Learning Points
Addiction is a highly prevalent and dangerous psychiatric illness and brain disease. It can result in massive harm to an individual’s physical and mental health, their occupational and social function, their families, and social networks.
Addiction psychiatry is a healthcare field led by physicians who are uniquely cross-trained, and board-certified in the neuroscience, diagnosis and treatment of both mental illness and addiction. Addiction psychiatrists are expertly qualified to treat these diseases whether they are encountered as stand-alone disorders or – as they most commonly occur – as complex combinations of comorbid illnesses (i.e., “dual diagnosis”).
Addiction is the leading root cause of morbidity and mortality in the United States. This is because, when untreated, addiction leads to so many other injuries and disorders of the mind and body that are incredibly destructive and imminently lethal.
Stigma has limited the healthcare system from appropriately recognizing, preventing, and treating addiction as a disease, even as it squarely fits five core criteria for what defines a disease. Addiction is a disease that (1) has a massive yet uneven public health impact; (2) is characterized by a well-defined symptomatology; (3) involves specific neuroanatomical substrates and a complex pathophysiology; (4) is exacerbated by biologically active genetic, environmental, and neurodevelopmental risk factors; and (5) is measurable, reduceable, and remittable through the expert use of reliable and effective diagnostic tools and biologically active treatment strategies.
Addiction is disproportionally highly prevalent in people with mental illness and those exposed to addictive drugs in adolescence – all as a reflection of its underlying neurobiology. However, there are many biologically active disease risk factors for addiction and most people carry some risk of becoming addicted. Some of the most well-educated, intelligent, and financially advantaged people in our society (e.g., physicians) are susceptible to the disease.
Introduction
Addiction is a brain disease that afflicts about one in five adults and is a leading root cause of injuries, illnesses, and mortality in the United States. In modern society, addiction, often comorbid with mental illness, is the leading killer of people who don’t die in old age. This stark reality is not well appreciated, or often taught, in medical schools. Stigma, a widely held social attitude of judgment, inferiority, and disgrace aimed toward people with certain attributes or diseases, is frequently leveraged against people with addictive disorders and mental illness. Lack of treatment infrastructure, paucity of well-trained professional workforce, and insufficient insurance coverage for behavioral health disorders all play a role in the underrecognition of addictive disorders (and its harmful relegation to the criminal justice system), adversely contributing to its morbidity and mortality. Diagnostic indications for medical or surgical hospitalizations and causes of death are often attributed to proximal causes (e.g., cardiovascular disease, malignant carcinoma, cerebrovascular disease, infections, accidents, and so on) rather than to the chronic underlying brain-based behavioral disorders that often lead to these conditions, such as addictions to nicotine, stimulants, alcohol, and opioids. However, recent public health calamities, like the iatrogenic (meaning disease caused by the improper/harmful delivery of health care) epidemic of opioid addiction, have increased awareness within the medical community that addiction diagnosis and treatment must become a high priority in mainstream medical and psychiatric care.
A longstanding lack of understanding about the scope and nature of addiction as a disease (covered in Chapters 1 and 2), its neurobiology (Chapter 3), its connection with mental illness (Chapter 4) and its treatability (Chapter 5) – even within medical and psychiatric education – has contributed to the healthcare system’s lackluster tradition in taking responsibility for identifying, preventing (or avoiding causing), and treating it to the extent we are capable of. The primary goal of this book is to provide the medical/psychiatric trainee and brain-behavioral health scientist with a relatively concise yet in-depth understanding of what addiction is, in all its five core dimensions as a disease process. In covering these illness dimensions, this book serves as an introduction to the field of addiction psychiatry. As such, it aims to integrate scientific and clinical information into one coherent framework of knowledge that will serve as a foundation on which a larger and more impactful addiction psychiatry workforce, treatment, training, and research infrastructure can be built as a core domain of psychiatry and public health.
What Is Addiction Psychiatry?
Addiction psychiatry, like its closely allied field addiction medicine, is focused on the diagnosis and treatment of addictions and various related substance use disorders (e.g., withdrawal syndromes). However, addiction psychiatry is uniquely and expertly focused on the neuroscience and treatment of the full spectrum of both mental health and addiction disorders, whether they occur as standalone or comorbid conditions. As such, addiction psychiatry is the only American Board of Medical Specialties (ABMS)-defined field of medicine that requires formal training in both psychiatry and addictionology, which in the US is accomplished via (a) the completion of a four-year general psychiatry residency program and (b) a year of addiction psychiatry fellowship training. In this way, addiction psychiatry is actually a broader and deeper scope of expertise in comparison to what general psychiatry training alone provides, allowing addiction psychiatrists to treat a much wider array of patients and comorbid diagnostic conditions, with higher levels of training spanning neuroscience, diagnostics, psychotherapeutics, and pharmacology. It is thus perhaps a misnomer to regard addiction psychiatry as a subspecialty of psychiatry when the training actually amplifies and broadens one’s diagnostic and treatment capability. Addiction psychiatry can be understood as advanced training in general psychiatry, with an emphasis on enhancing the expert management of patients with complex combinations of multiple addictions and mental illnesses, and for leading multidisciplinary treatment teams that make this care more impactful. Because patients with complex comorbidities of mental illness and addictions (i.e., “dual-diagnosis” patients) are so common and mainstream (due to biological reasons, reflecting fundamental design features of the mammalian brain described in Chapter 4), the unmet need for more addiction psychiatrists (who can integrate our highly fragmented and siloed systems of addiction versus mental health care) is immense.
Addiction medicine fellowship training and certification, in contrast to addiction psychiatry fellowship training, accepts both psychiatrists and nonpsychiatrists (e.g., family medicine doctors, neurologists, internists, surgeons, emergency medicine doctors, anesthesiologists, Ob-Gyn doctors, and so on). Also, unlike addiction psychiatry, addiction medicine certification does not require formal fellowship training (only a certification exam and letters of support). However, in the coming years, addiction medicine will likely transition to the more formal and rigorous training standards of addiction psychiatry certification, requiring a year of formal fellowship training as a subspecialty of physical medicine and rehabilitation. In general, psychiatrists who go on to train in either addiction psychiatry or addiction medicine fellowships are similarly equipped to provide integrated addiction and mental health care (i.e., integrated dual-diagnosis care, as an addiction psychiatrist), whereas nonpsychiatrists who pursue addiction medicine provide addiction treatment for patients in a way that is more limited in terms of providing psychiatric expertise or integration with mental health, yet integrated with their particular lines of medical practice (e.g., the Ob-Gyn physician who prescribes buprenorphine to her pregnant patients).
The unique expertise of addiction psychiatrists in providing care and leading teams that fully integrate mental health and addiction treatment is an important capability because (a) the majority of patients with significant mental illness have addiction comorbidity of some kind, and (b) addiction diseases routinely produce or worsen mental illness. Split care, where patients may be seeing one doctor for addiction treatment and another for psychiatric care in two different systems, at two different locations, is not as effective or efficient (for either the healthcare system or patients) and should be avoided if possible. As we will describe in Chapter 5, addiction psychiatrists are uniquely trained to provide care that avoids this split by providing and leading integrated dual-diagnosis care. This kind of integrated care not only allows for more coherent treatment planning, but it better supports longitudinal continuity of care and stronger therapeutic relationships; the addiction psychiatrist is able to support recovery even as patients progress through different phases of mental illness and/or addiction symptomatology.
For primary care doctors and other nonpsychiatrists attempting to practice behavioral healthcare in the form of addiction medicine, there are several boundary hazards and pitfalls that exist that psychiatrists, by nature of their practices and their training, are better equipped to avoid. These hazards include performing invasive physical examinations on patients who have significant histories of sexual-emotional trauma or having personal relationships (friendships or romantic) outside of the professional practice-based relationship with patients. Psychiatrists are trained in boundary awareness, to never have personal emotional or sexual relationships with patients they are treating (or have treated in the past), and they generally do not perform examinations of private/erogenous body zones. These guard rails serve to protect patients and psychiatrists from nontherapeutic, harmful, or exploitative directions that treatment can take in the context of (1) establishing quite intimate therapeutic alliances and familiarity with the mental life and emotions of patients; (2) the prescribing of mind-altering, controlled drugs; (3) the presence of certain mental illnesses that can make certain patients extremely vulnerable (e.g., to eroticized interactions); and (4) the considerable power differential that often exists between psychiatrists/therapists and their patients.
In addition to core training in maintaining boundary awareness, four years of general psychiatry training (as a prerequisite for pursuing addiction psychiatry training) also encompasses education and training in psychiatric neuroscience (e.g., neuroanatomy and cognitive/affective neuroscience), the diagnosis and management of personality disorders, and the science, theory, and delivery of various psychotherapies and pharmacotherapies. Personality disorder symptoms, which are not unusual in patients with addictions (and can be amplified by co-occurring addictions) can produce chaotic effects in a general medical practice, in doctor–patient relationships, and for physician’s decision-making, especially for doctors who are untrained in diagnosing and managing them. At the same time, understanding what psychotherapy is, how to deliver it, and how to supervise other professionals who are delivering it, are important skills for effective addiction treatment. Psychiatrists are the only physicians that are required to have formal training in psychotherapy. For optimal results, psychotherapies should often be integrated with medication management in the treatment of addictions and comorbid mental illness. Thus, psychiatrists entering addiction psychiatry have a significant foundational advantage in being already trained in key skill sets needed for expert practice in addictionology, whereas nonpsychiatrists entering addiction medicine must attempt to fill these training gaps in their one-year fellowship, or in other ways outside of what psychiatric residency training provides.
Given the considerable overlap between the allied fields of addiction psychiatry and addiction medicine, this book can serve as a useful primer for both fields, albeit through the lens of addiction psychiatry which places more emphasis on (i) the translational neuroscience of addiction (i.e., explaining how the brain science of addiction generates clinical–human-level phenomena); the (ii) integrated neurobiology of mental illness and addiction (i.e., explaining how mental illness and addiction are interconnected biologically and clinically); and (iii) the deployments of integrated treatments (e.g., using combinations of both psychotherapies and medications) to drive recovery and disease remission.
Addiction Is a Brain Disease
A usual stumbling block in understanding addiction for the public and even medical professionals is the challenge in appreciating and accepting its true nature as a disease. This lack of understanding is a major contributor to stigma, which infiltrates even the healthcare system, causing it to be uninterested, deficient, or incompetent in adequately diagnosing and treating addiction. Stigma, occurring in the form of denial that addiction is a real disease, can even contribute to a tendency of the healthcare system to sometimes cause it, via negligent or exploitative overprescribing of controlled drugs. Thus, in explaining addiction as a genuine biomedical condition that needs expert, science-based treatment (and not as a crime to be punished, or as a moral or religious failure of “bad apple patients”), it is important to discuss how it clearly fulfills our medical definitions and criteria for what constitutes a disease.
Taking this approach, this book will focus on addiction in terms of five core attributes, or criteria that modern medicine uses (and medical students learn) to define any given entity as a disease. A disease is an entity of biomedical attention that: (1) impacts a population of patients and has associated morbidity and mortality; (2) is associated with reliable sets of signs, symptoms, and clinical features; (3) is produced by an underlying biology of altered anatomical structure and function; (4) is associated with a range of biologically active risk factors; and (5) can be reliably diagnosed and treated by interventions that target the involved biological systems. As we introduce the reader to the field and knowledge of addiction psychiatry, this five-part definition will guide us in the content organization for the chapters of this book:
Chapter 1: Population Impact – Epidemiology. Addiction is a highly prevalent brain disease that produces extensive damage for individuals and society.
Chapter 2: Specific Symptoms Sets – Clinical Phenomenology. Addiction symptoms represent a disease of motivation that is comprehensively devastating to physical and mental health, yet strikingly similar across addictions to very different drug types.
Chapter 3: A Disorder of Anatomical Structure and Function – Neurobiology. Brain circuits that generate and adapt motivation are subject to progressive pathological changes in addictive disease as demonstrated across humans and other animal species.
Chapter 4: Biological Risk Amplification – Disease Vulnerability. Addiction disease risk is involuntary (not a simple matter of a person’s choice) and is unevenly distributed in the population; it is neurobiologically associated with mental illness, adolescent neurodevelopment, and various related genetic and environmental factors.
Chapter 5: Diagnosis and Treatment – Disease Tracking, Reduction, and Remission. Addiction psychiatry uses an array of subjective and objective diagnostic tools and science-based treatment strategies to comprehensively reduce or remit additions and mental illness comorbidities.
Core Definition of Addiction
At the crux of what the Western medical tradition says a disease should entail is that it involves abnormal anatomy and functions of biological/physical (body organ) substrates. Addiction disease most directly involves pathology in brain systems that generate and control the functions of motivation and free will. It is perhaps because these faculties are so wrapped up into who we are and what we are capable of as human beings – and our thinking about these faculties are so tied into philosophical and religious traditions – that we have a hard time understanding them from a biomedical/scientific point of view. But to understand addiction as a disease, we must understand motivation and free will from a biomedical point of view. So, we start with these two basic definitions:
Motivation is the brain-generated drive and sequencing of a series of goal-directed actions.
Free will is the brain’s capacity for choosing specific actions from an array of options.
Although motivation and free will are mediated by neurophysiological processes occurring in the brain, these concepts are more abstract and difficult to measure compared to more concretely testable abilities or functions like gait, memory, strength, urinary output, or glucose levels. For instance, someone can experience motivation toward taking several different actions all at once that is not visible to an outside observer. The observer is also not quite able to see a motivational pattern until a whole sequence of actions are acted out. At different junctures in the sequence, free will may intervene at different extents to determine the whole sequence. Where addiction comes in as a diseases process is that it represents a pathology of compulsive motivation that overrides other healthy motivations (choices of behavioral programs), thereby degrading the faculty of free will. Human cultures have long evaluated motivation and free will through a lens of morality. However, those with addiction are not inferior to the unaffected. Addiction is not a condition where someone has an immoral or criminal free will. Rather, it is a disease process that progressively destroys free will. Mastering addiction neurobiology requires us to expand and evolve our understanding of what motivation and free will are as more than just philosophical, psychological or moral concepts, but as neurobiologically generated products. Objective criteria that relate to an individual’s pathological motivation (in addiction) helps guide medical–psychiatric assessment of diagnosis so that treatment can always begin from a place of professional nonjudgment, with stigma removed as much as possible. The Diagnostic and Statistical Manual (DSM) for psychiatric disorders provides the most definitive current consensus of clinical criteria needed to make diagnoses of addiction (see Chapter 2). But as a foundation for helping us link the clinical phenomenology of addiction with the neuroscience of the disease, it is helpful to start with a very simple and yet accurate definition of addiction that boils down the DSM criteria as follows:
As we will discuss in Chapters 2 and 3, addictions are substance use disorders (SUDs) that are very different in symptoms and biology from intoxication and withdrawal states, which are also included under the umbrella term substance use disorders (SUDs). Intoxication and withdrawal involve the relatively acute, pharmacological and toxicological consequences of drugs on the brain that include transient sensory, cognitive, motor, and/or emotional effects. In contrast, addiction involves a chronic change in motivation caused by repeated drug use, which progressively diminishes the capacity for healthy decision-making and adaptive motivation. Behavioral addictions (or “impulse control disorders,” which addiction psychiatrists are also focused on treating) can also occur, involving reinforcers that are not strictly invoked by externally supplied chemicals, such as pathological gambling, binge eating, compulsive shopping, shoplifting, video gaming/technology use, or pathologically impulsive–compulsive sexual activity. These impulse control disorders are often highly comorbid with drug addictions (and other mental illnesses) and share many of the clinical features and neuroanatomy as drug addictions.
Health Impact of Addiction
The morbidity (sickness and injury causing consequences of disease) and mortality (lethality of disease) of addiction is massive in modern societies. In an influential 2004 paper that opened the eyes of the medical community to how big the untreated addictions and other behavioral conditions are in all-cause medical morbidity, Mokdad et al. (Reference Mokdad, Marks, Stroup and Gerberding2004) reported that the top three root causes of death in the United States are: (1) tobacco use; (2) poor diet/poor exercise; and (3) alcohol use. The medical mortality due to other illicit or iatrogenic addictions also ranked in the top 10. This accounting was made even before the iatrogenic opioid epidemic (c. 1995 to present), which by itself would become a leading cause of death in the US, had become fulminant.
To understand how addiction represents such a powerful cause of illness and pathways to premature death, one has to grasp how extensive, diverse, and potentially lethal the list is of secondary injuries, medical and psychiatric diseases that addictions can cause. A key to this understanding is an appreciation for how the chronic-toxicological nature of addiction is something that far outweighs the risks and damage of acute intoxication/withdrawal (e.g., that goes with initial use or any one episode of use). The compulsions of addiction result in years-long, incessant, heavy use that vastly increases the risk of death and disease via cumulative toxicological injury to multiple organ systems and repeated episodes of intoxication that drive injury-producing behaviors. Smoking one cigarette does not cause heart disease, chronic obstructive pulmonary disease (COPD), stroke, and cancer, but smoking one cigarette every few hours for many years almost certainly will. Similarly, chronic smoking greatly increases one’s cumulative chance of dying in a house fire far beyond what smoking a single cigarette will do.
The top 10 proximal causes of death in the US include the usual suspects as shown in Table 1.1. These causes accounted for about 74% of all mortality in 2016. The top five causes alone accounted for 62% of mortality. It is important to consider how these proximal causes of death, which at face value seem to have nothing to do with psychiatric/brain-based disorders, are largely attributable to or are caused by the use of addictive substances as root, or long-range causes of death that lead to these proximal-medical causes expressed at the end stage. For instance, consider the #1 cause of premature death in the United States: nicotine/tobacco addiction. Per a 2014 Surgeon General report, some 500,000 deaths a year in the United States are linked to tobacco use. This tobacco-related mortality, which kills about half of all people who die before they reach the average life expectancy, mainly results from chronic use that, initially at least, only minimally impedes function or represents a health threat. A strong addictive use pattern with nicotine often develops years before negative health consequences emerge. Table 1.2 shows estimates of how many deaths, produced by four of the top five common proximal causes of death shown in Table 1.1, are actually attributable to chronic tobacco use (i.e., nicotine addiction). Chronic tobacco use also greatly amplifies the organ damage effects of diabetes while also operating as a risk factor for dementia and the progression of chronic kidney disease. Again, while tobacco provides the toxic mixture of chemicals responsible for most of the negative health effects of smoking, it is nicotine (the key addictive chemical in tobacco) that is responsible for the chronic compulsive use that produces the cumulative multiorgan toxic exposure of tobacco. Chronic second-hand smoke (resulting from living with someone with nicotine addiction) also increases the risk of disease to those exposed, even if they are not directly smoking.
Table 1.1 Top 10 causes of death in the United States, 2016
| 1. Diseases of the heart | 6. Alzheimer’s disease |
| 2. Malignant neoplasms | 7. Diabetes mellitus |
| 3. Unintentional injuries (accidents) | 8. Influenza and pneumonia |
| 4. Chronic lower respiratory diseases | 9. Nephritis, nephrotic syndrome, and nephrosis |
| 5. Cerebrovascular diseases | 10. Intentional self-harm (suicides) |
Table 1.2 Estimated deaths attributable to smoking tobacco, 2005–2009
| Disease | Fraction of deaths attributable to tobacco (%) |
|---|---|
| Coronary heart disease and other diseases of the heart | 21.4 |
| Total cancer | 48.6 |
| Total pulmonary disease (includes COPD, emphysema, bronchitis, influenza, pneumonia) | 61.7 |
| Cerebrovascular disease | 11.3 |
| Diabetes mellitus | 12.7 |
Now, consider another hugely popular addictive drug (even among ancient humans, more than 10,000 years ago!): alcohol. Alcohol drinking results in about 90,000 deaths annually in the US. It is also a known risk factor for multiple proximal top causes of mortality, including cardiovascular disease, cerebrovascular disease, diabetes, and liver disease. Alcohol is also an established carcinogen, leading to a significant percentage of all cancer deaths involving multiple organ systems. This carcinogenicity probably occurs by several molecular mechanisms, including its metabolism to acetaldehyde, which interferes with DNA repair.
In addition to its chronic toxicological effects on multiple body organs, alcohol also produces profound acute and long-term effects directly on the brain, which are in turn associated with an incredibly wide array of behavioral and psychiatric illness pathways that lead to severe injuries and/or death. Alcohol intoxication is a leading cause of injuries and deaths by falls, fires, water (drownings), assaults and murders, and so on, and it is a leading cause of death by overdose either as a single agent or in mixture with other drugs. About a third of deaths from motor vehicle accidents (incidents included under “unintentional injury” – the #3 top cause of death in Table 1.1) are attributable to alcohol use. Alcohol also greatly amplifies the risk of completed suicide by both its acute and chronic psychiatric effects. While alcohol intoxicated, a person who might otherwise be only passively thinking about suicide may have that motive become disinhibited (i.e., increase the likelihood of being impulsively acted out). Also, with chronic use, alcohol contributes to the pathogenesis of several neuropsychiatric disorders like depression and dementia that can further amplify the long-term risk of death by accidents or suicide. Although substance use in general is associated with a 10–14× increased risk of suicide, addictions involving alcohol and opioids carry some of the highest risk, being associated with about a quarter to nearly half of all completed suicides.
The aforementioned discussion of nicotine and alcohol hasn’t even considered the burden of injuries, illness, and death caused by opioids and opioid addiction. Rates of chronic opioid use has increased by three- to four-fold in the general US population over the prior three decades, as triggered and spread by the iatrogenic opioid epidemic. By 2010, a person in the US was more likely to die from an opioid-involved overdose than from a motor vehicle accident or gunshot injury (National Safety Council, 2021). By 2020, drug overdoses, often involving combinations of opioids with alcohol and/or benzodiazepines, had become the leading cause of death for Americans under the age of 50. For the first time in modern history, the life expectancy of Americans began to drop (after a century of increases), largely due to “deaths of despair” (overdoses and suicide associated with untreated mental illness and addiction). By comparison, the last time a multiyear decrease in US life expectancy occurred was 1915–1918 in the aftermath of World War I and the H1N1 “Spanish flu” pandemic, which infected about one-third of the world’s population. Even COVID, which killed more than a million Americans from 2020 to 2022 (mostly dying over the age of 60), did not kill as many US citizens under the age of 50 as did drug overdoses and addiction. Even before a lethal outcome from opioid addiction, which may happen by any one of a very large number specific pathways besides overdose, opioid addiction can also produce or worsen a very wide range of secondary body organ diseases, injuries, and psychiatric consequences including but not limited to HIV–AIDs, endocarditis, viral hepatitis, liver cancer, sepsis, traumatic brain injury, depression, and posttraumatic stress disorder (PTSD).
So, in this brief overview of addiction’s health impact, we have considered just three substances (nicotine, alcohol, and opioids) in some detail, each of which independently represents a major root cause of many forms of injuries and secondary medical diseases that are all eventually quite lethal and expensive to treat medically and surgically. When considering these consequences as compounded further by the chronic misuse of an even wider array of addictive drugs (including cocaine, amphetamines, sedative-hypnotics, cannabinoids, inhalants, various designer drugs, and so on), it is readily appreciated how broad, deep, and frankly unparalleled addictions’ overall public health impact truly is in terms of the totality of human suffering and lives lost.
Economic Impact of Addiction
The National Institute on Drug Abuse (NIDA: the largest National Institute of Health (NIH) section that supports research on drug addictions) has estimated that based on data from various studies spanning the years 2007–2013, the economic impact of addictions involving tobacco, alcohol, illicit drugs, and prescription opioids was reaching beyond $820 billion annually due to lost worker productivity, related criminal-justice interventions, and increased healthcare utilization. As of 2020 and later, this economic burden is likely higher still – potentially near $1 trillion a year – which would account for about 5% of the United States annual gross domestic product (GDP). Opioids alone are thought to have cost a cumulative $1 trillion from 2001 to 2017 with the annual cost still increasing. At the same time, the cost of the “war on drugs” (the term given to US federal and state government efforts to reduce drug use and addiction through criminalization and mass incarceration) has reached beyond $1 trillion since the 1970s, while producing no measurable desirable results, and in fact corresponding to an increasing death toll due to addiction in parallel with increasing per-capita rates of mass incarceration.
Decreased labor force participation (which generally doesn’t count for loss of labor force due to early deaths from addiction or incarceration of addicted people) is one of the largest economic harms of drug addiction and reflects how debilitating addiction can be for individual functionality and society as a whole. Due to the widespread penetrance of and effects of addiction, particularly on young adult to middle-aged people, the workforce effects of addiction hit hardest precisely in those of prime working age (20s–40s). This depletes the ability of companies specializing in virtually all fields of services and production to hire and invest in new and long-term employees. In the example of opioid addiction, the chronic use of both prescribed and nonprescribed opioids is elevated several-fold among unemployed men of prime working age. Even those still in the workforce who take opioids have a higher likelihood of requiring sick days, having work absences, or utilizing workers’ compensation benefits. Loss or derailment of educational achievement due to addiction and extended removal or restrictions from access to employment due to criminal charges associated with addictions produce significant socioeconomic damages and worsening of educational and economic divides within the population. These trends may represent significant threats not only to economies but to the survival of democratic forms of government.
Demographic Scope and Subpopulations at Risk for Addiction
There have been hundreds of epidemiological studies of addiction and comorbid mental illnesses spanning both large and small population samples in the United States over the last 50 years. For the purposes of this chapter, we will draw mainly form the National Survey on Drug Use and Health (NSDUH) data, prepared by SAMHSA (Substance Abuse and Mental Health Services Administration, 2019), because (a) it provides fairly recent evidence (2018; national sample of n = 67,791) that generally agrees with trends identified elsewhere in the literature over recent decades; and (b) it also allows us to highlight some of the research design flaws that are present in this area of medical epidemiology. With that said, the reader should be aware that rates of addiction to specific drugs do wax and wane over time (somewhat like infectious disease epidemics), and they can also vary considerably by population subgroups, region, or across the urban/rural divide.
NSDUH findings from 2018 estimate that about 20.3 million people (7.4% of the US population aged 12 and over (~274 million people)) met criteria for a substance use disorder in the past year. Within this set, the top five substance disorders by prevalence of drug type included #1, alcohol (14.8 million, 5.4% of the population); #2, marijuana (4.4 million; 1.6%); #3, opioids (including “misused” prescription opioids and heroin; 2.2 million; 0.8%); #4 methamphetamines/amphetamines (including other “misused” prescription stimulants; 1.7 million; 0.6%); and #5 cocaine (1 million; 0.4%).
It is important to appreciate that these estimates exclude several addiction contexts or subgroups: (1) chronic use and disorders involving tobacco (estimated to be about 12–18% of the population when counting cigarettes, cigars, pipes, dipping, snuff and chewing); (2) the use of nontobacco nicotine products (vaping, e-cigarettes, nicotine gum); (3) those with addictions who are younger than 12; and (4) adults with addictions to opioids, stimulants, and/or sedative/hypnotics that they may be prescribed and taking as directed, even though they may actually have undiagnosed addictions to those drugs.
The actual percentage of the US population (age 12 years and older) meeting criteria for a substance use disorder is thus around 20% when tobacco/nicotine products are included. Notably, the fraction of the US population (12 and older) who used a particular addictive substance (spanning nicotine, alcohol, and illicit drugs) within the last month, but not necessarily in a pattern that would meet criteria for a substance use disorder, was 164.8 million, or 60.2% of the adult population!
Analyses that compare the fractions of the population who meet criteria for a SUD for a given drug compared to that drug’s rate of overall use (i.e., use that is and is not at levels that represent addiction) can provide a way to estimate which drugs are among the most addictive in human populations. From this perspective, which estimates a given drug’s relative addiction risk or addiction potency as a matter of how likely a person will get addicted if they experiment with it, the weight of the evidence suggests that stimulants (amphetamines/cocaine), opioids, and nicotine rank among the most addictive of all known substances. Alcohol, marijuana, and sedatives (to a large extent in this order) are moderately addictive; and the hallucinogens (e.g., LSD, psychedelic mushrooms) are least (or not at all).
Unfortunately, most epidemiological studies focused on describing rates of addictions involving illicit substances or alcohol typically exclude nicotine (and tobacco) despite its highly significant public health impact (e.g., as the most lethal of all addictive drugs in terms of total yearly death toll), and characteristic as one of the most highly addictive of all known substances. This frequent omission of nicotine from the research literature hampers understanding of overall substance disorder rates in the general population and in certain patient groups (e.g., the mentally ill). This has led to underestimations of the overall scope and impact addiction has on society and in certain subgroups, and how these drug addictions frequently intermingle. For example, the study of Lasser et al. (Reference Lasser, Boyd, Woolhandler, Heimmerlstein, McCormick and Bor2000) was among the first to show how concentrated nicotine addiction actually is in people with mental illness. This study showed that about half of all cigarettes smoked in the US are consumed by someone with mental illness, and lifetime rates of nicotine addiction were found in about 55% and 59% of those with lifetime or past month mental illness, respectively. Similarly, Weinberger et al. (Reference Weinberger, Gbedemah, Wall, Hasin, Zvolensky and Goodwin2018) found that 56% of those with an illicit substance use disorder also use tobacco, while Grant et al. (Reference Grant, Hasin, Chou, Stinson and Dawson2004) showed that 45% of people with alcohol dependence (i.e., alcohol addiction) also had nicotine addiction. Notably, Grant et al. also confirmed Lasser et al.’s earlier findings linking nicotine to mental illness. In Grant et al. (Reference Grant, Hasin, Chou, Stinson and Dawson2004), a third of all cigarettes were found to be consumed by just 7.1% of the US population – those who also have a mental illness. At the same time, people who have nicotine addiction and a mental health history of some kind comprised about 55% of all smokers! Together, these data showed that (1) polysubstance use disorders (i.e., having more than one type of drug encompassed within a patient’s addiction illness) is the rule and not the exception for those using illicit substances; (2) polysubstance use is present in nearly half of people suffering with alcoholism; and (3) having an addiction of any kind is the norm in half or more of people with current or history of mental illness.
The following sections will discuss substance use disorder epidemiology across various sub-groups. A range of genetic, environmental, and neurodevelopmental risk factors are typically in play to generate increased risk and penetrance of addiction disease in particular subpopulations. Often these factors co-conspire simultaneously within one subgroup or individual to greatly increase both disease risk and severity. This is particularly true in the context of adolescent/young-adult neurodevelopment and in mental illness as explained from a neurobiological perspective in Chapter 4.
In considering the following epidemiological subgroup information, it is important for the reader to know that addiction psychiatry as a field is sensitive to and aware of the harmful effects of adverse sociopolitical–cultural forces, including stigma, racism, misogyny, and anti-LGBTQ-ism on patients. This sensitivity probably comes from the fact that people suffering with both addiction and mental illness are among the most stigmatized and judged people in the world, and this stigma often must be born (by simple association) not just by these patients, but to a lesser extent by the expert physicians and allied professionals who are dedicated to using science to get them better.
Unfortunately, government-funded efforts and resources used to address addiction in patients as a criminal–legal matter (e.g., in the “war on drugs”) have also been admixed with laws and traditions that have reflected systematic racism, and/or disproportionally target the poor who cannot afford good legal representation (or sometimes mental health care). Thus, many of the same legal codes that have attempted to criminalize and punish addictive behavior out of existence also disproportionately target certain racial or socioeconomic groups with government-enforced fines, workhouse stays, and incarceration – all happening in competition with, or to the sacrifice of government funding needed to support evidence-based addiction and mental health care.
Addiction psychiatrists are also aware that stigma, racism, misogyny, anti-LGBTQ-ism, antisemitism, and so on, can operate as a form of group-on-group experiential and emotional trauma that can readily generate or worsen PTSD or affective disorders. Because these mental disorders are also brain conditions that biologically increase addiction risk manifesting as dual-diagnosis disorders (see Chapter 4), addiction psychiatrists are vigilant in trying to help, shield, and recover patients who are suffering in part due to the adverse out-casting and dehumanization effects of stigma, and the other “isms.” This vigilance includes the expert capacities of addiction psychiatrists to maintain appropriate nonjudgmental, compassionate therapeutic postures (see Motivational Interviewing in Chapter 5) for all patients, even those who may themselves express highly stigmatizing or bigoted thoughts despite, or because of, their own mental illnesses or internalized trauma histories. Finally, addiction psychiatrists are well familiarized with the necessary work of having to advocate for justice, equity, diversity, and inclusion in medical care and research, because dual-diagnosis patients include people from all racial, ethnic, age, and sexual diversity groups. Moreover, the stigma heaped upon addiction and dual-diagnosis patients in health care, and even from within some sectors of psychiatry, has adversely impacted support for clinical services, professional training, and research, that is greatly needed to more effectively treat patients that addiction psychiatrists take care of.
Mental Illness
The tight epidemiological association and overlap between addiction and mental illness has been a consistent, highly replicated finding across population studies in the US, and throughout the world for many decades. As reviewing this literature is too large for the purposes of this book, we will describe fairly recent US data that is well-representative of the enduring and pervasive scope of the association.
According to NSDUH data from 2018 (SAMSHA, 2019; national sample of n = 7,791 the US population aged 18 or older is estimated to have about 47.6 million people (19.1%) with a mental illness of some kind, with 11.4 million (4.6%) being categorized as have a severe mental illness that is significantly chronic and debilitating. Within each of these groups: 9.2 million (3.7% age 18 or older in US population) have any mental illness and a substance use disorder(s), while 3.2 million (1.3%) have a severe mental illness and a substance use disorder(s). There are three key observations to make about these numbers:
(1) Addictions and mental illness are closely linked epidemiologically (i.e., these diseases strike people in highly convergent and overlapping ways in the general population). Considering that 20.3 million of the US population (age 12 and older) has a SUD (non-nicotine) of some kind, these data tell us that about 9.2 million of the 20.3 million with SUDs (equal to 45% of those with SUDs) also have some kind of mental illness. Thus, nearly half of all addictions present in the US are concentrated in only a fifth of the population – those who also have a mental illness.
(2) Increasing severity of mental illness also corresponds to increasing risk of having an addiction. Note that while 9.2 million of 47.6 million (or 19%) with any mental illness also have a SUD(s), about 3.2 million of the 11.4 million (or 28%) with severe mental illness, have a SUD(s). This means that within the population with any mental illness, 3.2 million of 9.2 million (35%) of the addictions occur in the subpopulation with severe mental illness, even though the severely mental ill make up only 11.4 million/47.6 million = 24% of the population with any mental illness. Thus, people with severe mental illness who make up only 4.6% of the total adult US population, account for 3.2 million/20.3 million or 16% of all SUDs happening in the general adult population. As a rule of thumb then, mental illness roughly doubles the risk of acquiring addiction, whereas severe mental illness nearly quadruples the risk.
(3) These comorbidity figures, describing the epidemiology of what is variously called dual diagnosis or co-occurring disorders, likely represent underestimates of the close connection between mental illness and addiction. As mentioned above, these tallies of SUDs do not include use and disorders involving tobacco (estimated to be about 21.5% of the population when counting cigarettes, cigars, pipes, dipping, snuff, and chewing), and/or the use of nontobacco nicotine products (vaping, e-cigarettes, nicotine gum). This is a critical omission because we also know that nicotine ranks as among the most addictive and deadly of all addictive drugs, and it is even more concentrated in people with mental illness (>50%) or those with severe mental illness (>75%) than are other addictions.
Taken together, as summarized in Figure 1.1, these numbers make it clear that the overall public health impact of addiction (including its huge associated consequences in generating chronic medical diseases, injuries, and premature death) is disproportionately and massively shouldered by those who also suffer with mental illness. Although suicide is a major cause of death in people with mental illness, the death toll (and causation of chronic medical diseases and injuries) produced by addictions in the mentally ill is far greater than suicide, even as addiction is also a driver of suicide risk. Chapter 4 will provide an in-depth neuroscientific explanation for the close linkage between mental illness and addiction.
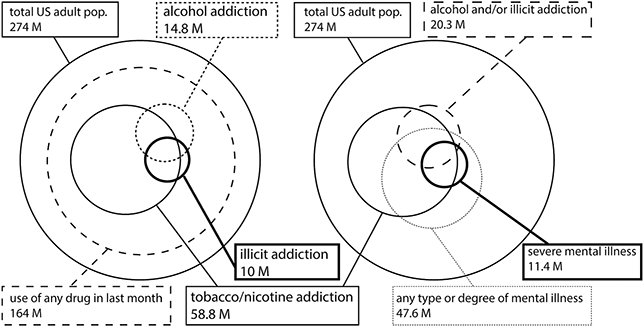
Figure 1.1 2018 US population SUD and mental illness prevalence and comorbidity (based on NSDUH/SAMHSA data). Left panel shows relative scales (size of circles) and overlaps within the US population (12+ years of age) and any substance use (pathological or not) versus addiction spectrum disorders involving tobacco/nicotine, alcohol, and illicit drugs (opioids, marijuana, methamphetamine). Right panel shows relative scales in the US adult population (12+ years of age) and numbers of people with any mental illness/severity versus those with severe mental illness and how those compare and overlap with tobacco/nicotine addictions, and other drug (illicit + alcohol addiction). As per factors described in the text and underreporting due to stigma, rates of substance use and disorders are likely actually greater than depicted here.
Age: Adolescence to Young and Older Adulthood
Adolescence is the age when most people who go on to acquire addiction, often by their young adult years, begin to experiment with substance use. From the NSDUH data set (the 2018 US sample of n = 67,791) we can assess the large increases in substance use across these age ranges. These data include past year use that may or may not qualify as representing acquisition of a substance use disorder. In the age range of kids (12–17 years old) to young adulthood (18–25) alcohol use increases about 6.2-fold from 9% of kids to 55.5% of young adults. Cigarette use (not including other forms of tobacco/nicotine) increases about 7-fold from 2.7% to 19.1%. Marijuana use increases about 2.8-fold from 12.5% to 34.8% while misuse of opioids (use of opioids without a prescription) doubles from 2.8% to 5.5%. Notably, heroin use is much smaller than diverted pharmaceuticals in this opioid uptake, going from <0.1% of kids to 0.5% in young adults. Misuse of stimulants (using prescription stimulants that are not prescribed, not including cocaine or methamphetamine) rises 4.3-fold from 1.5% to 6.5%.
Lifespan rates of substance use patterns diagnosable as addictions (based on DSM-5 criteria for substance use disorders involving alcohol, tobacco, cannabis, and opioids) are shown in Table 1.3 (from Vasilenko et al., Reference Vasilenko, Evans-Polce and Lanza2017). These data, drawn from an earlier US representative sample (n = 36,309; 2012–2013; NESARC-III), as comparable to the 2018 NSDUH data, provide an excellent snapshot of how peri-adolescent experimentation of drugs leads to age and gender-related trajectories of major addictions from 20 to 80 years old. Note how prevalence rates of addictions tend to level off and gradually decline with age after the early 20s, either because the addictions are killing their hosts or these people are able to survive after achieving illness remissions. This kind of pattern has been seen across many studies spanning multiple previous generations and many other countries. It also holds up well across most major addictive drug types as shown here. Adolescence is thus a rapid period of acquisition of addictions, while adulthood represents a long struggle with the disease, in which there is often only one victor. Chapter 4 provides a neurobiological explanation for adolescent addiction vulnerability that is interestingly similar to and developmentally interactive with mental illness–based addiction vulnerability.
Table 1.3 Age and gender-based prevalence rates for substance use disorders National Epidemiologic Survey of Alcohol and Related Conditions (NESARC-III); n = 36,309 participants. Based on DSM-5 criteria for substance use disorders/addictions (% of age cross-section). Percentages are bounded by 95% confidence intervals of approximately ±1% (Vasilenko et al., Reference Vasilenko, Evans-Polce and Lanza2017).
| Alcohol | % | Tobacco | % | Cannabis | % | Opioid | % | |
|---|---|---|---|---|---|---|---|---|
| Age | Male | Female | Male | Female | Male | Female | Male | Female |
| 20 | 29 | 23 | 22 | 16 | 14 | 7 | 3 | 3 |
| 30 | 30 | 17 | 30 | 21 | 5 | 3 | 3 | 2 |
| 40 | 19 | 11 | 26 | 19 | 3 | 2 | 2 | 2 |
| 50 | 15 | 10 | 26 | 20 | 3 | 2 | 3 | 2 |
| 60 | 11 | 5 | 21 | 15 | 2 | 1 | 1 | 1 |
| 70 | 6 | 2 | 10 | 7 | 1 | 1 | 1 | <1 |
| 80 | 2 | 1 | 5 | 5 | <1 | <1 | <1 | <1 |
Gender
Males have a higher prevalence of SUDs than females in the US population, also shown in Table 1.3. This trend has generally held up across different addictive drug types, different populations (and nations), and eras of sampling, although the ratios of male to female rates do fluctuate over time. In recent years, some studies have shown that female rates are “catching up” to males with respect to some drugs, suggesting that there are strong environmental–cultural forces in play that modify this risk, just as much as there are biological–genetic risk factors and behavioral traits associated with being male that increase addiction risk compared to females. Notably, although most studies have shown much greater risk of acquiring addiction in men compared to women, there is also evidence that when women do get it, it happens with a faster rate of onset. This effect, called telescoping, refers to a shortened amount of time from first use of a drug to onset of addiction, which may reflect situations where an individual has an unusually high concentration of risk factors for addiction (e.g., presence of mental illness) that may counteract relatively protective factors (e.g., being female). The data collection in Table 1.3, like nearly all large-scale studies, does not include analysis of people defined by additional gender/sex/sexual orientation classifications, such as the transgender population. There is less information available about nonbinary populations, and transgender data are often included within the umbrella of LGBTQ rather than on their own.
LGBTQ Populations
The LGBTQ population has more than twice the rates of using addictive substances compared to people who identify themselves as being in the cis-gendered heterosexual category. This is seen with alcohol binge drinking, marijuana use, and prescription pill use. Per NIDA data, LBGTQ individuals may start using addictive substances at earlier ages and thus eventually enter treatment with higher levels of addiction disease severity. Mental illness, which generates addiction vulnerability as discussed above, also occurs at higher rates in the LGBTQ community, as a possible consequence of trauma-related brain responses to social persecution and out-casting. Much more research is needed to understand the causality, neurobiology, and unique treatment needs of the LGBTQ community with addictions and dual-diagnosis disorders.
Racial/Ethnic Groups
Susceptibility to addiction disorders is comparable across most racial-ethnic populations. Higher- or lower-than-average rates of certain types of SUDs in certain ethnic groups are often associated with cultural or socioeconomic factors that are discussed in the remainder of this chapter. However, Chapter 4 will mention some genetic differences in addiction risk that do occur in different frequencies across different ethnic-racial groups. Regardless, a higher prevalence of addiction in any specific subpopulation can lead to downward socioeconomic drift, with transgenerational transmission of disease risk, making it even more difficult for family lines within certain subpopulations to recover.
Education
Lower levels of education have been found in some studies to be correlated with higher rates of substance misuse or addiction. However, this association is complex. A number of premorbid risk factors (presence of mental illness, family instability) that can increase addiction risk later on can also cause derailment of educational attainment. So can the onset of heavy substance use during teenage years. Per 2010 NSDUH data, those without a high school degree had a higher rate (10.2%) of SUDs than those with a high school degree (8.5%), followed by adults who finished college having the lowest rates (6.3%). However, the highest rate was seen in adults with some college education who did not finish their degree (10.6%). It is important to note that addiction is not a sign of lower intelligence. The book Deaths of Despair and the Future of Capitalism (Case and Deaton, Reference Case and Deaton2020) outlines how college education confers more than just a degree but grants social access to higher-paying careers, or careers that do not require physical exertion or introduce as much risk of injuries (e.g., that may lead to chronic opioid prescriptions), or allow for better health insurance plans. Having a college degree is generally associated with lower mortality rates due to suicide and drug overdose. It also associates with lower risk of alcoholic liver disease, lower pain scores, higher rates of marriage, and higher self-assessed overall health scores.
Interpretation of these associations should be made with caution, as there are likely many causal dynamics (some of which are hard to capture in studies) that could be giving rise to this association. Clearly, there are examples where an inverse relationship between lower addiction risk and higher educational obtainment (or socioeconomic status) does not hold up as demonstrated by the notable exception of physicians. Although doctors are among the most highly educated, health aware, and well-paid members of society, they suffer with addictions at rates that are comparable to or even higher than the general population (e.g., especially in the fields of anesthesiology, emergency medicine, and orthopedic surgery). Job-associated environmental factors like long work hours, high stress, and easy access or exposure to controlled drugs while on the job are associated with this increased risk. Notably, however, physicians as a group also show rates of successful addiction treatment outcomes that are better than the general population. This may be due in part to physicians enjoying better access to (and being able to afford) better-than-average quality and durations of care. A long-range goal of addiction psychiatry is to eliminate such disparities in access to care for all people regardless of socioeconomic status.
Another well-known occupational sector that suffers relatively high levels of addiction morbidity and mortality is in the upper echelons of the entertainment industry. Despite often being widely recognized for having rare intellectual gifts of creativity and high earnings, movie stars and rock stars are known to suffer higher risk of addictions and lethal outcomes. Multiple personal and occupational factors are likely in play to drive this risk, one of which may be the psychiatrically toxic effects of extreme fame. Extreme wealth may also, quite ironically, put entertainment stars at risk, because it may increase the risk of becoming surrounded by people (or pseudo-professionals) who want to use them for their fame and money rather than take care of them.
Employment Status
As already suggested in the section on the economic impacts of addiction, lower employment status is correlated with higher rates of substance misuse and addiction. As per NSDUH (2010) data, unemployed adults showed the highest rates of SUDs (17.5%) followed by adults employed part-time (11.2%) and adults employed full-time (8.4%). Educational attainment, family employment, and family socioeconomic status are all intercorrelated variables in the US, which are also tied to access to quality health care. Given that addictions cause damage to educational attainment and occupational performance, we observe that unemployment, low education, and addiction are all linked through multiple bidirectional relationships. For example, although substance use can impair job performance, unemployment can represent a significant source of psychological stress and mental health problems, which can raise addiction vulnerability. In turn, both mental illness and addiction increase risk of job loss and loss of insurance coverage (which in the US is tightly linked with employment) needed to support access to mental health and/or addiction treatment. As already mentioned, these trends should not lead to the assumption that addicted patients are generally poor and/or unemployed. Indeed, about two-thirds of people with treatable active SUDs are gainfully employed full-time. Regardless, an important take home implication of the fact that addiction and comorbid mental illness can produce downward educational and socioeconomic drift is that effective treatment has the potential to stop or even reverse this drift for patients and their families. Thus, the practice of addiction psychiatry offers society a positive social and economic impact beyond its direct public health benefits, in preventing worsening socioeconomic divisions.
Criminal Justice System Population
Adults who had been on parole or released from jail in the past year have 3–8 times greater rates SUDs (depending on specific drug type) comparable to a general population sample (NSDUH data collected 2002–2014, described in Fearn et al., Reference Fearn, Vaughn, Nelson, Salas-Wright, DeLisi and Qian2016). Nicotine addiction is also estimated to range from 50% to 90% (three- to six-fold general population rates) in Americans with criminal justice involvement both before and after incarceration. Similarly increased rates of mental illness are also found in incarcerated populations (e.g., as large city jails have replaced psychiatric treatment centers). Unfortunately, in the post deinstitutionalization era (c. 1960–2000) when most long-term psychiatric hospital beds were eliminated, and with the advent of “the war on drugs,” large numbers of people that have or are susceptible to mental illness, addictions, and dual-diagnosis disorders have been sequestered away from access to evidence-based treatment into circumstances of homelessness, criminalization, and mass incarceration. This dynamic, happening with substantial force over the last half century in the US and much of the western world, was initially described by the British psychiatrist Penrose over 80 years ago. In the Penrose effect, there tends to be (across modern economies) a reciprocal-inverse relationship between prison populations and psychiatric treatment infrastructures. Because mental illness is a strong biological vulnerability condition for addiction (as we describe in detail in Chapter 4), the “war on drugs,” has essentially and unfortunately operated as an accelerant for the Penrose effect (Grecco and Chambers, Reference Grecco and Andrew Chambers2019). This dynamic has in turn resulted in the overidentification of criminality with mental illness and addiction. This effect not only compounds stigma against these disorders, but it concretely damages society’s (and healthcare systems’) emphasis on and financial support for treatment. While the cost of mass incarceration is in competition with the costs of providing higher education and providing mental health care, patients who are criminalized often lose health insurance directly as a consequence of incarceration, or they are rendered unemployable (and thus uninsured) due to criminal records that are drug-use related.
Certainly, there remains a vital role for the legal system and law enforcement in monitoring, regulating, controlling, and interdicting the production, distribution, and misapplication of additive-psychoactive compounds. This is especially needed for stopping distribution by illegal channels and large-scale distribution networks mediated by organized crime groups, foreign adversaries, or even doctors and clinics that are operating as drug dealers under the disguise of health care. However, an overemphasis on prosecuting and incarcerating low-level consumers of addictive drugs in the war on drugs has had the unintended consequence of contributed to a weakening of treatment infrastructure, professional training, workforce development, and insurance coverage for behavioral health that is needed to prevent and treat addiction more effectively. Past and ongoing failures of the US healthcare system and its mental health sectors to fully accept addiction as a biomedical condition, and to grasp and respond to the interconnection between mental illness and addiction, has represented a root cause of the US iatrogenic opioid epidemic. Beginning in the 1990s and still unabated, the addiction epidemic in the US has grown in parallel with the mass incarceration of mentally ill/addicted people and an increasing death toll due to addictions and overdoses in this very same population.
HIV/AIDS
About a third to half of individuals with human immunodeficiency virus (HIV) are estimated to have had an SUD diagnosis, often involving multiple drugs. The two primary routes of contracting HIV – via unprotected sex or using unsterile needles – are both associated with substance use. Several forms of mental illness and substance use (e.g., involving opioids, methamphetamine, and alcohol) produce or are associated with high levels of impulsivity and/or rapid progression through multiple sexual partners. All these behaviors increase the risk of acquiring HIV and addictions. HIV and addiction are so often intertwined that an outbreak of one can be a sign for the other, as happened in the HIV outbreak in Scott County, Indiana in 2015. This event represented one of the largest and most explosive HIV outbreaks in US history. The rural town of Austin in Scott County, home to a population of 2,000 people, encompassed a remarkably high rate (25% of the total population!) who were not just opioid-addicted, but were actively injecting diverted pharmaceutical opioids (predominantly oxymorphone) that required delivery through large-bore needles. Among these 500 intravenous drug users, over 200 cases of HIV had spread in just 6 months.
In Austin, the makings of a perfect storm had emerged in a rural area, at the height of the iatrogenic opioid epidemic, where there was little to no access to legitimate addiction treatment, and the main approach to dealing with addiction had been arresting and jailing people. Generally, any group of people engaging in active iv. drug use who are HIV positive, and are unable to access addiction treatment, can show a high rate of HIV transmission. This occurs for several reasons, including the fact that patients in active addiction tend to be less likely to have their HIV diagnosed or be compliant on antiviral medications while maintaining other high-risk behaviors. Ironically, although the epidemic of addiction that led to the Austin HIV outbreak generated a quite rapid and effective state and federal response focused on the HIV (by 2016 the HIV spread had essentially been stopped, and no one had died of AIDS), the county had suffered for many years with incredibly high rates of per-capita incarcerations and overdose deaths. These trends continued due to the underlying addiction that was never adequately recognized or addressed as a disease in its own right. The failure of government and affiliated healthcare entities to have properly recognized and addressed the underlying addiction disease that caused the HIV outbreak, on par with how the HIV itself was decisively addressed, was a clear and stunning illustration of the effects of stigma, disparities in health equity, and lack of parity. Lack of parity refers to failures of healthcare systems and insurance companies to support adequate services needed for the diagnosis and treatment of addiction and dual-diagnosis diseases on par with other diseases that addiction may lead to, like HIV.
Location and Era
Different regions of a country can show differential rates of addiction, and addiction-related health consequences. In the United States, SUDs (excluding nicotine) have been reported to vary from highest to lowest rates regionally as follows: West (10%), Northeast (9.4%), Midwest (8.2%), South (7.8%). However, specific substances may not follow the same overall trends because geographical differences can be highly drug-specific based on the conditions of local supply or knowledge of drug-making. For example, methamphetamine use has been most prevalent in the West, Midwest, and South, with much lower levels of use in the Northeast. These patterns have reflected both the manufacturing techniques involved in Meth production (which readily utilize rural–agricultural products) and black-market importation trade routes. In the meantime, although the iatrogenic opioid epidemic started out strong particularly in rural, predominantly poor, white regions of the Midwest and Appalachia, it has evolved to attack more urban nonwhite populations as well in recent years. Strikingly, geographical proximity and access to primary care and pharmacies in the Midwest has been identified as a risk factor acquiring opioid addiction, as a reflection of its iatrogenic causality.
The spread of street knowledge that propagated the easy manufacturing of crack cocaine (smokable free base) from the powder form of cocaine (which is consumed by snorting) led to a significant epidemic of crack cocaine addiction in the 1990s that was far larger and more detrimental than patterns of cocaine use in the 1970s and 1980s. This epidemic, predominantly hitting large urban centers, especially in the Northeast, involved an interesting interplay between gang-controlled trade routes for the drug and knowledge that cocaine, in its smoked (crack) form, is a far more addictive. A parallel dynamic occurring in the legal tobacco industry has involved deliberate changes to the design and chemical content of cigarettes (e.g., including adding menthol) by tobacco companies to increase the addiction potency of their products (the reader is encouraged to see 1999 film The Insider, which dramatizes part of this history).
The Big Picture View of Addiction Psychiatry in Preventative and Public Health
This chapter has begun to describe the central role addiction disease plays as a major public health threat that is a leading root cause of body injuries, general medical illness, and all-cause mortality. At the same time, addiction is closely, causally interlinked with mental illness on the levels of whole populations and within individual’s brains (as we explore in Chapter 4). Accordingly, addiction psychiatry stands as a field of medicine (and form of training) that uniquely equips doctors to prevent and stop this complex disease propagation as it spreads from mental illness to addiction (and back again), eventually leading to very serious body organ damages, injuries, infections, and premature death. As a specialty that recognizes, embraces, and tackles complex comorbidities in behavioral health, addiction psychiatry is adept at interdicting dual-diagnosis disease impact as it tends to flow not just between brain and body organs, but transgenerationally within families (Figure 1.2), and from the suffering individual to our suffering society. In the next chapters we describe how addiction psychiatrists understand addiction disease clinically and neurobiologically, and how we diagnose it and treat it based on this knowledge. These descriptions are intended not just to educate the next generations of doctors and scientists who will have to confront this remarkable and terrible disease of the brain, but to generate larger interest and collective efforts in growing addiction psychiatry to where it becomes a major cornerstone of both behavioral health and public health.
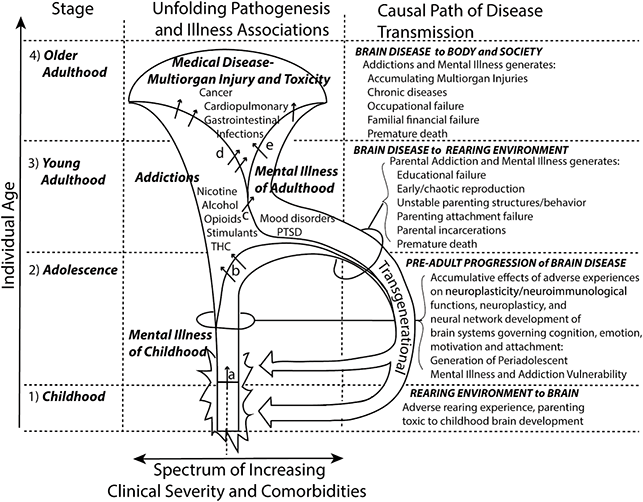
Figure 1.2 “Bugle-horn comorbidity pathway” of mental illness, addiction, and medical (multiorgan) morbidity. In (1) childhood and (2) adolescence, adverse rearing environments, impaired parental behavior, and attachment failures are biologically neurotoxic to the developing brain (and may compound with genetic loading for mental illness) resulting in preclinical or emerging signs of mental illness (a, arrow). In turn, mental illness–induced neurobiological vulnerability to drug addiction leads to the onset of one or more addictions in adolescence and/or (3) young adulthood (b, arrows), which further exacerbates the neurobiological and clinical dimensions of the underlying mental illness (c, arrow). The mental illness/addiction comorbidity experienced during young adulthood results in chaotic reproduction and parenting impairments and instability, exposing offspring to a new cycle of adverse rearing environments and experiences. The later causal dynamic (handle of the bugle) represents both a transgenerational and transenvironmental–neurobiological cycle: the brain illness of the parent generates an adverse environment for the child; the adverse environment for the child conspires with their genetic inheritance to generate adult mental illness, addiction, and impairments in their parenting capabilities for the next generation, and so on. Into (4) older adulthood, the scope, severity, and impact of addictions and mental illness comorbidities worsen (the girth of the bugle enlarges) so that greater varieties and severity of multiorgan toxicities and injuries (i.e., chronic medical diseases and early death rates) and social damages (financial collapse, criminalization) accumulate as consequences of addiction disease (d, arrows) and mental illness (e, arrows).