Take home message
A physically active lifestyle is important for health and development in all children.
Methodological variations and limitations in previous research interfere with the ability to establish whether the physical activity patterns in children with CHD differ compared to healthy controls, or due to the severity of the heart disease.
By supporting methodological understanding and providing guidelines for physical activity assessment using accelerometers, this review targets improved knowledge about the physical activity patterns in children with CHD.
The outcome of physical activity assessment using accelerometer is affected by measurement protocol, device settings, body placement (e.g. hip, thigh, wrist), raw data processing, value calibration method, and statistical methods.
The incidence of CHD is approximately 8 out of 1000 live births. Reference Van Der Linde, Konings and Slager1 However, the survival rate has radically improved due to advances in clinical care and surgical techniques. Reference Lundström, Berggren, Björkhem, Jögi and Sunnegårdh2,Reference Tchervenkov, Jacobs and Bernier3 A recently published, nationwide Swedish study shows that since the beginning of this century, over 97% of children born with CHD can be expected to reach adulthood. Still a relatively high mortality is associated with the most complex diagnoses, especially during the first years of life. Reference Mandalenakis, Rosengren, Skoglund, Lappas, Eriksson and Dellborg4 Among survivors, the severity of the CHD determines the physical capacity and complications experienced later in life. Reference Ryberg, Sunnegardh, Thorson and Broberg5–Reference Amedro, Picot and Moniotte7
The severity of the CHD may be divided into three broad categories (four categories may also be applied). Reference Ryberg, Sunnegardh, Thorson and Broberg5–Reference Siaplaouras, Niessner and Helm8 The most severe category includes complex CHD for which the long-term prognosis is uncertain, with serious complications and a peak oxygen uptake at 30 ml/kg/minute or lower, for example, univentricular heart lesions, pulmonary atresia with ventricular septal defect, and major aortopulmonary collaterals. The moderately severe category includes individuals treated with surgery and/or catheter intervention, who are followed up regularly due to risk for further complications and have a peak oxygen uptake varying around 40 ml/kg/minute, for example, transposition of great arteries, tetralogy of Fallot, and aortic stenosis. The mild severity category consists of individuals who are treated once with surgery or catheter intervention, are in most cases no longer followed up due to low risk of further complications, and may have a peak oxygen uptake similar to individuals with no CHD, that is, 40 ml/kg/minute or higher. Individuals with CHD have lower peak oxygen uptake than their healthy peers, especially those with more severe heart defects. Lower peak oxygen uptake is associated with lower cardiovascular health, academic achievement, and well-being. Reference Raghuveer, Hartz and Lubans9
Concerns have been raised about the increased risk of being overweight and having additional cardiometabolic disease later in life in patients with CHD and the risk is even higher with more severe CHD. Reference Andonian, Langer and Beckmann10–Reference De Ferranti, Steinberger and Ameduri12 Due to limitations in physical capacity, Reference Amedro, Gavotto and Guillaumont6,Reference Amedro, Picot and Moniotte7 but also because of restrictions from parents and caregivers and low self-efficacy, Reference Siaplaouras, Niessner and Helm8,Reference Bar-Mor, Bar-Tal, Krulik and Zeevi13 it may be assumed that children and adolescents with CHD are less physically active than children and adolescents in general. This creates a need to focus on aspects of health-related quality of life, physical activity, and prevention of acquired cardiovascular disease in this group of patients. As physical activity, sports participation, and aerobic fitness have been acknowledged as crucial for health and development in children and adolescents, their promotion has been emphasised by international cardiology associations. Reference De Ferranti, Steinberger and Ameduri12,Reference Budts, Pieles and Roos-Hesselink14,Reference Longmuir, Brothers and De Ferranti15 A recent review conducted by Caterini et al Reference Caterini, Campisi and Cifra16 especially argued for the importance of actively promoting physical activity in the younger CHD population for fostering a healthy, active lifestyle and also highlights the existing evidence gap in lack of models for implementing strategic physical activity in CHD populations as well as reliable and valid wearable technology for increasing and measure physical activity.
Acosta-Dighero et al Reference Acosta-Dighero, Torres-Castro and Rodríguez-Núñez17 and Van Deutekom and Lewandowski Reference van Deutekom and Lewandowski18 provided recent reviews of original studies using either subjective or objective methods to assess physical activity in children and adolescents with CHD. These reviews suggest similar physical activity level in children and adolescents with CHD compared to healthy controls, or in relation to the severity of the CHD, although several inconsistencies between studies were reported. This finding is somewhat unexpected, considering the physical limitations and other restrictions reported in children and adolescents with CHD. However, a deeper and more critical analysis of the measurement methodological limitations was missing from these review studies. This knowledge is crucial for explaining the unexpected finding, in order to determine the methodological progression required in future assessment of physical activity in clinical research.
Assessment of physical activity is mainly divided into two areas: subjective and objective measures. Former research of physical activity was primarily conducted using subjective methods like interviews and questionnaires as they are considered to be cost efficient, easily administrated, accessible, and is claimed to put little strain on patients. Reference Sylvia, Bernstein, Hubbard, Keating and Anderson19 However, extensive methodological limitations such as recall ability, memory, age, language, perception, understanding, and overestimation of both quantity and intensity of the performed physical activity have been identified, especially in the younger populations, causing poor reliability and validity. Reference Longmuir, Brothers and De Ferranti15,Reference Sylvia, Bernstein, Hubbard, Keating and Anderson19–Reference Westerterp24 In 2013, the American Heart Association stated: “…use of self-reports is recommended only when more objective measures cannot be obtained”. Reference Longmuir, Brothers and De Ferranti15 Thus, the quantification of physical activity is now merely performed using objective measures.
Objective devices to assess physical activity involve pedometers, accelerometers, heart rate monitors, multisensors (e.g. acceleration, heart rate, heat, sweat), indirect calorimetry, and doubly labelled water. Indirect calorimetry and doubly labelled water are considered golden standards of objective physical activity measures. Nevertheless, they are expensive and resource-intensive, thus not very convenient in most physical activity studies. Reference Arvidsson, Fridolfsson and Börjesson25 As an alternative, accelerometers are considered as cheap, well developed, and easy to use, showing greater validity than subjective measures. Reference Adamo, Prince, Tricco, Connor-Gorber and Tremblay22,Reference Atienza, Moser and Perna26,Reference Warren, Ekelund, Besson, Mezzani, Geladas and Vanhees27 However, even if being the most frequently used and evaluated objective method for assessing physical activity, Reference Migueles, Cadenas-Sanchez and Ekelund28 the use of accelerometers to assess physical activity holds certain limitations. Generally, there is a lack of knowledge regarding the field and function of accelerometers, how the specific settings and data management affect the outcome, and how these may be the source of measurement errors. Many accelerometer-based studies also fail to provide a transparency in the settings and data processing used, preventing others to uncover impacts on the measurement outcome or possible underlying measurement errors. In addition, the methodological transparency by the manufacturer may be quite low. Epoch lengths (time resolution of physical activity measures investigated), cut-points (threshold markers for the classification of physical activity intensity categories), and raw data filtration method represent three major issues that are seen to especially affect the outcome of the accelerometer-assessed physical activity. Reference Arvidsson, Fridolfsson and Börjesson25,Reference Aadland, Andersen, Anderssen, Resaland and Kvalheim29 Thus, even if the results are presented equally, the parameters may imply dissimilar aspects of the assessed physical activity, complicating comparisons of the physical activity measure. Reference Kerr, Marinac and Ellis30
The first objective of this study was to compile and organise the existing studies assessing physical activity in children and adolescents with CHD by subjective and objective (accelerometers) methods. The second objective was to critically evaluate the physical activity measurement methodology in the accelerometer studies and the consequences on results and conclusions. An important outcome from the second objective was to provide guidelines on the assessment of physical activity using accelerometers, in order to improve clinical research.
Methods
Search strategy
A literature search and a data extraction were performed between April 2020 and October 2020 in PubMed database. Two separate searches were conducted. The first search concerned subjectively assessed physical activity and the second search concerned accelerometer-assessed physical activity. We combined the following search terms in search one: Congenital heart disease OR defect, acquired heart defect OR disease, physical activity, exercise, children OR adolescents OR youth, surveys and questionnaires OR self-scattered OR self-reported OR subjective OR questionnaire; and search two: Congenital heart OR disease OR defect, acquired heart defect OR disease, physical activity, exercise, children OR adolescents OR youth, accelerometer OR accelerometry.
Inclusion/exclusion criteria
Inclusion and exclusion criteria are listed in Table 1. We included original articles studying children or/and adolescents with treated CHD, written in English, and published in peer-reviewed journals with a quantified physical activity outcome. Articles published in 2000 and later were included for subjectively assessed physical activity and 2009 and later for accelerometer-assessed physical activity due to developmental aspects in accelerometers. The patient group was set to children and adolescents with CHD between 3 and 20 years. Articles studying patient groups with known extensive health issues other than CHD were excluded.
Table 1. Inclusion and exclusion criteria for searches

Results
Characteristic of articles
Six articles were included for the subjectively assessed physical activity and nine for the accelerometer-assessed physical activity. Two of the articles were included for both searches as they used both subjectively and accelerometer-assessed physical activities. Figure 1 presents the article extraction. Two researchers reached consensus regarding the included articles. An overview of the included articles from the first and the second search is presented in Tables 2 and 3.

Figure 1. Flow chart of study selection process.
Table 2. Summary of characteristics search 1, methods, main findings and limitations of subjective-based studies

6MWT: 6-minute walk test; AC: accelerometry; COA: coarctation of aorta; DBP: diastolic blood pressure; HR: heart rate; IPAQ: International Physical Activity Questionnaire; PA: physical activity; PAQ-A: Physical Activity Questionnaire for Adolescents; PAQ-C: Physical Activity Questionnaire for Older Children; PedsQL: Pediatric Quality of Life Inventory; QoL: quality of life; RR: respiratory rate; SBP: systolic blood pressure; SpO2: peripheral oxygen saturation; TGA: transposition of the great arteries; TOF: tetralogy of Fallot; VPA: vigorous physical activity; VSD: ventricular septal defects
Table 3. Summary of characteristics search 2, methods, main findings and limitations of accelerometer-based studies

3DPAR: three-day physical activity record; 6MWT: 6-minute walk test; AC: accelerometry; ASD: atrial septal defect; CHD: congenital heart defect, general term; COA: coarctation of aorta; CSAPPA: children’s self-perceptions of adequacy and predilection for physical activity; EE: Energy expenditure; HD: heart disease; IPAQ: International Physical Activity Questionnaire; LPA; light physical activity; MET: metabolic equivalent of task; MPA: moderate physical activity; MVPA: moderate-to-vigorous physical activity; PA: physical activity; PAI: physical activity intensity; PAQ-A: Physical Activity Questionnaire for Adolescents; PAQ-C: Physical Activity Questionnaire for Older Children; PedsQL: Pediatric Quality of Life Inventory; QoL: quality of life; SED: sedentary behaviour; SV: single ventricle; TEE: total Energy expenditure; TGA: transposition of the great arteries; TOF: tetralogy of Fallot; TPA: total physical activity; VPA: vigorous physical activity; VSD: ventricular septal defects; WT: wear time
The study populations in the included studies differ substantially. Physical activity results are reported from both populations with mixed CHD, Reference Schaan, Feltez, Schaan and Pellanda31–Reference Brudy, Hock and Hacker36 from children and adolescents with one specific diagnosis, Reference Hedlund, Lundell, Villard and Sjoberg37 three specific diagnoses, Reference White, Willis and Panchangam38 from CHD as divided by mild to severe CHD group (different specifications), Reference Voss, Duncombe, Dean, de Souza and Harris39–Reference Ray and Henry41 between specific CHD diagnosis Reference Banks, Rosenthal and Manlhiot42 or between specific CHD diagnosis and as varied CHD group, Reference Zaqout, Vandekerckhove, Michels, Bove, Francois and De Wolf43 restricting comparisons and generalisation of the results.
Included articles, subjectively assessed physical activity
Six studies using subjectively assessed physical activity were included. Two articles reported physical activity data in CHD children, Reference Schaan, Feltez, Schaan and Pellanda31,Reference Brudy, Hock and Hacker36 one article compared different types of CHD and controls, Reference Zaqout, Vandekerckhove, Michels, Bove, Francois and De Wolf43 two studies compared different types of CHD with control samples from external databases, Reference Lunt, Briffa, Briffa and Ramsay40,Reference Ray and Henry41 and one article compared children with Fontan circulation to healthy controls. Reference Hedlund, Lundell, Villard and Sjoberg37 All of the six articles used different physical activity assessment questionnaires: Physical Activity Questionnaire for Older Children, Reference Zaqout, Vandekerckhove, Michels, Bove, Francois and De Wolf43 Youth Risk Behavior Survey, Reference Ray and Henry41 International Physical Activity Questionnaire-short version, Reference Schaan, Feltez, Schaan and Pellanda31 “The New South Wales Schools Fitness and physical activity Survey” Reference Lunt, Briffa, Briffa and Ramsay40 , one question assessment, Reference Brudy, Hock and Hacker36 and self-reported physical activity regarding organised physical activity. Reference Hedlund, Lundell, Villard and Sjoberg37
When looking at the comparison of children and adolescents with CHD towards healthy controls, contrasting results were present. Ray and Henry Reference Ray and Henry41 reported no significant difference in physical activity between patient and control groups in children with mild, moderate, and surgically treated CHD. Relatedly, Lunt et al Reference Lunt, Briffa, Briffa and Ramsay40 reported lower physical activity in male patients with mild and severe CHD and a similar trend in females, while as Zaqout et al Reference Zaqout, Vandekerckhove, Michels, Bove, Francois and De Wolf43 presented the opposite – a higher physical activity in the overall CHD patient group (ventricular septal defect, coarctation of aorta, transposition of great arteries, and tetralogy of Fallot) when compared to controls. Hedlund et al Reference Hedlund, Lundell, Villard and Sjoberg37 presented significantly lower physical exercise and significantly lower average intensity on Borg scale in patients with Fontan circulation than in healthy controls.
When comparing patients with different severity of CHD, two studies reported no significant differences in physical activity, Reference Lunt, Briffa, Briffa and Ramsay40,Reference Zaqout, Vandekerckhove, Michels, Bove, Francois and De Wolf43 whereas one failed to report the results for physical activity divided by the different severity groups. Reference Ray and Henry41
In the studies providing informative physical activity data, Schaan et al Reference Schaan, Feltez, Schaan and Pellanda31 reported low levels of patients in the “very active” (24%) and “active” (32%) output variables. Brudy et al Reference Brudy, Hock and Hacker36 found that the patients reported themselves as active 4.7 days/week, generally not meeting the World Health Organisation recommendations for children and adolescents in 60 minutes of moderate-to-vigorous-physical-activity a day. 44 These results are similar to those reported by Ray and Henry Reference Ray and Henry41 who reported that only 38% of the patients were physically active for at least 60 minutes and 7 days a week. Similarly, Hedlund et al Reference Hedlund, Lundell, Villard and Sjoberg37 reported a mean value of self-reported physical exercise of 135 minutes/week, indicating that the Fontan circulation patients generally fail to meet the World Health Organisation recommendations of physical activity. In contrast to these findings, both Zaqout et al Reference Zaqout, Vandekerckhove, Michels, Bove, Francois and De Wolf43 and Lunt et al Reference Lunt, Briffa, Briffa and Ramsay40 stated that most of the children and adolescents with CHD did meet the World Health Organisation recommendations of physical activity.
Included articles, accelerometer-assessed physical activity
In the accelerometer-based studies, nine articles were included (Table 4), whereas six studies compared children and adolescents with CHD towards healthy controls, Reference Ewalt, Danduran, Strath, Moerchen and Swartz32–Reference Arvidsson, Slinde, Hulthén and Sunnegårdh35,Reference Hedlund, Lundell, Villard and Sjoberg37,Reference White, Willis and Panchangam38 two studies compared types of CHD, Reference Voss, Duncombe, Dean, de Souza and Harris39,Reference Banks, Rosenthal and Manlhiot42 and one study compared children and adolescents with CHD to a healthy control group and type of CHD. Reference Zaqout, Vandekerckhove, Michels, Bove, Francois and De Wolf43
Table 4. Detailed methodological considerations and guidelines for improving assessment of physical activity
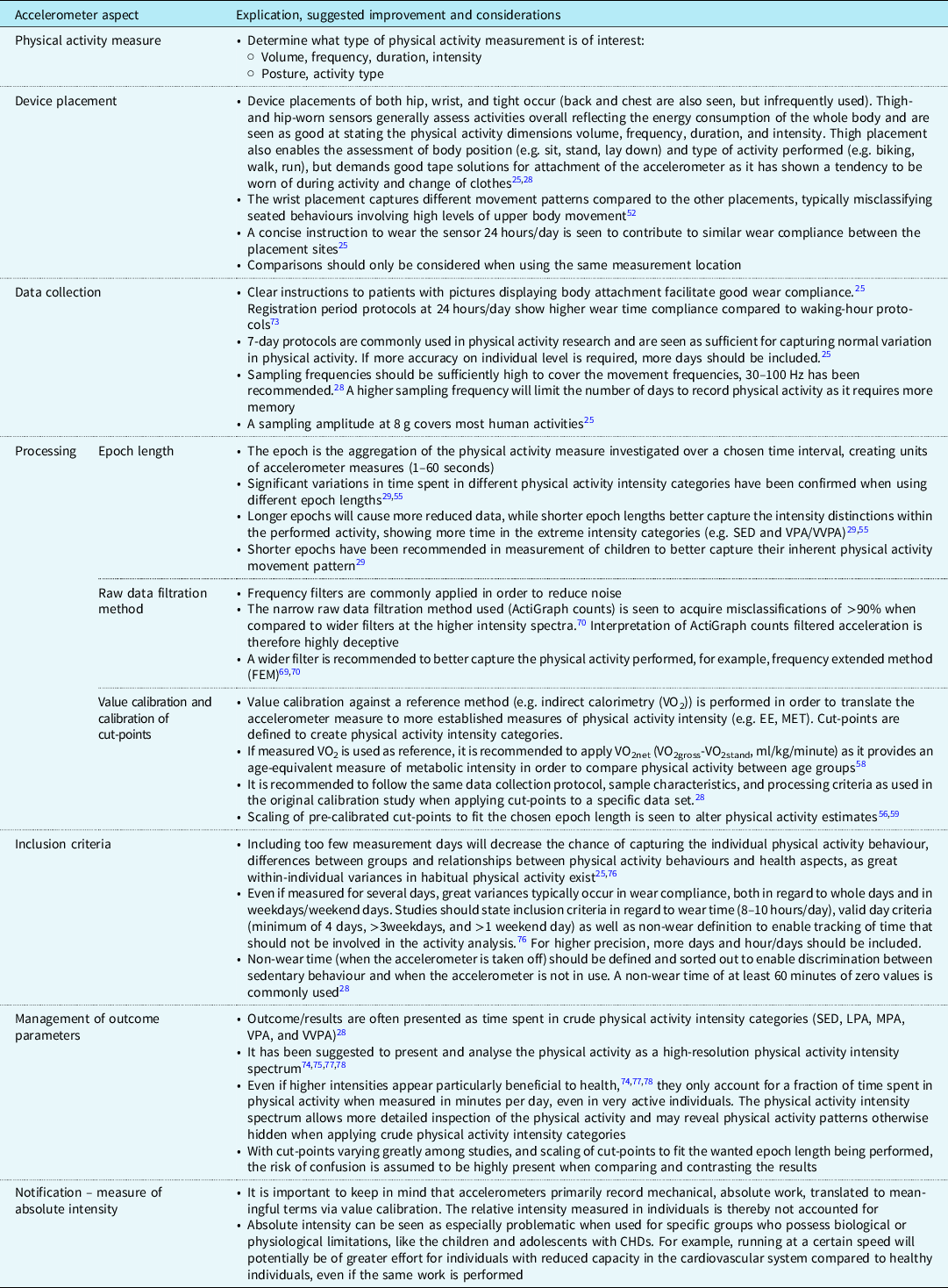
EE, energy expenditure; MET, metabolic equivalent of task (EEtotal/EErest); crude intensity categories; SED, sedentary behaviour (<1.5 METs); LPA, light physical activity (1.5–2.9 METs); MPA, moderate physical activity (3.0–5.9 METs); VPA, vigorous physical activity (6.0–8.9 METs); VVPA, very vigorous physical activity (≥9.0 METs); MVPA, moderate, vigorous, and very vigorous all together
Epoch lengths of 60 seconds were reported in three of the articles, Reference Arvidsson, Slinde, Hulthén and Sunnegårdh35,Reference Hedlund, Lundell, Villard and Sjoberg37,Reference White, Willis and Panchangam38 30 seconds epoch lengths were listed in one study, Reference Ewalt, Danduran, Strath, Moerchen and Swartz32 15 seconds in two of the studies, Reference Voss, Duncombe, Dean, de Souza and Harris39,Reference Banks, Rosenthal and Manlhiot42 and a 3 seconds epoch length in one study. Reference Stone, Obeid, Dillenburg, Milenkovic, MacDonald and Timmons34 Two of the included articles using accelerometer-assessed physical activity did not report the epoch length used in the study. Reference Kao, Chang, Chiu, Wu and Tsai33,Reference Zaqout, Vandekerckhove, Michels, Bove, Francois and De Wolf43
Eight articles reported the use of hip-worn accelerometers, Reference Ewalt, Danduran, Strath, Moerchen and Swartz32–Reference Arvidsson, Slinde, Hulthén and Sunnegårdh35,Reference White, Willis and Panchangam38,Reference Voss, Duncombe, Dean, de Souza and Harris39,Reference Banks, Rosenthal and Manlhiot42,Reference Zaqout, Vandekerckhove, Michels, Bove, Francois and De Wolf43 whereas one reported using wrist-worn accelerometers. Reference Hedlund, Lundell, Villard and Sjoberg37
Considering the cut-points used for defining the physical activity intensity categories, three articles Reference Hedlund, Lundell, Villard and Sjoberg37–Reference Voss, Duncombe, Dean, de Souza and Harris39,Reference Zaqout, Vandekerckhove, Michels, Bove, Francois and De Wolf43 reported using Evenson Reference Evenson, Catellier, Gill, Ondrak and McMurray45 cut-points for classification of physical activity intensity categories, one article Reference Stone, Obeid, Dillenburg, Milenkovic, MacDonald and Timmons34 reported using Pate‘s Reference Pate, Almeida, McIver, Pfeiffer and Dowda46 cut-points, one article Reference Ewalt, Danduran, Strath, Moerchen and Swartz32 reported using age-appropriate intensity levels from a metabolic equivalent prediction equation Reference Freedson, Pober and Janz47,Reference Trost, Pate and Sallis48 for generating cut-points, one article Reference Banks, Rosenthal and Manlhiot42 reported using Puyau Reference Puyau, Adolph, Vohra, Zakeri and Butte49 cut-points but did not submit how the threshold of moderate-to-vigorous-physical-activity > 1600 counts per minute was calculated, one article Reference Arvidsson, Slinde, Hulthén and Sunnegårdh35 reported using the ActiReg monitor with calibration equation for predicting intensity measures developed and evaluated by Arvidsson et al, Reference Arvidsson, Slinde and Hulthén50 whereas one reported transferred accelerometer (RT3) originated energy expenditure as intensity measure. Reference Kao, Chang, Chiu, Wu and Tsai33
Similar physical activity levels were found between the patient group and the healthy controls in the majority of the included accelerometer-based studies. Reference Ewalt, Danduran, Strath, Moerchen and Swartz32–Reference Arvidsson, Slinde, Hulthén and Sunnegårdh35,Reference Hedlund, Lundell, Villard and Sjoberg37,Reference Voss, Duncombe, Dean, de Souza and Harris39,Reference Banks, Rosenthal and Manlhiot42,Reference Zaqout, Vandekerckhove, Michels, Bove, Francois and De Wolf43 In contrast, White et al Reference White, Willis and Panchangam38 reported that the CHD group spent significantly more time in light physical activity and less moderate-to-vigorous-physical-activity than the healthy controls, typically engaging in more sporadic bouts (<5 minutes), fewer short (5–10 minutes) and medium-to-long (>10 minutes) bouts of moderate-to-vigorous-physical-activity than the healthy controls. Similarly, Kao et al Reference Kao, Chang, Chiu, Wu and Tsai33 observed significantly lower levels of total energy expenditure in boys with CHD compared to healthy controls, even if the reported moderate-to-vigorous-physical-activity was similar between the groups.
The majority of the accelerometer-based studies reported that the patients with CHD generally failed to meet the World Health Organisation recommendations of physical activity in children and adolescents. Reference Ewalt, Danduran, Strath, Moerchen and Swartz32,Reference Stone, Obeid, Dillenburg, Milenkovic, MacDonald and Timmons34,Reference Arvidsson, Slinde, Hulthén and Sunnegårdh35,Reference Voss, Duncombe, Dean, de Souza and Harris39,Reference Zaqout, Vandekerckhove, Michels, Bove, Francois and De Wolf43 Banks et al Reference Banks, Rosenthal and Manlhiot42 recognised that the majority of the atrial septal defect patients met the recommendations of physical activity, but not the transposition of the great arteries, tetralogy of Fallot, or single ventricle patients; however, they did not state the proportions. Hedlund et al Reference Hedlund, Lundell, Villard and Sjoberg37 studied the physical activity in Fontan circulation patients and observed an average moderate-to-vigorous-physical-activity of 148 minutes/day in the patient group, stating that they meet the World Health Organisation recommendations of physical activity.
Discussion
The main observation from all of the included studies was the contradicting finding of similar physical activity levels in children and adolescents with CHD compared to healthy controls, or due to the severity of CHD. These results are in line with the previous two review studies. Reference Acosta-Dighero, Torres-Castro and Rodríguez-Núñez17,Reference van Deutekom and Lewandowski18 Van Deutekom and Lewandowski Reference van Deutekom and Lewandowski18 raised the concern about the low level of physical activity in the general population, which could affect the possibility of detecting different physical activity behaviour in children and adolescents with CHD. Although this might be true, we argue for that the contradicting findings and absence of group difference in physical activity are largely explained by the methodological variations and limitations in the assessment of physical activity. In order to comply with the second objective of this study, and as it is recommended to use objective methods before subjective methods for obtaining more reliable assessment of physical activity, Reference Longmuir, Brothers and De Ferranti15 the discussion will mainly focus on the accelerometer-based studies included.
Subjectively assessed physical activity
As measurement errors in subjectively assessed physical activity have been stated by earlier research, demonstrating poor reliability and validity, especially in children, Reference Longmuir, Brothers and De Ferranti15,Reference Sylvia, Bernstein, Hubbard, Keating and Anderson19,Reference Vanhees, Lefevre and Philippaerts20 a potential misclassification and a variation among the results are seen as probable. Reports of both no significant differences towards healthy controls, Reference Ray and Henry41 significantly lower physical activity, Reference Hedlund, Lundell, Villard and Sjoberg37,Reference Lunt, Briffa, Briffa and Ramsay40 and significantly higher physical activity in the patient group Reference Zaqout, Vandekerckhove, Michels, Bove, Francois and De Wolf43 were found. The inconsistent and widely divergent findings may be a result of all six articles using different questionnaires for the assessment of physical activity. Dissimilar properties of physical activity are thereby captured. Thus, stating general conclusions or even comparing the physical activity outcome is seen as inappropriate. A similar verdict was reported by Acosta-Dighero et al. Reference Acosta-Dighero, Torres-Castro and Rodríguez-Núñez17 and by Van Deutekom and Lewandowski. Reference van Deutekom and Lewandowski18
Accelerometer-assessed physical activity
Concerning the accelerometer-based studies, the overall results suggest that there are no differences in the physical activity levels between children and adolescents with CHD compared to healthy controls. Reference Ewalt, Danduran, Strath, Moerchen and Swartz32–Reference Arvidsson, Slinde, Hulthén and Sunnegårdh35,Reference Hedlund, Lundell, Villard and Sjoberg37,Reference Voss, Duncombe, Dean, de Souza and Harris39,Reference Banks, Rosenthal and Manlhiot42,Reference Zaqout, Vandekerckhove, Michels, Bove, Francois and De Wolf43 Similar finding was reported by Acosta-Dighero et al Reference Acosta-Dighero, Torres-Castro and Rodríguez-Núñez17 and by Deutekom and Lewandowski. Reference van Deutekom and Lewandowski18 Two of the studies showed contradicting results. Kao et al. Reference Kao, Chang, Chiu, Wu and Tsai33 reported lower total energy expenditure in boys with CHD, indicating that they move less than their healthy controls even if the reported moderate-to-vigorous-physical-activity was similar between the groups, whereas White et al. Reference White, Willis and Panchangam38 reported the patient group as spending less time in moderate-to-vigorous-physical-activity and engaging in smaller bouts of moderate-to-vigorous-physical-activity than the healthy controls. As the physical activity outcome is highly dependent on the distinct settings made, Reference Migueles, Cadenas-Sanchez and Ekelund28,Reference Kerr, Marinac and Ellis30,Reference Sirard and Pate51 a likely explanation of the many cases of the unexpected “no-difference in PA” between patients and healthy controls can be related to the irregularities in the methodologies used in and between the studies.
Common variances in accelerometer-based studies regard matters such as device placement, raw data processing, epoch lengths, value calibrations, altered use of pre-calibrated cut-points, weekend-weekday-criteria, number of valid days/hours-a-day/week, and handling of sleep-time and non-wear time. The handling of these parameters is often poorly described or completely lacking, making comparisons between studies even more problematic. The lack of methodological consensus within accelerometry makes it difficult, or even impossible, to generalise and compare the results. Reference Migueles, Cadenas-Sanchez and Ekelund28,Reference Kerr, Marinac and Ellis30,Reference Sirard and Pate51 In the following section, we will go through the methodological issues of the included studies and their consequences on the results. This will be performed by considering each issue separately.
Device placement
As the activities of the arm not necessarily reflect the movements of the rest of the body, the registered data differ between the hip- and wrist-worn placement sites. Reference Noonan, Boddy, Kim, Knowles and Fairclough52 Hip-worn sensors typically capture movements that better reflect the whole-body energy consumption, Reference Migueles, Cadenas-Sanchez and Ekelund28 while wrist-worn sensors have been shown to be disposed for misclassifying seated behaviours that are involving high levels of upper body movement. Reference Noonan, Boddy, Kim, Knowles and Fairclough52 One of the accelerometer-based studies used a wrist-worn accelerometer but applied physical activity intensity cut-points developed from a hip-worn accelerometer. Reference Hedlund, Lundell, Villard and Sjoberg37 The use of wrist-worn accelerometers and the application of hip-worn accelerometer cut-points to wrist data reduce both study validity and comparability to the other studies included in this review.
Epochs
The epoch lengths are ranging from 3 to 60 seconds in the included studies, with two of the studies failing to report the epoch length used. The occurring epoch-length variances (and in many cases long epoch lengths) may result in different estimates of physical activity within the studied populations and thereby lead to distorted interpretations. Previous research has stated significant variation in physical activity volume and intensity using various epoch lengths, showing a progressive decrease in time spent in moderate-to-vigorous-physical-activity with longer epoch lengths. Reference Aadland, Andersen, Anderssen, Resaland and Kvalheim29,Reference Sanders, Cliff and Lonsdale53–Reference Banda, Haydel and Davila55 Also, with the movement pattern of children being highly intermittent, shorter epoch lengths have been recommended as longer epochs fail to capture the executed physical activity. Reference Aadland, Andersen, Anderssen, Resaland and Kvalheim29,Reference Mcclain, Abraham, Brusseau and Tudor-Locke56,Reference Aadland, Andersen, Anderssen, Resaland and Kvalheim57 To demonstrate, in the study by White et al Reference White, Willis and Panchangam38 the results showed similar amount of total physical activity measured as ActiGraph counts per minute compared to the control group, similar time in sedentary behaviour (SED), more time in light physical activity but somewhat less time in moderate-to-vigorous-physical-activity. An epoch length of 60 seconds was used in that study. Aadland et al Reference Aadland, Andersen, Anderssen, Resaland and Kvalheim29 showed that with 60-second epochs, a large proportion of SED would be misclassified as light physical activity, and vigorous physical activity would be misclassified as light physical activity or moderate physical activity, but the total physical activity would not be affected. Hence, the 60-second epochs will not capture the variation in physical activity in children and would distort/reduce expected group differences.
Pre-calibrated cut-points
By calculating the relationship between accelerometer counts and the criterion value over a fixed time frame (epoch length), thresholds for the categorisation of physical activity (SED, light physical activity, moderate physical activity, vigorous physical activity, and moderate-to-vigorous-physical-activity) are generated. Numerous pre-calibrated cut-points exist, and there is no consensus in which one to use at what occasion, even if age-specific recommendations have been made Reference Migueles, Cadenas-Sanchez and Ekelund28 With the included articles using a variety of different cut-points, the classification of physical activity intensity categorisation varies largely between them. Banks et al Reference Banks, Rosenthal and Manlhiot42 used a moderate-to-vigorous-physical-activity threshold of >1600 counts per minute; Ewalt et al Reference Ewalt, Danduran, Strath, Moerchen and Swartz32 used age-specific calibrated cut-points for moderate-to-vigorous-physical-activity: 6–11 years = >1400 counts per minute, 12–15 years = 2221 counts per minute, and 16–19 years = 3001 counts per minute; Stone et al Reference Stone, Obeid, Dillenburg, Milenkovic, MacDonald and Timmons34 used Pate Reference Pate, Almeida, McIver, Pfeiffer and Dowda46 moderate-to-vigorous-physical-activity cut-points of >1680 counts per minute; Hedlund et al. Reference Hedlund, Lundell, Villard and Sjoberg37 Voss et al. Reference Voss, Duncombe, Dean, de Souza and Harris39 White et al, Reference White, Willis and Panchangam38 and Zaqout et al Reference Zaqout, Vandekerckhove, Michels, Bove, Francois and De Wolf43 used the Evenson cut-points Reference Evenson, Catellier, Gill, Ondrak and McMurray45 of >2296 counts per minute for the same physical activity intensity category. With different cut-points being applied, the easiness to accumulate moderate-to-vigorous-physical-activity differs between the studies, not displaying the same variations of physical activity within each physical activity intensity category even if results are presented in the same terminology. Pre-calibrated cut-points are population specific as body mass and age are important factors for the calculated mechanical energy used in accelerometry. Thus, when applying the cut-points, it is recommended to follow the same data gathering and processing criteria upon the same age group that was utilised in the original calibration study.
In many of the included studies using pre-calibrated cut-points, the age group is not compatible with the age group used in the original calibration study. Only one of the studies used the same age-criteria. Reference Stone, Obeid, Dillenburg, Milenkovic, MacDonald and Timmons34 Instead, Banks et al Reference Ray and Henry41 applied cut-points calibrated for 7–18 year old on a population of 4–12 year old, and the Evenson Reference Evenson, Catellier, Gill, Ondrak and McMurray45 cut-points calibrated for 5–8 year old, were applied to populations of 8–20 year old, Reference Hedlund, Lundell, Villard and Sjoberg37 8–19 year old, Reference Voss, Duncombe, Dean, de Souza and Harris39 8–18 year old, Reference White, Willis and Panchangam38 and 6–14 year old. Reference Zaqout, Vandekerckhove, Michels, Bove, Francois and De Wolf43 Consequently, with children generally moving with a bigger effort and a higher energy cost at a given activity than older (and taller) individuals, Reference Arvidsson, Fridolfsson and Buck58 the calibrated cut-points used indistinguishably between the age groups will cause false estimates of physical activity categorisation.
Modifications, or scaling, of pre-calibrated cut-points to fit the chosen epoch length are frequently seen in accelerometer-based research. However, a modification of cut-points alters physical activity estimates. Reference Mcclain, Abraham, Brusseau and Tudor-Locke56,Reference Hibbing, Bassett and Crouter59 Only one of the accelerometer-based articles used the same epoch setting as in the original calibration study. Reference Voss, Duncombe, Dean, de Souza and Harris39 Banks et al Reference Banks, Rosenthal and Manlhiot42 applied 15-second epochs on a cut-point calibrated for 60-second epochs, Ewalt et al Reference Ewalt, Danduran, Strath, Moerchen and Swartz32 applied 30-second epochs on a cut-point equation calibrated for 60-second epochs, Stone et al Reference Stone, Obeid, Dillenburg, Milenkovic, MacDonald and Timmons34 applied 3-second epochs on a cut-point calibrated for 15-second epochs, Hedlund et al Reference Hedlund, Lundell, Villard and Sjoberg37 applied 60-second epochs on a cut-point calibrated for 15-second epochs, White et al Reference White, Willis and Panchangam38 applied 60-second epochs on a cut-point calibrated for 15-second epochs, and Zaqout et al Reference Zaqout, Vandekerckhove, Michels, Bove, Francois and De Wolf43 did not report used epochs on a cut-point calibrated for 15-second epochs, leaving us only with speculations on the effect upon the result.
Taken the age, epoch length, and device placement criteria for the usage of pre-calibrated cut-points all together, the divergent settings will affect the between-study comparisons and decline the internal validity of the measure within each study.
Calibration of cut-points and inclusion of whole-spectrum physical activity
Metabolic equivalent of task (VO2total/VO2rest) is a frequently used criterion measure of absolute physical activity intensity and is a way of expressing the energy cost of task-specific physical activity relative to body mass. Two articles reported calibrating cut-points via energy expenditure equations of MPA corresponding to 3 metabolic equivalent of task Reference Arvidsson, Slinde, Hulthén and Sunnegårdh35 or 4 metabolic equivalent of task. Reference Ewalt, Danduran, Strath, Moerchen and Swartz32 Validating cut-points against indirect calorimetry can be problematic as metabolic equivalent of task-calibrated cut-points are not comparable between ages. Typically, a 3 metabolic equivalent of task value is set for calibration of moderate physical activity threshold in both children, adolescents, and adults. However, when children walk at a speed of 5.6 km/hour, a metabolic equivalent of task value of 4.3 is reached, Reference Harrell, McMurray, Baggett, Pennell, Pearce and Bangdiwala60 whereas adults typically reach a metabolic equivalent of task of 5.0 at the same speed. Reference Kozey, Lyden, Howe, Staudenmayer and Freedson61 However, the internal effort and energy cost of a child are greater. A child will consume more O2 per kg body weight, Reference Arvidsson, Fridolfsson and Buck58 moving with higher step frequencies than taller individuals at a given speed. Reference Schepens, Bastien, Heglund and Willems62,Reference Schepens, Willems, Cavagna and Heglund63 Adding the fact that the resting energy expenditure decreases with age Reference Herrmann, McMurray, Kim, Willis, Kang and McCurdy64 and metabolic equivalent of task values for specific activities typically increase with age (even more distinct at higher intensities), Reference Harrell, McMurray, Baggett, Pennell, Pearce and Bangdiwala60,Reference McMurray, Butte and Crouter65 the usage of metabolic equivalent of task as a measure of effort across age groups when calibrating cut-points can be distortive.
To enable direct comparison of age groups and achieve age-equivalent measures of physical activity intensity categories (e.g. light physical activity, moderate physical activity, vigorous physical activity, moderate-to-vigorous-physical-activity), the VO2net (VO2total – VO2stand, ml/kg/minute) has been recommended to use as criterion measure for calibration of accelerometers. Reference Arvidsson, Fridolfsson and Buck58 When a child (shorter) and an adolescent (taller) attain the same VO2net, they will move with the same metabolic effort, but with the child generating less acceleration (or less mechanical work) as moving at a slower speed than the adolescent. Hence, minutes spent in, for example, vigorous physical activity will be directly comparable between age groups from a metabolic effort perspective. In contrast, when a child and an adolescent move at the same speed, they will generate similar acceleration (or mechanical work) but with different metabolic efforts.
Nevertheless, the crude classification of physical activity used in all studies included might cause a potential loss of information from the collected acceleration data. Aadland et al Reference Aadland, Andersen, Anderssen, Resaland and Kvalheim57 showed how presenting physical activity as a high-resolution physical activity intensity spectrum provides more comprehensive information regarding the physical activity behaviour. By presenting physical activity as an intensity spectrum, the concern with studies using different cut-points is resolved.
Raw data filtration
Even if seen as more reliable than subjective measures, accelerometers have been shown to possess difficulties in capturing intermittent and high intensity physical activity, generating a decrease in counts even if activity is increasing (e.g. the “plateau” effect). Reference Brønd, Andersen and Arvidsson66,Reference John, Miller, Kozey-Keadle, Caldwell and Freedson67 The “plateau” occurs mainly as a result of the raw data frequency filtration in the original, most commonly used ActiGraph counts. Reference Brønd, Andersen and Arvidsson66 This is believed to be particularly applicable in the measurement of children as their general movement pattern is sporadic and highly intermittent, Reference Sanders, Cliff and Lonsdale53,Reference Aadland, Andersen, Anderssen, Resaland and Kvalheim57,Reference Trost, Ward, Moorehead, Watson, Riner and Burke68 moving with a higher step frequency at a given speed, Reference Arvidsson, Fridolfsson and Börjesson25,Reference Aadland, Andersen, Anderssen, Resaland and Kvalheim57,Reference Trost, Ward, Moorehead, Watson, Riner and Burke68 consequently reducing the acceleration signal ever further. Processing the acceleration through a wider filter improves the assessment of physical activity and reduces the age variances in gait patterns. Reference Fridolfsson, Börjesson and Arvidsson69,Reference Fridolfsson, Börjesson and Buck70 Notably, when compared towards broader filters, the ActiGraph counts showed a misclassification of >90% in the higher intensity spectra. Reference Fridolfsson, Börjesson and Buck70 Consequently, the capture of physical activity intensities is considerably more accurate when processing the acceleration through a wider filter. With the previous raw data filtration being insufficient, it is likely that the included studies failed to capture the variance in physical activity at higher intensity levels as interpretations of ActiGraph filtrated moderate-to-vigorous-physical-activity are highly unreliable. Therefore, a possible larger difference in physical activity might be present between the studied groups than the included studies imply, as they rely on the narrow ActiGraph raw data filtration.
Fulfillment of World Health Organisation physical activity recommendation
When it comes to fulfilling the World Health Organisation recommendation of ≥60 minutes per day of moderate-to-vigorous-physical-activity, 44 the included articles point towards an agreement: children and adolescents with CHD generally fail to meet the recommended amount of physical activity, a result similar to that of Acosta-Dighero et al Reference Acosta-Dighero, Torres-Castro and Rodríguez-Núñez17 and by Van Deutekom and Lewandowski. Reference van Deutekom and Lewandowski18 However, the World Health Organisation guidelines are based upon subjective measures of physical activity. The results from the accelerometer-based studies regarding physical activity recommendations should therefore be interpreted with caution as they are based on different, incomparable methods. Further, the chosen cut-points and epoch lengths will affect the ratio of individuals reaching the physical activity recommendations as lower cut-points and shorter epochs will accumulate more moderate-to-vigorous-physical-activity; conversably, higher set cut-points and longer epochs will accumulate less moderate-to-vigorous-physical-activity. Reference Migueles, Cadenas-Sanchez and Ekelund28,Reference Aadland, Andersen, Anderssen, Resaland and Kvalheim29,Reference Aadland, Andersen, Anderssen, Resaland and Kvalheim57 The fulfillment of the physical activity recommendation is also dependent on how strict the criteria are, that is, if attaining 60 minutes of moderate-to-vigorous-physical-activity on most days or as a daily average. For example, Voss et al Reference Voss, Duncombe, Dean, de Souza and Harris39 applied Evenson cut-points on 15-second epoch data and the stricter criteria of fulfilling the physical activity recommendation on most days; only 8% of the patients were sufficiently physically active.
Further, difficulties may arise when attempting to implement the World Health Organisation recommendations of physical activity for healthy individuals on children and adolescents with physical restrictions. The included articles contain a range of different types and severities of CHD, with various physician subscribed (former) recommendations for engagement in physical activity. Accelerometers measure absolute intensity, regardless of the intensity relative to fitness level. A moderate intensity level for an individual with a severe CHD might differ from the same physical activity level for a healthy individual. In addition, the cut-point for moderate intensity level might be set too low in general, corresponding to normal walking speed rather than to brisk walking speed in accordance with the original definition of moderate-intense physical activity. Reference Arvidsson, Fridolfsson and Börjesson71
In summary, the methodological challenges, variances, and limitations might explain why we generally fail to see a difference between the groups even when a larger difference in physical activity is to be expected. We need to control for the discussed parameters and strive towards agreement between the methods used for enabling future comparisons and interpretation of the results. As long as there is no consensus concerning accelerometer protocols and settings, research protocols will be designed unequally, making between-study comparisons highly questionable. To enable further research on the effect of interventions, strategies, and models for promoting physical activity in CHD populations, valid and reliable baseline measures of physical activity patterns in CHD populations are needed. Interdisciplinary collaborations are advantageous when implementing accelerometry into clinical research for assessing valuable and accurate assessments of physical activity and thereby improve the quality of clinical physical activity research.
Figure 2 (a-f) presents a brief overview of methodological considerations for tailoring a physical activity measure using accelerometers together with a case scenario with implementation of the methodological steps of the accelerometer study protocol. More detailed information, concepts, and guidelines are provided in Table 4. Complementary information about existing methods may be provided in the work by Voss and Harris. Reference Voss and Harris72

Figure 2. Brief methodological considerations for tailoring a physical activity measure using accelerometers and a case scenario.
Conclusion
Previous research has been unable to establish whether the physical activity patterns in children with CHD differ to healthy controls, or due to the severity of CHD. These results are largely explained by methodological variation and limitations in the assessment of physical activity. This review provides methodological knowledge and guidelines for improved assessment of physical activity using accelerometers in clinical research.
Acknowledgements
We thank Jonatan Fridolfsson, Center for Health and Performance, Department of Food and Nutrition, and Sport Science, Gothenburg University for supporting us with the figures.
Financial support
This research received no specific grant from any funding agency, commercial or not-for-profit sectors.
Conflicts of interest
None.
Ethical standards
None.









