has been comparable to prior studies of FCU alone despite the risk of increased burden for parents because of receiving VIP before FCU, with 65% overall (68% in Pittsburgh, 62% in NYC) of families being offered FCU engaging in the intervention at 6 and/or 18 months, meeting FCU’s threshold of attending at the initial interview and feedback sessions (Dishion et al., Reference Dishion, Shaw, Connell, Gardner, Weaver and Wilson2008). Most importantly, data suggest that those intervention families offered FCU after VIP are more likely to engage in FCU when attending initial VIP sessions. In turn, those families engaging in FCU are more likely to continue their participation in future VIP sessions than those FCU-eligible families that do not engage in FCU (Canfield et al., Reference Canfield, Miller, Zhang, Shaw, Morris, Galan and Mendelsohn2023a).
Impacts from the Smart Beginnings randomized controlled trial
Since 2014, we have been testing the integrated SB model in pediatric primary care in an NICHD-funded (R01HD076390) randomized controlled trial (half randomized to the integrated Smart Beginnings model, half to usual care) including 403 low-income families living in two cities, New York City and Pittsburgh, PA. Critically, testing our approach in these two cities positions Smart Beginnings well for dissemination– optimally balancing a strong test of efficacy while supporting next-stage effectiveness. As one of the greatest challenges of going from efficacy to effectiveness is diffusion of implementation quality and dilution of effect sizes (Dearing, Reference Dearing2008; Ghate, Reference Ghate2016), the current design allows us to maintain some initial control over quality by implementing one component of the intervention model under the direction of the PI who originally tested the model (VIP, under the direction of PI Mendelsohn in New York; FCU under the direction of PI Shaw in Pittsburgh), and allows for the testing of the other component of the model (FCU in New York; VIP in Pittsburgh) at a remote location. Moreover, the Smart Beginnings Project has allowed us to examine the integration of VIP and FCU in two different pediatric primary care clinics with different populations served. Although the samples are similar in terms of having few economic resources, they vary considerably in terms of ethnicity/race (i.e., in NYC sample is 84% Latinx, in Pittsburgh sample is 81% Black/African American) and family structure (i.e., at NYC 81% of parents were married or cohabitating vs. 40% in Pittsburgh). Such diversity in clinics’ previous use of the interventions and family background characteristics has allowed us to look at similarities and potential differences in rates of engagement in VIP and FCU and in impacts of the combined intervention across settings.
Follow-up assessments have been conducted on the NYC and Pittsburgh samples at child ages 6, 18, 24, and 48 months, with age 6 assessments ongoing. As expected from prior independent trials of VIP and to a lesser extent, FCU (Brennan et al., Reference Brennan, Shelleby, Shaw, Dishion, Gardner and Wilson2013), intention-to-treat analyses have revealed important impacts on reading quality (ES = .38, p < .001) and quantity (ES = .23, p < .05), verbal play activities (ES = .25, p < .05), and teaching activities (ES = .35, p < .001) as measured via parent survey (StimQ), including a total StimQ measure (ES = .31, p < .01) at 24 months. These findings have been corroborated based on observations of parenting (assessed via videotaped, coded parent-child interactions), demonstrating statistically reliable impacts on parent support for children’s cognitive development (ES = .29, p < .05) and parent language quality (ES = .28, p < .05), together with a global observed measure of parental cognitive stimulation (ES = .27, p < .05). Longitudinal findings from 6 through 24 months show similar sustained results on survey and observational measures (Miller et al., Reference Miller, Coskun, Roby, Zhang, Rosas, Shaw, Mendelsohn and Morris2023). At 48 months, we continue to find sustained statistically reliable impacts on key subscales of cognitive stimulation (verbal everyday interactions [ES = .11, p < .05]), verbal play activities (ES = .11, p < .05), literacy teaching activities (ES = .12, p < .05). Notably, there are very few differences in impacts across the two NYC and Pittsburgh sites, suggesting the model works well with two very different groups of families in two different locations.
In terms of findings that address the utility of deploying a tiered model, we are also beginning to see some emerging trends in relation to impacts on child problem behavior and academic achievement that mirror the benefits shown by the Smart Beginnings program’s positive effects on attendance for the other program (Canfield et al., Reference Canfield, Miller, Zhang, Shaw, Morris, Galan and Mendelsohn2023a). Consistent with the conceptual premise of both programs, with VIP showing more pronounced intervention effects on parenting activities typically associated with cognitive and academic outcomes and FCU previously demonstrating more reliable effects on multiple forms of child socioemotional outcomes, we find indirect effects of Smart Beginnings on children’s outcomes through parenting. Following up on the intervention effects found for maternal cognitive stimulation, we find significant indirect effects on child early language (ES = .05, p < .05) and literacy (ES = .03, p = .05) at 48 months that were mediated by intervention effects on maternal cognitive stimulation in toddlerhood (Miller et al., Reference Miller, Coskun, Roby, Zhang, Rosas, Shaw, Mendelsohn and Morris2023 [under review]). Note this effect was found across levels of risk, as all families in the intervention group were offered VIP. Turning to early problem behavior, we found intervention effects on child internalizing symptoms at 18 months but only for children whose mothers scored above a cutoff for depression that made them eligible to receive FCU in addition to VIP (Canfield et al., Reference Canfield, Miller, Taraban, Rosas, Morris-Perez and Mendelsohn2023b). These results suggest that the tiered Smart Beginnings model provided appropriate services to families across levels of risk. In addition, the Smart Beginnings intervention was linked to a reduction in child externalizing behaviors at 48 months that was mediated through impacts of SB on negative demeanor of discipline (ES = −.06, p < .05). Importantly, this indirect effect was more pronounced for families eligible for FCU based on the presence of contextual and/or child risk (Canfield et al., Reference Canfield, Miller, Roby, Aviles, Hunter, Mendelsohn, Morris and Shaw2023c).
Next-stage implementation of a tiered model: The Pittsburgh Study
Although there are many merits of offering VIP and FCU as a tiered model within pediatric primary care, to more comprehensively account for equifinality and multifinality in preventing children’s early emerging problem behavior and promoting school readiness, scaling the tiered model to a broader set of platforms is important for meeting population-level goals. Indeed, this work is occurring in the context of Early Childhood Collaborative (ECC) of The Pittsburgh Study (TPS). The ECC-TPS is designed to meet the needs of a wider range of families, some of whom may require less or more intensive intervention and/or may not find program delivery to be optimally accessible or desirable delivered in-person in pediatric primary care or in-person at their home. The ECC-TPS is a population-level implementation of programs with different levels of prevention and intensity, offered across multiple levels of care from multiple platforms to address the challenges implicit in the principles of equifinality and multifinality, as well as the heterogeneity of risk among families. The primary goal of the ECC-TPS is to address established barriers that have limited prior implementation trials at the individual and population level by: (1) identifying and engaging vulnerable families; (2) scaling up at low cost utilizing existing service systems; (3) tailoring interventions to address the heterogeneity of risk among families, especially low-income families from minoritized backgrounds that experience a disproportionately high level of individual, family, and community adversity/risk (e.g., parent mental health, housing insecurity, involvement with child welfare, structural and/or individual discrimination); and (4) making programs accessible by offering them at locations families with young children already frequent (Weaver Krug et al., Reference Weaver Krug, Mendelsohn, Wuerth, Roby and Shaw2023). Following the metaphor introduced in the film, “Fields of Dreams,” “if you build it, they will come,” we are testing whether parents of young children, especially those facing multiple vulnerabilities, will demonstrate increased interest and participation in parenting support programs if we can tailor programs to their specific challenges and strengths, and maximize the program’s convenience for families. In essence, can we get a head start in preventing multiple pathways leading to psychopathology (i.e., equifinality) and promoting the potential divergent pathways of initial risk (i.e., multifinality) by maximizing family’s willingness to engage in early parenting programs. Thus, interventions in the ECC-TPS are intentionally varied in both intensity and platform and are offered at locations commonly frequented by low-income families with young children, including family’s residences, pediatric primary care and Federally Qualified Health Centers (FQHCs), Nutritional Supplement Centers for Women and Children (WIC), family support and early learning centers, and libraries. Consistent with the advent of telehealth technology following the onset of the pandemic, all programs are also offered virtually. If this approach is effective, improvements at the population level should be detectable in children’s school readiness (and eventually reading scores in middle childhood) and rates of child maltreatment. If ECC-TPS is successful in improving rates of engagement and demonstrating impact on children’s cognitive and social outcomes, findings could then inform social policy to making evidence-based interventions more accessible within counties in the US.
Initial findings from the first one-thousand participants
To date over 1,000 families with children from birth through 4 years have been enrolled in-person or remotely at health care and other community settings described above, with families receiving a comprehensive screening assessment every 6 months from 0 to 3 years and then annually through age 4. Following each screening, families are offered two or more preventive programs based on identified strengths and challenges. Following the successful engagement of families in the Smart Beginnings program, for the majority of low-income families, the core primary prevention program is VIP and the core secondary prevention program is FCU, with more intensive programs (e.g., Healthy Families America, VIP and FCU together – Smart Beginnings) and less-intensive (i.e., interactive and noninteractive texting programs including Text4Baby and Nurture Program) options also offered.
As shown in Figure 4, following completion of informed consent, parents complete a 20-30-minute screening assessment (i.e., following birth the time is closer to 20 minutes but increases to near 30 minutes for 2- and 3-year-olds with more items related to child behavior) for which parents are compensated $30 for their time. Screenings are completed on a Ipad tablet while waiting for a visit or when parents have free time, minimizing burden for staff at healthcare and other agencies where enrollment occurs. Intervention modalities vary by the design of the intervention, with less intensive ones always delivered online, and others delivered in-person at healthcare sites or families’ residencies, with the latter often provided via telehealth. As the ECC-TPS began recruitment in March of 2020 during the onset of the pandemic in the US, recruitment was initially conducted remotely and has gradually moved to both in-person and remote recruiting based on context (i.e., in hospitals and pediatric care now primarily in-person vs. remotely at WIC sites). There has been an effort to recruit two parents, termed Parent Ones (P1) and Parent Twos (P2), with P1 required to have legal custody and serve as the primary caregiver of a child under 4 years old to be eligible. Additional siblings of P1s are eligible to be enrolled if they are under 4 years of age. Using data from the first 1,045 target children, 96.6% of the recruited 878 P1s are target children’s biological mothers, with 52.2% being white and 53.7% having a family income of less than $30,000. 88.2% of the 190 P2s are children’s biological fathers with 64.2% of those P2s being white and 58.8% of those families earning less than $30,000 (Weaver Krug et al., Reference Weaver Krug, Mendelsohn, Wuerth, Roby and Shaw2023).

Figure 4. The Pittsburgh study’s tiered approach to providing supporting parenting options.
Screening assessments were scored in real time as surveys were completed, allowing to communicate to parents their menu of program options immediately following completion of their assessment. Families were assigned to one of the following four groups based on levels of resources and challenges (Weaver Krug et al., Reference Weaver Krug, Mendelsohn, Wuerth, Roby and Shaw2023). Participants were assigned to Group 1 if they endorsed no risk factors, indicating higher income status and few measured challenges. Participants were assigned to Group 2 based on an annual family income of less than $30,000 and/or endorsed only lower-risk challenges (e.g., teen parent, low frequency of reading to their child, Group 2). Participants were assigned to Group 3 if they reported moderate risk factors, such as clinically meaningful levels of depressive or anxiety symptoms but not more serious risk factors. Finally, participants were assigned to Group 4 if they reported more serious risk factors such as history of incarceration, opioid use, recent homelessness, and/or prior involvement with child welfare. The percentage of families that were assigned to the four groups based on P1’s baseline assessment ranged from 22.3% for Group 1 to 30.0% for Group 3. For Group 2, the most frequently endorsed risk factor was income below $30,000 and for Group 3, clinically elevated depressive symptoms. For the most challenged and less resourced group, Group 4, the most frequently endorsed risk factor was involvement with child welfare for P1s and a history of incarceration for P2s (Weaver Krug et al., Reference Weaver Krug, Mendelsohn, Wuerth, Roby and Shaw2023).
If you build it, he/she/they will come
To test our “Fields of Dreams” proposition, we were interested in the percentage of parents that selected at least one parenting program at baseline and then over time. We also were interested to see whether there were differences in the percentage of parents selecting parenting programs based on the family’s risk group status. Most research suggests that those with lower levels of challenges and higher levels of support are more open to engaging in preventive parenting programs (Haggerty et al., Reference Haggerty, MacKenzie, Skinner, Harachi and Catalano2006; Winslow et al., Reference Winslow, Bonds, Wolchik, Sandler and Braver2009), with notable exceptions when programs are modified to make more programs more accessible (e.g., using telehealth and/or media vs. in-person meetings) or directly addressing contextual factors that compromise parenting during early childhood (Baggett et al., Reference Baggett, Davis, Fell, Sheeber, Sandry, Leve and Johnson2017; Baydar et al., Reference Baydar, Reid and Webster-Stratonn2003). In the ECC-TPS among P1s, 78.0% chose to participate in at least one parenting program at baseline, with this level of engagement cumulatively increasing to 82.7% following their 6- and 12-month follow-up assessments. At baseline, those P1s in the moderate risk/low resource Group 3 were significantly more likely to select a program than parents in low risk/high resource Group 2 (81.4% vs. 72.8%; χ 2 (3) = 23.54, p < .001). Also consistent with the notion that those with greater challenges and fewer resources would be more motivated parents to engage in parenting support, those in the highest risk Group 4 were more likely to choose a program than those in the lower risk Groups 1 and 2 (83% vs. 74.1% and 72.8%, respectively; χ 2 (3) = 23.54, p < .001). Relatedly, as Groups 3 and 4 included a majority of P1s with mental health concerns, it is noteworthy that those with clinically elevated levels of depression included in Groups 3 or 4 had a selection rate of 81% at baseline. This percentage increased to having over 88% select at least one parenting program at annual follow-up screens.
Implications of Smart Beginnings and The Pittsburgh Study’s Early Childhood Collaborative: the broader context and possible future of early child development preventive initiatives in the context of principles of equifinality and multifinality
Guided by extensions of the principles of equifinality and multifinality, in this paper we described the potential afforded by tiered programs in early childhood to prevent early emerging psychopathology and promote school readiness, especially for those living in the context of poverty. Historically, some holistically oriented prevention programs initiated during the prenatal period or infancy have attempted to address many facets of the stressors associated with poverty, including parenting (e.g., Family Connects, Nurse Family Partnership, Healthy Families America, Early Head Start, Family Spirit, Child First; Morris et al., Reference Morris, Bierman, Harding and Gennetian2015); National Academies of Sciences, Engineering, & Medicine, Reference Breiner, Ford and Gadsden2016). However, scalability remains a major challenge for such programs to have impact at the population level (Shaw et al., Reference Shaw, Mendelsohn and Morris2021). Moreover, as these individual programs are a one size fits all approach, they are inherently limited in meeting the heterogeneity of needs facing families with young children living in poverty. We argue that taking equifinality and multifinality seriously necessitates a tiered approach to prevention.
The long-standing concepts of equifinality and multifinality applied to developmental psychopathology by Cicchetti and his colleagues three decades ago changed the way in which we understand the etiology and developmental sequelae of early developmental risk and its implications for child psychopathology. Yet, despite the wide-ranging implications of this seminal work for our understanding of developmental pathways associated with risk and protection, preventive interventions have not fully integrated these perspectives into their design. We see Smart Beginnings and ECC-TPS as not only an efficient way to support the mental health and school readiness of children from low-income families at the population level, but as exemplars of the ways in which concepts of equifinality and multifinality could transform the ways in which we address disparities of children living in poverty in the decades to come.
Funding statement
This work was supported by the Eunice Kennedy Shriver National Institute of Child Health & Human Development of the National Institutes of Health under Award Number R01HD076390.
Competing interests
None.







