Current management strategies for bipolar disorder focus on the treatment of acute episodes, relapse prevention and maintenance therapies (National Institute for Health and Clinical Excellence 2006). To date, early intervention in bipolar disorder has received relatively little attention, in contrast to the increasing numbers of articles published in recent years on early intervention in schizophrenia.
Bipolar disorder affects about 1% of the population worldwide. A recent international study reported that the median age at onset is 24 years for men and 27 years for women, with a range of 10 to 42 years (Reference Baldessarini, Bolzani and CruzBaldessarini 2009). In the majority of patients, bipolar disorder runs a chronic course, associated with significant morbidity in psychological, social and physical health (Reference KupferKupfer 2005). The estimated cost of bipolar disorder in the UK is £4.59 billion (estimated 2007 value; Reference Fajutrao, Locklear and PriaulxFajutrao 2009), including both direct costs such as those of hospitalisation for acute episodes, and indirect costs such as those of unemployment and suicide.
The need for intervention in the early stages of bipolar disorder
Arguably the most significant challenge is the timely recognition and treatment of the disorder. A large body of evidence across many different countries and service delivery systems has consistently reported delays of several years in making a diagnosis. In a study investigating history of illness prior to diagnosis in 240 patients with bipolar disorder, Reference Berk, Dodd and CallalyBerk et al (2007) found that participants first developed manic symptoms at a median age of 21, and had their first full episode of mania at 24. However, they did not receive a diagnosis of bipolar disorder until a median age of 30. Reference Hirschfeld, Lewis and VornikHirschfeld and colleagues (2003) had previously reported a delay of about 10 years from the first episode of illness to the first diagnosis.
An important difficulty in making an initial diagnosis is in differentiating bipolar disorder from a depressive disorder. Up to 89% of the first episodes of illness in bipolar disorder are depressive (Reference Duffy, Alda and HajekDuffy 2009a), and during the disorder’s course (bipolar I and II: Box 1), depressive symptoms dominate the clinical picture (Reference BenazziBenazzi 2006), so that milder manic or hypomanic episodes may be missed.
BOX 1 Bipolar I and bipolar II disorder
Bipolar I disorder
Characterised by at least one manic episode or mixed episode (clear manic and depressive features present in the same episode). There may also be a history of depressive episodes, although these are not necessary for establishing a diagnosis.
Bipolar II disorder
Characterised by one or more major depressive episodes, together with at least one hypomanic episode in the clinical course.
Bipolar-spectrum disorders, which include subthreshold mood states and milder manic presentations (Reference AngstAngst 2007), pose another challenge to early identification, as most patients do not seek help at that stage. Yet they represent a group that is likely to suffer functional impairment to varying degrees over time (Reference AngstAngst 2007). In addition, the current classification system may not be helpful in the identification of bipolar-spectrum disorders, as the majority of these presentations are classified under major depressive disorder (Reference AngstAngst 2007).
Mania is the diagnostic hallmark of bipolar disorder, but the presence of psychotic symptoms, especially in patients presenting with a manic onset, poses a diagnostic challenge. Psychotic symptoms may be present in 70–88% of patients presenting with a manic onset (Reference Tohen, Zarate and HennenTohen 2003; Reference Yatham, Kauer-Sant'Anna and BondYatham 2009). Additionally, in about 40% of such cases, the psychotic features are not mood congruent (Reference Tohen, Zarate and HennenTohen 2003). Up to 20% of patients with psychotic features at the first presentation of mania, especially those with auditory hallucinations or first-rank symptoms, are misdiagnosed as having a non-affective psychotic disorder such as brief psychotic disorder, psychotic disorder not otherwise specified or schizophreniform disorder (Reference Salvatore, Baldessarini and TohenSalvatore 2009). Particularly in younger patients, there is also the possibility of diagnostic confusion with attention-deficit hyperactivity disorder, personality disorders and substance use-related disorders (Reference Berk, Malhi and GinBerk 2009).
A delay in making a diagnosis of bipolar disorder has potential consequences for clinical outcome. Reference Gazalle, Andreazza and CereserGazalle et al (2005) found that the number of undiagnosed years was directly associated with the level of subsequent psychopathology, particularly depression, and a poorer quality of life. Furthermore, the delay in initiation of mood stabilisers may be associated with subsequent poorer social functioning and increased risk of lifetime suicide attempts (Reference Goldberg and ErnstGoldberg 2002). The present review examines the case for the development of disorder-specific pathways for early detection, and considers the priorities for the optimal treatment of the early stages of bipolar disorder.
High-risk status and the prodromal stage of bipolar disorder
Genetic risk
There have been attempts to identify groups that have a high risk of developing bipolar disorder, with a particular focus on individuals at genetic risk. In a large population-based study, Reference Lichtenstein, Yip and BjörkLichtenstein et al (2009) reported the relative risk of bipolar disorder in the offspring (RR = 6.4) and siblings (RR = 7.9) of probands with bipolar disorder. They also reported a heritability of 59% for bipolar disorder. Additionally, the offspring of probands with schizophrenia were found to have a relative risk of 5.2 for bipolar disorder. However, the majority of patients with bipolar disorder do not have a first-degree family history (Reference Correll, Penzner and LenczCorrell 2007a).
Biological markers of high-risk traits and transition to syndromal states
Another strategy to identify high-risk status of developing bipolar disorder is detection of endophenotypes (Reference Correll, Penzner and LenczCorrell 2007a). Although they do not represent a prodromal state, endophenotypes are biological traits or markers indicating high risk for a specific disorder (Reference Luby and NavsariaLuby 2010). These traits are heritable, state-independent, co-segregate with illness within families and present in unaffected relatives at a higher rate than in the general population (Reference Hasler, Drevets and GouldHasler 2006). Currently studied candidates for endophenotype status in bipolar disorder are shown in Box 2 (Reference Correll, Penzner and LenczCorrell 2007a; Reference Luby and NavsariaLuby 2010). Also being investigated are brain structural changes that may help with early identification of high-risk individuals who are more likely to undergo transition to syndromal states. A preliminary study comparing patients with bipolar I disorder and their unaffected relatives with major depressive disorder showed association of increased left insular volume with genetic predisposition, increased left substantia nigra volume with manic expression and increased left vermal volume with resilience to bipolar disorder (Reference Kempton, Haldane and FrangouKempton 2009).
BOX 2 Features currently studied for endophenotype status in bipolar disorder
Neuroanatomical abnormalities
-
• Amygdala
-
• Ventral prefrontal cortex
-
• Cingulate
-
• Basal ganglia
-
• Hippocampus
-
• White matter
Neurocognitive abnormalities
-
• Verbal memory
-
• Executive deficits
-
• Response inhibition deficits
-
• Visual spatial deficits
-
• Facial emotion labelling deficits
Neurophysiological abnormalities
-
• Prepulse inhibition
-
• Auditory evoked P300
-
• Circadian rhythm
Temperament and personality traits
-
• Cyclothymia
-
• Hyperthymia
-
• Behavioural disinhibition
Clinical characteristics of the prodromal stage
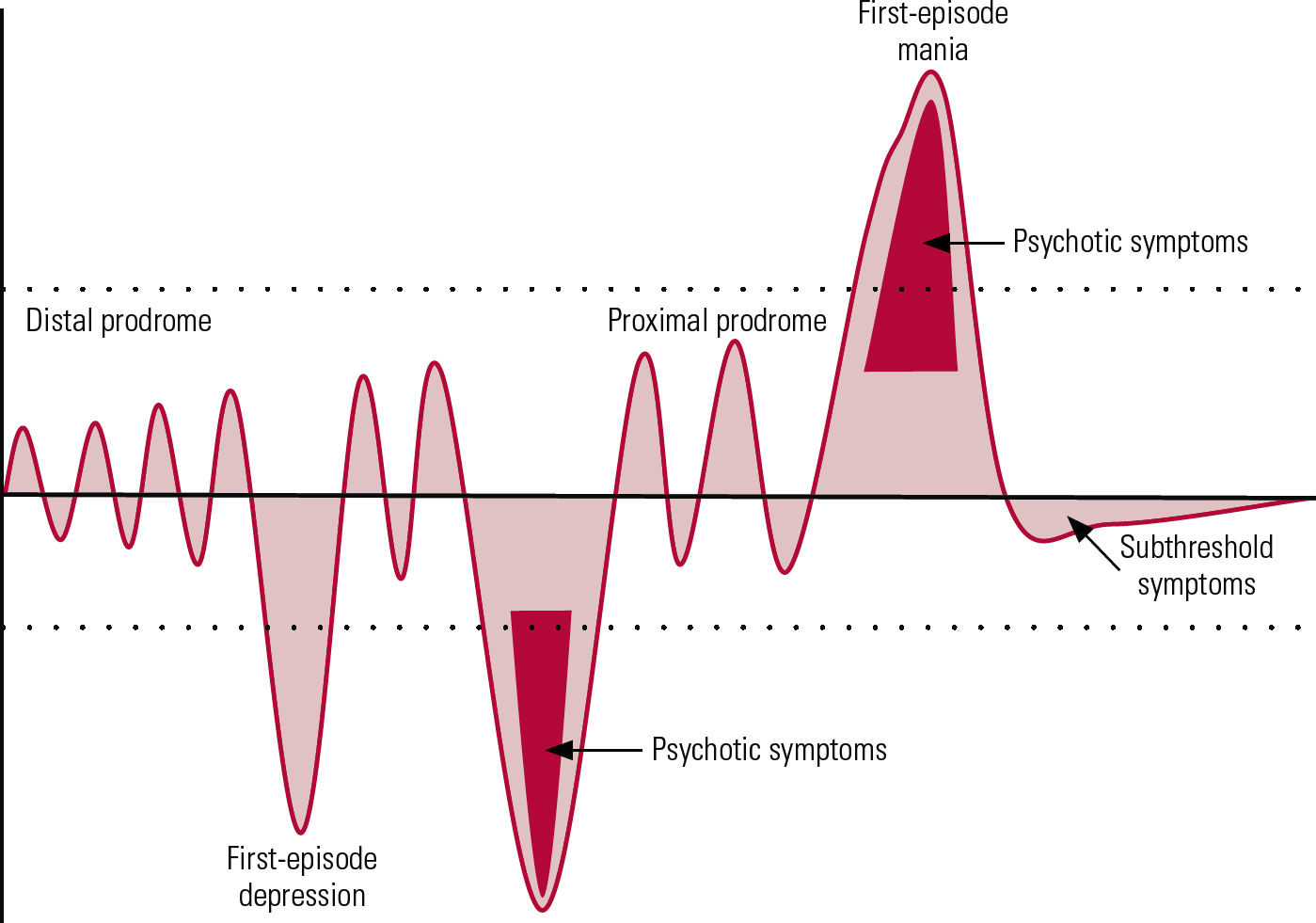
Recent studies have sought to define the prodromal stage of bipolar disorder and have highlighted the associated challenges in its recognition (Reference Howes, Lim and TheologosHowes 2010). This stage can span several years, with subthreshold symptoms beginning in childhood and adolescence (‘distal’ or ‘early’ prodrome), which increase in number, frequency and severity (‘proximal’ or ‘late’ prodrome) immediately preceding the first episode of mania (Reference Skjelstad, Malt and HolteSkjelstad 2009; Reference Howes, Lim and TheologosHowes 2010). The mean duration of the proximal prodrome has been reported as 1.8–2.3 years (Reference Correll, Penzner and FredericksonCorrell 2007b).
Most of the published studies reporting on the prodromal phase have used retrospective design and lacked a control group. This limits sensitivity and specificity analysis, and an effect of recall bias cannot be excluded (Reference Howes, Lim and TheologosHowes 2010). Reference Correll, Penzner and FredericksonCorrell et al (2007b), in a retrospective study on patients with bipolar I disorder using a structured assessment tool, reported a number of subthreshold manic and depressive symptoms and other symptoms in the prodromal phase. In a prospective study of a large community cohort, Reference Tijssen, van Os and WittchenTijssen and colleagues (2010) reported a dose-dependent relationship of persistent subthreshold hypomanic and depressive symptoms with 10-year clinical outcome of bipolar disorder. Although some of the prodromal symptoms (Box 3) have high specificity, all have relatively low sensitivity (Reference Howes, Lim and TheologosHowes 2010). With a high specificity, they yield fewer false positives and can rule out cases as not bipolar disorder, thereby helping in considering the use of interventions that may have adverse effects, such as medications. However, a low sensitivity means that they capture fewer true positives and do not effectively rule in cases, which can be disadvantageous where psychosocial interventions (with less risk of adverse effects) may have a role. In some patients, the prodromal stage is associated with a significant functional decline (Reference Skjelstad, Malt and HolteSkjelstad 2009). In the proximal prodromal phase there can be attenuated psychotic symptoms, particularly in those who subsequently develop mania with psychosis (Reference Correll, Penzner and FredericksonCorrell 2007b). The duration of these symptoms is much shorter than in the schizophrenia prodrome, occurring closer to the time of transition to full-blown bipolar disorder (Reference Correll, Penzner and FredericksonCorrell 2007b).
BOX 3 List of frequently reported prodromal symptoms
Subthreshold mania symptoms
-
• Elevated/irritable mood lasting more than 6 h/day Footnote a
-
• Racing thoughts
-
• Very rapid speech
-
• Increased energy
-
• Reckless/dangerous behaviour
Subthreshold depressive symptoms
-
• Depressed mood lasting more than 6 h/day Footnote a
-
• Anhedonia
-
• Self-harming Footnote a
-
• Suicidal thoughts Footnote a
Others
-
• Mood swings (fluctuation between elevated/irritable and depressive states)
-
• Sleep disturbances
-
• Anxiety symptoms Footnote a
-
• Drop in functioning
-
• Decreased concentration
-
• Social isolation
-
• Marked change in appetite
-
• Hearing voices Footnote a
(Reference Howes, Lim and TheologosHowes 2010)
a Features with a specificity >80% and low sensitivity
Reference Duffy, Alda and HajekDuffy et al (2010), in a prospective study of high-risk offspring of patients with bipolar disorder, reported that there is a chronological sequence of symptoms, starting with anxiety and sleep disorders, followed by mood disturbances, which in association with comorbid substance misuse progress to full-blown mood episodes. It is not yet clear whether this also applies to patients with bipolar disorder without a family history of mood disorders. Cyclothymic features such as mood swings/lability are precursors of bipolar disorder (Reference Angst, Gamma and EndrassAngst 2003; Reference Kochman, Hantouche and FerrariKochman 2005). However, it is not yet known whether these features constitute a personality disorder/trait or a prodromal state (Reference Howes, Lim and TheologosHowes 2010). Thus, combining the findings of certain clinical features with the presence of other high-risk factors could help clinicians to better identify the prodromal state of bipolar disorder.
Treatment challenges in the prodromal stage
The potential role of clinical intervention in the prodromal stage of bipolar disorder is even less clear. There have been studies showing an improvement in mood symptoms with quetiapine (Reference DelBello, Adler and WhitselDelBello 2007) and in aggression with valproate (Reference Saxena, Howe and SimeonovaSaxena 2006) in individuals at high risk for the disorder, but there have also been trials with negative results (Reference Salvadore, Drevets and HenterSalvadore 2008). Psychological treatments have an established role in reducing relapse in established bipolar disorder when used adjunctively (Reference Scott, Colom and VietaScott 2007), and might also be useful in reducing the risk of illness in those at high risk of bipolar disorder, as has been reported in individuals at high risk of psychosis (Reference Morrison, French and WalfordMorrison 2004). An ongoing study in the high-risk population is comparing interpersonal psychotherapy with educational clinical monitoring (http://clinicaltrials.gov/ct2/show/NCT00338806).
Neuroprotection in the early stages of bipolar disorder
Low doses of lithium have been reported to counteract hippocampal microstructural and metabolic changes, which correlated with the improvement of symptoms in individuals at ultra-high risk for psychosis (Reference Berger, Wood and Dell'olioBerger 2008; Reference McGorry, Yung and PantelisMcGorry 2009a). This would be consistent with its effects on pathways involved in neuronal plasticity and integrity, particularly through upregulation of the neuroprotective protein Bcl-2 and BDNF (brain-derived neurotrophic factor) genes and inhibition of pro-apoptosis glucose synthase kinase-3 signalling pathways (Reference Zarate, Singha and ManjiZarate 2006; Reference Schloesser, Huang and KleinSchloesser 2008). In preclinical studies, lithium promotes neurogensis, consistent with evidence from clinical studies that it may be associated with the preservation of brain volume in key limbic and paralimbic regions implicated in bipolar disorder (Reference Sassi, Brambilla and HatchSassi 2004; Reference Yucel, Taylor and McKinnonYucel 2008). Reference Moore, Cortese and GlitzMoore and colleagues (2009) reported that in patients with multi-episode bipolar disorder the neurotrophic changes induced by lithium were associated with clinical response. Quetiapine (Reference Atmaca, Ozdemir and CetinkayaAtmaca 2007) and valproate (Reference Schloesser, Huang and KleinSchloesser 2008) may also have neuroprotective potential, although the evidence for this is relatively limited.
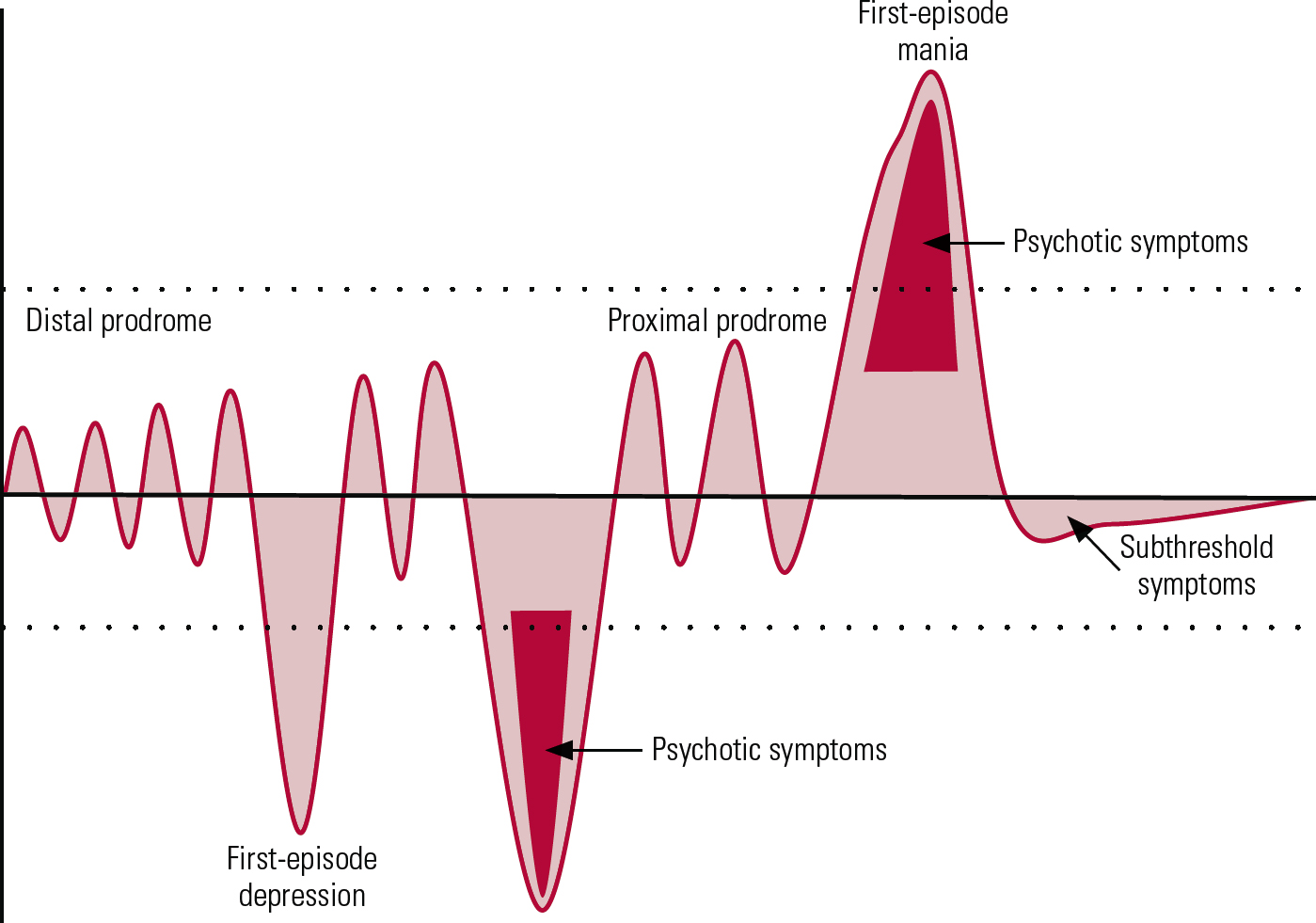
FIG 1 Simplified representation of the early stages of bipolar disorder. This figure does not include all clinical subgroups and presentations of the disorder. The shaded areas represent mood changes in relation to the euthymic state (black horizontal line) over a period of years spanning from teenage to early adulthood. The dotted lines indicate the current thresholds for diagnosis of manic and depressive episodes.
The challenge of recognising a depressive onset in bipolar disorder
The majority of patients with bipolar disorder initially present with a depressive episode (Fig. 1). Differentiating an episode of unipolar disorder from an episode of bipolar disorder (when there is no history of mania or hypomania) remains a challenge, despite substantial research efforts (Reference Forty, Smith and JonesForty 2008). Although not pathognomonic, a number of features are more commonly seen in bipolar depression than in unipolar depression (Box 4) (Reference Forty, Smith and JonesForty 2008; Reference Mitchell, Goodwin and JohnsonMitchell 2008). They assist the clinician in a probabilistic approach to considering bipolarity rather than helping to form a definite diagnostic tool.
BOX 4 Features indicative of bipolarity in depressive episodes
-
• Family history of bipolar disorder
-
• Nature of the onset:
abrupt onset and offset of episode
antidepressant-induced mania, hypomania or mixed states
younger age at onset of major depression
postnatal onset
-
• Symptom features:
psychomotor retardation/agitation
atypical features such as hypersomnolence, hyperphagia, leaden paralysis
psychotic features
melancholia
pathological guilt
lability of mood
irritability
mixed depression (manic features during depressive episode)
-
• Other features:
comorbid substance misuse
seasonality
brief episodes of depression (<3 months)
antidepressant wear-off (rapid emergence of depressive symptoms after remission while on antidepressants)
There have been recent attempts to differentiate bipolar disorder depression from major depressive disorder by neuroimaging and neurocognitive studies. In a review of 140 imaging studies, Reference Konarski, McIntyre and KennedyKonarski et al (2008) reported enlarged striatal and amygdala volumes in multi-episode bipolar disorder compared with major depressive disorder. In addition, in a preliminary functional magnetic resonance imaging study, Reference Almeida, Versace and HasselAlmeida and colleagues (2010) reported elevated amygdala activation to sad facial expressions in patients with multi-episode bipolar disorder depression compared with patients with major depressive disorder. In a study comparing unmedicated patients with bipolar disorder (depressed state) with healthy controls (Reference Roiser, Cannon and GandhiRoiser 2009), patients showed deficits mostly in emotion-dependent or ‘hot’ cognitive processing, rather than in emotion-independent or ‘cold’ cognitive processing. The deficits in the patients were apparent on tests involving reward processing, short-term memory storage and sensitivity to negative feedback. Reference Taylor Tavares, Clark and CannonTaylor Tavares et al (2007) reported a broader range of executive impairments in patients with major depressive disorder than in patients with bipolar II depression. Analogous studies in the early stages of bipolar disorder have yet to be conducted.
A number of screening tools are available that may aid clinicians when faced with making a diagnosis in a young patient presenting with depression. These include self-report tools such as the Mood Disorder Questionnaire (Reference Hirschfeld, Williams and SpitzerHirschfeld 2000), the Bipolar Spectrum Diagnostic Scale (Reference Ghaemi, Miller and BervGhaemi 2005) and the 32-item Hypomania Checklist (HCL-32; Reference Angst, Adolfsson and BenazziAngst 2005). In multi-episode bipolar disorder, a score of 20 or more on the HCL-32 yielded a sensitivity of 68% and specificity of 83% in distinguishing between bipolar disorder depression and major depressive disorder (Reference Forty, Smith and JonesForty 2009). These instruments represent a potentially useful adjunct to conventional clinical assessment. Clinical work in individuals at high risk of schizophrenia has been facilitated by the introduction of specialised instruments for the assessment of prodromal symptoms (Reference McGorry, Nelson and AmmingerMcGorry 2009b).
Treatment challenges in the early depressive episodes of bipolar disorder
Although there is a need for more reliable measures to identify bipolarity in a first episode presenting with depression (with no history of mania/ hypomania), little is known about the best course of treatment in such situations. The effects of antidepressants, mood stabilisers or psychological therapies used alone or in combination on the short- and long-term outcome in patients with this presentation is unclear. In a small-sample randomised study comparing paroxetine with a combination of paroxetine plus divalproex sodium in youths with depression at high genetic risk of bipolar disorder, Reference Findling, Lingler and RowlesFindling et al (2008) reported neither to be particularly effective in the long-term management of depressive symptoms.
For depression in patients with an established diagnosis of bipolar disorder, the latest guidelines (Reference GoodwinGoodwin 2009) suggest the use of quetiapine for early treatment effect. As quetiapine has unique antipsychotic and antidepressant properties (Reference Calabrese, Keck and MacfaddenCalabrese 2005), it is particularly useful for depressive episodes with psychosis. Lamotrigine is also recommended by the guidelines for initial treatment.
In patients with a history of mania, the guidelines (Reference GoodwinGoodwin 2009) warn against the use of antidepressant monotherapy and advise on combining antidepressants with antimanic agents, owing to increased risk of switching to mania. Tricyclic antidepressants and dual-acting antidepressants such as venlafaxine carry more risk of switching to mania than selective serotonin reuptake inhibitors. When antidepressants are used, it is recommended that they be tapered and discontinued as soon as remission is achieved (Reference GoodwinGoodwin 2009).
Use of psychological treatments such as interpersonal therapy, cognitive–behavioural therapy (CBT) or family-focused therapy can shorten acute depressive episodes (Reference GoodwinGoodwin 2009). Maintenance treatment in the early stages of bipolar disorder is discussed later in this article.
Treatment challenges in patients with a manic onset
Prognosis in the early stages of bipolar disorder
Accumulating evidence has challenged the notion that, compared with schizophrenia, bipolar disorder is a more benign illness with a relatively good prognosis. Following the first manic episode, of syndromal recovery is indeed high, with 84–90% patients achieving remission in 6 months (Reference Tohen, Hennen and ZarateTohen 2000; Reference Conus, Cotton and Abdel-BakiConus 2006). However, nearly 15% patients may cycle into depression without recovering from the initial manic episode (Reference Zarate, Tohen and FletcherZarate 2001), especially if they had a mixed affective picture at presentation. Even when syndromal remission is achieved, up to 40% of patients report depressive and anxiety symptoms at 6 months after remission (Reference Conus, Cotton and Abdel-BakiConus 2006). Furthermore, 40–50% of patients experience a recurrence within a year of disease onset, with time to a mood episode ranging from 6 to 8 months (Reference Tohen, Zarate and HennenTohen 2003; Reference Yatham, Kauer-Sant'Anna and BondYatham 2009). In general, following a first manic episode, depressive episodes dominate (Box 5). Inter-episode intervals are shorter for depressive episodes and their recurrence rate is higher than for manic episodes (Reference Yatham, Kauer-Sant'Anna and BondYatham 2009). Medication non-adherence during the treatment for first episode of mania ranged from 37 to 65%, which is considerably higher than that in patients who have had multiple episodes (Reference Craig, Grossman and MojtabaiCraig 2004; Reference Yatham, Kauer-Sant'Anna and BondYatham 2009).
BOX 5 Factors that may be associated with increased risk of relapse following first-episode mania
Manic relapses
-
• Substance misuse
-
• Initial manic presentation, as opposed to mixed state
-
• Early age at onset
Depressive relapses
-
• Initial mixed v. manic presentation
-
• Substance misuse
-
• Higher occupational status
-
• Higher initial depression scores
-
• Early age at onset
The concept of recovery in bipolar disorder goes beyond symptomatic remission, and includes patients’ function in their personal and social roles. In bipolar disorder, functional recovery is often poor, even after the first episode, with only 35% of patients recovering functionally by 6 months (Reference Conus, Cotton and Abdel-BakiConus 2006) and 43% by 2 years (Reference Tohen, Zarate and HennenTohen 2003). Factors associated with poor functional recovery include younger age, substance misuse and presence of depressive symptoms. As in the case of patients with multi-episode bipolar disorder, even subsyndromal depressive symptoms contribute to functional impairment (Reference Kauer-Sant'Anna, Bond and LamKauer-Sant’Anna 2009) following the first episode of mania.
The risk of attempted and completed suicide is of particular concern in the early stages of bipolar disorder. For example, in a prospective study, Reference Khalsa, Salvatore and HennenKhalsa (2008) reported 39 suicidal acts in 4 years in a cohort of 216 individuals. Of these, 87% occurred in the first year following disorder onset. An additional consideration is the high prevalence of comorbid disorders. Prevalence rates of substance misuse in this group range from 30 to 60%. In a preliminary report on 4-year follow-up of patients with first-episode bipolar I disorder, Reference Baethge, Hennen and KhalsaBaethge and colleagues (2008) reported that cannabis use selectively and strongly preceded and coincided with mania/hypomania, while a similar association was found between alcohol and depressive recurrences. Additionally, substance misuse is a key predictor of non-adherence to treatment (Reference Yatham, Kauer-Sant'Anna and BondYatham 2009).
Treatment of the first manic episode and subsequently
Treatment of first-episode mania
At present it is not clear whether special provisions or considerations should apply for the treatment of the early stages of bipolar disorder that are distinct from those for multi-episode bipolar disorder. Current guidelines have no specific recommendations (American Psychiatric Association 2002; Reference HirschfeldHirschfeld 2005; Scottish Intercollegiate Guidelines Network 2005; National Institute for Health and Clinical Excellence 2006; Reference GoodwinGoodwin 2009). Empirical evidence suggests that currently available antipsychotics have antimanic properties (Reference Perlis, Welge and VornikPerlis 2006). As in schizophrenia (Reference Gafoor, Landau and CraigGafoor 2010), it is unclear whether some antipsychotics are more efficacious or better tolerated in the early stages of the illness than others. In a small retrospective medical record study of first-episode acute mania with psychosis, olanzapine was associated with better symptom remission and shorter time to remission than risperidone (Reference Lambert, Conus and SchimmelmannLambert 2005). Results are awaited from a recently concluded trial comparing a combination of lithium plus chlorpromazine with lithium plus olanzapine in first-episode mania with psychotic features (http://clinicaltrials.gov/ct2/show/NCT00202293). A recently initiated clinical trial comparing quetiapine and lithium is examining functional and neurochemical brain changes in first-episode bipolar mania (http://clinicaltrials.gov/ct2/show/NCT00609193).
As patients with bipolar disorder may be more vulnerable than those with schizophrenia to developing antipsychotic-induced movement disorders (Reference Gao, Kemp and GanocyGao 2008), careful medication selection and dosing are indicated in the early stages of illness. The effective dose of antipsychotics is significantly lower for first-episode schizophrenia than for later episodes of chronic schizophrenia, and even lower for prodromal symptoms (Reference Gafoor, Landau and CraigGafoor 2010). It is not clear whether the same applies to antipsychotic use in the early phases of bipolar disorder.
In a naturalistic setting, patients with affective psychosis received lower doses of antipsychotics at discharge and at 6-month follow-up than those with non-affective psychosis, despite no differences in the peak treatment dose (Reference Zarate and TohenZarate 2000). In contrast to antipsychotics, the doses of mood stabilisers required in first-episode mania do not appear to be different from those needed in an established bipolar illness.
Maintenance therapy
As in multi-episode bipolar disorder, key issues in the management of first-episode bipolar mania concern the prevention of relapses and the reduction of residual symptoms. The NICE guidelines suggest that maintenance therapy in patients with bipolar I disorder should be considered after the second episode, or after a manic episode if it involved significant risk and adverse consequences (National Institute for Health and Clinical Excellence 2006). Therefore in the majority of patients, provisions for their long-term pharmacological treatment should be made at the early stages of the illness. The medications that are the focus of current studies on the treatment of this stage of bipolar disorder are lithium, quetiapine and valproate.
Lithium
A first-episode mania study in a naturalistic setting reported a trend towards earlier syndromal recovery and a reduced risk of relapse of either polarity in patients treated with lithium, compared with valproate and antipsychotics (Reference Tohen, Zarate and HennenTohen 2003). Lithium may also reduce the risk of suicide, self-harm and death from all causes in patients with mood disorders (Reference Cipriani, Pretty and HawtonCipriani 2005). Lithium treatment appears to have only few and minor negative effects on cognition, as reported in a meta-analysis (Reference Wingo, Wingo and HarveyWingo 2009). Safety and tolerability of long-term lithium administration is well established in young patients, although its use in young women of reproductive age requires additional monitoring, as described in current guidelines (Scottish Intercollegiate Guidelines Network 2005; National Institute for Health and Clinical Excellence 2006). The relatively high rate of medication non-adherence in the early stages of bipolar disorder may be particularly relevant for lithium, as sudden discontinuation could induce rebound (Reference MajMaj 2003).
Quetiapine
In addition to its antimanic properties, quetiapine also has antidepressant properties (Reference Calabrese, Keck and MacfaddenCalabrese 2005). Quetiapine treatment is shown to be effective across a broad range of mood symptoms and the drug is well tolerated in multi-episode bipolar disorder (Reference Vieta, Mullen and BrecherVieta 2005). In a small open-label study, Reference Duffy, Milin and GrofDuffy et al (2009b) reported that quetiapine was also effective and well tolerated in a relatively young population with bipolar disorder with intact neurocognitive function. A recently initiated study is comparing quetiapine with lithium on neuroanatomical, neurochemical, neurocognitive and prophylactic effects after first-episode mania (www.psychiatry.unimelb.edu.au/centres-units/mnc/projects/mania.html).
Valproate
Valproate maintenance has been associated with fewer depressive relapses in multi-episode bipolar disorder than lithium maintenance (Reference Smith, Cornelius and WarnockSmith 2007). Although the overall effect of valproate as maintenance therapy in multi-episode bipolar disorder is less compelling (Reference Vieta and RosaVieta 2007), it is not clear what effect it has in the maintenance phase after the first episode. Also, valproate’s teratogenic potential limits its use in female patients in the early stages of bipolar disorder.
Psychoeducation and psychological interventions
The high rate of medication non-adherence in the early stages of bipolar disorder emphasises the need to combine pharmacological treatment with psychoeducation. Psychoeducation is particularly effective in improving clinical outcomes by reducing non-adherence in patients with multi-episode bipolar disorder (Reference Vieta and ColomVieta 2004). Family psychoeducation can be more effective in the early stages of bipolar disorder than in the later stages, with improvement in time to recurrence (Reference Reinares, Colom and RosaReinares 2009). Comorbid substance misuse also requires management from the early stages (Reference Baethge, Hennen and KhalsaBaethge 2008). Cognitive–behavioural therapy may be helpful, with a focus on stress management and relapse prevention. Reference Gleeson, Cotton and Alvarez-JimenezGleeson et al (2009) conducted a randomised controlled trial of multimodal individual and family CBT for relapse prevention in a first-episode psychosis group, which showed promising results in comparison with standard case management. Reference Jones and Burrell-HodgsonJones & Burrell-Hodgson (2008) reported the use of manualised CBT, with results showing improvement in circadian activity, prodromal coping skills and cognitive style in patients after their first episode of bipolar disorder.
Directions for the future
There is clearly a need for more research on the characteristics of the early stages of bipolar disorder and on the development of treatments that can be implemented in the early phases. There is also a need for the development of validated rating instruments for better identification of the prodromal phase, and studies to evaluate the utility of interventions aimed at preventing transition to a full-blown disorder from a high-risk state. Specialised service organisation and provisions may improve the early detection of bipolar disorder and facilitate research into the early intervention in bipolar disorder, as they have done for schizophrenia. Analogous services and interventions need to be evaluated for their impact on the outcome of bipolar disorder. Some key diagnostic and treatment priorities for early intervention services for bipolar disorder are suggested in Box 6.
BOX 6 Priorities in the treatment of the early stages of bipolar disorder
-
• Enhancement of early detection and diagnosis
-
• Mood stabilisation (including treatment of subsyndromal mood symptoms)
-
• Neuroprotection
-
• Preservation of neurocognition
-
• Management of substance misuse and other comorbidities
-
• Improvement of medication adherence
-
• Management of risk
-
• Devising and administering appropriate pharmacological and psychological interventions
-
• Improvement in functional/educational/vocational outcomes
-
• Maintaining an optimistic treatment setting
MCQs
Select the single best option for each question stem
-
1 In bipolar disorder:
-
a peak age at onset is after 40 years
-
b the illness runs a chronic course in the majority
-
c the illness is usually diagnosed early
-
d delay in diagnosis is not associated with worse outcome
-
e a manic picture dominates the overall clinical picture.
-
-
2 In the prodromal phase and high-risk groups:
-
a the majority of patients with bipolar disorder have an affected first-degree relative
-
b prodromal symptoms have high sensitivity
-
c lithium may have a protective role
-
d psychological therapies have been shown to be ineffective
-
e substance misuse does not influence the course.
-
-
3 Regarding the first mood episode in bipolar disorder:
-
a the first episode is usually manic
-
b depressive first episodes are easy to identify as part of bipolar disorder
-
c certain clinical features may help to suspect bipolarity in patients with depression
-
d psychosis is rare in first-episode mania
-
e patients with first-episode mania always have manic relapses.
-
-
4 Prognosis following first-episode mania:
-
a the majority attain functional recovery quickly
-
b substance misuse is associated with poor medication adherence
-
c suicidal risk is less in the first year following the first episode
-
d less than 10% will have a recurrence
-
e subsyndromal depression does not affect functional outcome.
-
-
5 Treatment of first-episode mania:
-
a maintenance therapy is needed in the majority
-
b antipsychotics have no role
-
c poor medication adherence has no effect on lithium treatment
-
d psychoeducation is ineffective
-
e quetiapine has no neuroprotective effect.
-
MCQ answers
| 1 | b | 2 | c | 3 | c | 4 | b | 5 | a |



eLetters
No eLetters have been published for this article.