The global burden of micronutrient malnutrition
Micronutrient deficiencies affect about one-third of the world's population(Reference Muthayya, Rah and Sugimoto1,Reference Bailey, West and Black2 ). In many parts of Africa, the burden of disability-adjusted life-years attributable to deficiencies of iron, zinc and vitamin A exceeds 5000 per 100 000 population(Reference Muthayya, Rah and Sugimoto1). Micronutrient deficiencies may persist despite economic growth, as in South Asia(Reference Harding, Aguayo and Webb3). Deficiencies in sub-Saharan Africa are widespread(Reference Kihara, Bolo and Kinyua4). The purpose of this review is to set out the reasons why micronutrient deficiencies may have become so widespread, and to explore the contribution of environmental enteropathy (EE) to these deficiencies.
Why might an individual develop a micronutrient deficiency?
Geography and geochemistry
For wealthier people, food may be purchased from outside their region of residence but for poor people the majority of their diet comprises foods grown very locally. There are two important micronutrients, iodine and selenium, for which good evidence exists that human nutritional status depends to a large degree on where you live and the soil on which your crops grow. Iodine deficiency, which causes thyroid disease(Reference Zimmermann and Boelaert5), is well known to be common where soils and foods have low iodine content, such as in mountainous and landlocked areas(Reference Kelly and Snedden6). Selenium seems to be similar, with clear evidence of a relationship between soil selenium and human selenium status in Malawi(Reference Hurst, Siyame and Young7). However, in Kenya the relationship between soil selenium and crop selenium content was more complex and was also dependent on pH, organic matter and the presence of other inorganic chemicals(Reference Ngigi, Du Laing and Masinde8).
Food processing and anti-nutrients
In addition to deficiencies in soils and therefore crops, anti-nutrients and toxic compounds may also be present(Reference Frazzoli and Mantovani9). Examples include thyroid disrupting pollutants which exacerbate functional iodine deficiency, and fumonisins and arsenic which antagonise physiological effects of folate(Reference Frazzoli and Mantovani9). Fumonisins are fungal toxins which contaminate crops during harvesting and storage. The best-known anti-nutrient is phytate, which reduces bioavailability of iron and zinc(Reference Gibson, Raboy and King10). Anti-thiamin compounds are another example(Reference Titcomb and Tanumihardjo11). A striking example of the impact of food processing on micronutrient content of foods is the relationship between the type of maize milling and losses of zinc(Reference Chomba, Westcott and Westcott12). Processing of rice also impacts nutrient composition(Reference Atungulu and Pan13). Detailed discussion is beyond the scope of this review, but there is also evidence that appropriate food processing can enhance micronutrient availability(Reference Platel and Srinivasan14).
Clinical gastrointestinal disease
Individuals with clinical gastrointestinal disease, especially oesophageal disease, can lose weight very rapidly and develop severe wasting in a few weeks and such patients will have micronutrient deficiencies commensurate with their weight loss. Patients with anorexia nervosa also have micronutrient deficiencies. More subtly, patients who have had gastrointestinal surgery are at heightened risk of deficiencies. Gastrectomy is followed by iron and vitamin B12 deficiency(Reference Jun, Yoo and Lee15); ileal resection can be followed by vitamin B12 deficiency; jejunoileal bypass has been reported as leading to deficiencies of vitamins A, D, K, zinc, selenium and copper(Reference Joshi, McLarney and Abramoff16,Reference Haria, Sibonga and Taylor17) and multiple deficiencies have been reported both before and after bariatric surgery(Reference Bal, Finelli and Shope18). As the number of people undergoing surgery for obesity increases, this will become a significant clinical burden, but none of these disorders make a significant contribution to the scale of the problem outlined earlier.
Dietary diversity and poverty
Both food insecurity and limited dietary diversity, largely related to poverty, make a much greater contribution to the global burden of micronutrient deficiency than the clinical disorders described earlier. Even in populations with a double burden of malnutrition, including poor ones, micronutrient deficiencies can be prevalent(Reference Wells, Sawaya and Wibaek19). A lack of dietary diversity has been identified as a driver of micronutrient deficiency in Sri Lanka(Reference Weerasekara, Withanachchi and Ginigaddara20), but dietary diversity is a remediable problem, as recently demonstrated in Malawi(Reference Kansanga, Kangmennaang and Bezner Kerr21). The problem of dietary diversity in poor populations is a large subject, beyond the scope of this paper, but major initiatives are being implemented to attempt to improve micronutrient status around the world through drives to increase dietary diversity(Reference Thompson and Amoroso22). Poverty also predisposes to EE, to which we now turn.
Environmental enteropathy: what is it?
History
Studies of diarrhoea and malabsorption in the tropics in the early 1960s used apparently asymptomatic, healthy and well-nourished adults and children from the same population as control subjects. Unexpectedly, they identified a high prevalence of abnormal intestinal permeability (as measured by urinary sugar recovery) and/or histological abnormalities (villous blunting; crypt hypertrophy; villous fusion and mucosal inflammation) in these controls(Reference Louis-Auguste and Kelly23). Studies in American soldiers and Peace Corps volunteers stationed in Thailand and in Peace Corps volunteers in Bangladesh showed that the condition was acquired, and that these abnormalities were similar to those observed in the indigenous population(Reference Louis-Auguste and Kelly23). Furthermore, histological examination of fetal and neonatal intestine also showed that these abnormalities were not present during development, and only became apparent post-natally(Reference Baker24,Reference Walker-Smith25) .
These changes were reversible, as demonstrated by prospective assessment of small bowel histology and absorption. Peace Corps volunteers who had lived in India or Pakistan returned to histological and absorptive normality, usually within 2 years after returning to the United States(Reference Lindenbaum, Gerson and Kent26). Furthermore, adult students from endemic areas moving to the United States to study also normalised intestinal structure and function(Reference Gerson, Kent and Saha27), and in the UK it was noted that there was a relationship between villus morphology and the time from last visit to the tropics(Reference Wood, Gearty and Cooper28). Based on the initial studies which were exclusively conducted in the tropics, the condition was labelled tropical enteropathy(Reference Cook29).
The adoption of environmental enteropathy
However, an extensive global study of intestinal function using lactulose permeation and sugar absorption demonstrated that the observed abnormalities were not observed in some affluent, tropical populations (such as Singapore and Qatar)(Reference Menzies, Zuckerman and Nukajam30), and the condition is therefore more correctly termed EE. Brunser et al., working in Santiago which is not tropical, noted the same enteropathy in children living in insanitary slums(Reference Brunser, Araya and Espinoza31). Numerous subsequent studies have confirmed that EE is highly prevalent throughout the developing world irrespective of climate, and it is seasonal(Reference Kelly, Menzies and Crane32). The increased intestinal permeability to small sugars as measured by sugar absorption assays is correlated with significant and pathological abnormalities of intestinal barrier function, for example as measured by plasma lipopolysaccharide levels(Reference Lunn, Northrop-Clewes and Downes33,Reference Campbell, Elia and Lunn34) . More recently, the term ‘environmental enteric dysfunction’ has been used to emphasise the functional consequences of the enteropathy for child health, as it appears to be a major contributor to stunting(Reference Keusch, Denno and Black35–Reference Prendergast and Humphrey38). There is some evidence that EE may also contribute to the well-established impairment of responses to oral vaccines seen in many tropical and disadvantaged populations(Reference Marie, Ali and Chandwe39,Reference Church, Parker and Kosek40) .
Aetiology of environmental enteropathy
There is increasing evidence that EE is characterised by polymicrobial infection with a wide range of enteropathogens. The eight-country Mal-ED study revealed that asymptomatic infection is a major contributor to EE and to adverse growth outcomes in children(Reference Kosek41). This study recognised the impact of enteroaggregative Escherichia coli (Reference Rogawski, Guerrant and Havt42), and identified that Campylobacter infections make a major contribution to EE(Reference Amour, Gratz and Mduma43). Major impacts of Shigella, Giardia, norovirus, enteropathogenic E. coli, Cryptosporidium, and Enterocytozoon bieneusi were revealed by the quantitative measurement of pathogen burden(Reference Rogawski, Liu and Platts-Mills44). These effects probably interact with nutritional deficiencies, including those of micronutrients, in complex ways.
Given the apparent key role of enteropathogens, which are largely transmitted faeco-orally, in the genesis of EE, the failure of three large recent water and sanitation trials to solve the problem of stunting(Reference Null, Stewart and Pickering45–Reference Humphrey, Mbuya and Ntozini47) is surprising and disappointing. There is still debate as to why this is, but there are good grounds for thinking that water and sanitation interventions may need to be more transformative to achieve the desired effect(Reference Cumming, Arnold and Ban48). It would certainly be inappropriate to conclude that sanitation does not matter as there is little doubt that the sanitation transformations of the 19th century were a major contributor to massively improved public health in Europe.
The polymicrobial infections which characterise EE may reflect a general disturbance of the microbiota and the normal host–commensal relationship. Recent analysis of the duodenal microbiota in stunted children in Bangladesh identified fourteen taxa which were closely related to growth failure, and which could confer a malnutrition phenotype when adoptively transferred into gnotobiotic mice(Reference Chen, Kung and Das49). This study adds to a growing body of evidence that the microbiota can drive metabolic and other changes in the gut leading to malnutrition, playing a key role in driving, or at least perpetuating, malnutrition(Reference Stine50).
Mucosal abnormalities in environmental enteropathy
Mucosal biopsies from adults and children in disadvantaged populations show consistent villus blunting, leading to reduced absorptive surface area, and crypt hypertrophy(Reference Kelly, Menzies and Crane32,Reference Campbell, Murch and Elia51,Reference Kelly, Besa and Zyambo52) . There is also a marked lymphocytic inflammatory infiltrate in the lamina propria and the epithelium (Fig. 1). This predominantly affects the proximal small intestine; the author has never observed villus blunting in the ileum during hundreds of ileoscopies in Zambia. As the majority of micronutrients are absorbed in the proximal small intestine this may help explain how EE would affect micronutrient status. Recent, and ongoing, comparative histological analysis of intestinal biopsies from Bangladesh, Pakistan, Zambia and the United States have revealed that EE has other key features in addition to reduced surface area and inflammation. These include markedly reduced numbers of goblet cells and Paneth cells(Reference Liu, VanBuskirk and Ali53), both of which make a major contribution to barrier function by maintenance of a protective mucus layer on the epithelial surface which has antimicrobial properties. Defining the cellular and transcriptional changes in EE is currently the focus of intense research of which much will be published in the next 2–3 years. It is clear already that EE is characterised by increased gene expression of mucosal barrier function genes (mucins and NADPH oxidases(Reference Chama, Amadi and Chandwe54)) which are also transcriptional features of inflammatory bowel disease(Reference Haberman, Tickle and Dexheimer55). There is also emerging evidence of changes in solute transporters which mediate the intestinal absorption of micronutrients(Reference Amadi, Zyambo and Chandwe56). Another prominent feature of EE is the increased permeability referred to earlier, which over the past 40 years has been most extensively studied using lactulose permeation(Reference Menzies, Zuckerman and Nukajam30,Reference Lee, McCormick and Seidman57) . More recent studies have used fluorescein as a marker of the leakiness of the mucosa, either by showing leakage of fluorescein from the systemic circulation into the gut lumen during endoscopy(Reference Kelly, Besa and Zyambo52,Reference Amadi, Besa and Zyambo58) , or by showing leakage of oral fluorescein into the systemic circulation(Reference Dorshow, Hall-Moore and Shaikh59,Reference Maurice, Lett and Skinner60) . In an ingenious approach, transcriptomic analysis of shed enterocytes in stool samples identified mucin and inflammatory genes associated with EE in an entirely non-invasive way(Reference Ordiz, Wold and Kaimila61).

Fig. 1. Mucosal abnormalities in environmental enteropathy (EE). (a) Finger-like villi imaged endoscopically in the terminal ileum of a Zambian adult, which contrasts with marked villus fusion and reduced height in an adult with EE (b). (c) Histological image of duodenal biopsy showing enteropathy with inflammatory infiltrate but with preserved villus height, which contrasts with severe inflammation and loss of villus height (d). (e) Confocal laser endomicroscopy image of duodenal mucosa showing good barrier function, intact capillaries (white arrow) and no fluorescein in the intestinal lumen following systemic injection of fluorescein. (f and g) Focal leakage of fluorescein (black arrow), and a microerosion is seen where cellular integrity is lost (hollow arrow, g). (h) Gross leakage of fluorescein seen filling the gut lumen (*).
Maldigestion in environmental enteropathy
Impaired digestion could follow from achlorhydria (reduced or absent gastric acid secretion), exocrine pancreatic insufficiency or enterocyte damage leading to impaired activity of enzymes of the brush border. Achlorhydria would be expected to diminish the efficiency of protein digestion, and it is very common in Zambian adults(Reference Kelly, Shawa and Mwanamakondo62), but there have been few publications on this aspect of malnutrition. It has been proposed that impairment of the gastric acid barrier could lead to small intestinal bacterial overgrowth and contribute to malnutrition(Reference Sarker, Ahmed and Brüssow63). Pancreatic insufficiency would lead to malabsorption of lipids and lipid-soluble vitamins. Reduced expression of brush border digestive enzyme genes was apparent in Zambian adults and children (P Kelly, unpublished results) but the functional implications of these early findings for micronutrient status are not yet apparent.
Malabsorption in environmental enteropathy
The clearest evidence that EE is associated with malabsorption comes from stable isotope studies of zinc (using 68Zn and 70Zn). In Malawian children, fractional absorption of zinc was reduced and endogenous losses increased(Reference Manary, Abrams and Griffin64). For most micronutrients, direct evidence that EE causes or exacerbates the deficiency is lacking, and the only evidence of an association is their widespread prevalence (Table 1). Clearly, interpretation of geographical overlap data is problematic as inadequate intake is very common(Reference Harika, Faber and Samuel65). Stable isotopes remain the most promising way to evaluate directly the contribution of malabsorption to deficiency(Reference Davidsson and Kaskell66).
Table 1. Evidence of micronutrient deficiency in environmental enteropathy (EE)
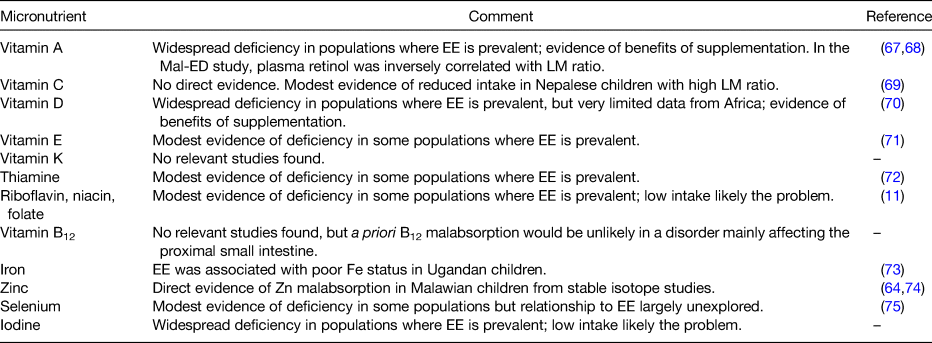
LM, lactulose:rhamnose. Summary of evidence of micronutrient malabsorption in EE. Only for zinc the evidence is direct; for vitamin A the evidence is correlational only.
Treatment of environmental enteropathy
In a trial of multiple micronutrient supplementation over 2 years in Zambian adults, plasma concentrations of folate increased over 2 years, plasma zinc showed a marginal increase, but vitamin A did not increase at all(Reference Kelly, Katubulushi and Todd76). Although not incompatible with the play of chance, or inadequate compliance, these data might suggest that malabsorption due to EE may blunt the efficacy of supplementation programmes. They do not support the idea that EE can be reversed by micronutrient supplementation. Trials of interventions to improve EE have included antibiotic therapy with rifaximin(Reference Trehan, Shulman and Ou77), albendazole(Reference Wang, Shulman and Crocker78), probiotic therapy(Reference Galpin, Manary and Fleming79), zinc(Reference Lauer, McDonald and Kisenge80) or multiple micronutrients(Reference Lauer, McDonald and Kisenge80). However, glutamine supplementation has been reported to have some efficacy in improving intestinal barrier function(Reference Lima, Anstead and Zhang81). In Zambian adults, a combination of glutamine, tryptophan and leucine led to a modest but significant increase in villus height(Reference Louis-Auguste, Besa and Zyambo82). Given this somewhat patchy and disappointing record, novel approaches are urgently required to treat the underlying causes of EE.
Solutions
If it is a valid generalisation that micronutrient malabsorption contributes to hidden hunger, there are two possible approaches to ameliorating the problem: either increase intake, or treat the enteropathy. Neither of these solutions would be easy to implement at scale. Treatment of EE would be highly desirable, as it may improve stunting and help with vaccine responses in addition to improving micronutrient status. However, those treatments which have been tried so far have been disappointing, as noted earlier. Combating the influence of the complex polymicrobial infections now known to be very common in EE will require novel approaches, either to restoring the normal balance of microbiota or to improving mucosal barrier function.
It is axiomatic that flux through a membrane transporter or enzyme system can be overcome by providing more substrate, at least up to a point of saturation, so it is likely to be possible to overcome degrees of malabsorption by increasing the concentration of micronutrients in the gut lumen. Shouldn't we just increase the reference nutrient intake of micronutrients in vulnerable populations? To match such increases in the reference nutrient intake, however, would almost certainly require biofortification(83) and/or supplementation strategies. Biofortification can be very effective, as demonstrated for iodine and thiamine(Reference Keats, Neufeld and Garrett84). Supplementation with folate, as an example, has dramatically reduced neural tube defects in many countries. More controversially, there are suggestions that increased meat consumption, especially by young children, may be an efficient way to increase micronutrient intakes(Reference Wyness85).
Conclusions
EE is a very widespread alteration in gut structure and function which predisposes disadvantaged populations to the consequences of inflammation, leakiness and reduced surface area. These include micronutrient deficiencies, through maldigestion, malabsorption, wastage of plasma constituents into the gut and possibly through inflammation-induced anorexia. The direct connections between enteropathy and malabsorption are just beginning to be explored; currently there is direct evidence only for zinc. These may require revision of fundamental assumptions about micronutrient requirements in disadvantaged populations, and in turn this is likely to necessitate major investments in micronutrient biofortification and/or supplementation. Ideally, a solution should be found to improve gut function in disadvantaged populations with the objective of improving micronutrient status globally.
Financial Support
None.
Conflict of Interest
None.
Authorship
The author takes full responsibility for the entire paper and all content.





