Introduction
Frontline workers, including healthcare workers, first responders, and workers in essential services, have been hailed as the ‘heroes’ of the COVID-19 pandemic, with the services they render being essential to the functioning of society and the care of those with COVID-19. Reference Cox1 However, these discourses often discount the mental health impacts on frontline workers exposed to the risk of contracting COVID-19, and the various impacts of supporting people struggling with the social, and economic, as well as emotional and physical effects of the virus. Reference Cox1–Reference Rumsey, Neill and Baird4 Psychosocial skills training is considered a key component of effective health promotion for frontline workers during the COVID-19 pandemic; it is also recommended by the World Health Organization (WHO), 5 and the United Nations Office for the Coordination of Humanitarian Affairs (OCHA). 6 However, research indicates that psychosocial skills training programs tend to be oriented towards the needs of first responders in the Global North and do not meet the requirements of frontline workers in low-to-middle income countries where health resources, contextually relevant information, and psychological support are often scarce. Reference Rumsey, Neill and Baird4,Reference Rumsey and Brown7,Reference Wang, Norman, Xiao, Li and Leamy8 This paper reports on the evaluation of a culturally adapted psychosocial skills program that sought to address this training gap for frontline workers in under-resourced countries across the Western Pacific Region and other international contexts. Reference Rumsey and Brown7
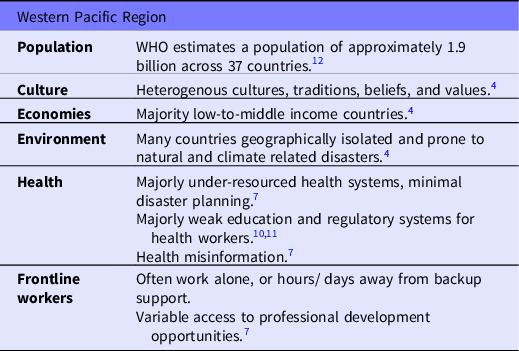
In this paper, the term ‘frontline workers’ is used to refer to essential workers as defined by the Centre for Disease Control (CDC), which includes healthcare workers (paid and unpaid) involved directly or indirectly in patient care; and non-healthcare workers, including first responders and essential workers involved in maintaining critical infrastructure and services e.g., police, and firefighters, as well as food manufacturing, agriculture, and teachers etc. 9 This definition not only captures the broad range of frontline workers who have higher work-related exposure to COVID-19, it is also useful for capturing the reality of frontline work in the Western Pacific context. Education and regulatory systems are weak across some countries within the Western Pacific Region, and even though healthcare workers may not have the right credentials, some may work formally or informally as frontline workers within their communities. 10,Reference Rumsey, Thiessen and Neill11 Information on the characteristics of the Western Pacific Region is provided in Table 1.
Table 1. Characteristics of the Western Pacific Region
Background
High levels of fear, stress, and uncertainty have been reported among frontline workers during the COVID-19 pandemic, as they face the potential for infection of themselves and family members. Reference Boden, Zimmerman and Azevedo13,Reference Vindegaard and Benros14 Distress among frontline workers is also reported in relation to multiple factors, including: the lack of available resources to provide safe and effective care Reference Kea, Johnson and Lin15 ; ‘letting down’ over-stretched co-workers who become infected with COVID-19; violation of values when enforcing COVID-19 visiting restrictions on family members in health services; Reference Smallwood, Pascoe, Karimi and Willis2,Reference Vindegaard and Benros14 and lack of adequate training to provide additional psychosocial support required for patients and community members during the pandemic. Reference Usher, Durkin and Bhullar16
Distress in frontline workers is linked to insomnia, anxiety, depression, and post-traumatic stress disorder (PTSD), as well as burnout, Reference Smallwood, Pascoe, Karimi and Willis2,Reference Boden, Zimmerman and Azevedo13,Reference Lange17,Reference Shanafelt, Boone, Tan, Dyrbye, Sotile and Satele18 however they may struggle to access mental health support, particularly if they must self-quarantine from friends, family, and the community as a protective measure. Indeed, research indicates that isolation can exacerbate distress, with frontline workers suffering higher levels of PTSD than the general population following quarantine. Reference Lange17 Frontline workers may also experience barriers to accessing support due to poorly funded and organized health systems, or during times when COVID-19 cases rapidly overwhelm health systems. Reference Shanafelt, Boone, Tan, Dyrbye, Sotile and Satele18 Internationally, governments, public health measures, and healthcare organizations have primarily focused on the pathogenicity and physiological effects of COVID-19, with less attention given to mental health and well-being of frontline workers. Reference Ornell, Schuch, Sordi and Kessler3 Protective factors identified for frontline workers include access to credible accurate information, social connection, psychological support, and actions for self-care. Reference Usher, Durkin and Bhullar16,Reference Lange17,Reference Xiong, Lipsitz and Nasri19
Psychological first aid (PFA) training can also mitigate the mental health impacts of pandemics and disasters by promoting frontline workers’ resilience and recovery from distressing events, and providing frontline workers with the skills, confidence and preparedness to deliver psychosocial supports to patients and community. Reference Shah, Bedi, Onyeaka, Singh and Chaudhari20–22 PFA training programs have become increasingly popular in disaster medicine post 9/ 11, as risk of PTSD and psychological distress has become more widely understood and acknowledged. Reference Wang, Norman, Xiao, Li and Leamy8 There is no universal definition for PFA training and a wide variety of training resources exist, Reference Wang, Norman, Xiao, Li and Leamy8 including evaluated models such as PFA Field Operations Guide, Reference Brymer, Jacobs and Layne23 WHO PFA Guide, 24 and John Hopkins PFA Guide. 22 PFA content varies, but commonly includes information on self-care, coping strategies, and skills in how to reduce distress and anxiety, as well as communication and problem-solving skills to assess, support, and facilitate access for people in crisis situations. Reference Wang, Norman, Xiao, Li and Leamy8,Reference Corey, Vallires, Frawley, De Brn, Davidson and Gilmore25,Reference Fox, Burkle, Bass, Pia, Epstein and Markenson26 Training has been delivered in online, blended, and face-to-face formats, Reference Wang, Norman, Xiao, Li and Leamy8,Reference Shah, Bedi, Onyeaka, Singh and Chaudhari20,Reference Everly and Lating27,Reference Everly, Barnett and Links28 most often by Non-Governmental Organization staff, healthcare workers, or community members. Reference Wang, Norman, Xiao, Li and Leamy8
A recent scoping review by Wang et al. Reference Wang, Norman, Xiao, Li and Leamy8 indicates that PFA training increased participants knowledge and preparedness for traumatic events, and improved communication, coping skills and detection of mental distress in real-world crisis events. Reference Wang, Norman, Xiao, Li and Leamy8 However, uptake of PFA programs is inconsistent and may not meet the specific needs of frontline workers in contexts with limited health resources. Reference Horn, O’May and Esliker29 Evaluations of PFA programs are predominantly of face-to-face training programs for first responders in the Global North. Reference Wang, Norman, Xiao, Li and Leamy8 Therefore, it is uncertain whether PFA programs are experienced as accessible, relevant, or culturally safe for all frontline workers, particularly since few incorporate Indigenous and Global South perspectives in the design phases. Reference Rumsey, Neill and Baird4,Reference Wang, Norman, Xiao, Li and Leamy8,Reference Kurtz, Janke, Vinek, Wells, Hutcinson and Froste30,Reference Rochecouste, Oiver and Bennell31
Cultural adaptation of PFA programs, with stakeholder input and expert online delivery, might be relevant to international frontline workers working in the COVID-19 pandemic in culturally diverse and poorly resourced settings. This paper reports on a cultural adaptation and evaluation of the United Nations and humanitarian partners Inter-agency Standing Committee (IASC), PFA, which is referred to as the ‘Basic Psychosocial Skills (BPS) guide for COVID-19 Responders.’ 32 The IASC BPS training was chosen for adaptation because, unlike other PFA training, it is not focused on acute disaster responses, but was developed specifically for frontline workers responding to the COVID-19 pandemic. 32 It incorporates WHO PFA principles of safety, self and community efficacy, strategies to promote comfort, and calm, as well as coping, connectivity, and a focus on community and individual strengths. 24,32 The cultural adaptation of the IASC BPS aimed to ensure it was accessible and appropriate for frontline workers in under-resourced countries within the Western Pacific Region, as well as other under-resourced international contexts where the program is being offered.
Methods
Cultural adaptation of a BPS training
In collaboration with WHO, the WHO Collaborating Centre (WHO CC) at the University of Technology Sydney (UTS) initiated a cultural adaptation of the IASC BPS using a ‘PARcific’ methodology as outlined by Rumsey et al. Reference Rumsey, Stowers and Sam33 PARcific methodology brings together participatory action research (PAR) methods with Pacific cultural methodologies, including Talanoa and Kakala, and allows collaborators to explore the nuanced cultural worldview and context of Pacific peoples and undertake culturally resonant action for change. Reference Rumsey, Stowers and Sam33
Drawing on the PARcific methodology, WHO CC educators and researchers first established partnerships with frontline workers and key stakeholders from the Western Pacific – including frontline workers from the Western Pacific Working Group and regional partner organizations, Western Pacific nurse leaders, and international WHO health system and service staff. Then, in virtual meetings, the project team gathered and used cultural, collective, and dialogical ways of working, which are central to many Pacific cultures across PAR cycles – listening, thinking, reflecting, and action. Through these dialogical cycles, the team collaboratively prioritized and designed culturally and contextually relevant content, communication, and dissemination strategies. Reference Rumsey, Stowers and Sam33
The final BPS training is an online, self-paced program with tutor facilitation consisting of 4 modules that cover: (i) personal safety, health, and well-being; (ii) therapeutic communication skills; (iii) practical frameworks for problem-solving, decision-making, and referral; and (iv) recognizing and responding to people in distress. 34 To promote accessibility for frontline workers in the Western Pacific, the program includes case studies representative of Pacific people’s cultural, social context, and identity; content is written in deliberately simple language and configured for online delivery by educational designers specializing in online, interactive, asynchronous format. Although the BPS was originally developed specifically for workers in the Western Pacific, it was made free and available for frontline workers in all international regions. The BPS is delivered via UTS Open, which offers free online university courses and micro-credentials to the local, national, and international community. 34 The program is promoted via the WHO and university media. 35 At the time of writing, 1000 individuals had completed the course online, with the hope that more will engage as awareness of the resource grows.
Evaluation of the culturally adapted BPS training
Following approval from the relevant human research ethics committee, the culturally adapted BPS program was evaluated with a cross-sectional survey. All frontline workers who had completed the online BPS training program between February 2021 and February 2022 were invited to participate via email. Inclusion was limited to those who had internet service, were English speaking, over 18 years, and met the Centre for Disease Control’s (CDC) definition of essential workers, which includes healthcare workers (paid and unpaid) involved directly or indirectly in patient care; and non-healthcare frontline workers essential for maintaining critical infrastructure and services. 9
Data collection
Data was collected via Qualtrics (Qualtrics International Inc., Provo, New York, USA) between March to April 2022. This period coincided with rapid spread of the COVID-19 Omicron variant, which was overwhelming health services across the globe. The survey consisted of 5 demographic and workforce characteristic questions including gender, age, country, and city of residence, as well as frontline worker role, and date of program completion. A Likert scale measured participants’ perceived level of confidence and their satisfaction with the course content (5 represented high-level agreement and 1 represented disagreement to statements posed). Statements sought to determine participants’ post-training perceived confidence in their ability to: manage personal distress; provide practical support to others; provide emotional support to others; and apply information and skills to daily life. Additional statements sought to determine participants’ perception of the BPS training programs, including: the value of the program for skill development; relevance of the program to participants’ context; interactivity of the program; and participants whether the program was perceived as engaging. The survey included 5 open-ended questions about the BPS training program that elaborated on quantitative data, including: participants’ reasons for undertaking the program; how culturally adapted content supported learning; most useful aspects of the program; accessibility of the program; and suggested improvements.
Data was extracted from Qualtrics (Qualtrics International Inc., Provo, New York, USA) and imported into Statistical Package for the Social Sciences (SPSS, Version 27) (IBM Corp., Armonk, New York, USA) for data cleaning, management, and analysis. The role of health professionals was recoded and categorized as Nurse, Midwife, Manager, or Other, and Country of residence were recoded into WHO geographical regions. Qualitative survey responses were checked for any identifying data and de-identified prior to analysis.
Data analysis
Descriptive statistics were undertaken in SPSS (IBM Corp., Armonk, New York, USA). Continuous data were reported as a mean value and standard deviation. Categorical data were reported as frequencies. 1-way ANOVA measured significant difference between participants’ perceived level of confidence, satisfaction mean scores, and variables of interest: age, country of residence by WHO region, and the position that participants were employed in at the time of the survey.
Qualitative survey responses were thematically analyzed, an approach used previously to analyze qualitative survey data. Reference Vaughn and Turner36 Analysis followed the steps outlined by Braun and Clarke: data familiarization, code generation, theme development, and team review, as well as definition and naming of themes, and reporting. Reference Braun and Clarke37 Following the approach taken by Kendall and Schussler, Reference Kendall and Schussler38 once codes and themes were agreed on, the researchers tallied the number of times they appeared in participant responses.
Results
Out of a total of 1000 people who had undertaken the online BPS training program and received an email invitation, 118 (11.8%) participated in this survey study.
Demographics of participants
Participants were from diverse backgrounds, organizations, and countries, and completed the online training at work or in their personal time. Participants predominantly identified as female (n = 80/118, 67.8%) and were employed as healthcare professionals (n = 73/118, 67%), first responders (n = 6/118, 5.5%), supervisors/ managers (n = 12/118, 11%), and other (n = 18/118, 15.5%) such as funeral workers, transport drivers and government utility workers (Table 2). Of those identifying as a healthcare professional (n = 73, 67%), 30 identified as a registered nurse working in a community setting, including Human Immunodeficiency Virus (HIV) clinics, and mental health settings, as well as nurse education or nurse administration; and 2 healthcare professionals identified as being a midwife. First responders (n = 6, 5.5%) reported working in mental health and/ or counselling services. All 6 WHO regions were represented in the survey (Table 3) although close to 50% of the participants (n = 49, 45%) resided in the Western Pacific Region.
Table 2. Demographic and workforce characteristics of participants
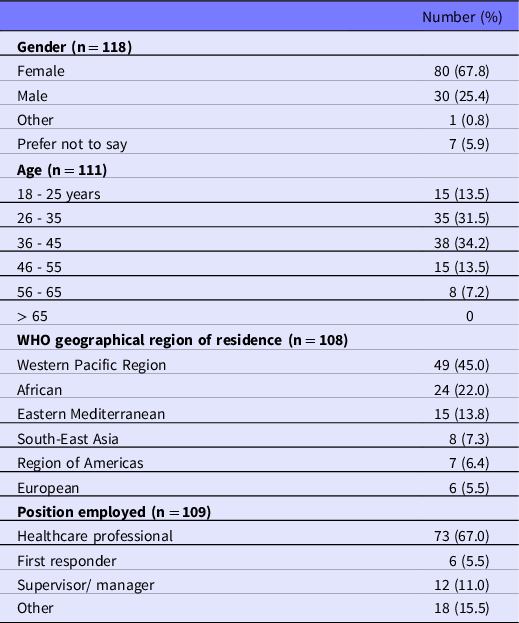
Table 3. Participants level of confidence and satisfaction mean scores

Quantitative descriptive analysis
Mean scores for perceived confidence levels ranged from 3.8 to 3.9 (Table 3). No significant difference was found between participants’ reported levels of confidence mean values and country of residence by WHO geographical region, age, or position of employment group. Similarly, participants’ satisfaction with the program content, relevance, and acquired knowledge reported a mean score of 4.0 to 4.3, and reported no difference between groups (WHO region and employment).
Qualitative thematic analysis
Open-ended questions elicited between 66 and 76 responses per question. Thematically analyzed responses generated between 2 and 4 key themes per question. Themes are reported below with a tally of number of responses per theme.
Reasons for undertaking the BPS training
Thematically analyzed open-ended responses (n = 76) to the question about participants’ reasons for undertaking the BPS program generated 3 key themes: ‘skills to support others,’ ‘personal benefit,’ and ‘professional development.’
The theme, skills to support others (n = 25), indicated that most participants undertook the BPS training program to develop psychosocial skills, including therapeutic skills to support community members, or patients. Of these participants, 8 indicated that they wished to support community members or patients going through ‘hard’ or ‘difficult’ times related to the COVID-19 pandemic, conflict, or disaster. This theme was encapsulated by the following statements:
‘[I] wanted to do what I could to ensure I was as skilled and competent as possible, to respond to increasing anxiety among patients.’
‘I took the course because I wanted to know how to respond to emergencies especially during this [sic] hard times.’
The theme, personal benefit (n = 24), indicated that participants also undertook the training to relieve personal stress and develop skills about stress management, with 2 participants reporting that this stress was directly related to the COVID-19 pandemic. The following statements capture this theme:
‘I took this basic psychosocial skills course to learn how to handle my own psychological stress.’
‘[I wanted to] enhance my knowledge and skills to manage stress.’
The theme professional development (n = 14) captured those participants who indicated that they undertook the training to earn or maintain professional credentials, and mandatory training (n = 9) captured those participants who were directed to undertake the BPS training by a service or organization.
Value of culturally adapted case studies
Of the 69 open-ended responses, 57 (83%) indicated that the culturally adapted content developed for the Western Pacific, supported participants’ learning. 17 responses merely stated ‘yes’ or ‘definitely,’ however the remaining responses (n = 40) reported how content and case studies supported learning and yielded 2 key themes: real-world learning and relevance to context.
The theme real-world learning (n = 23) captured participants’ view that the case studies provided real-world examples of the application of concepts that supported their knowledge and skill development. This theme was captured by 1 participant’s comment, who stated that ‘case studies are helpful with making links and being able to solve issues.’ 4 responses indicated that the cases prepared them to understand how to manage situations related to the COVID-19 pandemic, and another 4 indicated that the cases helped them to understand and manage their own stress.
The theme relevance to context (n = 20) indicated that participants found the content relevant to their day-to-day lives, and the quantitative data (mean score of 4.3 for relevance to current situation) indicated that relevance related to cultural context, current crises, or participants’ frontline worker role. Two people indicated that the content was relevant to their desire to understand the needs of culturally diverse people, and 1 further indicated that while the content was somewhat resonant, they would prefer content specific to the ‘Asian context.’ This theme was largely encapsulated by the statements:
‘I was able to identify closely with the issues because the cultures and traditions were similar to my own or at that at home.’
‘It actually depicts the daily living crisis that we are in now.’
Useful aspects of the BPS program
Of the 60 open-ended responses, 10 indicated that ‘all’ or ‘most’ aspects of the program were useful, and 4 indicated that overall, it built their knowledge. The remaining responses (n = 50) produced 3 themes: educational approach, building psychosocial skills, and learning to manage stress.
The theme, educational approach (n = 27) elaborates on quantitative data (mean satisfaction scores related to interactivity, 4.0 and engagement, 4.1), pointing to the specific value of incorporating case studies, videos/ interactive exercises, and summaries. 1 participant also stated that the structure was ‘simple and easy to follow’ without being ‘too basic.’ This helped them not only to learn but also in ‘calming anxiety levels.’
The theme, building psychosocial skills (n = 22), elaborates on quantitative data on satisfaction (new skills from completing the program, mean score 4.1) and confidence (ability to provide practical support and emotional support, mean score 3.9), indicating that the BPS program supported participants to learn psychosocial skills, with the majority of statements highlighting the value of therapeutic skill development, as well as social support, cross-cultural practice, and problem-solving skills. Statements that captured this theme include:
‘The aspects that helped most were those that teach you how to correctly respond to people dealing with problems, people that are sharing their feelings and concerns, and how not to invalidate those feelings. Most of the things that are taught in the program are helpful especially in communicating with different people and their respective cultures.’
The theme of Learning to manage stress (n = 10) elaborates on quantitative data on confidence (ability to manage personal stress and apply the information and skills from this course in my daily life, mean scores of 3.8 and 3.9 respectively). Data indicates that participants found the BPS program helped them to understand and manage personal stress, with 1 statement highlighting specific skills learned in the program for stress management: ‘managing stress, the types of breathing to help you to calm down.’
Challenges in accessing the program
Of the 66 open-ended responses, 38 (58%) indicated that participants had no challenges accessing the program. The remaining 28 responses were divided into themes of internet challenges and time and duration, with a grouping of miscellaneous challenges, including difficulty accessing the Certificate of Completion, or problems of being identifiable to other community members in the online course.
Internet challenges (n = 15) spoke to difficulties with internet connection in international contexts, which included stability of internet connection as well as access to sufficient available internet data to access the program. The theme of time and duration (n = 9) pointed to the issues of finding time for online learning, as well as managing time differences to engage in interactive sessions. A small number of responses (n = 2) also indicated that the BPS course was ‘too long’ or ‘longer than anticipated.’
Suggested improvements
Of the 66 open-ended responses, 38 (58%) indicated that participants had no improvements to suggest. The remaining 28 responses could be divided into 2 themes, enhancing online learning, and increasing diversity.
Enhancing online learning (n = 21) chiefly related to a desire for increased opportunities to interact with other participants and facilitators in the BPS program. However, 2 participants also indicated that they would prefer anonymous participation and found it difficult to post in online discussions as this required identifying information e.g., name. Some participants requested more program frequency, including a refresher program.
The theme of increasing diversity (n = 7) indicated suggestions for more diverse representation of cultures and languages. This theme was captured by the following statement:
‘Perhaps at a later stage we can provide these trainings in iTaukei (Fijian) and Indo-Fijian (Fiji Hindi) languages.’
Finally, under this theme, 2 participants noted that content was oriented towards health professionals and less relevant to their work context.
Discussion
This study reports on a cross sectional survey evaluation of an innovative cultural adaptation of the MHPSS BPS training program, adapted for use in the Western Pacific. It aimed to provide a culturally resonant, high-quality, online training program for delivery to large cohorts of international frontline workers in under-resourced contexts during the COVID-19 pandemic. The findings provide an understanding of participants’ experience of learning and their perceived confidence, satisfaction, accessibility, and acceptability of the BPS training program, and reinforce the benefits of a program designed to meet the learning needs of a culturally and linguistically diverse adult population.
Overall, high mean scores for confidence and satisfaction with the MHPSS BPS training program were reported. No significant difference between participant groups regarding age, WHO geographical region, or professional role were found and suggest that the effectiveness, accessibility of language and content of the program was appropriate. Position of employment may be considered a surrogate marker for a participant’s level of education and literacy. Given that education and literacy are acknowledged as important social determinants of health and have a long-term impact on social and economic development, continued refinement and evaluation of online learning program seems prudent.
Irrespective of participants region of residence, participants had high self-reported satisfaction scores. Survey data provides some elaboration on satisfaction scores, indicating that culturally adapted case studies – developed for the Western Pacific context – were well received, with many participants reporting that these were relevant to their culture, beliefs, and traditions similar to their ‘home.’ Nonetheless, participants recommended more diverse representation of culture and languages in the program; and some indicated that case studies were less relevant to Asian contexts and suggested that the BPS program be translated into languages other than English. The call for more cultural diversity may be due to the program being offered beyond the original intended audience in the Western Pacific via the international WHO Nursing and Midwifery Global Community of Practice site. 35 However, this finding indicates an international appetite for culturally and linguistically diverse PFA online programs.
While quantitative data indicate that interactivity and engagement with the program was perceived as highly satisfactory (mean scores of 4.0 and 4.1 respectively), qualitative data identified specific factors of the online program that were considered most useful, including case studies, multimedia, and interactive exercises. Besides being culturally resonant, case studies were perceived as providing ‘real-world’ examples that were relevant to multiple international contexts. The value of case studies in PFA training has been noted previously (e.g., Horn et al.). Reference Horn, O’May and Esliker29 In this study, 1 participant also reported that engagement was enhanced by the structure of the program, which was perceived as easy to follow and ‘calming.’ This may reflect the deliberately simple approach to language adopted in the cultural adaptation of the BPS. As previously argued, simple language in PFAs can support accessibility in diverse sociocultural settings. Reference Wang, Norman, Xiao, Li and Leamy8 However, this study indicates that an easy-to-follow format not only increases accessibility and supports learning, but also has the potential to reduce anxiety about participation. To date, the format of content in PFA has not been linked with key principles of ‘calming,’ which are central to PFA training. Reference Hobfoll, Watson and Bell39
While online delivery of the BPS may have aided access to the program across international settings, some participants reported challenges related to internet connection and data availability, as well as time constraints. This has been reported in other studies and was 1 of the concepts behind contextual development e.g., the need for asynchronous online content. Reference Rumsey, Thiessen and Neill40 Frontline workers preference for online training, as well as difficulties securing time to engage in PFA have been reported previously, with some adaptations involving abridged programs for health workers. Reference Wang, Norman, Xiao, Li and Leamy8,Reference Said, Molassiotis and Chiang21 However, since most evaluations of PFA training programs have occurred in middle/ high income countries, Reference Wang, Norman, Xiao, Li and Leamy8 issues of connectivity may be of more significance in the Global South, where participants may not only struggle with internet connection, but also access to, and cost of, internet data.
Participants reported that the BPS program useful for increasing confidence in their ability to provide practical support to others and manage personal stress. The acquisition of psychosocial skills, including therapeutic, social, cross-cultural, and problem-solving skills, as well as skills to manage personal stress, were considered particularly useful. This finding supports previous work on the value of self and community efficacy in PFA training. Reference Kilic and Simsek41 Qualitative data also provides some details about aspects of the program that supported participants’ ability to manage stress, including breathing exercises and case study examples. Breathing exercises have been described previously as useful in promoting calm, Reference Hobfoll, Watson and Bell39 however little has been said of how case studies, and in the case of this study, culturally adapted case studies, might contribute to this. This finding is important given that data indicate participants’ reasons for accessing the BPS training were for psychosocial skills to support others, as well as for personal stress management, with many reporting that they struggled with stress related to the COVID-19 pandemic.
More opportunities for peer and teacher interactions in online programs appear to be important, as well as an option for participant anonymity. Peer interactions would arguably promote connectivity, which is a key principle of the PFA approach to supporting frontline workers in crisis situations. 24 Anonymity, an issue not raised in previous studies, might also make the program more accessible for participants who could be easily identified by other community members attending online training. Indeed, anonymity may support participants to post about personal stress and stress management strategies that they might otherwise be reluctant to share.
Limitations
This global study, of a culturally adapted BPS is strengthened by a cross-sectional design that enabled the implementation of an on-line BPS training program and evaluation of the effectiveness of the content during the COVID-19 pandemic. However, a pre- and post- cross-sectional survey design would have provided rigor and more accurately measured the effect of the BPS program rather than a single survey. The findings are encouraging but may not be generalized given several study limitations: the small sample size, low response rate (likely influenced by the COVID-19 pandemic), and the timing of the survey that may be subject to recall bias. The sample size, while small was sufficient to undertake descriptive statistics, statistically compare differences between groups, and provide a snapshot evaluation of the BPS program. Additionally, the interpretation of the data is limited by self-reported responses and may be subject to selection bias, whereby participants responses may differ from non-participants as well as gender, and geographical biases.
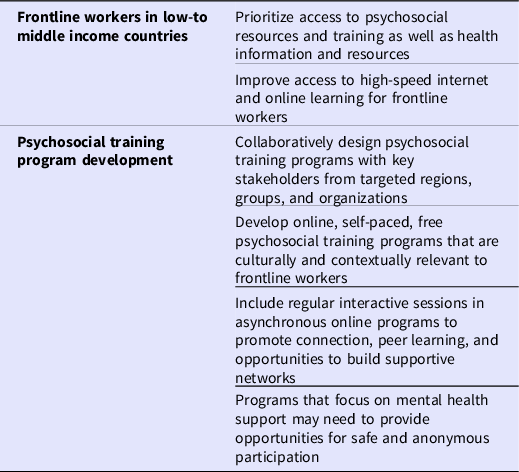
The findings have important policy implications (See Table 4) for future pandemic and disaster planning, including the need for access to culturally resonant psychosocial resources and training for frontline workers in under-resourced settings. Programs should be asynchronous to account for time and internet constraints but provide opportunities for online engagement and discussion as well as anonymous participation.
Table 4. Policy implications
Conclusions
This cross-sectional survey study presents an evaluation of an innovative BPS program that was culturally adapted to incorporate stakeholder perspectives from across the Western Pacific region and was delivered online to international cohorts in 6 WHO geographic regions. Findings indicate that the program enhanced participants’ perceived confidence and skills to manage personal stress and provide psychosocial support to others. Culturally adapted case studies, in simple language formats, were perceived as relevant to participants’ context and promoted a sense of calm in participants. International participants indicated an appetite for more diverse representation to enhance the cultural resonance of the program in contexts outside of the Western Pacific region. While online delivery enhanced accessibility of the BPS program, access was limited by unstable internet connection and limited internet data. In the design of online BPS training, designers should consider options for real-time peer engagement to promote connectivity, as well as an option of anonymity to enhance engagement with discussion boards.
Acknowledgements
The authors thank Jennifer Hall (WHO), Martin Vandendyck (WHO Regional Office for the Western Pacific, Manila, Philippines), and Yutaro Setoya PhD (WHO Country Liaison Office for Tonga, Ministry of Health, Nuku’alofa, Tonga.
Authors contribution
DB, JR, and SSL carried out the survey evaluation, and analysis, as well as wrote the manuscript with support from authors OC, JO, LT, EI, and MR. Authors MR, DB, and LT conceived and planned the BPS program and evaluation, while OC, JO, LT, and EI contributed expert advice on the cultural adaptation of the BPS program, BPS evaluation, and analysis.
Competing interests
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.






