Introduction
Peer victimization (PV) captures all forms of aggression against a peer (Gini et al., Reference Gini, Card and Pozzoli2018) and is characterized by repeated, intentional behaviors, and an imbalance of power (Olweus, Reference Olweus1994). It can occur in person and online (e.g., cyberbullying) and can be direct, including physical (e.g., hitting) and verbal (e.g., name-calling) victimization, or indirect, including relational victimization (e.g., social exclusion and rumor-spreading). Over five decades of research has demonstrated the mental health consequences of PV for children and adolescents globally (e.g., Due et al., Reference Due, Holstein, Lynch, Diderichsen, Gabhain, Scheidt and Currie2005; Olweus, Reference Olweus1977; Wolke et al., Reference Wolke, Copeland, Angold and Costello2013). In particular, adolescents who experience PV are at higher risk of developing internalizing problems such as depression (Bogart et al., Reference Bogart, Elliott, Klein, Tortolero, Mrug, Peskin, Davies, Schink and Schuster2014; Earnshaw et al., Reference Earnshaw, Elliott, Reisner, Mrug, Windle, Emery, Peskin and Schuster2017; van Geel et al., Reference van Geel, Vedder and Tanilon2014) and anxiety (Siegel et al., Reference Siegel, La Greca and Harrison2009; Stapinski et al., Reference Stapinski, Bowes, Wolke, Pearson, Mahedy, Button, Lewis and Araya2014).
Despite the abundance of empirical evidence documenting the robust associations between PV and poor mental health outcomes in adolescents, the mechanisms underlying this relationship remain unclear and we still do not know much about why, or under what circumstances, PV leads to maladjustment (Peets et al., Reference Peets, Turunen and Salmivalli2021). Further in-depth study of potential mechanisms is needed to better understand this relationship and assist in the identification of markers of PV, effective points of intervention, and the development of prevention strategies and treatment plans for victims. Notably, the past decade has seen the emergence of two bodies of literature which associate varying sleep problems with both PV and internalizing problems, including anxiety and depression. In line with this, the current study aimed to investigate the role of sleep as a mechanism underlying the relationship between PV and internalizing symptoms in adolescents.
Adolescent vulnerabilities to PV, insufficient sleep, and internalizing symptoms
Adolescents are particularly vulnerable to PV, insufficient sleep, and the onset of internalizing symptoms due to a myriad of biological, psychological and social factors unique to this developmental period. Rates of victimization, while generally more transient in younger children (Due et al., Reference Due, Holstein, Lynch, Diderichsen, Gabhain, Scheidt and Currie2005), increase and stabilize during adolescence, peaking in early adolescence (Earnshaw et al., Reference Earnshaw, Elliott, Reisner, Mrug, Windle, Emery, Peskin and Schuster2017). This is largely due to the increased salience of peer relationships and the importance of social status, power, and peer acceptance during adolescence (Rapee et al., Reference Rapee, Oar, Johnco, Forbes, Fardouly, Magson and Richardson2019). Boys are at a higher risk of direct victimization (e.g., physical and verbal), while indirect (e.g., relational) victimization is experienced equally (Carbone-Lopez et al., Reference Carbone-Lopez, Esbensen and Brick2010; Due et al., Reference Due, Holstein, Lynch, Diderichsen, Gabhain, Scheidt and Currie2005; Monks et al., Reference Monks, Smith and Kucaba2021).
Adolescence is also characterized by the onset of anxiety and depressive disorders, with girls being at significantly greater risk than boys (Altemus et al., Reference Altemus, Sarvaiya and Neill Epperson2014; Kessler et al., Reference Kessler, Berglund, Demler, Jin, Merikangas and Walters2005; Rapee et al., Reference Rapee, Oar, Johnco, Forbes, Fardouly, Magson and Richardson2019). Adolescents face a number of pubertal, neurobiological, and social changes that heighten negative affectivity, limit emotion regulation efficacy, and increase social sensitivity – all key characteristics of internalizing disorders (Rapee et al., Reference Rapee, Oar, Johnco, Forbes, Fardouly, Magson and Richardson2019). Given these dual vulnerabilities for PV and internalizing, it is unsurprising that adolescents who experience PV are at a higher risk for developing anxiety and depression (Christina et al., Reference Christina, Magson, Kakar and Rapee2021).
Adolescence is also characterized by significant changes to sleeping patterns and Australian data shows that one quarter of 12–15 year-olds do not get the recommended amount of sleep (i.e., 8–10 hours; Evans-Whipp & Gasser, Reference Evans-Whipp, Gasser, Daraganova and Joss2018). Notably, sex differences in sleep first appear in adolescence, with adolescent girls being two times more likely to develop insomnia than boys (Baker et al., Reference Baker, Yűksel, de Zambotti, Attarian and Viola-Saltzman2020). Carskadon’s (Reference Carskadon2011) seminal ‘perfect storm’ model, which ignited a significant and growing body of research on sleep in adolescence (see, e.g., Crowley et al., Reference Crowley, Wolfson, Tarokh and Carskadon2018), emphasizes a number of key factors which increase adolescent vulnerability to insufficient sleep. Namely, pubertal maturation of the sleep-wake homeostasis system (i.e., slower build-up of sleep pressure/sleepiness), changes in the circadian timing system leading to later bedtimes, increased social and academic demands, and early school start times all impinge upon and curtail adolescents’ sleep. Given the importance of sleep for healthy functioning, and the fact that sleep need does not meaningfully decrease across adolescence (Crowley et al., Reference Crowley, Wolfson, Tarokh and Carskadon2018), there are growing calls for more research examining the causes and consequences of insufficient sleep in this population.
PV and internalizing symptoms
Associations between PV and internalizing symptoms in adolescents are extremely robust (Biebl et al., Reference Biebl, DiLalla, Davis, Lynch and Shinn2011; Christina et al., Reference Christina, Magson, Kakar and Rapee2021; Gini et al., Reference Gini, Card and Pozzoli2018; Reijntjes et al., Reference Reijntjes, Kamphuis, Prinzie and Telch2010; van Geel et al., Reference van Geel, Vedder and Tanilon2014). Meta-analyses have demonstrated significant prospective associations between PV and increased internalizing problems, including both depression and anxiety (Christina et al., Reference Christina, Magson, Kakar and Rapee2021; Reijntjes et al., Reference Reijntjes, Kamphuis, Prinzie and Telch2010). This relationship also appears to be bidirectional and is consistent across both age and sex (Christina et al., Reference Christina, Magson, Kakar and Rapee2021).
Regarding the relationship from PV to later internalizing, including depression and anxiety, research supports the development of several processes that predict internalizing distress following PV. Two longitudinal studies of American (predominantly White) youth (11–16 year olds) provide support for the specific link between PV and depression, with similar associations found for boys and girls (Bogart et al., Reference Bogart, Elliott, Klein, Tortolero, Mrug, Peskin, Davies, Schink and Schuster2014; Earnshaw et al., Reference Earnshaw, Elliott, Reisner, Mrug, Windle, Emery, Peskin and Schuster2017). Research has shown that victimized adolescents exhibit key characteristics of depressive self-schemas, with stronger negative self-cognitions, weaker positive self-cognitions (Cole et al., Reference Cole, Dukewich, Roeder, Sinclair, McMillan, Will, Bilsky, Martin and Felton2014), and increased suicidal ideation and attempts (van Geel et al., Reference van Geel, Vedder and Tanilon2014). Additionally, ruminative cognitions about victimization experiences, and negative perceptions of the self and the future have been consistently linked to depression and depressive symptoms (Cole et al., Reference Cole, Dukewich, Roeder, Sinclair, McMillan, Will, Bilsky, Martin and Felton2014; Wang, Reference Wang2011). Wang (Reference Wang2011) proposed that this is because victimization reinforces negative evaluations about the self and the future, which undermines self-esteem and self-efficacy over time, leading to further negative cognitive styles.
Research also shows that, when compared to nonvictims, frequently victimized adolescents are two to three times more likely to develop an anxiety disorder (Stapinski et al., Reference Stapinski, Bowes, Wolke, Pearson, Mahedy, Button, Lewis and Araya2014). Relational victimization in particular has strong associations with social anxiety in younger and older groups of adolescents, both 2 months (Siegel et al., Reference Siegel, La Greca and Harrison2009) and 5 years later (Pickard et al., Reference Pickard, Happé and Mandy2018). As cognitions and emotions related to fear and threat are most closely associated with anxiety (Forbes et al., Reference Forbes, Fitzpatrick, Magson and Rapee2019), and adolescence is characterized by the salience of peer relationships and the importance of attaining social status, power, and peer acceptance (Rapee et al., Reference Rapee, Oar, Johnco, Forbes, Fardouly, Magson and Richardson2019), this relationship can be explained by victimization-induced hypervigilance and increased sensitivity to social threat, which, if sustained over time, can increase risk of ongoing social anxiety problems (Forbes et al., Reference Forbes, Fitzpatrick, Magson and Rapee2019). Notably, while Pickard et al. (Reference Pickard, Happé and Mandy2018) reported no sex differences, Siegel et al. (Reference Siegel, La Greca and Harrison2009) found that relational victimization predicted increases in later social anxiety for adolescent girls only. This was attributed to the higher level of interpersonal engagement by adolescent girls compared to boys, and the potential for boys’ responses to PV to be characterized by aggressive symptoms rather than social anxiety symptoms, suggesting that the relationship between PV and social anxiety may be more nuanced than the relationship between PV and depression.
In relation to the opposite relationship from internalizing problems to later PV, overt behaviors characteristic of social anxiety (e.g., social withdrawal, behavioral inhibition) and depression (e.g., apathy, crying, negativity) may elicit acts of aggression (Luchetti & Rapee, Reference Luchetti and Rapee2014), possibly motivated by bullies’ need for power and dominance (Crawford & Manassis, Reference Crawford and Manassis2011). Further, feelings of social anxiety and depression may prevent the formation of new peer relationships and limit social opportunities as youth move through secondary school, making them especially vulnerable to social exclusion and other negative interpersonal experiences (Siegel et al., Reference Siegel, La Greca and Harrison2009). In fact, research shows that internalizing behaviors appear to be less accepted by peers as children become older (Rubin et al., Reference Rubin, Bowker, Barstead, Coplan, Bukowski, Laursen and Rubin2018), and as anxious and depressed youth have smaller friendship networks (Rapee et al., Reference Rapee, Oar, Johnco, Forbes, Fardouly, Magson and Richardson2019), they have less social and emotional support, and thus less protection from perpetrators of PV (Crawford & Manassis, Reference Crawford and Manassis2011), which in turn can exacerbate their internalizing symptoms.
Sleep hygiene and sleep duration as mediators of the association between PV and internalizing symptoms
Sleep hygiene and duration as key mechanisms
Recent developments in the literature on prospective associations between PV, sleep, and internalizing problems highlight the importance of sleep as a potential mediator of the link between PV and internalizing problems among youth. The literature has explored a number of sleep mechanisms, including sleep deficit behaviors (e.g., difficulties getting to sleep; Chang et al., Reference Chang, Wu, Lin, Chang and Yen2019; Herkama et al., Reference Herkama, Turunen, Sandman and Salmivalli2019; van Geel et al., Reference van Geel, Goemans and Vedder2016), daytime dysfunction (e.g., sleepiness in class; Due et al., Reference Due, Holstein, Lynch, Diderichsen, Gabhain, Scheidt and Currie2005; Richardson et al., Reference Richardson, Oar, Fardouly, Magson, Johnco, Forbes and Rapee2019), subjective complaints (e.g., bad night’s sleep; Kubiszewski et al., Reference Kubiszewski, Fontaine, Potard and Gimenes2014; Tu et al., Reference Tu, Spencer, El-Sheikh and Erath2019), and nightmares (Biebl et al., Reference Biebl, DiLalla, Davis, Lynch and Shinn2011; Herkama et al., Reference Herkama, Turunen, Sandman and Salmivalli2019).
Operationalizations of sleep duration are regularly used, such as hours of sleep each night (Richardson et al., Reference Richardson, Oar, Fardouly, Magson, Johnco, Forbes and Rapee2019), irregularities between sleep and wake times and time spent in bed (Kubiszewski et al., Reference Kubiszewski, Fontaine, Potard and Gimenes2014; Tu et al., Reference Tu, Spencer, El-Sheikh and Erath2019; Lemola et al., Reference Lemola, Schwarz and Siffert2012). Given that sleep restriction is largely seen on school nights, many studies report adolescent sleep parameters for school nights only (e.g., Bartel et al., Reference Bartel, Scheeren and Gradisar2019; Richardson et al., 2018, 2021; Short et al., Reference Short, Gradisar, Lack, Wright and Carskadon2012). Further, while teenagers may be able to ‘catch up’ on sleep on weekends, this recovery sleep is not sufficient to overcome decrements in performance during the school week and researchers lose important information by simply averaging across school night and weekend sleep. Thus, in line with the previous literature, sleep duration was defined in the current study as the time spent asleep each school night, referred to henceforth as sleep duration.
Theoretical and empirical evidence suggests that sleep hygiene may also play a role in the associations between PV, sleep duration and internalizing symptoms. Sleep hygiene is defined as behaviors (i.e., activities, routines, cognitions) and states (i.e., physiological, emotional, and environmental) that “promote good sleep quality, adequate sleep duration and full daytime alertness” (p. 258, LeBourgeois, Reference LeBourgeois2005). The literature highlights a number of empirically supported conceptual domains of sleep hygiene, including physiological, behavioral, cognitive/emotional, environmental, daytime sleep, and sleep stability (Harsh et al., Reference Harsh, Easley and LeBourgeois2002; LeBourgeois, Reference LeBourgeois2005; Storfer-Isser et al., Reference Storfer-Isser, Lebourgeois, Harsh, Tompsett and Redline2013).
Poor sleep hygiene has been found to be a robust predictor of sleep problems such as poor sleep quality (LeBourgeois, Reference LeBourgeois2005), daytime sleepiness, and irregular sleep schedules (Bartel et al., Reference Bartel, Gradisar and Williamson2015), all of which are contributors or consequences of insufficient sleep duration. In particular, the literature consistently demonstrates a link between sleep hygiene and sleep duration. Indeed, Sun et al. (Reference Sun, Spruyt, Chen, Jiang, Schonfeld, Adams, Tseng, Shen and Jiang2014) demonstrated that better sleep hygiene using the full multidimensional Adolescent Sleep Hygiene Scale (ASHS; Harsh et al., Reference Harsh, Easley and LeBourgeois2002) was associated with earlier bedtimes and longer sleep duration. Galland et al. (Reference Galland, Gray, Penno, Smith, Lobb and Taylor2017) similarly demonstrate better sleep hygiene scores were associated with longer sleep duration, also using the full-scale ASHS. Further, two recent systematic reviews (Friedrich & Schlarb, Reference Friedrich and Schlarb2018; Hall & Nethery, Reference Hall and Nethery2019) demonstrate a positive association between sleep hygiene and sleep duration, suggesting that this association is robust.
PV as a critical interpersonal stressor
The dominant explanation for the mediating role of sleep hygiene and sleep duration lies in the understanding of PV as a critical interpersonal stressor for adolescents, which has negative physiological, cognitive, emotional, and behavioral impacts (Chang et al., Reference Chang, Wu, Wu, Lin, Yen and Chang2017, Reference Chang, Wu, Lin, Chang and Yen2019; Herkama et al., Reference Herkama, Turunen, Sandman and Salmivalli2019). PV has been shown to evoke feelings of threat and vigilance (Kubiszewski et al., Reference Kubiszewski, Fontaine, Potard and Gimenes2014), as well as fear, humiliation, and shame in adolescents (Chang et al., Reference Chang, Wu, Lin, Chang and Yen2019; Irwin et al., Reference Irwin, Li, Craig and Hollenstein2019). Dahl’s (Reference Dahl1996) widely cited vigilance-arousal theory of sleep disturbance posits that increased vigilance about the self and the environment interfere with sleep onset and maintenance, leading to reduced sleep quality and duration. Further, the literature highlights physiological and biological factors in this pathway between PV and dysregulated sleep. Spilsbury et al.’s (Reference Spilsbury, Korbin and Coulton2009) conceptual model highlights that violence-induced stress leads to dysregulation in brain areas associated with emotion regulation and executive processes, impacting sleep and functioning. Further, Chang et al. (Reference Chang, Wu, Wu, Lin, Yen and Chang2017) highlight that victimization is a stressor which triggers the abnormal release of cortisol, causing victimzzed adolescents to become hypervigilant and agitated, making it difficult to achieve the relaxation needed for sleep.
Accordingly, research shows that victims of PV have difficulty regulating their emotions and behaviors (King et al., Reference King, McLaughlin, Silk and Monahan2018; McLaughlin et al., Reference McLaughlin, Hatzenbuehler and Hilt2009) which can undermine their ability to engage in the behavioral, emotional and physiological self-regulatory practices (i.e., good sleep hygiene) that promote sleep preparedness and sleep quality (Lepore & Kliewer, Reference Lepore and Kliewer2013). Adolescents who are bullied may engage in a range of maladaptive strategies and practices at bedtime (i.e., poor sleep hygiene), which impact their sleep quality and duration. For example, staying awake to watch TV (behavioural), falling asleep listening to music (sleep environment), and overeating or drinking caffeine before bed (physiological).
Though there is currently no literature on the direct link between PV and sleep hygiene specifically, a growing number of studies have demonstrated an association between PV and various sleep problems in youth across adolescence, both concurrently (Kubiszewski et al., Reference Kubiszewski, Fontaine, Potard and Gimenes2014; van Geel et al., Reference van Geel, Goemans and Vedder2016) and prospectively (Biebl et al., Reference Biebl, DiLalla, Davis, Lynch and Shinn2011). Generally sex differences have not been observed (Kubiszewski et al., Reference Kubiszewski, Fontaine, Potard and Gimenes2014; van Geel et al., Reference van Geel, Goemans and Vedder2016) and are often not investigated (Kubiszewski et al., Reference Kubiszewski, Fontaine, Potard and Gimenes2014; Tu et al., Reference Tu, Spencer, El-Sheikh and Erath2019), however one study found that victimized girls exhibited higher vulnerabilities to sleep problems (Biebl et al., Reference Biebl, DiLalla, Davis, Lynch and Shinn2011). Tu et al.’s (Reference Tu, Spencer, El-Sheikh and Erath2019) recent longitudinal study of predominantly European American and African American 11–14 year-olds showed that youth-reported PV was associated with poorer sleep quality (e.g., not having a good night’s sleep) 10 months later, controlling for earlier levels of sleep quality and internalizing symptoms. Additionally, Sadeh et al.’s (Reference Sadeh, Tikotzky and Kahn2014) review highlights associations between PV and a number of facets of sleep, including sleep quality and duration.
Impacts on internalizing symptoms
The association between poor sleep and negative internalizing outcomes has been attributed to the important role that sleep plays in modulating affective neural systems and processing recent experiences (Astill et al., Reference Astill, Van der Heijden, Van IJzendoorn and Van Someren2012; Walker & van der Helm, Reference Walker and van der Helm2009). Poor sleep is associated with decreased emotion regulation and coping (Palmer et al., Reference Palmer, Oosterhoff, Bower, Kaplow and Alfano2018; Walker & van der Helm, Reference Walker and van der Helm2009), as well as increased reactivity to stress (Vargas & Lopez-Duran, Reference Vargas and Lopez-Duran2017), all of which are mechanisms by which sleep problems may increase risk for internalizing problems. Poor sleep may therefore dysregulate emotion processing systems and lead to deficits in emotion regulation, coping, and stress resistance, which have all been associated with subsequent internalizing problems (Eisenberg et al., Reference Eisenberg, Cumberland, Spinrad, Fabes, Shepard, Reiser and Guthrie2001). Thus, victimized adolescents may become caught in a vicious cycle of stress and sleep difficulties, which ultimately contribute to the development and maintenance of internalizing problems, such as anxiety and depression (Christina et al., Reference Christina, Magson, Kakar and Rapee2021; Forbes et al., Reference Forbes, Fitzpatrick, Magson and Rapee2019; Reijntjes et al., Reference Reijntjes, Kamphuis, Prinzie and Telch2010).
Sleep hygiene has also been directly linked with internalizing symptoms in a small number of studies. For example, Pieters et al. (Reference Pieters, Burk, Van der Vorst, Dahl, Wiers and Engels2015) found bidirectional relationships between internalizing symptoms and ‘sleep problems’, measured as a composite of sleep quality and the emotional-cognitive domain of sleep hygiene (LeBourgeois, Reference LeBourgeois2005). Another study by Santisteban et al. (Reference Santisteban, Bouchard, Tappe, Lane, Sommerville, Boursier and Gruber2018) showed that poorer mental illness was significantly correlated with greater emotional-cognitive arousal at bedtime. However, they found no association between mental illness and behavioral arousal (e.g., using electronics or exercising) at bedtime and did not comment on associations with other sleep hygiene domains. Finally, in a randomized control trial with depressed adults, participants allocated to the sleep hygiene conditions showed a significantly larger decrease in depressive symptoms post intervention when compared to those in the medication condition (Rahimi et al., Reference Rahimi, Ahmadpanah, Shamsaei, Cheraghi, Sadeghi Bahmani, Holsboer-Trachsler and Brand2016), suggesting sleep hygiene is causally linked with internalizing symptoms.
Meta-analytic evidence also demonstrates robust associations between sleep duration and internalizing symptoms (Astill et al., Reference Astill, Van der Heijden, Van IJzendoorn and Van Someren2012), with girls generally being more vulnerable than boys. For example, Short and Louca’s (Reference Short and Louca2015) laboratory study of 14–18 year-olds found that, while only one night of sleep deprivation could lead to mood deficits (e.g., anger, fatigue, confusion) the next day, only female participants exhibited increased depressed mood and anxiety. Growing longitudinal evidence also demonstrates associations between self-reported sleep problems and anxiety (Narmandakh et al., Reference Narmandakh, Roest, Jonge and Oldehinkel2020) and depression (Lovato & Gradisar, Reference Lovato and Gradisar2014), as well as parent-reported sleep problems and internalizing symptoms (Williamson et al., Reference Williamson, Zendarski, Lange, Quach, Molloy, Clifford and Mulraney2021). Further, Bai et al.’s (Reference Bai, Ricketts, Thamrin, Piacentini, Albano, Compton, Ginsburg, Sakolsky, Keeton, Kendall and Peris2020) study of predominantly White, non-Hispanic youth aged 11–26 found that dysregulated sleep (i.e., trouble sleeping, feeling drowsy, sleeplessness and nightmares) predicted clinician-rated anxiety and depression severity one year later, also reporting a smaller reciprocal effect. However, this finding of bidirectionality has not been replicated in later studies (Narmandakh et al., Reference Narmandakh, Roest, Jonge and Oldehinkel2020; Williamson et al., Reference Williamson, Zendarski, Lange, Quach, Molloy, Clifford and Mulraney2021).
Evidence of sleep hygiene and duration as mediators
The associations outlined above implicate both sleep hygiene and sleep duration as potential mediators of the relationship between PV and internalizing. To date, only two studies have addressed this hypothesis, however they have restricted their focus to sleep problems and depression only (Chang et al., Reference Chang, Wu, Lin, Chang and Yen2019; Herkama et al., Reference Herkama, Turunen, Sandman and Salmivalli2019). Herkama et al. (Reference Herkama, Turunen, Sandman and Salmivalli2019) found that both insomnia and nightmares mediated the relationship between PV and depressive symptoms, controlling for sex and school type in a sample of Finish 16–17 year olds. However, their reliance on cross-sectional data limits any conclusions about true mediation. In the only prospective study, Chang et al. (Reference Chang, Wu, Lin, Chang and Yen2019) showed that sleep problems mediated the association between PV and later depressive symptoms in 14–18 year old Taiwanese girls, but not at all in Taiwanese boys. Notably, both groups of researchers posited that PV is an interpersonal stressor that leads to sleep problems, impacting functioning and leading to increased depressive symptoms. However, these studies fail to address anxiety symptoms as an outcome or explore the potential mechanisms (e.g., sleep hygiene) linking PV to disturbed sleep and subsequent reductions in sleep duration. Additionally, both of these studies target a mid-to-late adolescent sample (14–19 years). Thus, despite the particular vulnerabilities that early adolescents face regarding the onset of PV, sleep problems, and internalizing problems, evidence for the role of sleep as a mediator in this age group is lacking.
The current study
The current study investigated sleep hygiene and sleep duration as potential individual and sequential mediators of the longitudinal relationship between PV and both social anxiety and depressive symptoms from early to mid-adolescence. Based on the empirical and theoretical evidence summarized above (e.g., Biebl et al., Reference Biebl, DiLalla, Davis, Lynch and Shinn2011; Christina et al., Reference Christina, Magson, Kakar and Rapee2021; Gini et al., Reference Gini, Card and Pozzoli2018; Reijntjes et al., Reference Reijntjes, Kamphuis, Prinzie and Telch2010; van Geel et al., Reference van Geel, Vedder and Tanilon2014), we posit that PV is an interpersonal stressor which will increase feelings of stress and vigilance (Dahl, Reference Dahl1996) and disrupt or impede adolescents’ ability to regulate their behavioural, environmental, physiological, emotional and cognitive processes when going to sleep (i.e., sleep hygiene). Consequently, this will reduce adolescents’ sleep duration due to delayed sleep onset, poor sleep maintenance, and early wake times (Friedrich & Schlarb, Reference Friedrich and Schlarb2018; Galland et al., Reference Galland, Gray, Penno, Smith, Lobb and Taylor2017; Hall & Nethery, Reference Hall and Nethery2019; Sun et al., Reference Sun, Spruyt, Chen, Jiang, Schonfeld, Adams, Tseng, Shen and Jiang2014). In turn, the cascading effects of poor sleep hygiene practices and reduced sleep duration will impact adolescents’ capacity to regulate, process, and cope with these stressful peer interactions (Palmer et al., Reference Palmer, Oosterhoff, Bower, Kaplow and Alfano2018; Vargas & Lopez-Duran, Reference Vargas and Lopez-Duran2017; Walker & van der Helm, Reference Walker and van der Helm2009), and increase internalizing symptoms (i.e., depression and social anxiety). Finally, given the evidence that girls tend be at higher risk for both sleep problems and internalizing symptoms (Altemus et al., Reference Altemus, Sarvaiya and Neill Epperson2014; Baker et al., Reference Baker, Yűksel, de Zambotti, Attarian and Viola-Saltzman2020; Kessler et al., Reference Kessler, Berglund, Demler, Jin, Merikangas and Walters2005; Rapee et al., Reference Rapee, Oar, Johnco, Forbes, Fardouly, Magson and Richardson2019), the current study also controlled for sex in the primary analysis and then explored possible sex differences within a multigroup framework.
Direct and indirect effects in the opposite direction were also explored (e.g., internalising symptoms to sleep variables to PV). While there is robust evidence supporting a bidirectional relationship between PV and internalizing problems (Christina et al., Reference Christina, Magson, Kakar and Rapee2021), evidence for the bidirectional nature of the sleep-internalizing association remains inconsistent, with some studies finding reciprocal effects from internalizing to sleep (Bai et al., Reference Bai, Ricketts, Thamrin, Piacentini, Albano, Compton, Ginsburg, Sakolsky, Keeton, Kendall and Peris2020) and others finding no reciprocal effects (Narmandakh et al., Reference Narmandakh, Roest, Jonge and Oldehinkel2020; Williamson et al., Reference Williamson, Zendarski, Lange, Quach, Molloy, Clifford and Mulraney2021). Further, studies examining the PV-sleep relationship are either correlational, and so cannot infer directionality (Kubiszewski et al., Reference Kubiszewski, Fontaine, Potard and Gimenes2014; van Geel et al., Reference van Geel, Goemans and Vedder2016) or, where longitudinal, only examine the relationship in one direction (i.e., PV to sleep; Biebl et al., Reference Biebl, DiLalla, Davis, Lynch and Shinn2011; Tu et al., Reference Tu, Spencer, El-Sheikh and Erath2019).
Accordingly, the following predictions were made: increases in PV will be bidirectionally associated with increases in depressive and social anxiety symptoms (H1); increases in PV will be associated with worsening sleep hygiene and decreased sleep duration, and worsening sleep hygiene and decreases in sleep duration will be associated with increases in depressive and social anxiety symptoms (H2); and sleep hygiene and sleep duration will mediate the association between PV and both depressive and social anxiety symptoms (H3). Finally, in relation to exploring the direct and indirect effects between sleep variables, internalizing symptoms, and PV in the opposite direction (sleep to PV, internalizing to sleep), no specific hypotheses were formulated as previous literature has been inconsistent or lacking.
Method
Participants
Participants were 528 boys (51.1%) and girls who participated in at least one wave of a five-wave longitudinal study entitled the ‘Risk to Adolescent Well-being (RAW) Project’. The aim of this longitudinal study was to examine risk and protective factors for social emotional disorders during adolescence (Rapee et al., Reference Rapee, Oar, Johnco, Forbes, Fardouly, Magson and Richardson2019). At T1, all participants resided in Australia, were in Grade 6 at school, and ranged in age from 10 to 12 years (M age = 11.19, SD = .55). Most participants were born in Australia (90.6%), spoke English as a first language (96.4%), and were in the top two quintiles of household income (68.4%) as classified by the Australian Bureau of Statistics (2022). The majority of the sample identified as White (81.9%), the remainder identified as Asian (6.4%), Middle Eastern (1.5%), or other (10.2%; Eurasian 4.4%, European 2.1%, The Americas 1.3%, Indian 1.1%, Maori/Islander 0.9%, unknown 0.4%). In subsequent waves, data were returned by 497 youth (51.6% boys; M age = 12.66, SD = .56) at T2, 478 youth (52.1% boys; M age = 13.68, SD = .57) at T3, 437 youth (51.7% boys; M age = 14.74, SD = .56) at T4, and 422 youth (51.9% boys; M age = 15.77, SD = .48) at T5, resulting in an overall attrition rate of 20.1% over the five measurement occasions.
Drop out analyses revealed that there were no differences between those who did and did not drop out of the study on levels of PV (p’s .209 – .916), depression (p’s .115 – .810), or social anxiety (p’s .094 – .672). There were significant group differences in sleep hygiene at T1 (t (526) = −2.34, p = .020), and T3 (t (474) = −2.51, p = .012) with those who ultimately dropped out of the study reporting more negative sleep hygiene practices (T1: M = 2.40, SD = .56; T3: M = 2.44, SD = .68) than those that remained (T1: M = 2.26, SD = .57; T3: M = 2.24, SD = .56). Correspondingly, there were significant differences in sleep duration at T1 (t (502) = -2.47, p = .014) and T3 (t (475) = -2.34, p = .020) with those leaving the study reporting less sleep on school nights (T1: M = 9.04, SD = 1.33; T3: M = 8.09, SD = 1.14) than those that stayed (T1: M = 9.36, SD = 1.13; T3: M = 8.47, SD = 1.14). There was no significant difference in the number of boys versus girls that dropped out of the study (x 2 (1) = 0.22, p = .882).
Measures
Peer victimization
PV was measured using a shortened version of the Revised Olweus Bullying/Victim Questionnaire (R-OBV-Q; Solberg & Olweus, Reference Solberg and Olweus2003). The shortened R-OBV-Q used in the current study was provided by Solberg and Olweus through personal communication and comprised of items from the victim subscale that had produced the best psychometric properties in their previous studies. The shortened R-OBV-Q comprised of 6 items measuring the frequency of general (1-item), physical (1-item), verbal (1-item), relational (2-items), and cyber (1-item) PV (e.g., “I was hit, kicked, pushed, shoved around, or locked indoors”) during the last school term (note there are four 10-week school terms in the Australian school year). Responses were measured on a frequency scale ranging from 0 (no, this didn’t happen to me this term) to 2 (yes, this happened to me three or more times). Scores on each of the six items were averaged to form a single mean score with higher scores reflecting more frequent PV. Previous research has shown the R-OBV-Q to have good internal reliability (e.g., Young, Reference Young2020, α = .85) and good psychometric properties generally (Solberg & Olweus, Reference Solberg and Olweus2003). In the current study the internal consistency of the shortened R-OBV-Q was acceptable at each measurement occasion (T1 and T2: α = .73; T3: α = .77; T4: α = .74; and T5: α = .76).
Sleep hygiene
Sleep hygiene was measured using subscales from the Adolescent Sleep Hygiene Scale (ASHS; Harsh et al., Reference Harsh, Easley and LeBourgeois2002). The ASHS is a 28-item, self-report measure that assesses sleep-facilitating and sleep-inhibiting practices in adolescents across eight subscales, five of which were used in the current study. Due to the large number of risk and protective factors examined as part of the RAW Project, only the following selected subscales were administered: physiological (5 items, e.g., “I go to bed feeling hungry”), behavioral arousal (3 items, e.g., “I go to bed and do things in my bed that keep me awake (e.g., watching TV, reading)”), cognitive/emotional (6 items, e.g., “I go to bed and worry about things happening at home or at school”), sleep environment (5 items, e.g., “I fall asleep while listening to loud music”) and bedtime routine (1 item; e.g., “I use a bedtime routine (e.g., bathing, brushing teeth, reading)”) factors, totalling 20-items which were rated on a 6-point scale ranging from 1 (never) to 6 (always). Subscale scores were generated by averaging relevant items. The total ASHS score used in the current study was derived by averaging each subscale score (ranging 1 to 6). The total ASHS score was reverse coded so that higher scores were indicative of worse sleep hygiene practices. Consistent with previous research (Storfer-Isser et al., Reference Storfer-Isser, Lebourgeois, Harsh, Tompsett and Redline2013), the reliability of the total ASHS scale was acceptable at all time points (T1: α = .76; T2: α = .78; T3: α = .81; T4 and T5: α = .82).
Sleep duration
The average number of hours of sleep on a school night was measured using a single retrospective item asking adolescent respondents to indicate “How many hours sleep do you usually get each night on a school night?” with respondents answering in whole numbers.
Depression
Depressive symptoms were measured using the 13-item Short Mood and Feelings Questionnaire – Child (SMFQ-C; Angold et al., Reference Angold, Costello, Messer, Pickles, Winder and Silver1995). Participants were asked to indicate how true each statement (e.g., “I felt miserable or unhappy”) was for them over the past two weeks on a 3-point scale from 0 (not true) to 2 (always true). Scores were summed across all items to create a total score ranging from 0 to 26 with higher scores indicating more depressive symptoms. While the SMFQ is not a diagnostic tool, the original authors recommend using a cut-off score of 8 to indicate elevated symptoms of depression. The number of participants meeting this criteria in the current study were: 105 (19.9%) at T1, 76 (14.4%) at T2, 90 (17%) at T3, 129 (24.4%) at T4, and 146 (27.7%) at T5. Mirroring previous research (e.g., Angold et al., Reference Angold, Costello, Messer, Pickles, Winder and Silver1995; Sharp et al., Reference Sharp, Goodyer and Croudace2006), the measure demonstrated good reliability across all five time points in the current study (T1: α = .88; T2: α = .89; T3: α = .92; T4: α = .94; and T5: α = .94).
Social anxiety
Social anxiety symptoms were assessed using the 6-item social phobia subscale of the Spence Children’s Anxiety Scale – Child (SCAS-C; Spence, Reference Spence1998). Participants rated how often each of the items listed (e.g., “I worry what other people think of me”) happens to them on a scale of 0 (never true) to 3 (always true). Scores were summed to create a total score for social anxiety, with possible scores ranging from 0 to 27. Although not a diagnostic instrument, it is recommended that a cut off score of 8 for girls and 10 for boys be used to indicate elevated symptom levels of social anxiety requiring further review. In the present sample, 79 (15%) met that criteria at T1, 70 (13.3%) at T2, 73 (13.8%) at T3, 100 (18.9%) at T4, and 129 (24.4%) at T5. Consistent with prior research (e.g., Rapee et al., Reference Rapee, Oar, Johnco, Forbes, Fardouly, Magson and Richardson2019), the Cronbach alpha values for the social anxiety subscale across all time points were acceptable (T1: α = .76; T2 and T3: α = .78; T4: α = .82; and T5: α = .84).
Procedure
The current study was part of the larger RAW Project. Following the necessary ethical approval, recruitment was based on convenience sampling (e.g., word of mouth, social media advertising, and flyers distributed in schools, sports clubs, medical centers etc.). Informed consent was obtained by all self-selecting participants and their primary caregivers who were recruited between August 2016 and July 2017 when youth were in grade 6 at school. The current study used data collected through an annual online questionnaire administered through the Qualtrics platform which took between 40 and 60 minutes to complete. The survey comprised a range of measures relevant to the larger RAW Project along with those used in the present study. Participants received $100 and were gifted with a small gratitude bag valued at AUD$20–$30 for each year of participation.
Data analysis
SPSS version 27 (IBM Corp, 2020) was used for all data preparation, aggregation, assumption testing and descriptive analyses. For the drop-out analyses, potential differences were explored using independent t-tests and chi-square difference testing for continuous and categorical variables respectively. Mplus version 8 (Muthén & Muthén, Reference Muthén and Muthén2017) was used for the main analysis using the maximum likelihood estimator (MLR) to account for any non-normality of the data and full information maximum likelihood (FIML) estimation to account for missing data.
Autoregressive cross-lagged panel models (CLPMs) controlling for sex were used to examine the bidirectional associations between PV, sleep variables (sleep hygiene and duration) and internalizing outcomes (symptoms of depression and social anxiety), with separate models estimated for symptoms of depression and social anxiety. As recommended by Orth et al. (Reference Orth, Clark, Donnellan and Robins2021) all autoregressive and cross-lagged paths were constrained to be equal across measurement occasions and the residuals of each variable were correlated within time-points. After initial models were estimated, hypothesized indirect effects were explored when the paths between the different variables were significant across three consecutive time points. The indirect paths were estimated using the model indirect command in Mplus, with 5,000 bootstrap replications.
We also looked at the correlations between the variables of interest and a number of potential covariates which included: sex, ethnicity, age, family income, parent education, country of birth, language spoken within the home, and whether either parent (or primary caregiver) had a current or past mental illness. Of these, only sex (r’s = .10 – .44) and mother’s history of mental illness (r’s = .11 – .16) were significantly associated with at least some of the variables under study. Thus, both were controlled for in the CLPMs.
Further, although the random intercept cross lagged panel model (RI-CLPM) has been proposed as a superior alternative to the CLPM (e.g., Hamaker et al., Reference Hamaker, Kuiper and Grasman2015) we chose to run traditional CLPMs for two reasons. First, although the RI-CLPM enables researchers to assess prospective within-person effects by partialling out the between-person variance using latent random intercepts, it does not allow researchers to test the prospective between-person effects (Orth et al., Reference Orth, Clark, Donnellan and Robins2021). Second, recent evidence suggests that power can be an issue with the RI-CLPM as it requires large sample sizes (>1000) to accurately detect even moderate effect sizes (Masselink et al., Reference Masselink, Van Roekel, Hankin, Keijsers, Lodder, Vanhalst and Oldehinkel2018). Therefore, as the research questions in the current study were primarily concerned with the prospective between-person differences (i.e., those that were and were not victimized), and the size of the current sample was 528, we chose to follow the recommendations of Orth et al. (Reference Orth, Clark, Donnellan and Robins2021) and examine between-person effects via CLPMs.
Potential sex moderation was tested using a multigroup analysis framework whereby the unconstrained model was simultaneously estimated for boys and girls, and then again with equality constraints imposed on all model paths for boys and girls. Evidence of moderation was examined using the criteria recommend by Chen (Reference Chen2007) with CFI changes greater than .01, and RMSEA changes greater than .015 as indicative of moderation. Model fit was evaluated using the comparative fit index (CFI) and root mean square error of approximation (RMSEA) with CFI values greater than .90 and .95, and RMSEA values below .080 and .050, indicative of acceptable and good model fit respectively (Hooper et al., Reference Hooper, Coughlan and Mullen2008). Lastly, given that several models were estimated within this study, the Benjamini–Hochberg procedure was carried out using a paper wide false discovery rate of 0.05, yielding an adjusted p-value of .039.
Results
Descriptive results
Univariate descriptive statistics for each of the study variables and t-test results for sex are presented in Table 1. As shown, participants engaged in fewer sleep hygiene practices over time, and PV and sleep duration decreased over the course of the study for both boys and girls. Depression and social anxiety increased markedly for girls and tended to fluctuate slightly for boys. There were no significant sex differences in the frequency of PV, whereas girls reported significantly higher levels of social anxiety symptoms than boys at all time points. Girls also reported significantly higher levels of depressive symptoms at T2, T3 and T4, more negative sleep hygiene practices at T3 and T5, and less sleep than boys at T3, T4, and T5.
Table 1. Descriptive statistics and independent t-test results for sex
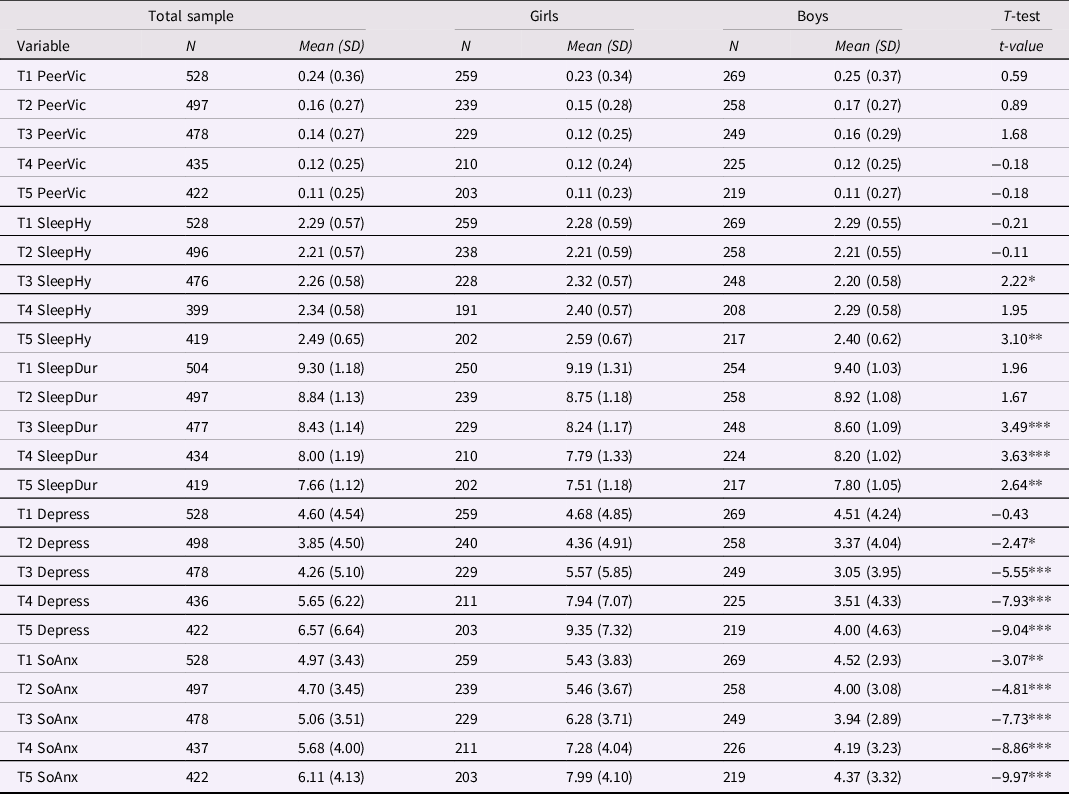
Note. *** p < .001, ** p < .01, *p < .039. PeerVic = peer victimization, SleepHy = sleep hygiene, SleepDur = sleep duration, Depress = depressive symptoms, SoAnx = social anxiety symptoms.
Bivariate correlations between each of the study variables are presented in Table 2. As shown, PV was moderately correlated with depression and social anxiety, weakly correlated with sleep duration, and had small correlations with sleep hygiene. Sleep hygiene was moderately correlated with sleep duration, and symptoms of depression and social anxiety, whereas sleep duration showed only negligible to small associations with depressive symptoms and social anxiety symptoms.
Table 2. Bivariate correlations between study variables
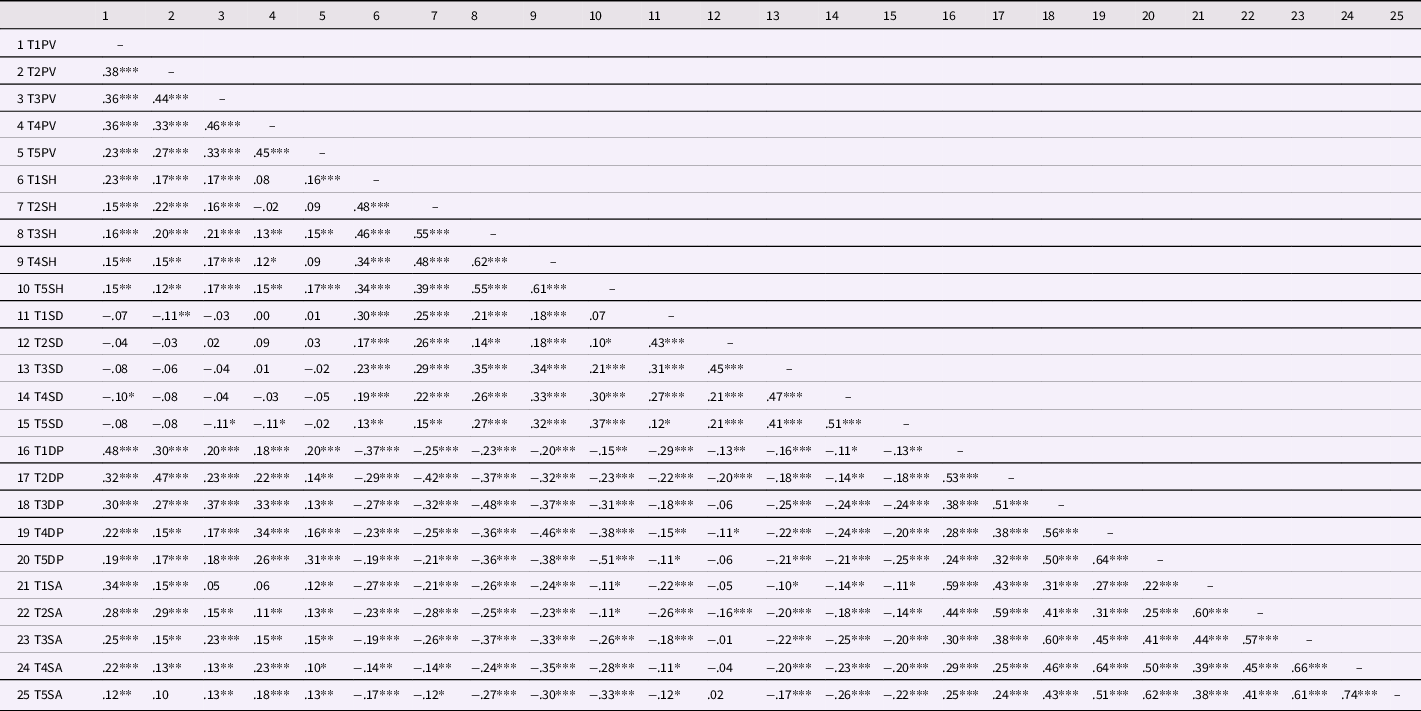
Note. *** p < .001, ** p < .01, *p < .039. PV = peer victimization, SH = sleep hygiene, SD = sleep duration, DP = depressive symptoms, SA = social anxiety symptoms.
Main analyses
The two initial CLPMs testing the unique associations between PV, sleep, and internalizing symptoms while controlling for sex and mother’s history of mental illness provided an adequate fit to the data (CFI > .90 and RMSEA < .080). However, mother’s history of mental illness was not uniquely concurrently or prospectively associated with any variables in either model, and as the pattern of results remained the same with and without this covariate, it was subsequently trimmed from the models. Thus, results reported below pertain to the CLPMs controlling for sex only.
Direct effects between PV, sleep hygiene, sleep duration, and depressive symptoms
The CLPM examining the reciprocal longitudinal associations between PV, sleep hygiene, sleep duration, and depressive symptoms provided an acceptable fit to the data (x 2 (N = 476) = 379.32, df = 156, CFI = .91, RMSEA = .055 [95% CI .048, .062]). As shown in Figure 1, all autoregressive paths were positive and significant, and showed moderate stability over time. PV and depressive symptoms were reciprocally associated over time whereby increases in PV predicted increases in depressive symptoms 12 months later and vice versa. PV also positively predicted increases in poor sleep hygiene practices 12 months later, although there was no evidence of the opposite association. There was no direct association between PV and sleep duration over time in either direction. Sleep duration and sleep hygiene were also negatively bidirectionally associated over time with decreases in sleep duration predicting worsening sleep hygiene 12 months later, and poor sleep hygiene predicting decreased sleep duration 12 months later. Finally, poor sleep hygiene predicted increases in depression 12 months later, but depression did not predict changes in sleep hygiene.
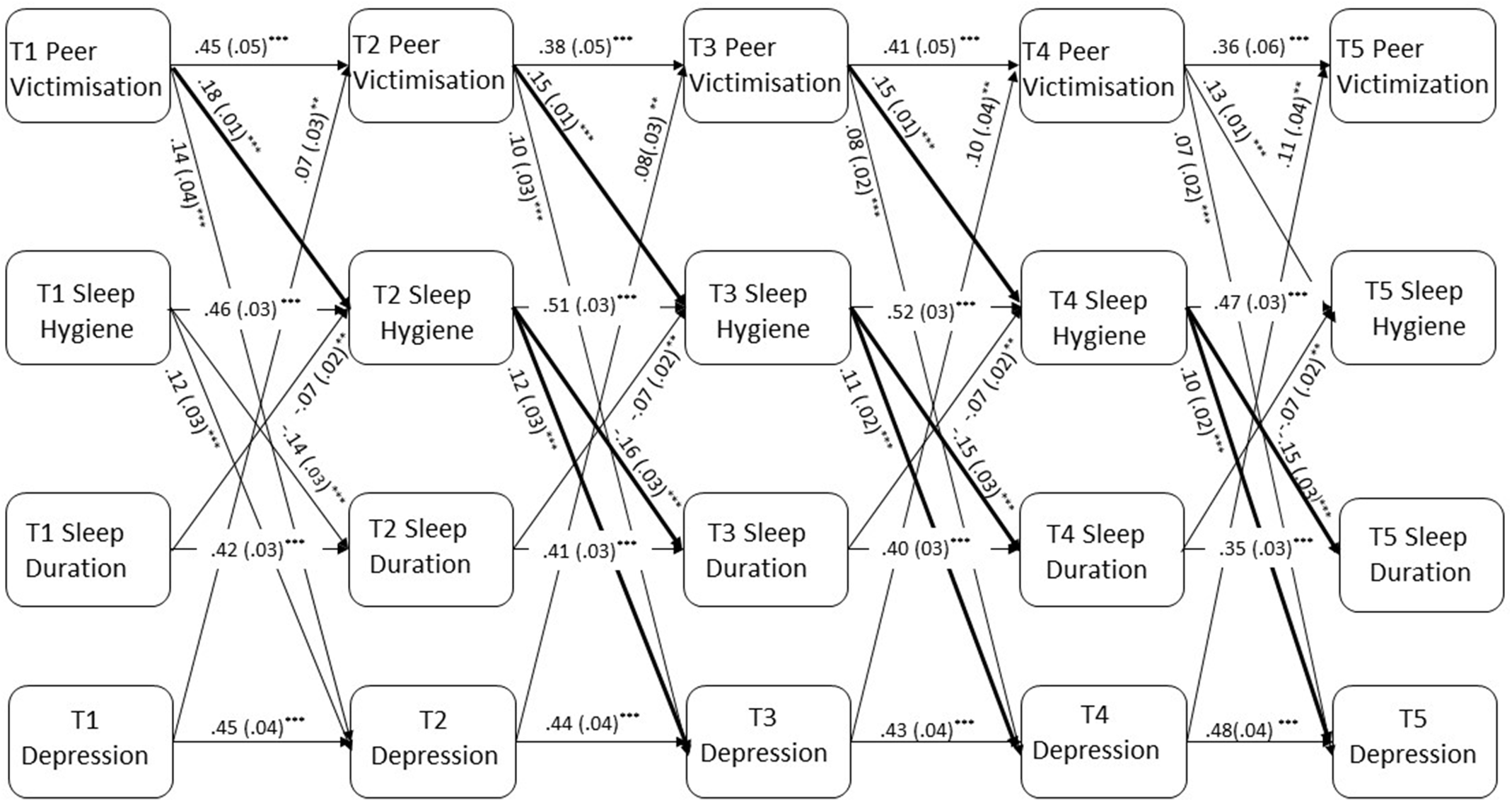
Figure 1. Cross-lagged panel model examining bidirectional associations between PV, sleep hygiene and duration, and depressive symptoms. Note. All cross-lagged paths were included in the estimated model but only the significant paths are shown. Values displayed in Figure 1 are standardized beta coefficients and their corresponding standard errors are shown in parentheses. Bolded paths represent significant indirect effects across all waves: indirect effect 1 = PV > sleep hygiene > depressive symptoms; indirect effect 2 = PV > sleep hygiene > sleep duration. *p < .039, **p < .01, ***p < .001.
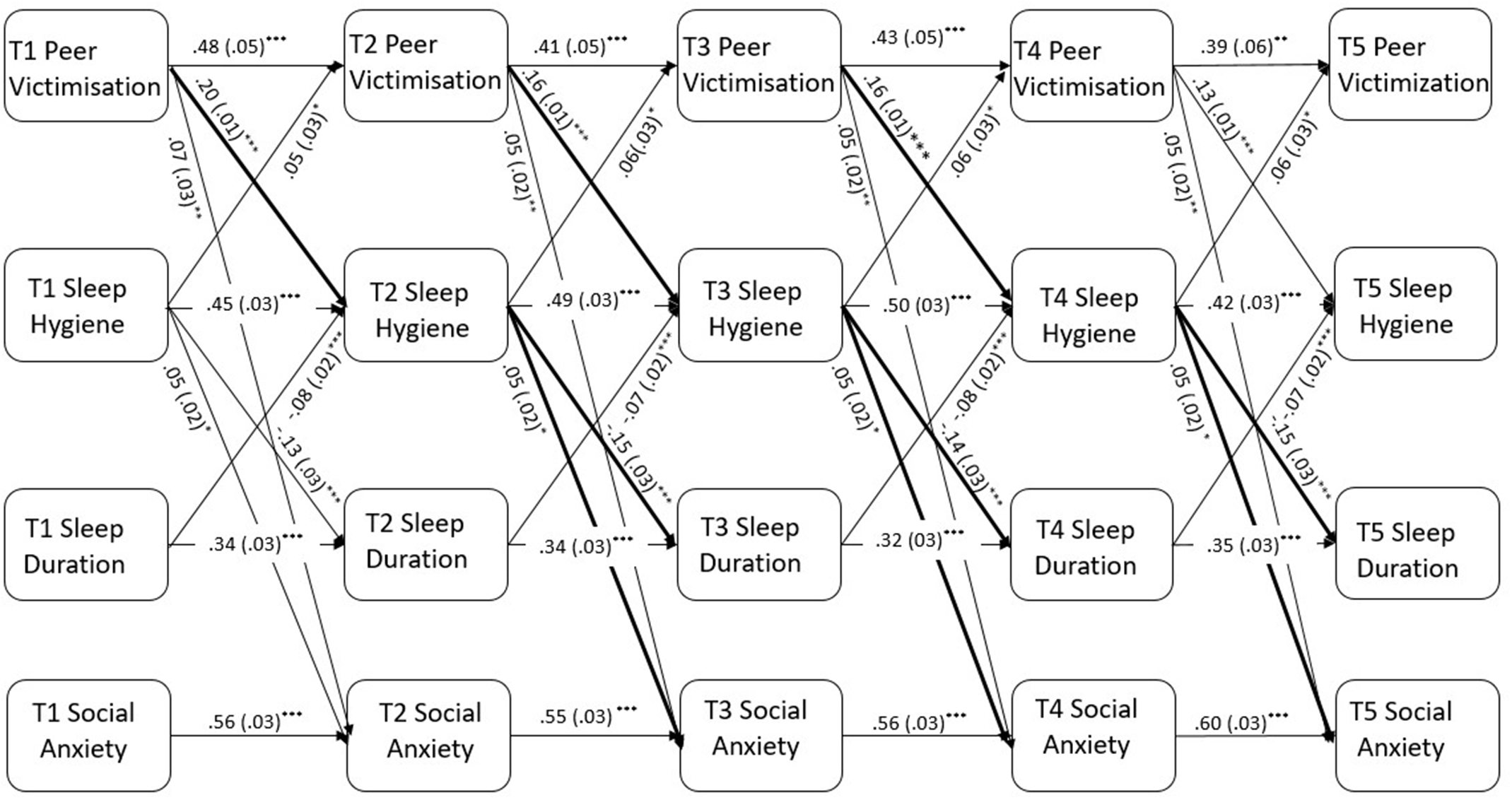
Figure 2. Cross-lagged panel model examining bidirectional associations between PV, sleep hygiene and duration, and social anxiety. Note. All cross-lagged paths were included in the estimated model but only the significant paths are shown. Values displayed in Figure 2 are standardized beta coefficients and their corresponding standard errors are shown in parentheses. Bolded paths represent significant indirect effects across all waves: indirect effect 1 = PV > sleep hygiene > social anxiety symptoms; indirect effect 2 = PV > sleep hygiene > sleep duration. *p < .039, **p < .01, ***p < .001.
Indirect effects between PV, sleep hygiene, sleep duration, and depressive symptoms
As there were significant direct paths from PV to sleep hygiene and from sleep hygiene to depressive symptoms across three consecutive waves, the hypothesized indirect effects were explored. Results showed that the indirect path from PV to depressive symptoms was partially mediated by sleep hygiene (b = .35, SE = .08, p < .001 [95% CI .23 – .47]), and the indirect path from PV to sleep duration was fully mediated by sleep hygiene (b = −.09, SE = .02, p < .001 [95% CI −.13 to − .06]. There was no support for the hypothesized sequential mediation of PV on depressive symptoms via sleep hygiene and sleep duration.
Direct effects between PV, sleep hygiene, sleep duration, and social anxiety symptoms
The CLPM examining the bidirectional longitudinal associations between PV, sleep hygiene, sleep duration, and social anxiety symptoms provided an adequate fit to the data (x 2 (N = 475) = 370.57, df = 156, CFI = .91, RMSEA = .054 [95% CI .047, .061]). As shown in Figure 2, all autoregressive paths were positive and significant, and showed moderate stability over time. PV significantly predicted social anxiety over time but in contrast to the depression model, this association was not reciprocal. PV and sleep hygiene were reciprocally associated across all waves, with increases in PV predicting worsening sleep hygiene which in turn predicted further increases in PV. There were no significant direct prospective associations between PV and sleep duration, or social anxiety and sleep duration, in either direction. As in the depression model, sleep duration and sleep hygiene were negatively bidirectionally associated over time, with decreased sleep duration predicting worsening sleep hygiene, and poor sleep hygiene predicting decreases in sleep duration. Finally, PV and sleep hygiene also significantly predicted social anxiety symptoms at all waves, however there was no evidence for reverse associations.
Indirect effects between PV, sleep hygiene, sleep duration, and social anxiety symptoms
As there were significant direct paths between PV, sleep, hygiene, and social anxiety symptoms across consecutive waves, the hypothesized indirect effects were investigated. Results revealed that the path from PV to social anxiety symptoms was partially mediated by sleep hygiene (b = .10, SE = .05, p < .039 [95% CI .02 – .17]), and the path from PV to sleep duration was fully mediated by sleep hygiene (b = −.09, SE = .02, p < .001 [95% CI −.12 to − .06]). There was no evidence of any other individual or sequential mediation and significant results are summarized in Figure 2.
Multigroup analyses
Depression model
Multigroup analyses revealed that imposing gender equality constraints on the paths in model assessing associations between PV, sleep hygiene, sleep duration, and depression did not adversely affect model fit, as indicated by a nonsignificant Satorra-Bentler scaled chi-square difference test (p = .680), no change in the RMSEA, and a CFI change of less than .01 (ΔCFI = .005).
Social anxiety model
Multi-group analyses revealed that imposing gender equality constraints on the paths of the model assessing PV, sleep hygiene, sleep duration, and social anxiety did not adversely affect model fit, as although the Satorra-Bentler scaled chi-square difference test was significant (Δ x 2 (Δ df = 16) = 28.95, p = .024), there was no change in the RMSEA value and the change in the CF1 value did not exceed 0.01 (Δ CFI = .005). Therefore it was concluded that there was no evidence of sex differences in either the depression or social anxiety models tested.
Discussion
The current study aimed to untangle the role that sleep plays in the link between PV and internalizing symptoms. Specifically, we aimed to investigate sleep hygiene and sleep duration as potential individual and sequential mediators of the longitudinal relationship between PV and both depression and social anxiety in pre- to mid-adolescents. The CLPM results showed partial support for the expected associations, which were consistent across boys and girls. Each specific hypothesis is discussed in turn below.
PV, depression and social anxiety
As expected, PV was a positive predictor of depressive symptoms 12 months later, consistent with previous research on the relationship between PV and internalizing symptoms (Christina et al., Reference Christina, Magson, Kakar and Rapee2021; Reijntjes et al., Reference Reijntjes, Kamphuis, Prinzie and Telch2010), as well as the specific relationships between PV and depression (Bogart et al., Reference Bogart, Elliott, Klein, Tortolero, Mrug, Peskin, Davies, Schink and Schuster2014; Earnshaw et al., Reference Earnshaw, Elliott, Reisner, Mrug, Windle, Emery, Peskin and Schuster2017). Additionally, the association between PV and depression was bidirectional at each time point, replicating meta-analytic summaries of the extant literature (Christina et al., Reference Christina, Magson, Kakar and Rapee2021; Reijntjes et al., Reference Reijntjes, Kamphuis, Prinzie and Telch2010), with a novel focus on early to mid-adolescence. This indicates that adolescents who exhibit high levels of depressive symptoms are at increased risk for future victimization which is consistent with Liu and Alloy’s (Reference Liu and Alloy2010) stress-generation hypothesis, whereby depressive vulnerabilities increase susceptibility to stressful events, due in part, to the tendency of depressed individuals being more socially withdrawn and lacking in social skills.
While the reciprocal effect is well-established for PV and depression, very little research has examined the bidirectional effects between PV and social anxiety (e.g., a recent meta-analysis found that only three out of 85 studies examined social anxiety specifically). Thus, the current study finding that PV was a positive predictor of social anxiety symptoms 12 months later is consistent with, and adds to, the limited literature on the specific longitudinal relationship between PV and social anxiety, which to date, has only focused on relational victimization (see Pickard et al., Reference Pickard, Happé and Mandy2018; Siegel et al., Reference Siegel, La Greca and Harrison2009). This result is consistent with suggestions that PV may cause hypervigilance and reactivity to interpersonal stressors, increasing the risk of developing social anxiety symptoms (Pickard et al., Reference Pickard, Happé and Mandy2018; Siegel et al., Reference Siegel, La Greca and Harrison2009; Stapinski et al., Reference Stapinski, Bowes, Wolke, Pearson, Mahedy, Button, Lewis and Araya2014).
However, inconsistent with predictions, the association between PV and social anxiety was not bidirectional, as social anxiety did not predict PV. This unidirectional finding is consistent with some longitudinal evidence (Vernberg et al., Reference Vernberg, Abwender, Ewell and Beery1992; Storch et al., Reference Storch, Masia-Warner, Crisp and Klein2005), but is inconsistent with other previous studies, which found bidirectional relationships between PV and internalizing symptoms generally (Christina et al., Reference Christina, Magson, Kakar and Rapee2021; Reijntjes et al., Reference Reijntjes, Kamphuis, Prinzie and Telch2010) and small but significant unique bidirectional relationship between relational PV and social anxiety specifically (Siegel et al., Reference Siegel, La Greca and Harrison2009).
It is possible that the age of participants explain these discrepant findings as the current study, along with the two previous studies (Vernberg et al., Reference Vernberg, Abwender, Ewell and Beery1992; Storch et al., Reference Storch, Masia-Warner, Crisp and Klein2005) finding only a unidirectional relationship, examined the associations from early to mid-adolescence (11−15 years), whereas, Siegel et al’s (Reference Siegel, La Greca and Harrison2009) bidirectional findings included older adolescents aged 14−19 years. As social anxiety typically emerges in mid-adolescence (Rapee et al., Reference Rapee, Oar, Johnco, Forbes, Fardouly, Magson and Richardson2019), it is possible that the current study did not capture youth with more serious social anxiety symptoms which may have a greater impact on PV from mid- to late adolescence. Collectively, this small body of evidence suggests that PV is linked with an increase in social anxiety symptoms from early to mid-adolescence, with a later reciprocal association emerging from mid- to late adolescence. However, more longitudinal research examining the effect of age on these bidirectional associations is needed.
PV and sleep
Consistent with our prediction, increases in PV were associated with worsening sleep hygiene 12 months later, making this the first longitudinal study directly linking PV with sleep hygiene. This novel finding adds to the literature already demonstrating a longitudinal relationship between PV and varying sleep problems (Biebl et al., Reference Biebl, DiLalla, Davis, Lynch and Shinn2011; Kubiszewski et al., Reference Kubiszewski, Fontaine, Potard and Gimenes2014; Tu et al., Reference Tu, Spencer, El-Sheikh and Erath2019; van Geel et al., Reference van Geel, Goemans and Vedder2016). Additionally, the current study found a bidirectional association between PV and sleep hygiene when social anxiety, but not depressive symptoms was the outcome. This finding advances the PV-sleep literature by providing novel support for bidirectionality, with previous studies being correlational and/or only examining this relationship in one direction (i.e., PV to sleep; Biebl et al., Reference Biebl, DiLalla, Davis, Lynch and Shinn2011; Tu et al., Reference Tu, Spencer, El-Sheikh and Erath2019). While this finding will need to be replicated in future research, it suggests that the reciprocal relationship from sleep hygiene to PV may be specific to social anxiety as an outcome and should be explored further in future research.
Inconsistent with our predictions, the prospective association between PV and youth-reported sleep duration on school nights was not significant. This finding does not align with previous research, which has found significant associations between PV and self-reported sleep/wake patterns (i.e., usual bed and wake-up times; Kubiszewski et al., Reference Kubiszewski, Fontaine, Potard and Gimenes2014). This in part may be due to the fact that within the present study sleep duration was only assessed using a single-item measure which may not have accurately captured participants’ true sleep duration. Future research should use well established measures of sleep duration such as the Pittsburgh Sleep Quality Index, combining child and parent report, using sleep diaries, or objective measures such as wrist actigraphy. However, prior research has utilised numerous different measures of ‘sleep problems’, which, along with the current findings, suggests that different sleep measures may be differentially related to PV (i.e., sleep problems may be more closely linked than sleep duration). Nevertheless, these results indicate that sleep hygiene is important to examine when investigating the link between PV and sleep problems generally, and that future research should continue to investigate the process or mechanisms by which PV can lead to specific sleep problems in adolescents.
Findings on the relationship between the two sleep measures showed that poorer sleep hygiene was associated with decreases in sleep duration 12 months later. This aligns with the literature, which shows that sleep hygiene behaviors can promote or inhibit healthy sleep (LeBourgeois, Reference LeBourgeois2005; Walker et al., Reference Walker, Johnson, Miaskowski, Lee and Gedaly-Duff2010), and are specifically associated with sleep duration (Friedrich & Schlarb, Reference Friedrich and Schlarb2018; Hall & Nethery, Reference Hall and Nethery2019; Sun et al., Reference Sun, Spruyt, Chen, Jiang, Schonfeld, Adams, Tseng, Shen and Jiang2014). This relationship was also bidirectional, suggesting a negative mutually reinforcing cycle whereby poor sleep hygiene predicts decreased sleep duration, and those experiencing decreased sleep duration then engage in more unhealthy sleep hygiene practices (e.g., consuming coffee and energy drinks, daytime napping) to compensate for the lack of sleep, resulting in further inadequate sleep (Irish et al., Reference Irish, Kline, Gunn, Buysse and Hall2015).
Sleep, depression, and social anxiety
Consistent with our hypotheses, worsening sleep hygiene was associated with increases in depressive and social anxiety symptoms. However, inconsistent with predictions, decreases in sleep duration were not directly associated with these outcomes. This latter finding does not align with the literature, which has shown concurrent correlational associations between participant-reported sleep duration and internalizing symptoms (Astill et al., Reference Astill, Van der Heijden, Van IJzendoorn and Van Someren2012). As previously stated, this inconsistent finding maybe due to the fact that sleep duration was assessed with only a single item. However, it may also suggest that while sleep duration may be concurrently associated with internalizing symptoms, it may be a less effective unique predictor of internalizing symptoms over time, especially when sleep hygiene is included in the same model. Additionally, the current study focused on the longitudinal associations between variables, controlling for previous levels of each variable at each time point and the concurrent associations between them. This more stringent analysis may explain why the small concurrent relationships found in the current study (see Table 2), and reported elsewhere (Astill et al., Reference Astill, Van der Heijden, Van IJzendoorn and Van Someren2012) were no longer evident in the longitudinal analyses.
Conversely, the finding that sleep hygiene was associated with later internalizing symptoms (i.e., depression and social anxiety) is consistent with the literature (Pieters et al., Reference Pieters, Burk, Van der Vorst, Dahl, Wiers and Engels2015; Rahimi et al., Reference Rahimi, Ahmadpanah, Shamsaei, Cheraghi, Sadeghi Bahmani, Holsboer-Trachsler and Brand2016; Santisteban et al., Reference Santisteban, Bouchard, Tappe, Lane, Sommerville, Boursier and Gruber2018). The current findings demonstrate significant predictions from the full range of sleep hygiene practices to both depression and social anxiety, extending previous research that focused solely on cognitive-emotional arousal at bedtime and only investigated generalized internalizing outcomes (Pieters et al., Reference Pieters, Burk, Van der Vorst, Dahl, Wiers and Engels2015; Santisteban et al., Reference Santisteban, Bouchard, Tappe, Lane, Sommerville, Boursier and Gruber2018). Interestingly, the association from sleep hygiene to depression in the current study was stronger than the association from sleep hygiene to social anxiety, indicating that while transdiagnostic, poor sleep hygiene may be a stronger risk factor for depression than social anxiety during early adolescence. This finding provides support for the role of sleep hygiene in Lovato and Gradisar’s (Reference Lovato and Gradisar2014) model of sleep disturbance and depression in adolescents, which posits that increased wakefulness in bed reinforces dysfunctional cognitions about sleep, such as repetitive, intrusive and ruminative thought patterns, further perpetuating sleep disturbance and resulting in depressive symptoms. Further, while poorer sleep hygiene predicted both depression and social anxiety, there was no evidence of the opposite associations. Thus, sleep hygiene practices specifically appear to precede internalizing symptoms and therefore may be a useful target in the formulation of prevention and intervention programs for depression and social anxiety.
Sleep hygiene as a mediator
As expected, PV had a small, positive indirect effect on depressive and social anxiety symptoms via sleep hygiene, indicating sleep hygiene mediates the relationship between PV and symptoms of both depression and social anxiety. Aligning with prior research (Chang et al., Reference Chang, Wu, Lin, Chang and Yen2019; Herkama et al., Reference Herkama, Turunen, Sandman and Salmivalli2019), these mediation findings provide further evidence for the process by which PV negatively impacts sleep which in turn increases depressive symptoms. The current study also extends the literature by demonstrating that sleep factors also mediate the associations between PV and social anxiety.
These mediation findings provide evidence for the theoretical understanding of stress-induced sleep disruption and the cascading impacts on internalizing vulnerabilities. That is, PV is an interpersonal stressor that increases vigilance and arousal (Dahl, Reference Dahl1996) and impedes adolescents’ ability to regulate their behaviors and cognitive-emotional states when preparing for sleep (i.e., sleep hygiene), which in turn undermines their ability to go to sleep at appropriate bedtimes (Galland et al., Reference Galland, Gray, Penno, Smith, Lobb and Taylor2017; Sun et al., Reference Sun, Spruyt, Chen, Jiang, Schonfeld, Adams, Tseng, Shen and Jiang2014). Notably, a number of specific physiological processes in this stress response have been suggested, including abnormal cortisol release (Chang et al., Reference Chang, Wu, Wu, Lin, Yen and Chang2017) and dysregulated brain areas associated with sleep, emotion regulation, and decision-making (Spilsbury et al., Reference Spilsbury, Korbin and Coulton2009). Consequently, these poor sleep hygiene practices increase mental and physical arousal, adversely impacting adolescents’ ability to cope with stress (Palmer et al., Reference Palmer, Oosterhoff, Bower, Kaplow and Alfano2018) and regulate their negative emotions, thus increasing the risk of social anxiety and depressive symptoms (Chang et al., Reference Chang, Wu, Lin, Chang and Yen2019; Dahl, Reference Dahl1996; Herkama et al., Reference Herkama, Turunen, Sandman and Salmivalli2019; Tu et al., Reference Tu, Spencer, El-Sheikh and Erath2019; Williamson et al., Reference Williamson, Zendarski, Lange, Quach, Molloy, Clifford and Mulraney2021).
Also consistent with our predictions, PV had an indirect effect on later sleep duration via sleep hygiene, indicating sleep hygiene also mediates the relationship between PV and sleep duration. However, there was no indirect effect in the opposite direction, suggesting that PV experiences precede reductions in sleep duration via sleep hygiene, but reduced sleep duration does not impact PV experiences despite increasing undesirable sleep hygiene practices. While previous research has demonstrated a relationship between increased PV and decreased sleep duration (e.g., Kubiszewski et al., Reference Kubiszewski, Fontaine, Potard and Gimenes2014), the current study is novel in that it provides directional evidence of this association and the possible mechanism through which it occurs. Collectively, these findings suggest that stress responses to PV lead to poorer sleep hygiene, and along with a number of environmental, social, and physiological factors (e.g., school start times, social media before bed) identified by Carskadon (Reference Carskadon2011), increase adolescent vulnerabilities to sleep disruption and decrease adolescents’ time spent asleep (i.e., sleep duration) hence creating a negative and mutually reinforcing cycle between poor sleep hygiene and decreased sleep duration.
Interestingly, the current results did not provide support for sleep duration as a mediator of the relationship between PV and depression and social anxiety. Similarly, PV did not have an indirect effect on depressive and social anxiety symptoms sequentially via sleep hygiene and sleep duration. The lack of findings relating to sleep duration may be due to the single-item measure used in the current study or it may indicate that different sleep variables differentially impact the victimization-internalizing link. To better disentangle the role of sleep duration in the link between PV and internalizing symptoms, future research could use other subjective and/or objective (e.g., sleep diary or actigraphy) measures of sleep duration as well as explore other potential sleep variables as mediators, such as sleep quality, latency, or efficiency.
Notably, the indirect effect of PV on depression via sleep hygiene was consistently larger than the indirect effect of PV on social anxiety via sleep hygiene, indicating that victimized adolescents may be at greater risk of developing depression than social anxiety when engaging in poor sleep hygiene practices. This aids in the understanding of the unique relationships that PV may have with both internalizing outcomes (see e.g., Cummings et al., Reference Cummings, Caporino and Kendall2014). Further, given sleep hygiene is made up of a number of conceptually and empirically distinct domains (e.g., behavioral versus cognitive/emotional; Storfer-Isser et al., Reference Storfer-Isser, Lebourgeois, Harsh, Tompsett and Redline2013), future research identifying which particular domains of sleep hygiene produce the strongest indirect effects from PV to each individual internalizing outcome may have important implications for the development of more targeted and efficacious prevention and intervention programs.
Finally, the current study controlled for sex differences in the initial analyses and subsequent multigroup analyses confirmed that the identified associations held true for both adolescent boys and girls. However, the lack of sex differences in the current study is not consistent with some previous research, which found a significant mediating effect of sleep problems on PV and depression for girls but not boys (Chang et al., Reference Chang, Wu, Lin, Chang and Yen2019). Chang et al. (Reference Chang, Wu, Lin, Chang and Yen2019) theorized that this was because adolescent girls generally make greater interpersonal investments, are more dependent on peers for emotional support (Rose & Rudolph, Reference Rose and Rudolph2006; Rudolph, Reference Rudolph2002) and react more strongly to traumatic events (Green et al., Reference Green, Korol, Grace, Vary, Leonard, Gleser and Smitson-cohen1991), leading to the greater experience of sleep problems (Umlauf et al., Reference Umlauf, Bolland, Bolland, Tomek and Bolland2015). However, the measure of PV used by Chang et al. (Reference Chang, Wu, Lin, Chang and Yen2019) focused primarily on relational victimization, which is generally more common in females (Denson et al., Reference Denson, O’Dean, Blake and Beames2018). Unsurprisingly, Chang et al. (Reference Chang, Wu, Lin, Chang and Yen2019) reported significantly higher levels of PV in girls than boys which may have been because the measure used did not adequately capture male PV experiences. Comparatively, the measure of PV used in the current study is widely validated and addressed five forms of PV, thus better incorporating the PV experiences of both boys and girls. Nonetheless, further research in this area is required to understand whether sex differences exist, and in which direction.
Limitations
The current study had a number of limitations. First, as convenience sampling methods were used, the sample is unlikely to be representative of the broader adolescent population. In particular, the sample was limited to Australian adolescents of medium-high socioeconomic status, with generally good sleep hygiene practices, and low levels of PV and depressive and social anxiety symptoms. Thus, the generalisability of the current study is limited and caution should be taken when applying findings to disadvantaged, non-Western, and highly victimized samples with poor sleep hygiene practices and high levels of depressive and social anxiety symptoms. Given the majority of the literature draws from Western, White samples, future research should utilize more diverse or non-Western samples.
Second, the main analyses used in the current study (i.e., CLPMs) prevented us from examining change over time within individuals (Hamaker et al., Reference Hamaker, Kuiper and Grasman2015). There is however, variation in how individuals respond to and cope with PV and internalizing symptoms (e.g., Rudolph et al., Reference Rudolph, Troop-Gordon and Granger2011). Further, several individual difference variables (e.g., resilience, self-esteem, social support) moderate and mediate the associations between PV and internalizing (Freitas et al., Reference Freitas, Coimbra, Marturano, Marques, Oliveira and Fontaine2017; Morin et al., Reference Morin, Bradshaw and Berg2015). Therefore, future research interested in intra-individual variation in the associations between PV and internalizing symptoms over time, and/or possible mechanisms underpinning this association, may choose to adopt alternative models such as the random intercept cross lagged panel model (RI-CLPM) which allows researchers to specifically assess prospective within-person effects by removing the between-person variance via latent random intercepts (Hamaker et al., Reference Hamaker, Kuiper and Grasman2015).
Finally, the current measures of PV, sleep hygiene, depressive, and social anxiety symptoms were single-informant self-report, potentially introducing common-method variance. While PV is often covert and sleep hygiene relates to subjective experiences, making self-report appropriate (Furlong et al., Reference Furlong, Sharkey, Felix, Tanigawa, Green, Jimerson, Swearer and Espelage2010), future studies could use multi-informant methods for measuring internalizing outcomes, such as teacher and parent report. Similarly, our measure of sleep duration utilized a single, self-report item, and future research may benefit from inclusion of objective measures (e.g., actigraphy).
Implications and conclusions
This study was the first to explore sleep hygiene and sleep duration as mediators of the relationship between PV and depressive and social anxiety symptoms longitudinally, adding to prior mediation research on insomnia, nightmares (Herkama et al., Reference Herkama, Turunen, Sandman and Salmivalli2019), and general sleep problems (Chang et al., Reference Chang, Wu, Lin, Chang and Yen2019). It is also the first to investigate social anxiety symptoms in this context, and one of very few addressing depressive symptoms, thus contributing to the emerging literature examining the associations between PV, sleep and internalizing symptoms.
Accordingly, the present findings have implications for early identification, prevention, and intervention in relation to PV and internalizing symptoms in adolescents. This is particularly significant given the heightened vulnerabilities that adolescents face to PV, sleep problems and internalizing symptoms. For example, parents, teachers, and clinicians can screen for poor sleep hygiene practices as both a marker of PV and a modifiable risk factor in the prevention of depression and social anxiety originating from experiences of PV. Thus, interventions can be developed to target barriers to good sleep hygiene practices, such as regulating the use of technology, avoiding the use of caffeine in the afternoon/evening, and reducing stress, worry and emotional arousal before bed (Bauducco et al., Reference Bauducco, Flink, Jansson-Fröjmark and Linton2016). Specifically, strategies could be focused on psychoeducation (e.g., Rahimi et al., Reference Rahimi, Ahmadpanah, Shamsaei, Cheraghi, Sadeghi Bahmani, Holsboer-Trachsler and Brand2016), emotion regulation, meditation and calming practices, and general stress resistance and resilience. This could assist in breaking the cycle between interpersonal stress and psychological harm in adolescents, and protect against the negative internalizing symptoms associated with victimization.
Funding statement
This paper was supported by Australian Research Council grant FL150100096 awarded to Ronald M Rapee.
Conflicts of interest
None.







