INTRODUCTION
Salmonella enterica serovar Saintpaul (S. Saintpaul) accounted for 4·2–5·1% of Australian annual Salmonella notifications between 2003 and 2005 (Australian Government Department of Health and Ageing, National Notifiable Diseases Database, unpublished data.). Reports of infection with S. Saintpaul are more common in the northern states of Australia, Queensland and Northern Territory, and relatively uncommon in the remaining states. In Australia, foodborne outbreaks with this Salmonella serotype have previously been associated with the consumption of boiled eggs, untreated drinking water and bean sprouts [Reference Taylor1–3]. Internationally, S. Saintpaul outbreaks have been attributed to the consumption of paprika and paprika-flavoured potato chips, bean sprouts, hospital prepared formula and mangoes [Reference Beatty4–Reference O'Mahony7].
Salmonellosis outbreaks associated with the consumption of fresh produce have previously been uncommon in Australia. The Australian Commonwealth Government funds and coordinates OzFoodNet, a network of foodborne disease epidemiologists based in each of Australia's eight states and territories (jurisdictions), and maintains a national database of all reported foodborne disease outbreaks. Review of OzFoodNet outbreak data found only 15 outbreak reports implicating consumption of fresh produce between 2001 and 2005, representing 2·4% of all reported foodborne or suspected foodborne outbreaks. None of these outbreaks were associated with the consumption of cantaloupe (scientific name Cucumis melo L. var. reticulatus Naudin), which is also known as rockmelon [8]. Internationally, outbreaks of salmonellosis have been associated with the consumption of cantaloupes. A published review of the international literature and other data sources, for the period 1973–2002, identified 28 outbreaks associated with the consumption of cantaloupes, with 11 outbreaks (39%) caused by Salmonella spp. (S. Chester, S. Poona, S. Saphra, S. Oranienburg, S. Berta and Salmonella Group E1) [Reference Bowen9].
We describe the investigation of a large outbreak of S. Saintpaul, with 115 confirmed cases with the multiple locus variable-number tandem repeat analysis (MLVA)-defined outbreak-related strain, that occurred in six Australian jurisdictions with its epicentre in the south-eastern mainland jurisdictions of Australia (New South Wales, Victoria and Australian Capital Territory) between September and November 2006. In New South Wales a sudden increase in the number of human notifications of S. Saintpaul infection was detected through routine surveillance in late September 2006. Shortly after a national alert was issued, Victoria and the Australian Capital Territory also reported a higher number of notifications of S. Saintpaul infection than expected. In response, a multi-state public health investigation was initiated to identify the cause of the outbreak and risk factors for infection amenable to public health control measures.
METHODS
Hypothesis generation
Fourteen newly notified S. Saintpaul cases were interviewed with a standardized 7-day retrospective hypothesis generating and trawling questionnaire to identify possible foodborne and environmental risk factors for infection. Food exposures commonly reported by these cases were cantaloupe (n=11), cucumber (n=8), pear (n=8), grapes (n=8), strawberries (n=8) and cooked broccoli (n=8). These food items were consumed more frequently by cases than expected when compared with food consumption data for controls from an Australian Campylobacter case-control study [Reference Stafford10].
Epidemiological investigation
A multi-jurisdictional case-control study was initiated to test the hypothesis that S. Saintpaul infection was associated with the consumption of fresh produce items including cantaloupe. Cases were defined as an infection with the outbreak strain of S. Saintpaul isolated from a faecal specimen by MLVA on or after 6 October 2006 in residents of New South Wales, Victoria and the Australian Capital Territory. Cases were identified through routine passive notification. Two control recruitment methods were used with New South Wales and the Australian Capital Territory utilizing progressive/regressive digit dialling based on the case's telephone number to select four and three controls respectively, while Victoria recruited two controls for each case using a control bank comprising consenting respondents from a state-based population health survey. Controls were selected from the same broad age band as cases (<16 years or ⩾16 years), except in Victoria where ages were closely matched.
Cases were asked whether they had consumed cantaloupe, strawberries, grapes, pears, cucumber, beef mince, chicken or eggs (the food items identified during hypothesis-generating interviews), in the 4 days preceding onset of illness. For fruit and vegetable items they were asked whether these had been consumed alone, or in a mixed fruit juice or fruit salad. For each food item consumed, place and date of purchase and specific product handling information was sought. Identical questions were posed to controls for the 4-day period prior to interview. The three jurisdictions interviewed the cases and controls residing within their borders, and responses were entered onto NetEpi Case Manager, an open source software tool designed to allow for secure entry onto a web-based outbreak database [11].
Statistical analysis
Statistical analysis was conducted using Intercooled Stata version 8 [12]. Case and control demographic details were compared using Pearson's χ2 test for trend. Univariate analysis was used to calculate crude odds ratios (OR), with 95% confidence intervals (CI), for all exposures and risk factors. A maximum-likelihood logistic regression model was constructed using sequential backward elimination of variables to explore the association between food items and illness, adjusted for age group as frequency-matching was by age group <16 years or ⩾16 years, with food items that had a P value <0·1 in univariate analysis included in the model. As controls were age-matched in Victoria, matched analysis was also conducted to confirm findings.
Microbiological investigation
Patients with S. Saintpaul infection were identified by reference public health laboratories in New South Wales, Queensland, Victoria and South Australia. The same laboratories tested cantaloupe samples collected from retailers, wholesalers and processors implicated during the trace-back investigation.
All human isolates of S. Saintpaul serotyped in Australia prior to and during the outbreak period were subjected to the MLVA method adapted from Lindstedt et al. for S. Typhimurium [Reference Lindstedt13] to determine whether they were of the outbreak-specific strain.
Trace-back, sampling and environmental investigation
Information on the places and dates of cantaloupe purchase were used by food safety regulators in each affected jurisdiction to initiate trace-back investigations. Individual retailers' records were used to identify common suppliers. Samples of cantaloupe on the day of visit at retailers and their suppliers were submitted for microbiological analysis. Records from suppliers were used to attempt to identify processors and farms that may have been the original source of implicated product.
The investigation team observed production and packing practices, and reviewed documented quality assurance procedures at processing sheds and farms that were identified as the possible source of implicated cantaloupes during the trace-back investigation. Environmental and produce samples were collected from each premises and submitted for microbiological analysis.
RESULTS
Epidemiological investigation
There were 232 S. Saintpaul cases notified in Australia during the period 1 September–30 November 2006, compared with the 5-year average for the same period of 45·4 cases per year (2001–2005) (Australian Government Department of Health and Ageing, National Notifiable Diseases Surveillance Scheme data: Salmonella Saintpaul notifications 2003–2006).
Thirty-six consecutive cases with the outbreak strain and 106 matched controls were recruited into the case-control study, which was conducted from 25 October to 8 November 2006. The symptom profile of cases included diarrhoea (100%), fever (86%), abdominal cramps (69%), vomiting (53%), headache (42%), bloody diarrhoea (36%), nausea (39%) and muscle/body aches (36%). The median duration of illness was 7 days (range 3–28 days), with nine cases (33%) requiring hospitalization. The median age for cases was 10 years (range 1–86 years), with males representing 44·4% of cases. There was no statistical difference between age group or sex for cases and controls (Table 1).
Table 1. Characteristics of cases and controls recruited into the Salmonella Saintpaul study, Australia, 25 October–8 November 2006
Univariate analysis
Cases were significantly more likely to have consumed cantaloupe (OR 14·60, 95% CI 5·50–40·20) during the 4-day exposure period compared with controls. The association between illness and cantaloupe consumption was found for each jurisdiction and remained statistically significant (Table 2). Seventy-two percent (26/36) of cases recollected cantaloupe consumption compared to 55% (20/36) for strawberry consumption, which demonstrated the second largest odds ratio. S. Saintpaul infection was not associated with the consumption of strawberries, raw broccoli, cucumber, pears, grapes, chicken, mince or eggs, either on their own, or, for the fruit items, as part of a mixed fruit juice or fruit salad. No association was found between S. Saintpaul illness and the nature of cantaloupe at purchase; half or whole fruit and refrigerated or unrefrigerated. No association was found between S. Saintpaul illness and whether it was stored refrigerated or unrefrigerated in the case's home; how it was prepared at home or whether it was consumed with skin removed or not removed.
Table 2. Association between food items, risk factors and Salmonella Saintpaul infection: case-control study, Australia, 25 October–8 November 2006

OR, Odds ratio; CI, confidence interval.
When examining associations in the two age groups (<16 years and ⩾16 years), we found that cases aged <16 years were significantly more likely to have consumed cantaloupe (OR 17·0, 95% CI 4·3–78·8), cantaloupe as part of a fruit salad (OR 10·0, 95% CI 1·6–72·6), and strawberries (OR 3·8, 95% CI 1·2–13·3) during the 4-day exposure period than controls, whilst for cases aged ⩾16 years, consumption of cantaloupe (OR 7·1, 95% CI 1·7–31·3) was the only variable where a statistically significant association between exposure and illness was identified (Table 2).
Multivariate analysis
Cantaloupe (on its own and as fruit salad), strawberries (on their own and as fruit salad), pears, gender, jurisdiction and age group were included in a multivariate model. After adjusting for these factors, only consumption of cantaloupe (adjusted OR 23·9, 95% CI 5·1–112·4) was found to be significantly associated with illness. This result was not affected by age-matched analysis.
Microbiological investigation
The outbreak strain of S. Saintpaul (MLVA pattern: 01-11-00-00-05) was identified as being distinct from other strains of S. Saintpaul that were circulating prior to and after the outbreak, from January 2003 to December 2006. During the outbreak, 115 patients in six jurisdictions were confirmed as having the outbreak strain of S. Saintpaul (Fig. 1). Since the outbreak in 2006, notified cases of S. Saintpaul have returned to baseline level.
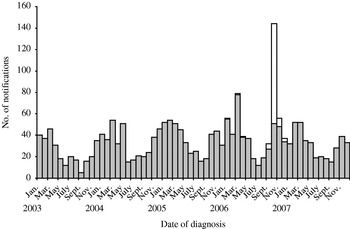
Fig. 1. Salmonella Saintpaul notifications in Australia, including those cases with the outbreak strain, 2003–2007. □, Outbreak strain; ![]() , non-outbreak strains.
, non-outbreak strains.
Trace-back investigation
Thirty-three of the 36 cases confirmed with the outbreak strain of S. Saintpaul included in the case-control study were able to identify the point of sale of cantaloupe purchased prior to their onset of illness. Unfortunately mingling of cantaloupe from different processors, poor documentation by some retailers and suppliers, poor traceability of fresh produce and limited recall by some cases of the places and dates of their cantaloupe purchase complicated trace-back. As no single primary source could be reliably implicated, the six processors from two jurisdictions, Queensland and Northern Territory, that had supplied produce to the various points of sale identified by cases at the time of their purchase, were all inspected.
In total, 141 samples of whole cantaloupe, three half-cantaloupes and one cantaloupe piece were tested during the trace-back investigation and S. Saintpaul was detected on the skin of two cantaloupes (one whole/one half-cantaloupe) obtained from a single point of sale identified by a case. The MLVA profiles of these isolates were identical to isolates from human cases. The cantaloupes supplied to this outlet, both at the time of purchase by the case and at the time of sampling, were grown and processed in the Northern Territory. In addition, S. Oranienburg and S. Orion were detected on two samples of cantaloupe grown and processed in Queensland.
Environmental investigation
Environmental investigations with microbiological sampling were performed at the six processors in the two jurisdictions supplying cantaloupes to implicated outlets at the time of the outbreak.
Fifty-nine environmental samples, including water, soil, fertilizers, organic material, dust, and swabs from equipment, and cantaloupe samples were collected during the investigation of farms and processors in the two jurisdictions. Salmonella spp. were detected in 13 samples from two sites, one in each jurisdiction, although S. Saintpaul was not detected in these samples (Table 3).
Table 3. Source of environmental samples with Salmonella spp. detected

The environmental investigations in both jurisdictions identified a number of critical food safety issues during the production and processing of cantaloupes that may have contributed to the contamination of fresh produce. These included the use of untreated or inadequately treated water on ready-to-eat cantaloupes; processors not using disinfectants according to manufacturers' instructions; temperature differentials between the fruit and wash water in which they were immersed; and processing of bruised or damaged fruits. Despite all processors having a documented quality assurance programme additional problems detected included incomplete record-keeping; presence of cattle feed bins in cantaloupe-packing sheds; cracked bore-casings on bore heads; and apparent limited appreciation of the purpose of quality assurance processes amongst growers and processors as assessed through informal discussion.
DISCUSSION
We report the first Australian Salmonella outbreak associated with the consumption of cantaloupe. The multi-state outbreak investigation coordinated by OzFoodNet identified a strong epidemiological association between S. Saintpaul infection and consumption of cantaloupe, with cases being 23 times more likely to have consumed cantaloupe in the 4 days prior to onset of illness than controls. This is supported by the detection of the outbreak strain of S. Saintpaul on the skin of two Northern Territory cantaloupes sampled from the retail venue where a case had purchased cantaloupe. However, S. Saintpaul was not isolated from environmental samples collected as part of the environmental investigation, nor was the mechanism for contamination specifically identified, which is not surprising given the ~1 month delay between cantaloupe harvesting and environmental investigation/sampling.
Although the environmental investigation was unable to identify precisely where the contamination of cantaloupes implicated in the outbreak occurred, the identification of Salmonella serotypes in environmental samples and the food hygiene and safety issues that were commonly identified in both the Northern Territory and Queensland suggest that opportunities for contamination existed before and during harvesting, and during whole cantaloupe processing, packaging or storage. Although the farms and processors had quality assurance programmes in place, it appears likely that current processes are ineffective in reducing microbiological contamination. The use of untreated water for surface irrigation and washing of cantaloupes, the potential for contamination of product in the field, temperature differentials between the fruit and wash water in which they are immersed that could facilitate transmigration of organisms from the surface to the interior of the fruit, and processing of bruised or damaged fruits found during the environmental investigation have previously been shown to facilitate the attachment and infiltration of pathogenic bacteria, including Salmonella spp. [Reference Bowen9, Reference Stine14–Reference Richards and Beuchat17].
The surface texture of cantaloupe rind provides an ideal surface for attachment of bacteria, due to irregular lenticles which create a net-like pattern on the skin of the fruit [Reference Ukuku and Fett18]. When open, the lenticles may provide ideal habitats for colonization by microorganisms while providing protection to bacteria against disinfection [Reference Gagliardi19]. Pathogens may be introduced into the flesh of the cantaloupe when the rind is bruised or damaged. When cantaloupe wounds were inoculated with S. Poona (a Salmonella serovar associated with cantaloupe outbreaks in the United States), the pathogen was found to have migrated to a depth of 3–4 cm into the tissue after 7 days [Reference Richards and Beuchat16].
Storage time and temperature of potentially contaminated cantaloupes by wholesalers, retailers and consumers may also facilitate the growth of Salmonella spp. (including S. Saintpaul) on the rind or flesh of cantaloupe. Richards et al. recovered S. Poona from the rinds of intact cantaloupes stored up to 21 days at 4°C or up to 14 days at 20°C [Reference Richards and Beuchat17]. Contaminated cantaloupes may also serve as a source of cross contamination for other ready-to-eat fruit and vegetables, both in the retail and home environment [Reference Ukuku and Sapers20, Reference Ukuku, Pilizota and Sapers21]. This may explain why 28% (n=10) of cases with the outbreak strain of S. Saintpaul could not recall consuming cantaloupes or product containing cantaloupe in the 4 days prior to illness onset.
During the outbreak the Australian public were advised through media releases and interviews not to purchase bruised or damaged cantaloupe, refrigerate cut melons, discard cut fruit if left at room temperature for more than 2 h and avoid cross-contamination in the kitchen.
This study has several limitations. Recall of cases is always a concern in retrospective case-control studies, and in the current study may have led to an underestimate of the true association between salmonellosis and consuming cantaloupes, as the median delay from illness onset to interview of cases was 19 days (range 11–33 days). This delay was attributable to the time taken to access a medical doctor or hospital, and delays in specimen submission, laboratory identification and reporting. To optimize recall by controls, food exposure was restricted to the 4 days prior to the interview, and the seasonal nature of fresh produce may have influenced consumption patterns.
The trace-back investigation was impeded by case recall of date and place of purchase of cantaloupes, mingling of produce from different processors at the wholesale and retail level, relatively poor record-keeping throughout the supply chain and limited product labelling. The specific source of contamination could not be identified due to the time delay between harvesting and the environmental investigation.
Although this is the first documented outbreak of gastrointestinal illness associated with cantaloupe consumption in Australia, this food item has been implicated in outbreaks in the United States [22, Reference Mohle-Boetani23]. It appears that the association of Salmonella infection with cantaloupes is not limited to a single country or growing region but is rather related to the methods of production and harvesting of cantaloupes which may lead to contamination. This was one of four salmonellosis outbreaks detected in Australia during 2006 associated with the consumption of fresh produce items [3].
Currently, there is no national food safety legislation governing the production and processing of fresh produce, including cantaloupes, in Australia. Food Standards Australia New Zealand is in the process of developing standards to address this recently recognized local public health threat [24]. It is clear that guidelines for limiting food safety risks associated with cantaloupes are required. While consumers should be encouraged to consume fresh fruit and vegetables to maintain a healthy lifestyle, readily available advice at the point of purchase is needed to guide consumers on appropriate storage and preparation of these products. Thus, an approach from production to consumption is required to prevent future outbreaks of foodborne disease associated with cantaloupes.
ACKNOWLEDGEMENTS
The authors thank the following individuals who assisted in the outbreak investigation (in alphabetical order): Frank Beard, Robert Bell, Kerry Bell, Julie Burke, Robert Chiew, Susie Collins, Nick Corones, Barry Coombs, Alison Crombie, Victor DiPaola, Emily Davis, Ballant Eyeson-Annan, Tenille Fort, James Fielding, Kathleen Fullerton, Michelle Harlock, Geoff Hogg, Peter Howard, Jenny Jackson, Rick Jacobson, Eric Johnson, Martyn Kirk, Rod Knutson, Karin Lalor, Diane Lightfoot, Christopher Luthy, Peter Markey, Ian Marshall, Ian McKay, Tony Merritt, Lillian Mwanri, Annie Ng, Rhonda Owen, Beverley Parker, Simone Pozanski, Mark Salter, Cameron Sault, Russell Stafford, Nicola Stephens, Peter Sutherland, Lisa Szabo, Agnes Tan, Kirsten Tanner, Mary Valcanis, Christopher Villavicencio and Ian Wells. A limited review of the Victorian state data was published in a local public health bulletin, the Victorian Infectious Diseases Bulletin, as a short report.
DECLARATION OF INTEREST
None.






