No CrossRef data available.
Article contents
What are the changes in mothers’ diets after the birth of a child: results from the NutriNet-Santé cohort
Published online by Cambridge University Press: 18 October 2024
Abstract
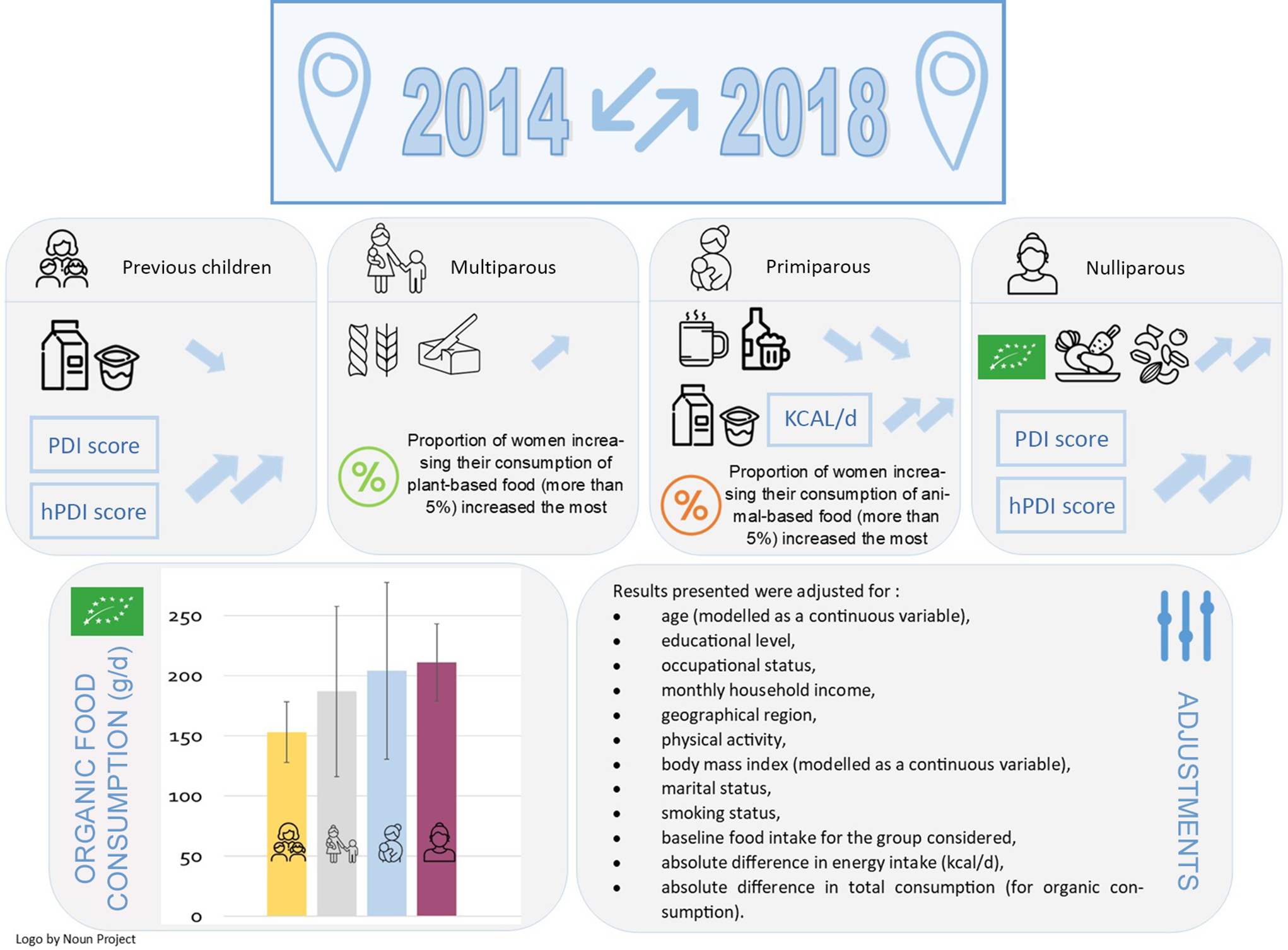
Childbirth is a major life-changing event, this period is an opportunity to improve eating habits. The aim of this longitudinal study was to identify and characterise dietary changes in women according to their parity status. Dietary intake data from 4194 women of childbearing age included in the NutriNet-Santé cohort were derived using a FFQ, administered in 2014 and 2018, distinguishing between organic and conventional food consumption. Women were classified into four groups: ‘previous children’, ‘multiparous’, ‘primiparous’ and ‘nulliparous’. Multi-adjusted ANCOVA models were used to estimate the changes according to the parity group. Changes in food consumption towards a more plant-based, healthier and organic diet were observed in all four groups of women, although to various degrees. In multivariable models, ‘Nulliparous’ women showed a greater improvement in terms of ‘sustainable’ food consumption than ‘previous children’ women. ‘Primiparous’ women significantly increased their energy intake (+349 (269–429) kcal/d) and their consumption of dairy products (+30 (3–56) g/d), and they significantly decreased their consumption of alcohol (–23 (–32–15) g/d), coffee and tea (–107 (–155–60) g/d). Regarding organic food, ‘nulliparous’ women increased their consumption more than ‘previous children’ and ‘primiparous’ women were those who were most frequently in the top quintile of organic food increase. Although there were dietary changes in all groups of women according to their parity, childless women have a shift moving towards a more sustainable diet. Women who had a first child reduced their alcohol and caffeine consumption.
- Type
- Research Article
- Information
- Copyright
- © The Author(s), 2024. Published by Cambridge University Press on behalf of The Nutrition Society



