Introduction
The impact of hurricane-related flooding on infectious diseases in the US is not well understood. Hurricane Matthew made landfall in North Carolina in October, 2016 and caused extensive inland riverine flooding. Prior work examining hurricane impact in North Carolina suggests small but significant increases in emergency department (ED) visits for gastrointestinal illness immediately following hurricane exposure, Reference Quist, Fliss, Wade, Delamater, Richardson and Engel1 and in waterborne pathogen illness among Medicaid enrollees in the year following a hurricane, Reference Setzer and Domino2 for those living in flooded areas. Using health record data for infectious outcomes and antimicrobial prescribing, and linking patient residential address with high-resolution flood maps, we documented whether similar increases in infections and use of infection-related medications were observed among US veterans living in flood-exposed areas of eastern North Carolina following Hurricane Matthew.
Methods
Active users of the Veterans Health Administration (VHA) residing in the 45 counties declared disaster areas by FEMA following Hurricane Matthew were identified. Patients who died before the hurricane made landfall, resided in a nursing home or other care facility, or had an address that could not be geocoded to a specific location, were excluded.
Residential flood exposure based upon geocoded address was assessed using RIFT, a physics-based (shallow water equations) flood model developed by Pacific Northwest National Laboratory which used a 90-meter resolution digital elevation model data and spatiotemporally varying rainfall data. Additional patient characteristics included self-identified race, Charlson comorbidities, Reference Charlson, Szatrowski, Peterson and Gold3 and rurality, defined by Rural-Urban Commuting Area (RUCA) codes based on patient residence census tract.
Infection-related outpatient and ED visits, and antimicrobial prescriptions were assessed on a weekly basis during 2016, as well as for the 2016 cohort in the year prior to Hurricane Matthew (2015) to account for seasonal trends in infectious outcomes and antimicrobial prescribing. No major hurricanes made landfall in North Carolina during 2015. Outpatient and ED visits included both VHA visits as well as VA-funded community care. Clinical Classifications Software CCS (US Department of Health and Human Services, Washington, USA) was used to identify diagnoses for infectious diseases of multiple systems with multiple causative organisms (Supplemental Table 1). A subset of relevant antimicrobials, from the National Healthcare Safety Network’s standardized list, was identified based upon clinical expertise (Supplemental Table 2). For each year of data, flags were set to indicate a baseline period (calendar weeks 1-40), weeks 0-2 after Hurricane Matthew (weeks 41-43), and 3 or more weeks after Hurricane Matthew (weeks 44-52).
Table 1. Characteristics of the patient population

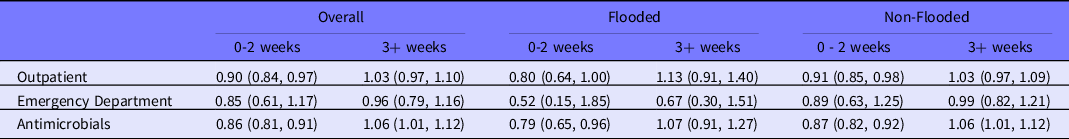
Table 2. Model results representing relative change versus baseline in Matthew year versus the same period in the year prior to the hurricane
Binomial regression models with logit link functions were used to assess changes in infection-related outcomes during weeks 0-2 and 3 or more weeks after Hurricane Matthew, relative to the baseline period. Models included an exchangeable working correlation matrix with robust standard errors to account for the multiple weeks per patient. Interactions between year and the indicators for baseline, weeks 0-2 and weeks 3+ were used to assess changes in outcomes associated with the hurricane. Models were generated separately for patients residing in flood-exposed and unexposed neighborhoods. All models adjusted for race, Charlson comorbidities, and rurality.
Statistical analysis was completed in SAS version 8.2 (SAS Institute, Cary, NC, USA), residential flood assignment was done in ArcMap version 7.1 (ESRI, Redlands, CA, USA). The study was approved by the Institutional Review Board at the University of Iowa.
Results
Of the 62762 eligible patients, 6061 (9.7%) experienced residential flooding during Hurricane Matthew (Table 1). Residential flooding did not differ by age but did differ by race, rurality, and some comorbidities.
When controlling for race, comorbidities, and rurality, significant declines in outpatient visits for infectious diseases and antimicrobial prescriptions in weeks 0-2 versus the baseline period relative to the non-Matthew years were observed in both the overall and the non-flooded cohort, and in prescriptions for the flooded cohort (Table 2). Significant increases in antimicrobial prescriptions were observed in weeks 3+ for the overall cohort and in prescribing in the non-flooded cohort. No significant changes in ED visits for infections were observed.
Discussion
These findings contradict other studies that found slightly increased ED visits for flood-related acute gastrointestinal infections in weeks 0-2 following Hurricane Matthew, for residents of highly flooded ZIP codes. Reference Quist, Fliss, Wade, Delamater, Richardson and Engel1 The current analysis used a more specific determination of flood exposure and a broader set of infections. The increase in antimicrobial prescribing observed in weeks 3+ could be due to an onset of less acute infections resulting from hurricane exposure or reflect a delay and then rebound in healthcare seeking behavior as the hurricane disrupted typical activities, as has been previously observed in VHA users. Reference Carrel, Clore and Kim4 The delayed healthcare seeking behavior is also potentially responsible for the relative decline in outpatient visits for infections in weeks 0-2 versus the baseline period. Taken together, hurricane and flood exposure appear to have had minor impacts on infectious outcomes in North Carolina veterans, not resulting in large increases in infections or antimicrobial prescribing.
Supplementary material
To view supplementary material for this article, please visit https://doi.org/10.1017/dmp.2023.9
Acknowledgements
MC, GC, and SK were supported by a Carnegie Fellowship from the Carnegie Corporation of New York. We thank Cynthia Rakowski of the Pacific Northwest National Laboratory for providing the RIFT flooding data.
Author contributions
MC, MG, ENP conceived of the study; MC, GSC, MG, SK MVS performed the analysis; all authors wrote the manuscript and approved of the final version.
Funding statement
Margaret Carrel, Gosia Clore, and Seungwon Kim received financial support for the work from the Carnegie Corporation of New York. All other authors declare they have nothing to disclose.




