Manuscript
Objectives
Load balancing of constrained healthcare resources has become a critical aspect of assuring access to care as the United States manages pandemic related impacts. These impacts include COVID-19 patient surges, widespread staffing shortages, limitations in specialty resources such as hemodialysis, and specialty procedures (e.g., GI, cardiac, surgical).
The US healthcare infrastructure relies upon highly resourced tertiary and quaternary hospitals receiving patients from hospitals unable to provide specialty level care. Referring hospitals are often in sparsely populated rural regions, or in under resourced urban locations that are unable to provide access to time sensitive specialty medical care.
As pandemic surges have occurred across the US, access to tertiary and quaternary centers has been highly constrained and led to poor outcomes detailed in press accounts. 1 Without resources for care coordination and load balancing of the health care system, hospitals within a region may be overwhelmed while capacity exists elsewhere. Reference Dwyer2,Reference Mitchell, Rigler and Baum3 In addition, evidence has suggested that up to 1 in 4 COVID-19 deaths were potentially attributable to hospitals under severe strain from surging caseloads. Reference Kadri, Sun and Lawandi4 In response, calls for organized and equitable patient load balancing systems of care have been endorsed by the National Academy of Medicine, the Task Force for Mass Critical Care, and prominent ethicists as a means of assuring equitable access to care. In addition, the Administration for Strategic Preparedness and Response (ASPR) has encouraged the creation of Medical Operations Coordination Centers (MOCCs) as a means of accomplishing load balancing within regions. Reference Mitchell, Rigler and Baum3,5,Reference Maves, Downar and Dichter6
In the State of Washington (WA), the WA Medical Coordination Center (WMCC) has served as a statewide MOCC, serving to load balance WA hospitals since the outset of the pandemic in March 2020. The WMCC has been funded using Hospital Preparedness Program funds in collaboration with the WA State Department of Health. Since March 6, 2020, through April 21, 2022, the WMCC has managed over 3821 requests for assistance from WA hospitals in their efforts to load balance the state healthcare system and achieve equitable excess to care for patients and hospitals impacted by pandemic surges. The objective of this paper is to examine the establishment and fundamental operations of WA State’s MOCC. This system has been effectively employed to handle healthcare surges related to the pandemic. Moreover, this paper intends to provide a valuable resource for states considering the implementation of a MOCC in their respective regions.
Methods
How it was Developed
Keys to success of development include:
-
1) Broad coalition from healthcare executive leadership, academia, and government.
-
2) Commitment to load balance across all hospitals in order to avert crisis while capacity exists in the state health system.
-
3) Statewide data platform.
Harborview Medical Center in Seattle, WA serves as the Disaster Medical Coordination Center (DMCC) for western WA. In response to the first North American outbreak of COVID-19, the DMCC was activated to manage load balancing of COVID-19 patients from a single nursing home which had overwhelmed a regional hospital. Reference Morris, Resnick and England7,Reference Arentz, Yim and Klaffy8 Key leaders from the Department of Emergency Medicine at the University of WA, Harborview Medical Center, Public Health Seattle King County and the Northwest Healthcare Response Network (healthcare coalition), worked to utilize the DMCC framework of disaster coordination to extend its model to mitigate a regional surge in COVID-19 patients. The WMCC was founded on the principle that no single hospital or system should go into crisis while capacity exists elsewhere in the broader health care system.
To put this principle into practice, a coalition from within healthcare executive leadership, academia, and government, came together to create a load balancing cooperative structure. This included leadership from the WA State Hospital Association, the WA State Department of Health, hospital executive leadership, and the healthcare coalitions, namely the Northwest Healthcare Response Network and the Regional Emergency and Disaster Healthcare Coalition.
This broad coalition, along with assistance from the private sector (Microsoft), facilitated the creation of a statewide data platform for tracking resources likely to be constrained in the pandemic. This platform, termed WA Health, has since been adopted and funded by the State of WA for tracking and reporting key metrics such as patient volumes, bed capacity, staffing, and supplies. Data is updated by every hospital daily at the minimum, although numerous systems provide real-time data feeds that are refreshed every 30 to 60 minutes. This platform, along with a pre-existing manually updated bed tracking platform (WA TRAC) is fundamental to the WMCC’s load balancing work. Reference Mitchell, Bulger and Duber9
How it Works
Keys points on how it works
-
1) Hospitals first utilize existing referral patterns and relationships.
-
2) Hospitals utilize WMCC when unable to find needed bed/ specialty care.
-
3) WMCC assists with all patient types but prioritizes critical care.
-
4) Load balancing includes utilizing capacity at smaller facilities.
-
5) WMCC may utilize “guaranteed acceptance” in a geographically and acuity-based rotation.
Hospitals are first asked to utilize their normal referral patterns to facilitate required patient transfers. Unsuccessful hospitals then self-refer to the WMCC for assistance. All WA hospitals may utilize this service, but requests from outside of WA are redirected to their originating states.
Calls are received by critical care nurses who work exclusively to support the WMCC. The nurses are employed by Harborview Medical Center but are not affiliated with a health system transfer center. Each have a comprehensive understanding of statewide hospital capabilities. The nurses are backed by emergency physicians who assist with triage questions. The WMCC team then utilizes statewide data platforms, geographic and EMS considerations, as well as insights from real-time regional, and system level availability reports, to match patient needs with hospital availability. The WMCC assists with all acute medical conditions for patients of all ages, though prioritization is given to critical care patient acuity. This is distinct from other state level MOCC’s that have focused on load balancing exclusively for COVID-19 or critical care patients. Reference Villarroel, Christ and Smith10,11 While there are no exclusions for patient type, it is rare to receive requests for patients with conditions that fall within organized health systems such as stroke, ST elevation myocardial infarction, and trauma.
Importantly, in addition to the typical pattern of load balancing from critical access and rural facilities to larger tertiary centers, the WMCC works to not “over send” patients who can be cared for at smaller facilities with suitable resources for a particular need. At times, this may include patient movements from a small facility without a specific resource, yet a similar sized regional facility may be able to accommodate the patient. The WMCC has also worked to offload tertiary centers during periods of surge and has utilized rural and critical access facilities to accomplish this goal. In addition to these patient level efforts, the WMCC encourages routine regional conference calls to coordinate hospitals within a region where they discuss status and load balancing. A key component of these conversations is the offloading of tertiary centers by utilizing swing bed programs or real time capacity at smaller facilities able to accommodate patients who no longer require the specialty care of the tertiary center, yet still require hospitalization.
During the Delta surge of 2021, the WMCC faced significant challenges in carrying out load balancing activity. In response, the WMCC and the WA State Hospital Association came to an agreement to allow for guaranteed patient acceptance when standard operational means have been unsuccessful. The guaranteed acceptance applies only to those patients determined to have a life or limb threatening condition and anticipated to decline within 8 - 12 hours and is done in consultation with the on-call WMCC physician. This agreement is meant to be for short periods of extreme surge and requires increased daily reporting of patient distribution to hospital executive leadership. As of April 2022, the guaranteed acceptance requirement was utilized during a single 72- hour period and was limited to 3 patient requests during that period.
Though WA state hospitals and health systems have prioritized acceptance of WMCC patients, senior executive leadership at times have been unaware of their systems inability to accommodate WMCC requests. As such, since August of 2021, senior hospital leadership have been asked to be involved in decision making when a system believes they are unable to accommodate a request.
Results
Evidence of Effectiveness/ Lessons Learned and Future Direction
Key points on evidence of effectiveness, lessons learned and future direction
-
1) 3821 WMCC requests with 2025 patient transfers completed, 1228 independently by the WMCC.
-
2) Importance of broad coalition of all health systems; state hospital association.
-
3) Load balancing is needed for all patient types.
-
4) Centralized view of hospital waiting lists.
-
5) Improvement in state-to-state coordination.
Evidence of effectiveness
By April 21, 2022, the WMCC had received 3821 requests for assistance from hospitals in Washington State unable to transfer patients through their usual referral process. Nearly 75% of these requests originated at hospitals that are federally designated as rural facilities. Nearly 90% of these requests were received between July 2021 and May 2022 when the Delta and Omicron variants predominated and resulted in a rapid rise in hospitalizations and hospital staffing shortages.
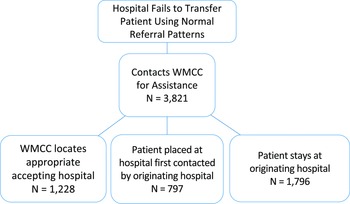
During this time, the WMCC collaborated to coordinate 2025 patient movements. Of these, the WMCC independently managed the transfer in 1228 cases. As the WMCC assists when a hospital’s initial transfer attempts fail, in 797 instances the referring hospital’s initial requests were accepted before the WMCC’s parallel work was completed. Finally, in 1796 cases, the originating hospital elected to keep the patient at their facility and later rescind the transfer request (Figure 1).

Figure 1. WMCC process and coordination summary.
There have been few occurrences where patients have been unable to be transferred – though at times the process has been extended (12 - 48 hours). Though priority is given to keeping patients close to their originating hospital, many patients were sent across state to find a suitable hospital (Figure 2). In 35% of cases, patients were identified as needing a critical care bed. While there have been a few instances where critically ill patients died before being transferred, these occurrences have been rare. Despite the WMCC providing support to patients of all age groups, there were no requests for pediatric patients during this period.

Figure 2. Heat map of originating and receiving hospital coordinations by WMCC.
The suspension of elected procedures assisted in creating hospital med capacity and occurred due to state governmental mandates in March 2020 and January 2022, along with voluntary pauses initiated by health systems in August 2021. Till date, Washington State has not implemented crisis standards of care, which has been a primary operational objective of the WMCC in collaboration with statewide partners.
One limitation of this report is that it lacks information about the specific characteristics of the patients being transferred such as the nature of their medical conditions, the length of time to place the patient and the distance traveled to the accepting hospital. This represents an important opportunity for future study.
Conclusions
Lessons Learned
A broad coalition of support has been needed to successfully implement load balancing efforts. In the spring of 2020, a broad-based commitment from key healthcare stakeholders was achieved which committed to equitable load balancing and a shared objective of avoiding crisis standards of care, if the state’s healthcare system possessed capacity. Key support included executive leadership from across all hospitals and health systems to prevent silos of data sharing and bed availability. It is believed that this was best facilitated by the State Hospital Association working closely with the regional healthcare coalition, the Northwest Healthcare Response Network. State governmental leadership from both public health and elected administrative leadership were also vital. Government leaders assisted with waivers and proclamations which endorsed load balancing efforts. In the state, the hospital association desired to avoid a broad shutdown of hospital services which occurred with the original COVID-19 surge. Their support of the WMCC was viewed by state governmental leadership as evidence of the health system’s commitment to equitable access for all Washingtonians. Though some states have utilized governmental proclamation to function, the WMCC has not required a specific governmental proclamation to conduct load balancing efforts. Reference Villarroel, Christ and Smith10
Widespread pandemic surges have resulted in pervasive capacity issues at most hospitals and a general lack of staffed beds in the state. All patient types who required acute hospital care were impacted by lack of access. Load balancing efforts, as such, needed to be focused on both COVID and non-COVID patients to assure equitable access to care for all. This includes a focus on maintaining availability of services such as trauma, stroke, and ST elevation myocardial infarction care – while conducting load balancing operations.
The downstream pandemic impacts have also resulted in a modification in approach to load balancing by the WMCC team. For instance, prior to the Delta surge of July 2021, the WMCC team performed load balancing services in addition to other hospital roles. This had been functionally possible as the number of requests per 24 hours ranged from 0 to 6. However, the impact of the Delta and Omicron variants led to a rapid increase in requests, averaging 20 - 25 per day, which mandated that a dedicated team be assembled. Since that time, the WMCC has incorporated a team of critical care nurses to function in this role. These nurses are backed up by an on-call physician’s medical direction.
The operational effectiveness of the WMCC has faced challenges during periods of significant statewide surges caused by the COVID-19 Delta and Omicron variants. However, key stakeholders have provided feedback on the advantages of the WMCC’s statewide healthcare surveillance, coordination, and load balancing efforts during these critical periods.
These benefits include gaining a more comprehensive understanding of the impact and trends of surges on specific populations, particularly those requiring additional support such as GI services (ERCP) and hemodialysis. Regional variations in surges have also been identified, leading to targeted efforts with hospitals in these regions. These efforts involve increasing awareness, improving bi-directional load balancing (where larger hospitals transfer patients to smaller hospitals to create capacity for specialty patients), and utilizing alternative solutions such as expanded staffing ratios and alternate care areas to meet the healthcare needs of specific regions.
Furthermore, as Washington State has a significant number of rural hospitals that are not affiliated with larger health systems, stakeholders from these unaffiliated hospitals have expressed the benefits of improved bed availability awareness and a coordinated system. This has resulted in improved access for their patients to larger specialty centers necessary for their care.
Future Directions
In WA state, a centralized view of hospital waiting lists is needed to avoid redundancy of efforts and delays. During periods of surge, hospitals routinely place their patients on the waiting lists of several hospitals within their catchment area. In addition, the WMCC may request a patient be placed on waiting lists, particularly for those patients who require non-time sensitive specialty care. Once a patient is accepted at 1 facility, there is no means of notifying other hospitals of the need to remove the patient from their list.
State-to-state coordination is also a future focus. The WMCC currently focuses only on requests from WA state hospitals. This has been at the request of state government leaders due to variability in state governmental responses to the pandemic, and a concern that load balancing patients from neighboring states would lead to detrimental impacts on patients from WA. However, representatives from each state within FEMA Region X have formed a task force to create a streamlined process to achieve state level patient movement between states as a key function of disaster preparedness.
Despite the unprecedented surge in hospital patient loads and the resulting staffing crisis caused by the pandemic, there have been limited published reports documenting regional load balancing initiatives. Reference Mitchell, Rigler and Baum3,Reference Villarroel, Christ and Smith10 This paper is meant to provide a brief review of the development, structure, and results of 1 state’s efforts to coordinate patient load balancing at the state level. Future research efforts are needed to identify the prevalence, design, and performance characteristics of other regional capacity coordination centers. Additionally, there is a need to establish national best practices and standards for these centers.
Author contribution
Steven Mitchell: Drafting of manuscript, editing, data collection
Mark Taylor: Editing of manuscript, data collection
Maria Paulsen: Editing of manuscript, data collection
Stephen Morris: Drafting of manuscript, editing manuscript, data collection
IRB review
The University of Washington IRB has determined that this activity is not considered research and is thus exempt from IRB review (UW IRB ID: STUDY00015481).