Introduction
Hospice palliative care addresses not only physical symptoms but also psychosocial needs for patients with terminal illnesses and their family members. Bereavement care is one of the major components of hospice palliative care (Hudson et al., Reference Hudson, Remedios and Zordan2012). When patients and family members recognize the approach of death, they may have anticipatory grief; after a patient's death, family members might experience a grief reaction and need time to adjust to their new lives (Stroebe et al., Reference Stroebe, Hansson and Schut2008). Clinical staff provide bereavement care for patients who received hospice palliative care and extents the care to after a patient's death.
Bereavement care is a facet of psychosocial care and all clinical staff should take responsibility for bereavement care (NICE, Reference McCloskey and Taggart2013). Both physicians (Lemkau et al., Reference Lemkau, Mann and Little2000; Boyatzis et al., Reference Boyatzis, Blight and Vieira2003) and nurses (Chan and Arthur, Reference Chan and Arthur2009) agreed about the importance of bereavement care in clinical service. In a large sample survey (n = 2,583) of pediatric oncologists, 96% of participants agreed that bereavement care is part of good clinical care, and 82% sometime engaged in some type of bereavement care (phone calls, condolence cards, memorial services, family meetings, or referrals for counseling). Being female, an attending physician, and having worked longer in clinical practice were significantly related to active participation in bereavement care (Jensen et al., Reference Jensen, Weng and Spraker-Perlman2017). In a survey about perceptions of bereavement care by physicians and nurses in an acute setting in Hong Kong, 60.0% of participants reported that they wanted to take an active role in managing grief for relatives of terminally ill patients (Tse et al., Reference Tse, Wu and Suen2006).
However, caring for patients with a terminal illness and their family members caused stress (Vachon, Reference Vachon1995; McCloskey and Taggart, 2010), and clinical staff may experience emotional and behavioral reactions (Katz and Genevay, Reference Katz and Genevay2002), even leading to burnout and compassion fatigue (Keidel, Reference Keidel2002). Compared to those who did not provide psychosocial support, clinical staff who provided psychosocial support to patients and/or families had higher levels of compassion fatigue and burnout (Slocum-Gori et al., Reference Slocum-Gori, Hemsworth and Chan2013).
There were barriers for clinical staff providing bereavement care. Lack of time (Tse et al., Reference Tse, Wu and Suen2006; Jensen et al., Reference Jensen, Weng and Spraker-Perlman2017), lack of knowledge and skills (Tse et al., Reference Tse, Wu and Suen2006; McAdam and Erikson, Reference McAdam and Erikson2016; Fan et al., Reference Fan, Lin and Hsieh2017; Jensen et al., Reference Jensen, Weng and Spraker-Perlman2017), and lack of resources and professional support (Lemkau et al., Reference Lemkau, Mann and Little2000; Boyatzis et al., Reference Boyatzis, Blight and Vieira2003; Jensen et al., Reference Jensen, Weng and Spraker-Perlman2017) were the most common barriers in surveys. Lack of adequate educational training was also an important barrier (McAdam and Erikson, Reference McAdam and Erikson2016). However, the barriers came from not only the systems but also from intrapersonal factors.
Weiner and Cole (Reference Weiner and Cole2004b) provided a conceptual framework for cognitive, emotional, and skill barriers to communicating about advance care planning. Emotional barriers were adverse emotional experiences in clinical communication, such as anxiety, sadness, anger, frustration, helplessness, shame, and guilty (Weiner and Cole, Reference Weiner and Cole2004b). Cognitive barriers were maladaptive beliefs. For example, patients generally do not want to discuss end-of-life issues, discussing relevant issues might reduce patients' hope, and the physicians must always have something to say when facing patients and family members (Weiner and Cole, Reference Weiner and Cole2004a).
Regarding emotional responses, 46.3% of pediatric oncologists were emotionally drained from working with dying patients and their families; 21.4% had a feeling of failure when a patient died; and 20.0% felt anxious when speaking with family members after the patient's death (Jensen et al., Reference Jensen, Weng and Spraker-Perlman2017). Compared with medical and radiological oncologists, palliative care physicians were significantly more likely to engage in active bereavement practices and had less sense of failure or anxiety speaking to family members after a patient's death (Chau et al., Reference Chau, Zimmermann and Ma2009). Qualitative studies also revealed that clinical staff had emotional responses to bereavement care (Wenzel et al., Reference Wenzel, Shaha and Klimmek2011; Walker and Deacon, Reference Walker and Deacon2016). Staff also thought about the appropriateness of management that whether they provided the right care. They were bereaved by the death of familiar patients and needed to grieve and express emotion (Saunderson et al., Reference Saunderson, Jewell and Ridsdale1999).
Many studies surveyed the system barriers, such as lack of time and resources, or lack of professional support, but few studies explored intrapersonal factors related to cognitive and emotional barriers among physicians and nurses. For those providing bereavement care, such as physicians and nurse, it is necessary to explore attitudinal or other barriers — including general discomfort in discussing death and loss — and to develop educational training courses based on these results (Ghesquiere et al., Reference Ghesquiere, Patel and Kaplan2014). Therefore, the aims of the study were (1) to explore the emotional and cognitive barriers when hospice palliative care staff provided bereavement care to patients with a terminal illness and their family members and (2) to identify the demographic characteristics and work variables related to these emotional and cognitive barriers.
Method
Study design
First, the potential items were developed from the literature review (Weiner and Cole, Reference Weiner and Cole2004a, Reference Weiner and Cole2004b) and the clinical experiences of the research team. Second, expert validity was tested. Six experts were invited, including one physician, two nurses, two social workers, and one psychologist. One expert had a bachelor's degree, and all the others had a master's degree or above. All of them had been working in hospice palliative care units for more than 15 years. These experts rated the appropriateness of the items. Third, the questionnaire was administrated to collect data from hospice palliative care staff from April 2015 to December 2015. Before beginning the study, ethical approval was obtained from the institutional review board at Chi Mei Medical Center (IRB number: 10302-L01).
Participants
The participants were clinical staff working in hospice palliative care units, including hospice wards, home care, and hospital-based palliative care teams. The staff included physicians, nurses, social workers, psychologists, and chaplains. The participants were recruited from hospice training courses about psychosocial care, bereavement care, and family dynamic facing death, held by a National Hospice Organization. The researchers explained the aims of the study and the clinical staff who were willing to participate completed the questionnaire.
Measures
Demographic and work characteristics
Demographic characteristics included age, sex, educational level, and material status. Working experience including years in medical care and hospice palliative care, self-rated working stress in hospice palliative care (5-points: 5 = extreme stress, 1 = no stress), self-rated confidence in ability to provide bereavement care (5-points: 5 = very confident, 1 = not confident at all), self-rated inner growth from hospice palliative care work (5-points: 5 = a great deal, 1 = not at all), experienced with major loss in life (yes or no), and the negative impact of major losses and the positive impact of major losses (5-points: 5 = a great deal, 1 = not at all).
Emotional barriers for bereavement care
Thirteen items were developed based on a literature review and experts' suggestions. The items started with: “When providing bereavement care for patients and family members, I would feel ….” A five-point Likert scale was used to rate the level of impact of a certain emotional response on bereavement care (5 = very great and serious influence/impact and 1 = not at all).
Cognitive barriers for bereavement care
There were nineteen items related to cognitive belief. The participants rated the impact of certain cognitive beliefs on bereavement care using a five-point Likert scale (5 = very great and serious influence/impact and 1 = not at all).
Statistical analysis
Content validity index was calculated (Polit and Beck, Reference Polit and Beck2006), and the items were modified based on the experts' suggestions. Exploratory factor analysis (Fabrigar et al., Reference Fabrigar, Wegener and MacCallum1999) using principal axis factoring with oblique rotation was used to explore the core factors of the emotional and cognitive barriers. The items with low factor loading (<0.3) or cross-loading between two factors were deleted. The naming of the barriers was based on the meaning of the items. Cronbach's α was used to examine the internal reliability of the dimensions.
Multiple regression was used to explore the significant variables related to emotional and cognitive barriers. The predictors included age, gender, educational level, years working in medical care and hospice palliative care, working stress and inner growth, self-rated ability for bereavement care, and negative impact and positive impact of major life losses. Regarding professional categories, because there were few cases of physicians, chaplains, and others, two categories were used: medical professionals, including physicians, nurses, and other professionals; and psychosocial professionals, including social workers, psychologists, and chaplains. Kruskal Wallis test was used to test the differences in the barriers between physicians, nurses, social workers, psychologists, chaplains, and others; and t-test was used to test the differences between medical and professionals.
All statistical analyses were performed with SPSS for Windows version 21.0 (IBM Corp., Armonk, NY, USA). A 2-tailed p-value of equal to or below 0.05 was considered statistically significant.
Results
Content validity index
The CVIs of emotional and cognitive barriers were 0.92 and 0.90, respectively. Based on the experts' suggestions, some minor revisions related to rhetoric were made.
Demographic characteristics of participants
A total of 343 potential participants were recruited. Of these, 42 who did not have any working experience in hospice palliative care were excluded. Therefore, 301 participants were included in this study. The mean age of the participants was 35.63 (SD = 7.13), 279 (92.69%) were female, 143 (47.51%) were single, and 148 (49.17%) were married. More than 60% had an undergraduate degree. Regarding professional categories, 57.14% was nurses, 19.60% was social workers, and 11.30% was psychologists. The mean length of experience was 10.66 years working in medical care (SD = 6.56) and 6.16 years in hospice palliative care (SD = 4.82) (see Table 1).
Table 1. Demographic and work characteristics of the participants

Factor analysis
Regarding emotional barriers, Bartlett's test of sphericity showed that there were correlations between variables (χ 2 = 2,077.45, p < 0.001), and KMO was 0.930. Therefore, the data were suitable for factor analysis. Only one factor was extracted, and this factor was named “negative emotional reaction,” and the extraction sum of squared loadings was 48.77% and the Cronbach's α was 0.92. The five most impactful emotional barriers were helplessness, frustration, anxiety and nervousness, sadness, and loss (see Table 2).
Table 2. Factor loading and internal reliability of emotional barriers

Regarding cognitive barriers, three items were deleted due to the cross-loading between different factors. Bartlett's test of sphericity showed that there were correlations between variables (χ 2 = 2,427.04, p < 0.001), and KMO was 0.930. Therefore, the data were suitable for factor analysis. Three factors were extracted. The first factor included seven items related to bereavement care ability and was named “lack of ability.” The second factor included five items related to the assumption of patients avoidance of bereavement issues and was named “belief in avoidance.” The third factor included four items related to expectations for care outcome and was named “outcome expectancy.” The extraction sum of squared loadings was 54.20% and the Cronbach's α of the three factors and total scale were 0.85, 0.86, 0.85, and 0.92, respectively. The six most impactful cognitive barriers were work loading, personal limitations, working alone, the feeling that skills can do nothing, lack of ability, and the responsibility to improve (see Table 3).
Table 3. Factor loading and internal reliability of cognitive barriers

Demographic and work characteristics related to barriers
The results of Kruskal Wallis test showed that there was no difference between all clinical professionals in “negative emotional reactions” (χ 2 = 3.36, p = 0.645), “lack of ability” (χ 2 = 11.08, p = 0.053), “belief in avoidance” (χ 2 = 10.50, p = 0.062), and “outcome expectancy” (χ 2 = 3.44, p = 0.633). Then, the results of t-test showed that medical professionals had a higher score in “belief in avoidance” (t = 7.18, p = 0.008) than psychosocial care professionals. Therefore, two categories (medical vs. psychosocial professionals) were entered in the regressions.
For “negative emotional reactions,” the significant predictors included work-related stress in hospice palliative care (t = 3.42, p = 0.001), self-rated ability for bereavement care (t = −3.13, p = 0.002), and negative impact (t = 5.94, p < 0.001) and positive impact from major life loss (t = −2.54, p = 0.012). For “lack of ability,” the significant predictors included age (t = −3.12, p = 0.002), work-related stress in hospice palliative care (t = 3.01, p = 0.003), self-rated ability for bereavement care (t = −2.24, p = 0.026), and negative impact from major life loss (t = 4.00, p < 0.001). For “belief in avoidance,” the significant predictors included having an undergraduate degree (t = −2.40, p = 0.017), inner growth from hospice palliative care (t = −3.06, p = 0.003), self-rated ability for bereavement care (t = −2.20, p = 0.029), and negative impact from major life loss (t = 2.44, p = 0.012). For “outcome expectancy,” the significant predictors included age (t = −2.75, p = 0.006), work-related stress in hospice palliative care (t = 3.24, p = 0.001), and negative impact from major life loss (t = 1.98, p = 0.049) (see Table 4).
Table 4. Summary of regression analyses: unstandardized coefficients (B) and 95% confidence interval
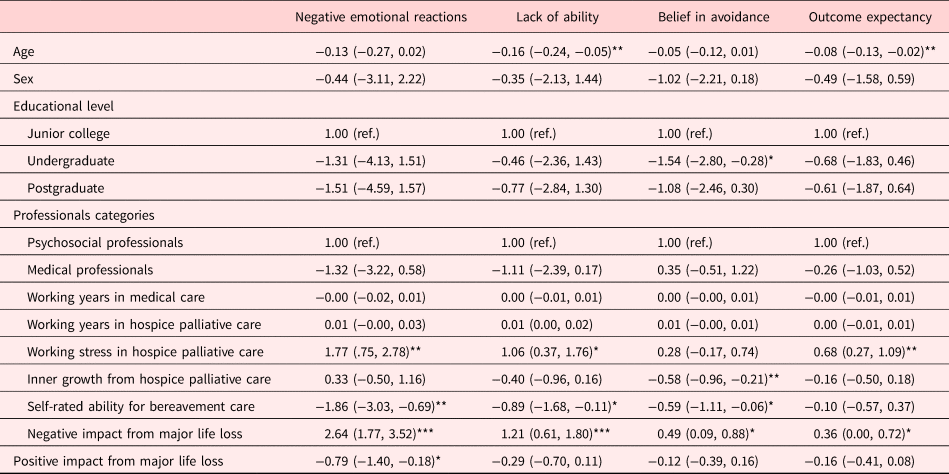
* p < 0.05; **p < 0.01; ***p < 0.001.
Discussion
This study explored the emotional and cognitive barriers for bereavement care among clinical staff in hospice palliative care. One emotional barrier, negative emotional reactions, and three cognitive barriers, lack of ability, belief in avoidance, and outcome expectancy were identified. In addition, the significant demographic and work characteristics related to those barriers were identified, including work-related stress in hospice palliative care, self-rated ability for bereavement care, and negative impact from major life loss.
Negative feelings in the bereaved included grief response. Providing bereavement care was a type of “emotional work” that they had to deal with not only in regard to the relatives of the deceased but also their own emotional wellbeing (Walker and Deacon, Reference Walker and Deacon2016). They had to be aware of patients' and family members' negative emotional responses and help them through the grief journey. Some staff anticipated negative impacts from addressing bereavement-related issues, such as the fear of inducing grief reactions among patients and family members and the fear of harming the doctor-patient relationship (De Vleminck et al., Reference De Vleminck, Houttekier and Pardon2013).
Previous studies revealed that clinical staff were concerned about their ability to engage in bereavement care (McAdam and Erikson, Reference McAdam and Erikson2016; Jensen et al., Reference Jensen, Weng and Spraker-Perlman2017). Bereavement care is one type of psychosocial care, which are not like medical care or treatments that have standardized procedures. Not knowing how to do this is one of difficulties in providing psychosocial care (Fan et al., Reference Fan, Lin and Hsieh2017). Staff acknowledged a lack of experience and confidence and addressed self-imposed limits on their contributions to care (Walker and Deacon, Reference Walker and Deacon2016). The ability to engage in bereavement care includes knowledge, skill, and attitude. They needed to understand grief reactions, manage negative emotional responses, accept the grief reactions of patients and family members, and provide support. Furthermore, they needed educational training and support from psychosocial care professionals (Chan and Arthur, Reference Chan and Arthur2009).
Belief in avoidance involved assumptions about patients' and family members' reactions. Clinical staff assumed patients and family members did not want to discuss the issue (Weiner and Cole, Reference Weiner and Cole2004a). On the other hand, they worried that discussions related to bereavement would make patients and family members feel worse or cry. This unverified belief would be an excuse to avoid the relevant discussion or neglect relevant information and needs. Thus, staff did not provide appropriate care or follow-ups. Clinical staff thought that other healthcare professionals were better positioned to provide care, that patients or family member did not want to talk, or that it was the personal business of the patients or family members (De Vleminck et al., Reference De Vleminck, Houttekier and Pardon2013).
A survey revealed that 33.5% of physicians and nurses did not have confidence in their ability to manage relatives' grief, and that their reasons for not taking action included the desire to leave the bereaved alone (25.0%) and the fear of hurting relatives (14.1%) (Tse et al., Reference Tse, Wu and Suen2006). Personal discomfort about death and dying, reluctance to deliver bad and painful information, and perceptions of personal failures about end-of-life discussions made physicians avoid relevant issues (Granek et al., Reference Granek, Krzyzanowska and Tozer2013). These cognitive beliefs would stop clinical staff from taking action or approaching patients and family members.
The outcome expectancy was that participants expected they could make the patients and family members feel better or reduce their grief responses. Clinical staff believed that it was their responsibility to help family members progress through grief because not expressing empathy after the patient's death might make family members feel abandoned (Jensen et al., Reference Jensen, Weng and Spraker-Perlman2017). This expectation would increase psychological burden when approaching patients and family members.
The participants who rated themselves as experiencing higher work-related stress in hospice palliative care, less ability for bereavement care, and having negative impacts from major life loss, tended to have higher emotional and cognitive barriers. Previous studies showed that nurses who held religious beliefs, positive attitudes toward the policy of bereavement care, and specialized training tended to have more positive attitudes toward bereavement care (Chan and Arthur, Reference Chan and Arthur2009). However, the results of this study also showed the importance of stress management, work ability, and recovery from personal loss.
Clinical staff members' stress may come from the responsibility of hospice palliative care, the workload in clinical care, or the lack of sufficient professional support from colleagues. Similar to previous studies (Tse et al., Reference Tse, Wu and Suen2006; McAdam and Erikson, Reference McAdam and Erikson2016; Fan et al., Reference Fan, Lin and Hsieh2017; Jensen et al., Reference Jensen, Weng and Spraker-Perlman2017), perceptions of lack of ability made clinical staff avoid the relevant care. In addition, caring for dying patients and bereaved family members while witnessing their suffering may induce various emotional reactions (Walker and Deacon, Reference Walker and Deacon2016). Past major life loss caused negative impacts on clinical staff, and unsolved grief or loss experiences became barriers for approaching patients or discussing similar issues.
Professional category was not a significant predictor of the barriers; however, medical and psychosocial professionals have different training backgrounds and tasks in the medical team. Medical professionals may encounter a bereavement reaction when providing physical care. For psychosocial professionals, it is their main task to deal with patients’ and family members' grief reaction and provide bereavement care. They may have different barriers and need different training programs.
Clinical staff should learn the relevant skills and prepare themselves to interact with terminally ill patients and their family members, as well as to provide bereavement care (Raymond et al., Reference Raymond, Lee and Bloomer2017). The foundation of an educational training program should be to foster expectations for external resources from mental healthcare professionals, reduce their workload, and understanding intrapersonal barriers. Clinical staff can engage in self-introspection to explore the barriers of providing bereavement care and try to overcome those barriers.
This study used a quantitative analysis method to explore the barriers of bereavement care. There are some limitations to this study. First, most of the participants were female and various kinds of professionals were recruited; however, medical professionals and mental health professionals may experience different barriers and need different training education. Second, the participants were interested in the course of psychosocial care and might have high self-reflection or awareness of their psychosocial care work. Third, personal variables related to barriers needed comprehensive measurement, including the personal loss or work-related stress. Fourth, the initial items were reviewed by an expert panel for the concept of items and wording, but a pilot study was not conducted for demonstrating the acceptability of wording. Future studies can address the impact of barriers on clinical work, and the effects of educational training programs that aim to modify these barriers.
In conclusion, the barriers to bereavement care by clinical staff in hospice palliative care included not only negative emotions but also cognitive barriers. These cognitive barriers included lack of ability, belief in avoidance, and outcome expectations. In addition, the significant predictors were work-related stress, self-rated ability, and negative impact from major life loss.
Acknowledgments
We would like to thank the experts who provided opinions in content validity and Hospice Foundation of Taiwan for funding support.
Funding
This study was supported by Chi Mei Medical Center (grant number CLFHR10433) and Hospice Foundation of Taiwan.
Conflicts of interest
The authors declare that there is no conflict of interest in this study.







