Obsessive–compulsive disorder (OCD) has similar prevalence rates across the World. Reference Fontenelle, Mendlowicz and Versiani1,Reference Ruscio, Stein, Chiu and Kessler2 Within Western countries, including the UK, the prevalence of OCD has been shown to be roughly consistent across ethnic groups. For example, the Ethnic Minority Psychiatric Illness Rates in the Community (EMPIRIC) study Reference Weich, Nazroo, Sproston, McManus, Blanchard and Erens3,Reference Sproston and Nazroo4 examined the prevalence of mental disorders across adult British White, Black Caribbean, Indian, Pakistani, Bangladeshi and Irish ethnic groups. A similar point prevalence of OCD of around 1% was found across all ethnicities. Heyman et al Reference Heyman, Fombonne, Simmons, Ford, Meltzer and Goodman5 conducted a nationwide (UK) epidemiological survey to establish the prevalence of OCD in young people aged 5–15 (n>10 000) and reported a significantly greater proportion of children from ethnic minorities among those with OCD (24%) compared with healthy controls (8.8%) and psychiatric controls (7.4%). Given the similar, if not higher, prevalence of OCD across ethnic groups in Britain Reference Weich, Nazroo, Sproston, McManus, Blanchard and Erens3–Reference Heyman, Fombonne, Simmons, Ford, Meltzer and Goodman5 and elsewhere, Reference Himle, Muroff, Taylor, Baser, Abelson and Hanna6 a proportional representation of different ethnic groups would be expected in mental health services. However, there is substantial evidence to indicate that patients from ethnic minorities, both children Reference Goodman, Patel and Leon7 and adults, Reference Cooper, Spiers, Livingston, Jenkins, Meltzer and Brugha8 tend to be underrepresented in mental health services in Britain, although data specifically relating to OCD is lacking. Research conducted in North America suggests that patients with OCD from ethnic minorities are underrepresented in clinical trials. Williams et al Reference Williams, Powers, Yun and Foa9 reviewed 21 randomised controlled trials of OCD conducted in North America and found that ethnic minorities were seriously underrepresented in such studies (91% of participants were White). As OCD has rarely been studied separately, there is little data relating specifically to ethnic inequalities in access to clinical services of this major, yet treatable, psychiatric disorder. The overall aim of the present study was to explore whether individuals with OCD from ethnic minorities are underrepresented in secondary and tertiary clinical services within a large mental health trust in South London, relative to the ethnic composition of the corresponding catchment area. We also aimed to determine whether ethnic inequalities, if found, are restricted to a particular age group (children v. adults) or type of clinical service (community mental health clinics v. specialist clinics) or specific to OCD (compared with depression).
Method
Study setting
The South London and Maudsley (SLaM) NHS Foundation Trust is Europe's largest specialist mental healthcare trust. It serves a population of approximately 1.2 million residents of four South London boroughs: Lambeth, Southwark, Lewisham and Croydon. A proportion of SLaM services are tertiary care national referral units, Reference Stewart, Soremekun, Perera, Broadbent, Callard and Denis10 including three national specialist clinics for OCD: the Clinic for Young People with OCD and Related Disorders (Maudsley Hospital; child and adolescent out- and in-patients), the Centre for Anxiety Disorders and Trauma (CADAT; Maudsley Hospital, adult out-patients) and the Anxiety Disorders Residential Unit (ADRU; Bethlem Royal Hospital, adult in-patients).
The SLaM Biomedical Research Centre (SLaM BRC) Case Register is a data resource containing de-identified electronic records of all secondary and tertiary mental healthcare service users from SLaM. The Clinical Record Interactive Search (CRIS) is a program which automatically and effectively de-identifies full clinical records derived from the electronic clinical records system in SLaM, Reference Fernandes, Cloete, Broadbent, Hayes, Chang and Jackson11 enabling researchers to search and retrieve de-identified data from these electronic medical records that include over 180 000 individuals. Of these, approximately 35 000 are receiving active care from SLaM at a given time. CRIS was established in 2006 but contains some information that goes back to 1999 as, at its implementation, data from previous electronic records were migrated into the system. The protocol for this case register has been described in detail elsewhere. Reference Stewart, Soremekun, Perera, Broadbent, Callard and Denis10 CRIS has been used in numerous research studies. Reference Chang, Hayes, Perera, Broadbent, Fernandes and Lee12–Reference Chang, Hayes, Broadbent, Fernandes, Lee and Hotopf15 CRIS was approved as a data-set for secondary analysis by Oxfordshire Research Ethics Committee C (reference 08/H0606/71). Approval for the present study was sought and obtained from the CRIS Oversight Committee.
Participant cohorts
Diagnoses recorded in CRIS are based on the ICD-10 16 and reflect diagnoses assigned in routine practice by clinicians within SLaM. For the present study, the variable that defined the main cohort was at least one diagnosis of OCD (F42; either as primary or secondary diagnosis) made during the study period (1999–2013). In order to test the specificity of the results for OCD, we also defined a cohort of patients with at least one diagnosis of a depressive episode or recurrent depressive disorder (F32–F33) during the study period. All individuals with OCD or depression were included, regardless of comorbidity.
Other relevant variables were retrieved for both cohorts of participants, including ethnic background, date of birth, date at diagnosis, clinical services where they had been seen and postcode. In order to avoid the identification of individuals, only the month and year of birth (but not the day) and the first part of the post-codes corresponding to the broad geographical area (but not the second part that normally corresponds to a street, part of a street or single address) are available in CRIS. These variables are routinely recorded on SLaM electronic patient records in designated fields. For the OCD cohort, individuals were classified as currently being seen (or last contact) by local community services or at any of the three above-mentioned national, specialist OCD services.
Participants in all cohorts who did not have information about their ethnic background (i.e. value for the variable was missing or coded as ‘not stated’) were excluded from the analyses. Those who were from outside the catchment area (i.e. coming from other London boroughs or other locations in the UK) were also excluded in order to allow a fair comparison with the population data from the local catchment area.
Ethnic groupings
The ethnic composition of the population covered by SLaM (London boroughs of Lambeth, Southwark, Lewisham and Croydon) during the studied time frame (i.e. 1999–2013) was obtained from the London 2001 Census 17 and the London 2011 Census. 18 As the 2011 Census contained a slightly higher proportion of ethnic minorities, compared with the 2001 Census (45% in 2011 v. 34% in 2001), Reference Stewart, Soremekun, Perera, Broadbent, Callard and Denis10,18 we averaged the number of inhabitants from each ethnic group in the two Censuses to obtain a more accurate approximation of the population composition during the 14-year study period.
Ethnic groupings in both Censuses are virtually identical, with the exception that the Chinese group was included under the category ‘Any other group’ in the 2001 edition and moved to the ‘Asian’ category in the 2011 Census. 17,18 For the purposes of this study, we operationalised the ethnicity variable to match the ethnic groups as defined by the London 2011 Census (i.e. the Chinese group was included in the Asian group). Ethnic classification is fraught with problems as country of origin is compared with skin colour. Both the Censuses and CRIS use a detailed classification, but in order to make a direct comparison, we collapsed these categories. The five different categories encompassing the 15 ethnic groups included in CRIS were the following: (a) White (including British, Irish and any other White background groups); (b) Mixed/multiple ethnic groups (including White and Black African, White and Asian, and any other mixed background groups); (c) Asian/Asian British (including Indian, Pakistani, Bangladeshi, Chinese and any other Asian background groups); (d) Black/African/Caribbean/Black British (including African, Caribbean and any other Black background groups); and (e) any other ethnic group.
Data analyses
Data from CRIS was retrieved in March 2013 and downloaded onto a spreadsheet for data analyses. Frequencies and percentages for each ethnic group were calculated in all cohorts of clinical diagnoses. Next, the number of new mental health service users per 100 000 inhabitants year was calculated for each cohort during the 14-year time frame. For example, there were 1188 new White OCD service users from an average population of 696 836 White inhabitants during the 14-year period. Thus, 1188 new service users/696 836 inhabitants/14 years × 100 000 = 12.2 new White service users with OCD per 100 000 inhabitants year. Finally, the numbers of new mental health service users per 100 000 inhabitants year from each ethnic minority were compared with that of the White group by calculating the per cent difference and its confidence interval.
Results
Ethnic distribution in OCD
A total of 2677 patients meeting ICD-10 criteria for OCD were identified in the CRIS records. Of these, 235 did not have information about their ethnic background (missing or coded as ‘not stated’) and were excluded from the analyses. Another 914 individuals were from outside the catchment area and were also excluded. Thus, a final sample of 1528 individuals with OCD was included in all further analyses (Fig. 1).

Fig. 1 Selection of participants with obsessive–compulsive disorder and depression.
Individuals with the ethnic group missing or not stated, as well as those out of the South London and Maudsley (SLaM) NHS Foundation Trust catchment area were excluded. CRIS, Clinical Record Interactive Search.
Table 1 and Fig. 2 show the ethnic composition of the OCD cohort as well as the ethnic composition of the catchment area based on the 2001–2011 censuses. Overall, there was an obvious discrepancy in the proportion of patients with OCD who were White v. Black and minority ethnic (BME) in the CRIS register (78% v. 22%, respectively), compared with the expected proportions in the catchment area (60% v. 40%, respectively). This same pattern was observed independently of the type of clinical setting, whether the individuals were treated in community clinical services (Tier 3) or in child and adolescent or adult national and specialist services (Tier 4) (Table 1).
TABLE 1 Ethnic distribution of the population of the South London and Maudsley (SLaM) NHS Foundation Trust catchment area (Censuses 2001 and 2011) and obsessive–compulsive disorder and depression service users during the 14-year time frame: 1999–2013 a

| n (%) | ||||||
|---|---|---|---|---|---|---|
| ICD-10 psychiatric disorder | ||||||
| Obsessive-compulsive disorder (F42) | ||||||
| Ethnic group | Average population
in the SLaM catchment area during the studied time frame a |
All services,
community and national and specialist services |
Community services |
Child and adolescent
national and specialist services (only SLaM area) |
Adult national and
specialist services (only SLaM area) |
Depression (F32–F33) |
| White | 696836 (60.0) | 1 188 (77.7) | 774 (76.6) | 166 (80.2) | 248 (79.7) | 15429 (67.9) |
| Black and minority ethnic | 463752 (40.0) | 340 (22.2) | 236 (23.3) | 41 (19.8) | 63 (20.2) | 7287 (32.2) |
| Black | 269279 (23.2) | 129 (8.4) | 90 (8.9) | 17 (8.2) | 22 (7.1) | 3945 (17.4) |
| Asian | 107867 (9.3) | 89 (5.8) | 62 (6.1) | 11 (5.3) | 16 (5.1) | 1 173 (5.2) |
| Mixed | 65000 (5.6) | 31 (2.0) | 21 (2.1) | 1 (0.5) | 9 (2.9) | 267 (1.2) |
| All other ethnicities | 21 607 (1.9) | 91 (6.0) | 63 (6.2) | 12 (5.8) | 16 (5.1) | 1 902 (8.4) |
a. Percentages do not always add to 100.0% because of rounding.
b. Average of the London 2001 and 2011 Census. Includes boroughs of Lewisham, Croydon, Southward and Lambeth.
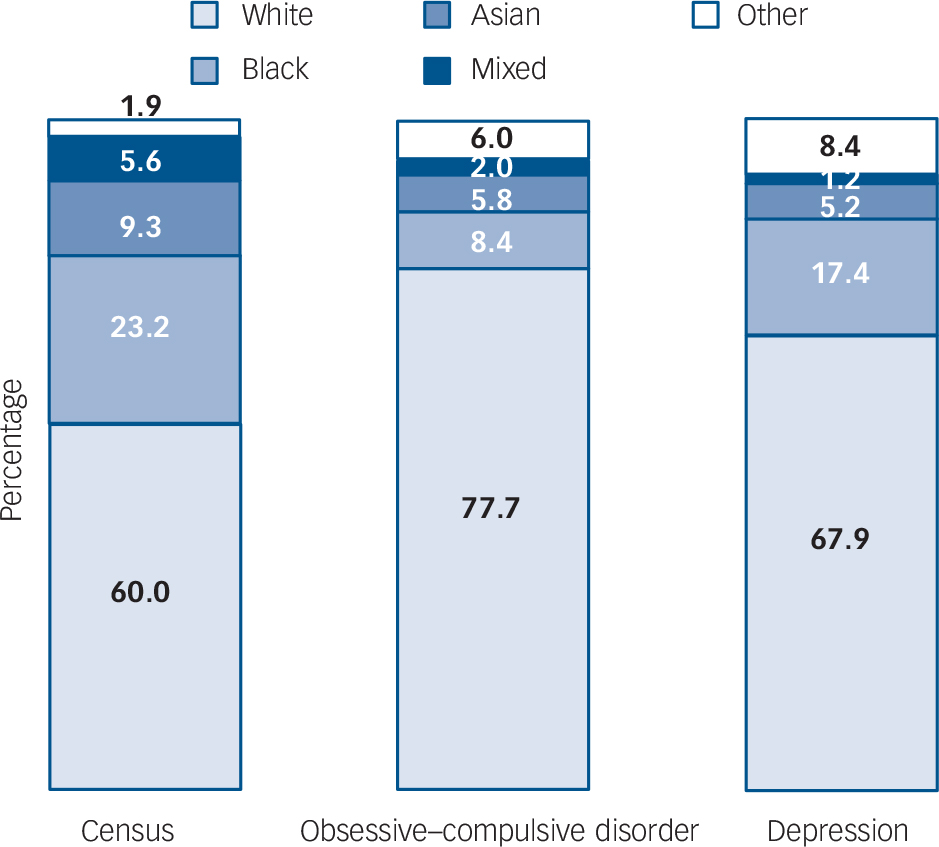
Fig. 2 Ethnic distribution of the population of the South London and Maudsley (SLaM) NHS Foundation Trust catchment area (Censuses 2001 and 2011) and obsessive–compulsive disorder and depression service users during the 14-year time frame: 1999–2013.
Percentages do not always add to 100.0% because of rounding.
Table 2 shows the number of new service users per 100 000 inhabitants year by ethnic group in both the White and BME groups. The per cent difference in relation to the reference (White) ethnic group in the use of services is also shown for each ethnic group. The number of new service users with OCD per 100 000 inhabitants year was 57% (95% CI 51.5–61.9%) lower in the BME group compared with the White group (Table 2). This pattern was particularly pronounced for patients from Black (−71.9%, 95% CI −76.6 to −66.3%) and Mixed (−72.0, 95% CI −80.4 to −60.0%) backgrounds, and somewhat less pronounced in patients from Asian backgrounds (−51.6, 95% CI −61.0 to −40.0%). The findings were largely constant across different types of clinical settings, with substantially lower proportions of patients in the BME group in community services, child and adolescent national and specialist services, and adult national and specialist services (Table 2).
TABLE 2 New service users per 100 000 inhabitants year in the different services for obsessive–compulsive disorder (OCD) and depression in the South London and Maudsley (SLaM) NHS Foundation Trust and per cent difference of the Black and minority ethnic group in relation to the reference (White) ethnic group

| ICD-10 psychiatric disorder | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Obsessive-compulsive disorder (F42) | Depression (F32-F33) | ||||||||||
| Average population in
the SLaM catchment area during the studied time frame a |
All services, community and national and specialist services |
Community services | Child and adolescent national and specialist services (only SLaM area) |
Adult national and specialist services (only SLaM area) |
|||||||
| Ethnic group | New
service users per 100 000 inhabitants year |
Per cent difference
in relation to the White ethnic group (95% CI) |
New
service users per 100 000 inhabitants year |
Per cent difference
in relation to the White ethnic group (95% CI) |
New
service jsers per 100 000 inhabitants year |
Per cent difference
in relation to the White ethnic group (95% CI) |
New
service users per 100 000 inhabitants year |
Per cent difference
in relation to the White ethnic group (95% CI) |
New
service users per 100 000 inhabitants year |
Per cent difference
in relation to the White ethnic group (95% CI) |
|
| White | 696 836 | 12.2 | – | 7.9 | – | 1.7 | – | 2.5 | – | 158.2 | – |
| Black
and minority ethnic |
463 752 | 5.2 | −57.0% (−61.9 to −51.5%) |
3.6 | −54.2% (−60.4 to −47.0%) |
0.6 | −62.9% (−73.6 to −47.8%) |
1 | −61.8% (−71.1 to −49.7%) |
112.2 | −29% (−31.0 to −27.0%) |
a. Average of London 2001 and 2011 Censuses. Includes boroughs of Lewisham, Croydon, Southwark, and Lambeth.
Ethnic distribution in depression
The psychiatric control cohort consisted of a total of 22 716 individuals with depression (Fig. 1). The proportion of each ethnic group in this comparison cohort is shown in Table 1 and in Fig. 2. Table 2 shows the number of new service users with depression per 100 000 inhabitants year by ethnic group, and the per cent difference in relation to the reference (White) group. The number of new service users with depression per 100 000 inhabitants year was also lower in the BME group than in the White group (29%, 95% CI 27.0–31.0 lower).
Discussion
Main findings
The present study aimed to explore whether individuals with OCD from ethnic minorities were underrepresented in secondary and tertiary care clinics of a large mental health trust, compared with the ethnic distribution of the local catchment area. In line with our clinical impression and data from North American clinical trials, Reference Williams, Powers, Yun and Foa9 the results confirmed that individuals from ethnic minority groups were significantly underrepresented in this clinical population. This is at odds with the fact that OCD is at least as prevalent in individuals from ethnic minorities as it is in the White majority. Reference Weich, Nazroo, Sproston, McManus, Blanchard and Erens3–Reference Heyman, Fombonne, Simmons, Ford, Meltzer and Goodman5
The observed inequalities were not specific to a particular age group (child and adolescent v. adult services) or type of service (community v. national specialist services), although the over-representation of people from White backgrounds was slightly higher in national and specialist services. The fact that underrepresentation of patients from ethnic minority backgrounds was comparable in community and national specialist clinics suggests that there are no specific barriers associated with the complexities of national specialist services; rather, the barriers seem broader and apply to secondary and tertiary mental health services in general. Because our catchment area is particularly rich in ethnic minorities (60% v. 86% White people in the SLaM catchment area compared with the whole of England and Wales), 19 our results may not generalise to other parts of the UK. However, our findings are well in line with other studies that have found that ethnic minorities are underrepresented in mental health services across Britain, Reference Goodman, Patel and Leon7,Reference Cooper, Spiers, Livingston, Jenkins, Meltzer and Brugha8 as well as in the USA. Reference Alegria, Canino, Rios, Vera, Calderon and Rusch20–Reference Manseau and Case24
Overall, our findings are partially consistent with those of a study by Manseau & Case Reference Manseau and Case24 who found that non-Hispanic Black individuals were treated markedly less frequently than their White counterparts for anxiety disorders – particularly OCD – as well as for dysthymia, personality disorders, nicotine use disorder, and attention-deficit hyperactive disorder in adult out-patient physician offices and hospital-based clinics in the USA. However, comparisons between the two studies are difficult because of context differences (i.e. USA v. UK) and the inclusion of different ethnic groups (i.e. White non-Hispanics, Black non-Hispanics and Hispanics).
Interestingly, the observed ethnic inequalities were significantly more pronounced in OCD compared with the depression control group, highlighting important challenges that seem specific to OCD. Depression may be more visible and easily detected or may be linked to increased risk of self-harm or suicide, potentially promoting referral to mental health services.
Possible explanations for the ethnic differences
The reasons why patients with OCD from ethnic minorities are so clearly underrepresented in our clinical population are unknown. The ethnic differences in prevalence ratios are too modest to explain the inequalities in the use of services and access to treatment. Possible explanations include that OCD is perceived by ethnic minorities as being a less impairing disorder so they do not seek help for its symptoms. However, there is little evidence to date that would indicate this. Alternatively, it is also possible that the embarrassing and sometimes taboo nature of the symptoms in OCD may be associated with higher levels of shame and stigma in some ethnic groups because of the way they perceive psychiatric services, making it more difficult for people with OCD to seek help. It is also possible that the explanatory models (i.e. patient's understanding of the illness) of the patients from ethnic minorities may well be different and these need to be explored further. It is possible that some ritualistic behaviour may get subsumed under religious rituals and thus not be seen as clinical problems. Furthermore, individuals from ethnic minorities may be more likely to seek help from resources other than mental health services (for example elder relatives, religious institutions or community) or the way they come into contact with services may vary. Reference Hatch and Thornicroft25 Urgent research is needed on pathways into secondary and tertiary care for these conditions to determine where and when help is sought. Future research should also investigate if the inequalities reported here are also present in primary care settings.
The low number of referrals to secondary and tertiary mental health services in the ethnic minority groups could be because of primary care clinicians not detecting the symptoms of OCD in this population. Although, as already mentioned, rates of OCD across ethnicities may be similar, some reports, specifically focused in the Black minorities, suggest that their clinical presentation might be slightly different. Reference Guarnaccia and Friedman26–Reference Karadag, Oguzhanoglu, Ozdel, Atesci and Amuk28 Himle et al Reference Himle, Muroff, Taylor, Baser, Abelson and Hanna6 found that Black Americans were more likely to have a later age at onset (31.8 years v. 19.5 years in the general population). They also found that once Black patients met criteria for OCD, they were very unlikely to experience remission, partly because of the limited access to state-of-the-art treatments. Sussman Reference Sussman29 pointed out that patients who present with less common OCD symptoms may not be identified. It is possible that some ethnic groups (mostly the Black group) with the most severe form of the disorder, especially those with uncommon symptoms, may be misdiagnosed as psychotic. Reference Hollander, Cohen and Friedman30,Reference Ninan and Shelton31 Similarly, Williams and colleagues Reference Williams, Proetto, Casiano and Franklin32 have also found differences in the clinical presentation of the symptoms, with African Americans reporting greater concerns about contamination on OCD inventories. However, one would expect this symptom would be as easily detected in the Black ethnic group as it is among White patients.
In addition to possible referral barriers and differences in presentation among ethnic minority groups, it is possible that obstacles exist in accurate diagnosis post-referral to secondary and tertiary mental health services. Williams et al Reference Williams, Domanico, Marques, Leblanc and Turkheimer33 suggested that ethnic minority participants may answer questions about symptoms in a different way in the presence of a therapist from a different ethnic background. For example, Williams & Turkheimer Reference Williams, Turkheimer and Sebeki34 found that, in an OCD assessment study, African American participants expressed significantly more washing concerns in the presence of a Black experimenter than a White experimenter. Similarly, Malgady & Constantino Reference Malgady and Costantino35 found that ethnic and language matching of patient and clinician promoted improved clinical judgements of psychopathology severity for Hispanic patients. Hence, an ethnic mismatch of patients and clinicians may decrease identification of OCD. Reference Williams, Domanico, Marques, Leblanc and Turkheimer33
In their systematic review, Williams et al Reference Williams, Powers, Yun and Foa9 concluded that, as ethnic minorities were underrepresented in North American OCD trials, it is actually not known if empirically validated treatments are effective for these groups. To date, only two small studies have compared OCD treatment outcomes across ethnic groups Reference Friedman, Smith, Halpern, Levine, Paradis and Viswanathan36,Reference Fernández de la Cruz, Jassi, Krebs, Clark and Mataix-Cols37 and, although both concluded that patients from ethnic minorities benefited from treatment as much as the White majority groups, further research with larger and representative samples is warranted.
Implications
The current study has a number of important implications for clinical practice, health policy and future research. Our findings should inform efforts to reduce racial/ethnic disparities in OCD diagnosis and access to treatment. To date, clinicians and policy-makers have had very little information about disparities in diagnoses and treatment of minority groups. Efforts should be made to ensure sensitivity to differing cultural values about mental health and to encourage symptom recognition and help-seeking behaviours by these populations. However, improving access to secondary and tertiary mental health services among ethnic minority groups will be facilitated by better understanding the barriers that currently exist. There is currently little research in this field. As pointed out by Hunt et al, Reference Hunt, Sullivan, Chavira, Stein, Craske and Golinelli23 it is critical to determine whether there are differences in beliefs about mental healthcare and treatment preferences across different ethnic groups. If these differences exist, they could partially explain the gap in care between minority and non-minority populations. However, if the differences in illness perceptions and help-seeking behaviours are small or do not exist, then it becomes crucial to seek out, understand and eventually eliminate the barriers to achieving more equitable care. Further studies should focus on the reasons for these ethnic inequalities in order to ensure a good quality of mental healthcare across all ethnic groups.
Limitations
First, because the cohorts were not actively followed up, we cannot fully exclude potential confounding factors such as patients from ethnic minorities deciding to be treated in other parts of London or in private health providers more frequently than White patients, although this seems unlikely. Second, as our data ranged from 1999 to 2013, we used the average of the London Census 2001 and 2011 to compare its ethnic composition against the ethnic composition of all the selected cohorts of clinical diagnoses in CRIS. The use of the most recent Census only would not have reflected the ethnic change of the population across the years and pooling both Censuses seemed the best approximation. It is also worth noting that, although both the Censuses and the NHS records aim to collect self-assigned ethnicity, the lists of available ethnic categories in CRIS, as well as the ethnic categories in the two different Censuses, are not identical. Third, it is likely that not all patients that were seen in the Trust from 1999 to 2005 – before CRIS was formally introduced – were included in the system, but only those whose mental health service had implemented an independent electronic system whose electronic records were migrated into the system (for more details, see Stewart et al Reference Stewart, Soremekun, Perera, Broadbent, Callard and Denis10 ). However, in our view, there is no reason to think that this would affect the validity of our results. Fourth, it is likely that most of the diagnoses were assigned based on clinician's judgement and not on a structured instrument. However, this would be true for OCD and also for depression. Also, in the case of OCD, an underrepresentation of ethnic minority groups was found across settings, which suggests these groups are less likely to be diagnosed independently of clinician biases. Fifth, we did not have data on socioeconomic status. For example, some studies have found higher rates of depression in ethnic minority groups particularly when socioeconomic status is not controlled for (for example see Stockdale et al Reference Stockdale, Lagomasino, Siddique, McGuire and Miranda38 ). Hence, the reported ethnic inequalities may in fact reflect more general socioeconomic status inequalities. Finally, the ethnic background was missing or ‘not stated’ for a proportion of participants with OCD (8.8%) and depression (11.4%). It is possible that the likelihood of stating one's ethnic group may vary according to ethnicity, with more individuals from ethnic minorities electing not to state their ethnicity. However, on reanalysis of the data with the assumption that all those that did not state their ethnicity were from ethnic minority groups, the direction of our results did not change (i.e. compared with the White group, the BME group was still underrepresented in both OCD (−43.5%) and depression (−15.7%).
In summary, the current study provides concerning evidence that individuals with OCD from ethnic minority groups are significantly underrepresented in secondary and tertiary mental health services. These findings highlight the urgent need to understand the barriers that exist to ethnic minority groups accessing these mental health services in order to facilitate the development of effective strategies and policies for reducing inequalities.
Funding
The authors acknowledge financial support from the South London and Maudsley Charitable Funds. BRC Clinical Records Interactive Search (CRIS) is supported by the NIHR Biomedical Research Centre for Mental Health BRC Nucleus at the South London and Maudsley NHS Foundation Trust and Institute of Psychiatry, King's College London jointly funded by the Guy's and St Thomas' Trustees and the South London and Maudsley Trustees. P.V.-R. is supported by a fellowship from the Alicia Koplowitz Foundation. S.L.H. receives salary support from the National Institute for Health Research (NIHR) Mental Health Biomedical Research Centre at South London and the Maudsley NHS Foundation Trust and King's College London. The views expressed are those of the authors and not necessarily those of the NHS, the NIHR or the Department of Health.







eLetters
No eLetters have been published for this article.