Home care is typically categorized as (a) home health care (nursing and medical services) and (b) home support (personal care, homemaking, meals, shopping, respite care) (Canadian Institute for Health Information, 2007), and is aimed at providing substitution for acute and long-term care, as well as maintenance or preventative care (Canadian Healthcare Association, 2009). Approximately one million Canadians age 65 and older use formal home care services each year (Hoover & Rotermann, Reference Hoover and Rotermann2012), and these numbers are expected to rise in the coming years for reasons such as population aging, attempts to reduce more costly health care, and the desire of older adults to age in place (Health Council of Canada, 2012). Based on the 2009 Canadian Community Health Survey (CCHS), approximately 53 per cent of older adults receiving home care do so from informal (mainly family) sources only; 18 per cent receive home care exclusively from paid employees or unpaid volunteers; and 29 per cent obtain blended sources of care (Hoover & Rotermann). While formal home care expenditures have more than doubled in a decade from $1.6 billion in 1994/95 to $3.4 billion in 2003/04 (Canadian Institute for Health Information, 2007), they represent only about five per cent of public health care dollars (Hermus, Stonebridge, Theriault, & Bounajm, Reference Hermus, Stonebridge, Theriault and Bounajm2012). Despite the increased resources and efforts to provide home care services, many older adults with complex care needs still are not receiving the home care services they require (Chappell & Hollander, Reference Chappell and Hollander2013; Health Council of Canada, 2012), and long-term and maintenance and preventative home care services have been disappearing in favour of acute services (Canadian Healthcare Association).
Studies addressing the efficacy of professional or formal home care have been largely confined to health outcomes, quality assurance, utilization and cost-benefits, delay of relocation to hospital or institutional environments, and need, rather than investigation of quality of life dimensions (Chappell, McDonald, & Stones, Reference Chappell, McDonald and Stones2008; Lévesque et al., Reference Lévesque, Wolfson, Bergman, Béland, Trahan and Perrault2004; Wister & McPherson, Reference Wister and McPherson2014). While studies have addressed client satisfaction, adverse consequences due to unmet home care needs (e.g., weight loss, falls, and dehydration), as well as some limited quality of life indicators (e.g., SF-36 subscales) of home care (Desai, Lentzner, & Weeks, Reference Desai, Lentzner and Weeks2001; Hollander, Miller, MacAdam, Chappell, & Pedlar, Reference Hollander, Miller, MacAdam, Chappell and Pedlar2009; LaPlante, Kaye, Kang, & Harrington, Reference LaPlante, Kaye, Kang and Harrington2004; Markle-Reid et al., Reference Markle-Reid, Browne, Weir, Gafni, Roberts and Henderson2008; McCall, Korb, Petersons, & Moore, Reference McCall, Korb, Petersons and Moore2004; Miller, Hollander, Corbett, & van der Valk, Reference Miller, Hollander, Corbett and van der Valk2008; Miller, Hollander, & MacAdam, Reference Miller, Hollander and MacAdam2008), there remains a gap in knowledge pertaining to social-psychological benefits of home care.
Furthermore, studies that have compared home care users and non-users have been limited by several factors: (1) the confounding effects of health status on a variety of outcomes (i.e., users are more frail); (2) health that often deteriorates among subjects in prospective studies, thereby masking associations; (3) randomized trials that tend to focus on medical outcomes; and (4) the challenges of selection biases in home care populations (those with less informal social support, fewer resources, and those experiencing rapid health deterioration are more likely to rely on home care). One way of addressing these problems is to analyse the consequences for individuals with home care needs that either are met through the receipt of home care or remain unmet (LaPlante et al., Reference LaPlante, Kaye, Kang and Harrington2004). This article builds on current research into the benefits of home care by focusing on three specific psychosocial domains that have been found to be important in the lives of persons as they age – life satisfaction, loneliness, and perceived life stress (Chappell et al., Reference Chappell, McDonald and Stones2008; Pearlin, Reference Pearlin2010; Perlman, Reference Perlman2004). This research is important because it provides evidence pertaining to the hidden consequences of home care for the psychosocial health and well-being of clients, including mental health and reduction of social isolation. In particular, this research may provide evidence to support the long-term and maintenance and preventative functions of home care. We begin by asking the question: Would filling the home care gap positively influence quality of life?
Review of Literature
Home care has been found to decrease mortality risk (Albert, Simone, Brassard, Stern, & Mayeux, Reference Albert, Simone, Brassard, Stern and Mayeux2005; Rahme et al., Reference Rahme, Kahn, Dasgupta, Burman, Bernatsky and Habel2010), reduce hospitalizations (Xu et al., Reference Xu, Weiner, Paul, Thomas, Craig and Rosenman2010), and improve health-related quality of life (King, Parsons, Robinson, & Jörgensen, Reference King, Parsons, Robinson and Jörgensen2012). There have also been a number of evaluations of home care to measure cost-effectiveness, usually by calculating the costs of home care services in comparison to other forms of health care. A key finding of Hollander and Chappell’s (Reference Hollander and Chappell2002) synthesis of 15 studies on home care in Canada was that home care costs less than residential care, particularly for stable clients, but mixed results were found for home care as a substitute for acute care.
Indeed, evidence of the financial and health-related benefits of home care has accumulated over the years, but began as inconclusive, particularly for long-term and maintenance and preventative home care. In part, this has been due to difficulty in obtaining a comparison group, combined with a lack of outcome measures that capture the full range of potential benefits. For instance, one of the first studies on home aid in Quebec, which used a non-equivalent control group design, found no evidence of the effectiveness of home support services (Contandriopoulos, Tessier, & Larouche, Reference Contandriopoulos, Tessier and Larouche1986). Moreover, the Health Services Utilization and Research Commission (HSURC, 2000) discovered that older adults receiving home support services had higher rates of mortality and health care costs than older adults not receiving them. However, the authors noted that a major limitation of this study may have been their inability to control for certain health characteristics, including pre-existing functional limitations.
Conversely, a study by Hollander and Tessaro (Reference Hollander and Tessaro2001) in British Columbia found higher health costs and mortality rates for individuals who had been cut from receiving maintenance and preventative home care. Furthermore, research by Hollander and colleagues over the past decade has established that investment into home care can be cost-effective because of trade-offs between it and more costly institutional and hospital care (Chappell & Hollander, Reference Chappell and Hollander2011, Reference Chappell and Hollander2013; Hollander & Chappell, Reference Hollander and Chappell2002; Hollander et al., Reference Hollander, Miller, MacAdam, Chappell and Pedlar2009). Integrated models of care for frail elderly adults that include home care services have also been shown to be cost-effective in Canada (Hébert et al., Reference Hébert, Raîche, Dubois, Gueye, Dubuc and Tousignant2010; Hébert, Reference Hébert2011). Yet studies have focused primarily on medical outcomes or health care utilization/costs as their outcomes of interest, leading an HSURC review of the preventative home care literature to conclude that there has been a lack of studies investigating quality of life, functional limitations, and social support (HSURC, 2002).
Most studies have examined home care use and various health outcome measures for the full population of older adults, often resulting in confounding health status effects, since comparisons are made between users and non-users, with non-users often having significantly better health and higher levels of functioning than users (Hollander et al., Reference Hollander, Miller, MacAdam, Chappell and Pedlar2009). A more accurate comparison would be between those who are receiving home care and those who have unmet home care needs, as presumably these two groups would be more similar in health and functional status. In one of the few studies of this kind, Capitman, Abrahams, and Ritter (Reference Capitman, Abrahams and Ritter1997) discovered that unmet home care needs among frail elders were associated with depression and reduced morale. In a prospective cohort study, Markle-Reid et al. (Reference Markle-Reid, Browne, Weir, Gafni, Roberts and Henderson2008) examined the effects of home support on functional health status, quality of life, depression, perceived social support, and cost of health services. Older adults using over one hour per week of home support services had lower levels of improvement in health and quality of life, but also lower health service costs than those using no home support services or under one hour per week. While all participants were technically eligible for home support services, some of the negative results for individuals receiving greater hours of home support can be explained by the fact that these individuals were more likely to have severe cognitive and physical impairments, which are difficult to completely statistically control in analyses. There is a need to extend this work to other quality-of-life indicators, and examine the potential mediating effects of other domains such as informal social support, since it can potentially substitute for formal sources. We therefore pose the research questions: (1) Do older adults who report that their home care needs are being met have higher levels of life satisfaction, and lower levels of loneliness and perceived life stress, than older adults with unmet home care needs?; (2) Furthermore, are there mediating effects on these associations?; and (3) In particular, what is the role of informal social support?
Conceptually, life satisfaction, loneliness, and perceived life stress dimensions of quality of life (QOL) represent key interconnected psychosocial elements of life span development that have been linked to social, community, family, household, and individual spheres of influence on the adaptation process (Pearlin, Reference Pearlin2010; Perlman, Reference Perlman2004; Stones, Kozma, McNeil, & Worobetz, Reference Stones, Kozma, McNeil and Worobetz2011). One bridging conceptual framework is a resilience model (Wild, Wiles, & Allen, Reference Wild, Wiles and Allen2013), which the authors applied to mobility resilience in later life. Wild et al. (Reference Wild, Wiles and Allen2013) contend that unmet service needs, including those addressing mobility concerns, cut across individual and environmental domains and thereby shape QOL especially among older persons with disability challenges. Home care attempts to fulfill mobility and functioning needs of clients at the juncture of the person and environment, by balancing environmental demands and individual competence but also increasing adaptation and QOL (Wister & McPherson, Reference Wister and McPherson2014). Life satisfaction, loneliness, and perceived life stress capture key elements of psychological well-being, mental health, and social isolation important for adapting to aging processes. We used these three outcome measures as multidimensional, linked indicators of QOL and resilience, in order to test whether they are influenced, in part, by met/unmet home care needs.
Life satisfaction was chosen as a principal indicator of quality of life. Research has suggested that subjective indicators termed life domain satisfactions have a significant effect on overall life satisfaction. Life domain satisfactions pertain to specific domains of life such as housing, health, and finances (Stones et al., Reference Stones, Kozma, McNeil and Worobetz2011). Up-down theoretical models suggest that both dispositional (e.g., personality) and situational factors (e.g., life domain indicators, burdens, negative environments, and social support) will shape life satisfaction (Berg, Hoffman, Hassing, McClearn, & Johansson Reference Berg, Hoffman, Hassing, McClearn and Johansson2009; Chappell et al., Reference Chappell, McDonald and Stones2008). Up-down models can provide a basis for the hypothesis that home care services may positively influence life satisfaction. For instance, a qualitative study by Wilson (Reference Wilson2012) found that clients identified improvements in their lives due to home support volunteer services in terms of quality of life, positive human contact, and help with daily activities. Other research indicates that increasing coping resources and support systems for frail older adults also enhances life satisfaction (Berg et al., Reference Berg, Hoffman, Hassing, McClearn and Johansson2009; Lohr, Essex, & Klein, Reference Lohr, Essex and Klein1988).
Loneliness is another dimension of quality of life among older adults that can lead to negative health outcomes (Hawton et al., Reference Hawton, Green, Dickens, Richards, Taylor and Edwards2011; Luo, Hawkley, Waite, & Cacioppo, Reference Luo, Hawkley, Waite and Cacioppo2012; Theeke, Reference Theeke2010), including a higher risk for developing Alzheimer's disease (Wilson et al., Reference Wilson, Krueger, Arnold, Schneider, Kelly and Barnes2007). Hawton et al. (Reference Hawton, Green, Dickens, Richards, Taylor and Edwards2011) found that social isolation (a construct related to loneliness) among seniors was associated with several health-related quality of life measures (e.g., SF-12), to a degree that was clinically relevant, even after controlling for depression, co-morbidities, age, gender, living arrangements, housing type, and employment status. Loneliness is not uncommon among older adults; in fact, Theeke (Reference Theeke2010) reported a prevalence rate of 16.9 per cent in a survey of older U.S. residents, and Pinquart and Sorensen (Reference Pinquart and Sorensen2001) estimated a prevalence of frequent loneliness between five per cent and 15 per cent based on a meta-analysis of 182 international studies. Home care clients, particularly those who are homebound, may be more vulnerable to loneliness and social isolation compared to other members of the population due to factors such as functional limitations, health problems, and a lack of social support. Home care workers have been identified as actors who can potentially help combat the problem of loneliness in homebound older adults through positive human contact (Aebischer, Reference Aebischer2008; Wilson, Reference Wilson2012).
Stress has been defined as “a relationship between the person and the environment that is appraised by the person as taxing or exceeding his or her resources and endangering his or her well-being” (Lazarus & Folkman, Reference Lazarus and Folkman1984, p. 19). Stressors are problematic conditions or experiences that challenge the adaptive abilities of individuals (Pearlin, Reference Pearlin2010), and can lead to poor physical and mental health, as well as premature mortality (Keller et al., Reference Keller, Litzelman, Wisk, Maddox, Cheng and Creswell2012). Previous research on stress has suggested that while older adults tend to experience everyday stress events less often than younger adults, they are more susceptible to negative affect when these stresses occur (Mroczek & Almeida, Reference Mroczek and Almeida2004), and furthermore, that natural declines in immune function and resilience can be exacerbated by chronic stressors (Gouin, Hantsoo, & Kiecolt-Glaser, Reference Gouin, Hantsoo and Kiecolt-Glaser2008; Graham, Christian, & Kiecolt-Glaser, Reference Graham, Christian and Kiecolt-Glaser2006). The absence of home care services is a potential stressor for older adults who have home care needs, and conversely, receipt of home care may buffer or reduce stress. For instance, Wagnild and Grupp (Reference Wagnild and Grupp1991) reported that older adult home care clients who have recently been discharged from the hospital can experience stress due to early discharge, illness, the need for physical care and emotional support, financial difficulties, unsuitable home environments, isolation, and the overwhelming demands placed on their caregivers. Results from a qualitative study by Turpin, McWilliam, and Ward-Griffin (Reference Turpin, McWilliam and Ward-Griffin2012) suggest that the comfort of knowing that a home care worker is available may allow some older adult home care clients to feel less stressed about their situation.
Methods
This study utilized data from the cross-sectional Canadian Community Health Survey (CCHS) Healthy Aging component collected by Statistics Canada. A three-stage design was used: (a) first, geographical areas called clusters were selected; (b) second, households were selected within each sampled cluster; and (c) finally, one respondent per household was randomly selected (Statistics Canada, 2010, p. 22). To ensure a high response rate, introductory letters were sent to each participant explaining the survey. Also, interviewers made multiple attempts to arrange for an interview at the convenience of the respondent, and left a notice at the door if no one was home. Consent was obtained before interviews were conducted. A total of 30,865 valid interviews from community-dwelling Canadians aged 45 and older were collected by way of a computer-assisted electronic interviewing instrument between December 2008 and November 2009. Approximately 94 per cent of interviews were conducted face-to-face by decentralized field interviewers who utilized the computer-assisted interviewing instrument. The remaining interviews were conducted over telephone due to extenuating circumstances.
The purpose of the survey was to collect data on the factors, influences, and processes that contribute to healthy aging. Data were collected from all 10 provinces. Individuals living in the territories, on Indian reserves/Crown lands, in institutions, and in some remote regions were excluded, as were full-time members of the Canadian armed forces (Statistics Canada, 2010). A total of 16,369 participants were aged 65 and older. The sub-sample used in our analysis was restricted to older adults aged 65 or older who had received home care services and/or identified that they had unmet professional home care needs (n = 3,244). The cases were weighted using the CCHS population weights and then rescaled to the original sub-sample size so that the analysis was not overpowered.
Dependent Variables
Life Satisfaction
Global life satisfaction was based on the Satisfaction With Life Scale developed by Diener, Emmons, Larsen, and Griffin (Reference Diener, Emmons, Larsen and Griffins1985) that uses the aggregate sum of five items (e.g., “I am satisfied with my life”). It has been established as a valid and reliable measure of well-being, and used with a wide range of age groups and applications (Pavot, Diener, Colvin, & Sandvik, Reference Pavot, Diener, Colvin and Sandvik1991). Cross-method convergence with more complex well-being measures has also been supported. The mean value for respondents’ satisfaction with life scores on these items was 25.25 (range = 5–35, SD = 6.24), indicating a positive skew (see Table 1).
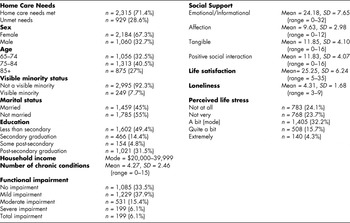
Table 1: Sample characteristics (n = 3.244)
Loneliness
Loneliness was measured using the three-item Revised UCLA Loneliness Scale (R-UCLA) (e.g., “how often do you feel that you lack companionship: hardly ever, some of the time, or often?”). The scale has previously been tested in the 2002 wave of the U.S. Health and Retirement Study (HRS) and the Chicago Healthy Aging and Social Relations Study (CHASRS) and has been shown to perform as well as longer-form measures of loneliness (Hughes, Waite, Hawkley, & Cacioppo, Reference Hughes, Waite, Hawkley and Cacioppo2004). The mean for the loneliness scale was 4.31 (range = 3–9, SD = 1.68), indicating a negative skew (see Table 1), where a low score indicated low levels of loneliness.
Perceived Life Stress
Psychosocial perceived life stress was measured using single-item Likert responses to the question “Thinking about the amount of stress in your life, would you say that most days are … not at all stressful, not very stressful, a bit stressful, quite a bit stressful, or extremely stressful?” The reliability and validity of single-item psychosocial stress measures compared to multiple item instruments has been established, showing their usefulness in large population-based epidemiological studies (Littman, White, Satia, Bowen, & Kristal, Reference Littman, White, Satia, Bowen and Kristal2006). Given the ordinal level of measurement, this variable was dichotomized into not at all and not very stressful versus the other three stress categories and used in a logistic regression analysis. As shown in Table 1, the distribution was skewed towards low levels of stress, with the answer a bit stressful as the mode.
Independent Variables
Home Care Needs
The principal independent variable was professional home care needs, which was created by combining two separate home care questions (with yes/no responses) in the CCHS. In the data set, participants were asked “whether they received home care services provided by professionals (formal home care) during the past 12 months because of a health condition or limitation that affects their daily activities?” In addition, participants were asked “whether they had ever needed professional home care services but not received them?” Although this question is broad, participants likely considered this to refer to professional home care services given the preceding question. It should also be noted that some individuals receiving home care services over the past 12 months could also be classified as having unmet home care needs if they identified that they were not receiving all the services that they needed. Therefore, we computed a new dichotomous variable (home care needs) from the four possible response quadrants, where unmet home care needs combined (a) individuals who currently received home care but also stated that they still had unmet home care needs with (b) those participants who stated that they needed professional services but had never received this type of care.
Participants were classified as having home care needs met if they received home care and responded in the negative to needing home care but not ever receiving it. However, persons not receiving home care and who stated that they had never needed it were excluded, since we could not determine whether there was an actual home care need or not, given that these were self-reported questions rather than professional assessments. Based on this home care need variable classification, a total of 71.4% per cent (n = 2,315) of the sample had home care needs that were met, and 28.6 per cent (n = 929) had unmet needs. Although not studied here, potential reasons for unmet needs included personal circumstances (i.e., ability to pay); issues with access within the health care system; or a combination of both.
Co-variates
Co-variates in this analysis have been selected from literature on predictors of home care, life satisfaction, loneliness and perceived life stress, including age, sex, marital status (married/common law as reference category), visible minority status (yes/no, with no as reference category), education, income, functional impairments, number of chronic conditions, and social support (see Table 1). Education identified the highest level completed and was classified as less than secondary, secondary graduation, some post-secondary, or post-secondary graduation (with less than secondary as the reference category). Income was measured as total household income (<$20,000, $20,000–$39,999, $40,0000–$59,999, $60,000–$79,999, >$80,000), with the lowest level as the reference category. Functional impairments were measured using the Basic and Instrumental Activities of Daily Living instrument developed by the CCHS working group based on the OARS Multidimensional Functional Assessment Questionnaire (Fillenbaum & Smyer, Reference Fillenbaum and Smyer1981). The OARS classifies individuals as having no functional impairment, mild impairment, moderate impairment, severe impairment, or total impairment (no impairment as reference category). Number of chronic conditions was calculated by counting the number of chronic conditions respondents had reported from a list of 21 possible chronic conditions (such as arthritis, heart disease, diabetes, etc.) (see Statistics Canada, 2010).
The Medical Outcomes Study (MOS) Social Support Survey was used to measure social support (Sherbourne & Stewart, Reference Sherbourne and Stewart1991). The MOS includes four social support subscales: affection, emotional/informational support, positive social interaction, and tangible social support. All of the scales consisted of the summed scores of items that used a four point (0–4) response set (none of the time, a little of the time, some of the time, most of the time, all of the time). The affection scale represented the levels of love and affection the respondent received and was the summed score of three items (range = 0–12, mean = 9.63, SD = 2.98). The emotional/informational support scale represented the expression of positive affect and understanding, and the availability of advice and guidance. This variable was the summed score of eight items (range = 0–32, mean = 24.18, SD = 7.65). The positive social interaction scale represented the availability of other people with whom to positively interact. This variable was the summed score of four items (range = 0–16, mean = 11.83, SD = 4.07). The tangible social support scale represented the availability of material aid and behavioural assistance and also consisted of four items (range = 0–16, mean = 11.85, SD = 4.10). Home care use could not be included as a co-variate in the analysis since it is highly correlated with unmet home care needs (r = 0.80).
Missing values were imputed to the mean or the mode for all variables. For multi-item scales, the group mean was used for imputation due to the small number of items in these scales. Income data were missing for a significant proportion of respondents (22.8%): it was imputed based on age, sex, and level of education of the respondent. Only income (22.8%), loneliness (8.2%), life satisfaction (8.9%), and the social support scales (affection, 11.5%; emotional/informational support, 13.4%; positive social interaction, 12.1%; and tangible social support, 12.2%) had a significant amount of missing data. Analyses were repeated using two additional methods of assigning missing values to check for potential bias: (1) with all missing values removed, and (2) using means of answered questions for multi-item scales; however, all findings were replicated with virtually no changes in point estimates. In cases where the selected respondent was, for reasons of physical or mental health, incapable of completing an interview, proxy respondents were used (2.2% of all cases). However, any questions that were more sensitive or personal were left unanswered (i.e., missing), including the dependent variables used in this study. Every effort was taken to keep proxy interviews to a minimum (Statistics Canada, 2010).
Selected Sample Characteristics
In the sample, 71.4 per cent (n = 2,315) of respondents had home care needs that were met, and 28.6 per cent (n = 929) had unmet home care needs (see Table 1). Of those who had unmet home care needs, 7.9 per cent reported receiving some home care services. A total of 32.5 per cent of the sample were aged 65–74, 40.5 per cent were aged 75–84, and 27 per cent were aged 85 or older. In addition, 67.3 per cent of the sample were female and 32.7 per cent, male. About 45 per cent of the sample were married or in common-law relationships. Approximately half of the sample (49.4%) had less than secondary-level education. Also, 73 per cent of the sample reported household incomes of less than $40,000 per year. The majority of the sample reported no functional impairment (33.5%) or mild functional impairment (37.9%), and the mean for number of chronic conditions reported was 4.27 (SD = 2.46).
Regression Modelling
Identical hierarchical regression models were used for the ordinary least squares (OLS) regression on life satisfaction and loneliness, as well as for the logistic regression on the dichotomous stress variable. Variables were added in five ordered main effects blocks: home care needs, demographic factors, socioeconomic status, health factors, and social support. The home care needs variable was included in block 1 in order to assess potential mediating effects on the relationship between home care needs and the dependent variables. Subsequent blocks of variables were sequentially added. There were four different social support scales (tangible, emotional/informational, affection, and positive social interaction), all of which exhibited high degrees of collinearity with each other (r ≥ 0.65). Therefore, each social support scale was tested in the model separately, and only the model containing the social support scale that explained the most variance was reported, given virtually identical results across the analyses (full results available from authors upon request). In addition, multiplicative interaction terms were entered in a final block between levels of ADL/IADLS and home care needs in order to examine their simultaneous effects on the outcome variables.
Results
Linear Regression: Life Satisfaction
As shown in Table 2, all of the linear regression models for life satisfaction were statistically significant (total R 2 = 24.3%). Model 1 included home care needs (R 2 = 0.034, R Change = 0.034 p < .001), model 2 added demographic factors (R 2 = 0.065, R Change = 0.033, p < .001), model 3 added socioeconomic status (R 2 = 0.070, R Change = 0.006, p < .001), model 4 included health factors (R 2 = 0.178, R Change = 0.109, p < .001) and model 5 added positive social interaction (R 2 = 0.243, R Change = 0.066, p < .001). Overall, health factors explained the most variance (10.9%) in life satisfaction, followed by social support (6.6%) and home care needs (3.4%).
Table 2: Life satisfaction linear regression
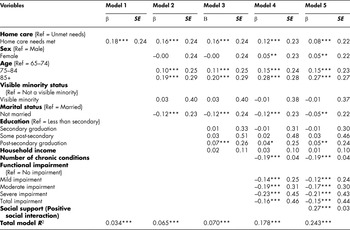
*p < .05, **p < .01, ***p < .001.
SE = standard error
Home care needs (being met) resulted in a weak to moderate positive relationship with life satisfaction (β = 0.18, p < .001, SE = 0.24) in model 1. This provides support for the hypothesis that older adults whose home care needs are being met have higher levels of life satisfaction than older adults with unmet home care needs. The relationship between home care needs and life satisfaction was modestly weakened throughout the hierarchical modelling process, and resulted in a weak positive association with life satisfaction after controlling for the co-variates (β = 0.08, p < .001, SE = 0.22). Positive social interaction appeared to have a partial mediating effect on the relationship between home care needs and life satisfaction.
Only the final main effects model results will be presented below for the co-variates (full hierarchical results for all models are shown in Tables). In the final model, there was a weak positive association between being female (β = 0.05, p < .01, SE = 0.22), and for those aged 75–84 (β = 0.15, p < .001, SE = 0.23), and the 85 and older age group (β = 0.27, p < .001, SE = 0.27) with life satisfaction (compared to the 65–74 age group). Marital status exhibited a weak negative relationship with life satisfaction (β = –0.05, p < .01, SE = 0.22), with those who were unmarried expressing lower levels of life satisfaction. Completion of post-secondary education had a very weak positive relationship with life satisfaction (β = 0.05, p < .01, SE = 0.24). Number of chronic conditions (β = –0.19, p < .001, SE = 0.04) showed a moderate negative relationship with life satisfaction. Mild functional impairment (β = –0.12, p < .001, SE = 0.24), moderate functional impairment (β = –0.17, p < .001, SE = 0.30), severe functional impairment (β = –0.21, p < .001, SE = 0.43), and total functional impairment (β = –0.15, p < .001, SE = 0.44), all resulted in moderate negative relationships with life satisfaction in comparison to those with no impairment. Social support in the form of positive social support had a moderate positive relationship with life satisfaction (β = 0.27, p < .001, SE = 0.03). Finally, none of the interaction effects were supported (not shown in tables).
Linear Regression: Loneliness
As shown in Table 3, all of the linear regression models for loneliness were statistically significant (total R 2 = 24.1%). Positive social interaction contributed the most (12.3%) to the variance in loneliness, followed by demographic factors (6.6%), and home care needs (3.1%).
Table 3: Loneliness linear regression
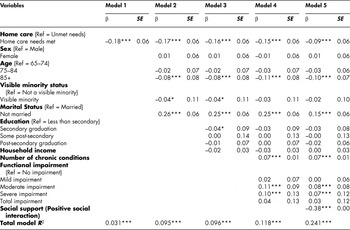
*p < .05, **p < .01, ***p < .001.
SE = standard error
In model 1, home care needs (being met) had a statistically significant weak to moderate negative relationship with loneliness (β = –0.18, p < .001, SE = 0.06), which remained statistically significant after all co-variates were statistically controlled (β = –0.09, p < .001, SE = 0.06). The inclusion of positive social interaction resulted in the largest decline in the association between home care needs and loneliness, suggesting a partial mediating effect. These findings showed that older adults whose home care needs were being met exhibited lower levels of loneliness than older adults with unmet home care needs.
In the final model, being in the 85 and older age group (β = –0.10, p < .001, SE = 0.07) exhibited a weak negative relationships with loneliness. Being unmarried (β = 0.15, p < .001, SE = 0.06) and reporting more chronic conditions (β = 0.07, p < .001, SE = 0.01), exhibited weak positive relationships with loneliness. Also, moderate impairment (β = 0.08, p < .001, SE = 0.08), and severe impairment (β = 0.07, p < .001, SE = 0.12) had weak positive relationships with loneliness, compared to no impairment. Finally, there was a moderate inverse association between positive social interaction and loneliness (β = –0.38, p < .001, SE = 0.01). In addition, one of the four multiplicative interaction effects exhibited a borderline association. The simultaneous effect of having home care needs met and experiencing severe ADL/IADL impairment (compared to having unmet home care needs and no impairment) increased loneliness (β = 0.24, p < .05, SE = 0.24).
Logistic Regression: Perceived Life Stress
As shown in Table 4, all of the logistic regression models for perceived life stress were statistically significant (Total model χ2 = 258.66, df = 16, p < .001). In model 1, a negative relationship was found between home care needs and perceived life stress (β = –0.71, p < .001, OR = 0.49). The odds of reporting being stressed were decreased by a factor of 0.49 (or about half) for older adults whose home care needs were being met in comparison to those with unmet home care needs. This relationship weakened throughout the hierarchical modelling process, from an odds ratio of 0.49 to 0.62, after controlling for all co-variates (β = –0.49, p < .001, OR = 0.62). These findings provide support for the hypothesis that older adults whose home care needs are being met would exhibit lower levels of perceived life stress than older adults with unmet home care needs. The largest mediating effect, albeit modest, was observed when tangible social support was added to the model, suggesting that it is a significant intervening variable in the relationship between home care needs and perceived life stress.
Table 4: Perceived life stress logistic regression

*p < .05, **p < .01, ***p < .001.
df = degrees of freedom
OR = odds ratio
In the final model, a statistically significant positive relationship was found between sex and perceived life stress (β = 0.21, p < .05, OR = 1.23), where the odds of reporting being stressed were increased by a factor of 1.23 for older adult women, in comparison to older adult men. A statistically significant negative relationship was found between age and perceived life stress for those aged 75–84 (β = –0.21, p < .05, OR = 0.81) and those 85 and older (β = –0.61, p < .001, OR = 0.54), compared to those aged 65–74. Unexpectedly, a negative relationship was found between marital status and perceived life stress (β = –0.43, p < .001, OR = 0.65), where the odds of reporting being stressed were decreased by a factor of 0.65 for those who were not married in comparison to those who were married. Secondary graduation had a negative relationship with perceived life stress (β = –0.26, p < .05, OR = 0.77), where the odds of being stressed decreased by a factor of 0.77 for those who had completed secondary school in comparison to those who had not. On the other hand, some post-secondary education had a positive relationship with perceived life stress (β = 0.36, p < .05, OR = 1.44). The odds of being stressed increased by a factor of 1.44 for older adults with some post-secondary education in comparison to those who had not completed secondary education. Surprisingly post-secondary graduation was not associated with stress. Income exhibited a very weak positive association with perceived stress (β = 0.08, p < .05, OR = 1.09).
Number of chronic conditions (β = 0.09, p < .001, OR = 1.10), mild impairment (β = 0.29, p < .01, OR = 1.34), moderate impairment (β = 0.44, p < .001, OR = 1.55), severe impairment (β = 0.67, p < .001, OR = 1.95), and total impairment (β = 0.42, p < .05, OR = 1.52) all showed weak positive relationships with perceived life stress. Finally, social support in the form of tangible social support had a negative relationship with perceived life stress (β = –0.06, p < .001, OR = 0.94). The odds of being stressed decreased by a factor of 0.94 for each unit increase in tangible social support scores. Also, none of the interaction effects were found to be statistically significant.
Discussion
This study extended prior research on the non-medical benefits of home care through an investigation of met/unmet home care needs among older adults. Persons receiving professional home care who stated that their home care needs were met were compared to those with unmet needs (with or without home care services) on three important quality of life indicators – life satisfaction, loneliness, and perceived life stress. Older adults whose professional home care needs were being met had significantly higher levels of life satisfaction, and lower levels of loneliness and perceived life stress than older adults with unmet needs. Alternatively, if home care needs were not being met, either because an individual required home care, or they were not receiving an appropriate level of home care, then their quality of life was compromised. This is consistent with a U.S. study that showed a decline in patient quality of life, including life satisfaction, after reductions to home care due to changes to Medicare policy (McCall et al., Reference McCall, Korb, Petersons and Moore2004).
These findings suggest that home care can enhance quality of life through positive human contact, in addition to providing direct help with daily activities (Wilson, Reference Wilson2012). Together, these important and potentially reinforcing aspects of home care may strengthen resilience of frail older adults in key domains of their life as reflected in the associations with life satisfaction, loneliness, and perceived stress (Wild et al., Reference Wild, Wiles and Allen2013). For instance, the provision of home care for persons perceiving a need can enhance individual, social, and environmental resilience by raising the confidence of the person to maintain independence, sustain a beneficial level of social connectedness to the community and neighbourhood, and in managing household demands. This research suggests that “aging in place” as a generic perspective or policy does not come without certain demands on the individual, especially if their functional ability is significantly challenged; and furthermore, this approach may overlook more-subjective, psychosocial values of receiving home care. Thus, filling the home care need gap can influence the ways in which an individual experiences the challenges of aging.
With respect to feelings of social isolation, home care workers are in close contact with home care clients, and their presence and interactions with clients, particularly those clients who are homebound, may help to ameliorate feelings of loneliness (Aebischer, Reference Aebischer2008; Patmore, Reference Patmore2002; Wilson, Reference Wilson2012). Home care workers may also help arrange social activities for the client or encourage clients to take part in such activities (Aebischer, Reference Aebischer2008). Indeed, some older adults have paid out of pocket for home care workers to come to their home solely for the purpose of having company and positive social interaction (Andrews, Gavin, Begley, & Brodie, Reference Andrews, Gavin, Begley and Brodie2003). For this reason, Patmore (Reference Patmore2002) has suggested that a specific social support function needs to be developed as part of the responsibilities of home care workers.
Furthermore, receiving adequate home care services helps older adults cope with care needs and decreases the level of burden felt in everyday life. Home care clients may face a number of stressors including early discharge from hospital, illness, functional limitations, the need for physical care and emotional support, financial difficulties, unsuitable home environments, isolation, and the overwhelming demands placed on their caregivers (Wagnild & Grupp, Reference Wagnild and Grupp1991). It has been suggested that in order to optimize the health and wellness of home care clients, home care workers should screen clients for major stressors, identify problems from the clients’ perspectives, and then identify strategies to help the clients deal with the stressors (Wagnild & Grupp). In the present study, lower levels of stress were associated with having home care needs met at a level that has practical importance.
Turning to the co-variates we investigated, social support in the form of positive social interaction exhibited the most influential, albeit partial, mediating effect for the associations between home care needs and life satisfaction and loneliness. Similarly, social support in the form of tangible social support had the most influential mediating effect on perceived life stress. In other words, the presence of social support can buffer the negative influence of a home care gap when perceived to be required, likely through positive reassurance, positive social interaction, and help with daily tasks. However, it appears that social support cannot completely fill this gap, indicating that meeting the home care needs of the older population is a necessary requisite for the maximization of quality of life. It is not clear whether these findings support a substitution or complementary model of the informal-formal support interface; however, one can conclude that the presence of social support remains pivotal in the lives of older adults whether they receive home care or not. Several other co-variates were relatively consistent in their prediction of life satisfaction, loneliness, and perceived life stress. Age exhibited a positive association with life satisfaction, and an inverse association with loneliness and perceived life stress, similar to other studies (Boeninger, Shiraishi, Aldwin, & Spiro, Reference Boeninger, Shiraishi, Aldwin and Spiro2009; Bourque, Pushkar, Bonneville, & Beland, Reference Bourque, Pushkar, Bonneville and Beland2005; Mroczek, & Almeida, Reference Mroczek and Almeida2004; Theeke, Reference Theeke2010; Victor, Scambler, Bowling, & Bond, Reference Victor, Scambler, Bowling and Bond2005). However, the relationship between age and these quality-of-life indicators remains unclear due to conflicting evidence. Older age has been associated with smaller social networks and increased isolation; however, studies have also found that not all older adults who are socially isolated or have smaller social networks report being lonely (Perlman, Reference Perlman2004; Schnittger, Wherton, Prendergast, & Lawlor, Reference Schnittger, Wherton, Prendergast and Lawlor2012; Victor et al., Reference Victor, Scambler, Bowling and Bond2005; Wenger, Davies, Shahtahmasebi, & Scott, Reference Wenger, Davies and Shahtahmasebi1996).
Older women showed higher levels of life satisfaction, but also higher levels of stress, net of other factors. Perhaps older women have more positive outlooks on life, while concurrently being in the position of caregiver more often than men. Compared to married older adults, the non-married exhibited slightly lower levels of life satisfaction, and higher levels of loneliness, but actually showed lower stress levels. While consistent with other research, the pathways for these relationships may vary by gender (Bourque et al., Reference Bourque, Pushkar, Bonneville and Beland2005). For instance, men tend to enjoy more benefits of marriage in old age than women, since the latter are more likely to be caregivers (Lavela & Ather, Reference Lavela and Ather2010). Post-secondary graduation had relatively weak associations with the quality-of-life indicators, but generally in the anticipated direction, supporting earlier work (Bourque et al., Reference Bourque, Pushkar, Bonneville and Beland2005; Pinquart & Sorenson, Reference Pinquart and Sorensen2000). Surprisingly, income was positively associated with perceived life stress, after all co-variates were statistically controlled. This finding is a bit perplexing and conflicts with other studies (e.g., Scott, Jackson, & Bergeman, Reference Scott, Jackson and Bergeman2011), although one possible explanation could be that only a crude grouped income measure was available. Not surprisingly, and consistent with other literature (Abu-Bader, Rogers, & Barusch, Reference Abu-Bader, Rogers and Barusch2003; Bourque et al., Reference Bourque, Pushkar, Bonneville and Beland2005; Theeke, Reference Theeke2010), the number of chronic conditions and functional health status had relatively robust associations with life satisfaction, loneliness, and perceived life stress. Health problems, for instance, can be significant stressors, and health-related stresses tend to increase with age (Martin, Grunendahl, & Martin, Reference Martin, Grunendahl and Martin2001).
Finally, we supported only one borderline interaction effect between home care needs and functional status. Having home care needs met and experiencing severe ADL/IADL impairment, compared to having needs met with no limitations, resulted in increased loneliness. This may be indicative of the person-environment challenges experienced by persons with significant health challenges; however, further research is warranted.
Limitations and Conclusions
One limitation of this study was that the home care need question was based on the receipt of home care over the past 12 months, coupled with the presence of any unmet home care needs. The creation of the met/unmet need variable therefore relied on information covering 12 months for home care use, and “ever” for the unmet-need question. This could potentially bias the results. It was also necessary to exclude persons not receiving home care who did not report any unmet needs, since we were unable to determine if this self-reported information deemed them “at risk” or not of requiring home care. However, most older persons fall in this quadrant, and the vast majority do not receive nor require home care (not “at risk”), thereby minimizing the amount of introduced measurement error. Ideally, a consistent time period for both variables would have been preferable, especially given fluctuations in need. However, the robust and consistent findings for the home care need variable and all three of the dependent variables increases confidence in its measurement, as well as in the primary findings.
A second limitation was that we were unable to examine actual home care use as a separate co-variate in the analyses due to collinearity with the home care need variable. Another limitation was that there were no variables that assessed personality factors. While life satisfaction, loneliness, and perceived life stress are all subjective measures, personality factors could potentially have important effects on these variables. In particular, personality characteristics and genetic factors have both been linked to subjective well-being and life satisfaction (Stones et al., Reference Stones, Kozma, McNeil and Worobetz2011).
In conclusion, this study suggests that filling the gap in home care could have a significant positive impact on key quality of life indicators, specifically life satisfaction, loneliness, and perceived life stress. Furthermore, these results provide consistent evidence that home care services have additional benefits for older adults beyond traditional medical and health service utilization outcomes. Meeting unmet home care needs can improve many facets deemed central to the maintenance of quality of life in the face of declining health, all of which coalesce in a manner to strengthen social and environmental resilience, and allowing more people to “age in place” in a positive manner. Given that most older adults receiving home care are limited in functional ability or are frail, the positive effects of having home care needs met on salient psychosocial aspects of life, even after controlling for a number of co-variates, emphasizes the diverse ways in which home care improves the lives of older adults. These findings provide a stronger rationale for expanding home care – including long-term and maintenance and preventative home care – to those in need, given that it may reduce social isolation, buffer the deleterious effects of aging-related stressors, and help individuals to maintain better mental health.
Future research should explore the relationships between home care and a wider range of potential outcomes. Furthermore, longitudinal studies, such as the Canadian Longitudinal Study on Aging, would be especially useful in providing further support for these relationships – in particular, confirming the directionality and causation of the variables of interest. Ultimately, if we are able to better identify and quantify the full set of benefits of home care, a stronger case can be made for extending, integrating, and improving home care services for older adults.






