The number of Latino older adults in the United States is expected to surpass 14 million by the year 2050 (Vincent and Velkoff, Reference Vincent and Velkoff2010), which corresponds to a 550% increase from 2017. This demographic trend forebodes significant healthcare challenges given the high prevalence of chronic conditions such as obesity and diabetes in this population (Daviglus et al., Reference Daviglus, Talavera, Aviles-Santa, Allison, Cai, Criqui, Gellman, Giachello, Gouskova, Kaplan, Lavange, Penedo, Perreira, Pirzada, Schneiderman, Wassertheil-Smoller, Sorlie and Stamler2012). Despite the high rate of disease, Latino elders have lower mortality rates than other ethnic groups. Unfortunately, this extended longevity in combination with high prevalence of chronic conditions results in more years per capita in which disease or disability is present (Hayward et al., Reference Hayward, Hummer, Chiu, Gonzalez-Gonzalez and Wong2014).
Compounded by the aforementioned healthcare challenge, Latinos in rural communities comprise 9.3% of the total US population (Housing Assistance Council, 2012) and, relative to urban-dwelling Latinos, experience additional health inequities such as greater prevalence of hypertension and type 2 diabetes (Koopman et al., Reference Koopman, Mainous and Geesey2006; Bale, Reference Bale2010). These disparities stem from risk factors found in rural communities such as decreased health service availability and accessibility (Lutfiyya et al., Reference Lutfiyya, Bianco, Quinlan, Hall and Waring2012; Reference Lutfiyya, Mccullough, Saman, Lemieux, Hendrickson, Mcgrath, Haller and Lipsky2013), shortages of healthcare professionals (Weinhold and Gurtner, Reference Weinhold and Gurtner2014), economic disadvantages (Lutfiyya et al., Reference Lutfiyya, Mccullough, Saman, Lemieux, Hendrickson, Mcgrath, Haller and Lipsky2013; Weinhold and Gurtner, Reference Weinhold and Gurtner2014), and environmental barriers that impede physical activity (Swenson et al., Reference Swenson, Marshall, Mikulich-Gilbertson, Baxter and Morgenstern2005).
Interventions that utilize specialized strategies and adaptations have been proposed to effectively reach rural-dwelling individuals and address their unique health-related barriers. Examples of these recommendations include building local partnerships to support implementation, offering telemedicine, accommodating long-distance travel, integrating services into primary care, seeking aid from ‘natural helpers’ in the community, and broadening providers’ skillsets to make up for service shortages (Chipp et al., Reference Chipp, Johnson, Brems, Warner and Roberts2008; Lutfiyya et al., Reference Lutfiyya, Bianco, Quinlan, Hall and Waring2012; Calancie et al., Reference Calancie, Leeman, Jilcott Pitts, Khan, Fleischhacker, Evenson, Schreiner, Byker, Owens, Mcguirt, Barnidge, Dean, Johnson, Kolodinsky, Piltch, Pinard, Quinn, Whetstone and Ammerman2015). Community-based lifestyle interventions that are both designed for delivery in a rural setting and sensitive to Latino culture, though not great in number, have successfully achieved such outcomes as enhanced glycemic control and engagement in health behaviors (Goldhaber-Fiebert et al., Reference Goldhaber-Fiebert, Goldhaber-Fiebert, Tristan and Nathan2003; Sanchez et al., Reference Sanchez, Cacari Stone, Moffett, Nguyen, Muhammad, Bruna-Lewis and Urias-Chauvin2014).
Despite promising results for culturally sensitive, rural community-targeted interventions, efficacy has not been studied through the lens of patient-centered outcomes. Such outcomes were recognized as a priority in the Patient Protection and Affordable Care Act of 2010 and commonly incorporate psychosocial concerns that reflect individuals’ preferences, feelings, needs, and functional status (Rubenfeld, Reference Rubenfeld2003). Examples of patient-centered outcomes include activity participation, sleep quality, stress, and symptom management. Use of such outcomes complements conventional physiological measures (Verhoef et al., Reference Verhoef, Mulkins and Boon2005). Patient-centered outcomes not only correlate with traditional, objective outcomes such as cardiovascular risk profile (De Smedt et al., Reference De Smedt, Clays, Annemans, Doyle, Kotseva, Pajak, Prugger, Jennings, Wood and De Bacquer2013) and cognitive functioning (Scullin and Bliwise, Reference Scullin and Bliwise2015), but also provide a more complete picture of health and well-being.
In this study, the feasibility and efficacy of a culturally tailored lifestyle intervention, ¡Vivir Mi Vida! (¡VMV!; Live My Life!), intended to improve the health and well-being of high risk 50–64-year-old Latino adults, was pilot tested. This activity-centered intervention was delivered by partnered community health workers (CHWs) and occupational therapists (OTs) within the context of a primary care system. A preliminary qualitative needs assessment resulted in identification of a set of patient-valued health domains and health promotion strategies that informed ¡VMV! module construction (Schepens Niemiec et al., Reference Schepens Niemiec, Carlson, Martínez, Guzmán, Mahajan and Clark2015). ¡VMV! was then adapted by incorporating strategies for rural healthcare delivery such as a strong reliance on home-based sessions, use of telemedicine, and a focus on local resources and supports. It was hypothesized that the adapted intervention would be feasible to administer and improve both physiologic and patient-centered health-related outcomes in the target population. In addition, it was hypothesized that key stakeholders – including intervention supervisors, CHWs, assessors, and the partnering community wellness organization administrator – would be satisfied with the program and view it as practical to implement in their community.
Method
Design
Study procedures were approved by the University of Southern California (USC) Institutional Review Board. The design entailed a one-arm, feasibility and pre-post pilot efficacy study of the rural-adapted program in the Antelope Valley of California during 2016. Antelope Valley is located in northern Los Angeles County and comprises the western tip of the Mojave Desert.
Participants & setting
A total of 40 eligible participants were recruited between February and March 2016 through randomized selection of referred patients listed as potentially eligible by the partnering health clinic (Antelope Valley Community Clinic [AVCC]), as well as through community information booths, word-of-mouth, and flyers. Inclusion criteria limited enrollment to individuals who were 50–64-years-old, Latino, fluent in Spanish (to facilitate group session interactions), available by phone, and oriented to person, place, and time. In addition, participants were required to have visited AVCC during the past year, with self-reported capacity to complete a 16-week intervention and no plans to move outside of Antelope Valley within six months. The decision to target late middle-aged adults was based on: (a) recent theory, which emphasizes healthy aging as a continuous process throughout the lifespan (Hansen-Kyle, Reference Hansen-Kyle2005); (b) the desirability of instilling sound health habits during a temporal window that precedes major health declines experienced in older age (Sudano and Baker, Reference Sudano and Baker2006); and (c) indications that Latino adults in this age group are willing to undertake health-promoting lifestyle changes (Osuna et al., Reference Osuna, Barrera, Strycker, Toobert, Glasgow, Geno, Almeida, Perdomo, King and Doty2011; Schepens Niemiec et al., Reference Schepens Niemiec, Carlson, Martínez, Guzmán, Mahajan and Clark2015).
Procedure
Greater detail of all study procedures can be found in (Schepens Niemiec et al., In Press). With support from AVCC, this community-based participatory research was conducted in partnership with Antelope Valley Partners for Health (AVPH), a community wellness organization located in Antelope Valley. AVPH supplied two CHW interveners who were Spanish-English bilingual. The USC research team provided two bilingual intervener supervisors: a treating OT and senior promotor (ie, a CHW who has deep ties to the Latino community, specialized cultural knowledge, and shared lived experiences; Latino Health Access et al., 2011). The USC team led 12- and 40-h training workshops for the assessors and intervening CHWs, respectively.
Participants were screened for eligibility primarily by telephone and subsequently consented and enrolled in person. Using schedule availability, individuals were allocated to one of four intervention groups (n=10 per group; two groups per CHW). Assessments took place at baseline (pretest) and post-intervention (posttest).
Data collection & instruments
Table 1 summarizes the tools/indices and study variables used to evaluate intervention efficacy. Assessors collected data at each time point (unless otherwise noted) typically at participants’ homes. All pre-existing assessments had been validated for Latino populations and were available in Spanish. The primary patient-centered outcomes consisted of sub-scores on the Measure Yourself Medical Outcome Profile 2 (MYMOP2; Paterson, Reference Paterson1996). MYMOP2 is a patient-centric questionnaire that requires respondents to identify one or two current and personally bothersome symptoms. Participants rate symptom severity, as well as how much each symptom interferes with daily activities and well-being. The MYMOP2 produces an overall profile score as well as sub-scores of symptom severity, general well-being, and impact of symptoms on daily activity. Secondary outcomes ranged from lifestyle factors (eg, physical activity engagement) to cardiometabolic measures (eg, cholesterol level). Comorbidity information was collected via self-report and from AVCC electronic medical records. Assessors entered self-reported data obtained orally and cardiometabolic measurements into Research Electronic Data Capture (REDCap) – a web-based application to support data collection (Harris et al., Reference Harris, Taylor, Thielke, Payne, Gonzalez and Conde2009).
Table 1 Overview of study variables and data collection tools/procedures used to evaluate intervention efficacy
a Measurement tool is self-explanatory.
b Assessed only at baseline.
c Assessed only at posttest.
d Calculated from other collected variables.
Intervention
As described in Schepens Niemiec et al. (In Press), ¡VMV! integrated theoretical constructs from (a) OT Lifestyle Redesign® – holistic wellness, habits and routines, and participation in culturally defined activities (Carlson et al., Reference Carlson, Clark and Young1998; Clark et al., Reference Clark, Blanchard, Sleight, Cogan, Floríndez, Gleason, Heymann, Hill, Holden, Murphy, Proffitt, Schepens Niemiec and Vigen2015); and (b) social cognitive theory – self-efficacy, self-regulation, social support, and outcome expectations (Bandura, Reference Bandura1986; Reference Bandura2004). Intervention delivery was also underpinned by behavior change techniques such as goal-setting, building social support, acknowledging past successes, and educating individuals about the consequences of behavior (Michie et al., Reference Michie, Ashford, Sniehotta, Dombrowski, Bishop and French2011).
¡VMV! utilized CHWs as frontline interveners who were supervised by a senior promotor-OT team. The supervising promotor educated the CHWs about community health outreach, provided community resources and supports for participants, and assisted the CHWs in delivering content in a culturally sensitive and understandable manner. The OT held a dual role as a supervisor and clinical interventionist. As a supervisor, the OT facilitated the CHWs’ use of health behavior change techniques and guided the CHWs in grading and adapting participants’ activities to support long-term goal attainment. As part of the OT’s clinical role, she reviewed health information from the electronic medical record, concatenating it with treatment; monitored participants’ activity participation, and discussed with individuals integration of healthful routines. Digital communication was established between the CHW-OT team and participants’ primary care physicians to report health-related updates. The senior promotor and OT held weekly supervisory sessions with the CHWs to discuss participant cases, implementation challenges, and forthcoming sessions.
The first intervention session included a home visit with a CHW, combined with a telemedicine OT consultation. During this session, the participant created a personalized health action plan (HAP), which was revisited at subsequent sessions. CHWs led weekly visits (including seven one-on-one home sessions, two group sessions held at local community facilities, and two telephone check-ins) over 16 weeks. In addition, the OT provided two 20-min telephone consultations to discuss individually experienced wellness facilitators, as well as troubleshoot barriers to health-related goals.
CHWs were provided with a structured manual, supplemented with a picture-based flip-over booklet and demonstration tools. Participants were given health-related materials and tools throughout the program such as a Garmin Vivofit activity monitor and a measuring cup. Overarching modular topics included healthy eating and physical activity, healthcare navigation, chronic disease management, and mental well-being.
Data analysis
All analyses were organized using a rubric that addresses pilot interventions’ feasibility based on scientific merit (efficacy results) and study processes, resources, and management (Thabane et al., Reference Thabane, Ma, Chu, Cheng, Ismaila, Rios, Robson, Thabane, Giangregorio and Goldsmith2010). Given 10% attrition, use of a two-tailed test with α=0.05, and an effect size of 0.454, a sample size of 40 was required to achieve 80% power for detecting change on a continuous outcome variable. Similar interventions (Parikh et al., Reference Parikh, Simon, Fei, Looker, Goytia and Horowitz2010; Koniak-Griffin et al., Reference Koniak-Griffin, Brecht, Takayanagi, Villegas, Melendrez and Balcazar2015) suggested an effect size of 0.454 would be appropriate for examining efficacy. Wilcoxon signed rank tests were used to compare pre- and post-intervention scores on primary and secondary outcomes. Statistical analyses were performed using SAS 9.4 for windows (SAS, Cary, NC, USA).
Feasibility evaluation & analysis
Feasibility was assessed using a mixed-methods process evaluation that considered viewpoints of participants, stakeholders, and the study team. Immediately after the posttest, assessors queried each participant about program feasibility and acceptability using a semi-structured interview guide and Likert-style survey. In addition, all participants were invited to attend one of two focus groups – led by experienced qualitative researchers who were unrelated to the study – to further discuss their intervention experiences. A research assistant took detailed field notes during these groups. Slightly less than one-half of the participants attended the groups (n=7 and n=8), which resulted in sizes optimal for group interaction (Patton, Reference Patton2001). In addition, stakeholders (ie, intervention supervisors, CHWs, assessors, and AVPH administrator) were queried using semi-structured interviews. All interviews and focus groups were audio-recorded.
Fidelity of intervention delivery by the CHWs was assessed by the supervising OT using a study-specific index that listed theoretically postulated core content and processes comprising ¡VMV! (Schepens Niemiec et al., In Press for details). Intervention elements such as culturally sensitive delivery of materials or attention to a participant’s personal support system were rated as ‘completed,’ ‘not completed,’ ‘unsure,’ or ‘not applicable.’ The OT applied the fidelity index during two individual and two group sessions per CHW, as well as during two audio-recorded individual sessions (randomly selected, but contingent upon participant permission). Finally, feasibility was assessed through recruitment logs, daily correspondences, attendance reports, and adverse event logs.
Focus group and interview audio recordings were transcribed, and translated to English as necessary. Using Dedoose (Version 7.5.9) web application for qualitative data (SocioCultural Research Consultants, 2017), a surface-level content analysis (Berg, Reference Berg2001) was conducted to identify themes specific to feasibility. This type of analysis permits classification of qualitative information using a predetermined coding scheme. Two research team members generated codes independently, which were later checked by a third member and stored in a master codebook. Analysts documented decision pathways for purposes of maintaining an audit trail of analytic memos. Quantitative data resulting from participant interviews and supplemental sources (eg, attendance logs) were summarized via descriptive statistics. Because the present study did not involve comprehensive qualitative procedures, alternative in-depth analyses methods were not warranted. Thabane and colleagues’ (2010) recommended organizational structure and rubric for evaluating pilot studies served as overarching themes under which both quantitative and qualitative information was filed. Doing so enabled efficient integration of mixed-methods data that are easily compared across studies that have used a similar thematic scaffold.
Results
Study sample
Table 2 describes characteristics of participants who completed post-testing (n=37). Age ranged from 50.7 to 64.9 years. Most participants were female (n=34, 91%), born outside of the United States (n=36, 97%), non-smoking (n=28, 76%), and/or unemployed (n=28, 76%). The mean body mass index (32.1±6.5) fell within the range of Class I obesity (Nuttall, Reference Nuttall2015). All participants reported an income of less than US$24 000/year. Information on comorbidities was collected from complete electronic medical record data (n=27) and self-report questionnaires (n=33). Of participants with electronic medical record data, more than half were diagnosed with pain (n=21, 78%), dyslipidemia (n=18, 67%), diabetes (n=15, 56%), and gastrointestinal/liver disease (n=14, 52%). Charlson comorbidity indices for those with electronic medical record data ranged from 0 (44%) to 4 (4%), with a mean score of 1.1±1.2. Common self-reported conditions included dyslipidemia (n=18, 55%), arthritis (n=14, 42% versus 11% in electronic medical records), diabetes (n=13, 39%), depression (n=12, 36% versus 19% in electronic medical records), and hypertension (n=12, 36% versus 18% in electronic medical records).
Table 2 Characteristics of pilot study participants at pretest (n=37) who completed post-testing
Scientific feasibility
No intervention-related adverse events occurred. Patient-centered outcomes improved significantly (P⩽0.01) from pretest to posttest (Table 3) for the overall MYMOP2 profile score and subscales (ie, symptom severity, symptom impact on activity, and well-being), with all effect sizes medium-to-large (0.50–1.06). Results for secondary outcomes are presented in Table 4. Participants improved significantly for the patient-centered outcomes of stress, satisfaction with social roles, and satisfaction with social activity (effect sizes=0.39–0.45). Relative to clinical health, participants’ systolic blood pressure improved (P=0.006). Other outcomes such as weight, HbA1c, cholesterol level, and diabetes and cardiovascular disease risk did not change. Regarding lifestyle behaviors, intake of sodium and saturated fat decreased significantly (P⩽0.0001) and sugar consumption showed a marginally significant reduction (P=0.07), but no significant changes were noted for physical activity engagement. Reductions in systolic blood pressure were associated with reduced intake of sodium (r=0.43, P=0.01) and saturated fat (r=0.43, P=0.01); data not shown.
Table 3 Measure yourself medical outcome profile (MYMOP2) scores from pretest to posttest

A decrease in scores is considered improvement.
a Wilcoxon signed rank test.
Table 4 Changes in secondary outcomes from pretest to posttest
HDL=high density lipoprotein; MET=metabolic equivalent; n=36–37, unless otherwise indicated.
a Wilcoxon signed rank test with significant values bolded.
b Of participants diagnosed as diabetic (n=18), HbA1c was available for 11 participants at pretest, 18 at posttest and 11 for both time-points.
c Cholesterol values were available for 15 participants at pretest, 28 at posttest, and 14 for both time-points.
d Coronary heart disease risk scores are the 10-year congenital heart disease risk; values were available for 15 participants at pretest, 28 at posttest, and 14 for both time-points.
e Diabetes risk scores of 534–585 and 586–657 are associated with 3.0–4.9% and 5.0–9.9% incidence of diabetes within five years, respectively; values are calculated only for non-diabetics and were available for 16 participants at pretest, 17 at posttest, and 16 for both time-points.
Process feasibility
Recruitment, retention, & adherence
Recruitment and retention data are presented in Figure 1. A total of 74 potentially eligible individuals were screened: 14 failed to meet inclusion criteria, eight declined participation, and 12 were excluded for other reasons such as unresponsiveness to repeated telephone messages. In all, 37 participants (93%) completed post-testing. Participant adherence was defined as percent completion of all possible intervener contacts (n=15) – including individual, group, telephone, and OT sessions – within the 16-week program. We operationalized ‘successful’ adherence as ⩾75% completion of all contact opportunities based on a similar study (de Heer et al., Reference de Heer, Balcazar, Wise, Redelfs, Rosenthal and Duarte2015). Adherence averaged 77% for all session types, 88% for individual sessions, 61% for group sessions, and 76% for telephone check-ins. Participants received an average of two of the three intended OT consultations.
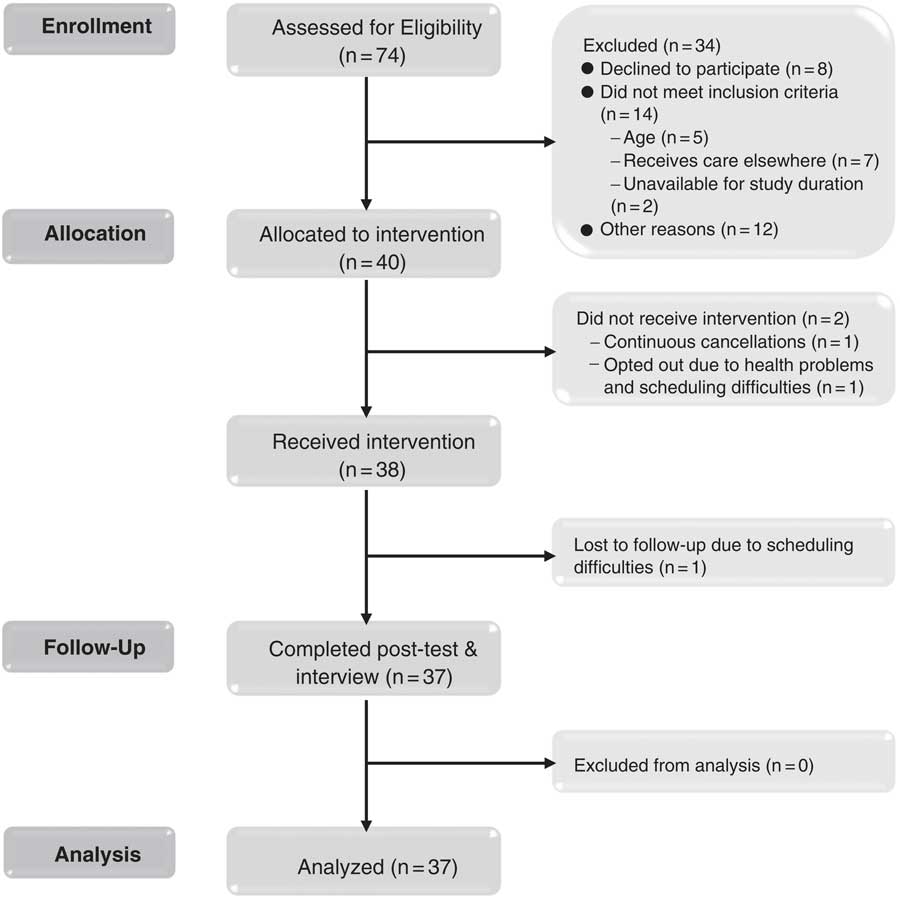
Figure 1 Recruitment and retention of participants
Fidelity
With ⩾80% integrity constituting ‘high’ and ⩽50% representing ‘low,’ session fidelity (Perepletchikova and Kazdin, Reference Perepletchikova and Kazdin2005) the CHWs delivered the majority of ¡VMV! with high fidelity (when items were applicable). Nine of the 12 fidelity items the OT reviewed were rated as performed properly ⩾85% of the time. The OT noted that the CHWs engaged in participant-skill building only 71% of the time. One area in need of improvement was the CHWs’ confidence and ability to deliver the intervention fluently in Spanish (Spanish was their second language); the OT rated this as occurring only 20% of the time. In addition, the CHWs did not utilize motivational interviewing techniques in any of the reviewed sessions.
Implementation alterations
Over the course of the study, the team made three major alterations to ¡VMV!. First, although the intervention was originally designed to be delivered by promotores, the limited supply of qualified personnel in the targeted rural area made it necessary to broaden intervener eligibility more generally to Spanish-speaking CHWs. To prevent this change from compromising the program’s cultural sensitivity, our promotor devoted more attention during supervisory sessions to guiding the CHWs in delivering ¡VMV! in a culturally competent manner. The second alteration occurred shortly after the onset of implementation and consisted of allowing participants to schedule make-up sessions outside of the intended sequence of intervention modules or to attend alternate group sessions when experiencing scheduling conflicts. Finally, the intervention manual was originally in English. Based on feedback from the CHWs during their training, we generated a certified translation of the manual so that the CHWs could more easily conduct sessions in Spanish. Other, more minor modifications are noted below in the discussions of implementation barriers and resource and management feasibility.
Implementation facilitators & barriers
The following implementation facilitators were noted by CHWs: (a) adjusting supervisory meetings to provide more review of content for upcoming sessions; (b) having the supervising OT available to discuss health-related issues that fell outside of the CHWs’ scope of practice; and (c) conducting individual sessions in participants’ homes. Participants strongly endorsed the last item, stating that in-home sessions reduced the need to travel, making it easier for them to engage in program activities. Though some participants viewed in-home sessions as affording privacy that fostered trust, confidence, and more intimate interactions, others equally valued group sessions as an opportunity to receive peer support. Participants also shared that simply knowing that someone cared about them provided them with needed encouragement to carry out health behaviors. Finally, participants described that CHWs’ demonstrations and activities (eg, measuring food portions, reading nutritional labels) were very helpful.
Implementation barriers largely revolved around resource limitations (see Resource Feasibility); however, process-related issues were also noted. The CHWs felt that the required computerized session documentation was too challenging, including the volume of data they were obligated to record and the process of uploading image captures of handwritten forms. To lessen this burden, the documentation process was streamlined mid-intervention. The CHWs also expressed feelings of being overloaded due to issues such as scheduling difficulties, partly stemming from packed caseloads, and having to spend time on evenings and weekends to offset laggard notes. In addition, they articulated uneasiness in covering topics outside of their comfort zones such as money management or grief; topics that are commonly addressed by OTs but not by CHWs. Finally, participants reported some process-related implementation barriers: (a) difficulty attending groups due to transportation challenges; (b) limited time to delve into intervention topics because the program was short; and (c) trouble activating and using the Garmin Vivofit activity monitors given to them in week 4, due to not having a computer or smartphone.
Satisfaction, acceptability, & adoption
On a 0–10 scale, participant satisfaction with the overall ¡VMV! experience was high (M=9.4±1.8); 81% of respondents rated the program as 10. When asked about the acceptability of different intervention components, participants responded almost exclusively with highly positive feedback (Table 5). One participant stated, ‘They explain everything very meticulously and you learn, like the program is named, how to live your life individually and how to start trusting in yourself, in people, and […] live day by day.’ They expressed intense appreciation for ¡VMV!, with many describing the provision of the program as a ‘gift from God’ to the community. One individual suggested making ¡VMV! the focal point of a community health program: ‘I would like for there to be an institution that has programs like this, but in the center it would be ¡Vivir Mi Vida!.’ Participants’ willingness to adopt healthier lifestyles on a more long-term basis was also promising. One participant noted, ‘I can utilize what I learned here for the rest of my life, because you stay with it for the rest of your life.’
Table 5 Descriptive statistics for participant satisfaction survey post-intervention (n=37)
Though not to the same degree as participants, the stakeholders also disclosed high satisfaction with ¡VMV!. For example, the CHWs felt that ¡VMV! offered social and emotional support that was much needed in the rural population. The AVPH administrator said that her organization was eager to adopt health programs for older people, including ¡VMV!, because seniors in Antelope Valley are in dire need of support for their well-being.
Resource feasibility
The feasibility of ¡VMV! was chiefly dictated by the level of available resources (ie, time, space, equipment/materials, budget, and personnel). Accordingly, stakeholders’ and participants’ views about implementation barriers often focused on resource limitations. The CHWs expressed that the time needed to travel between participants’ homes was burdensome due to Antelope Valley’s vastness. Stakeholders all stated a desire for more time – for session and program length – to cover a greater range and depth of content; participants echoed this request. The promotor and OT supervisors pointed out that supervisory meetings, designed to assist CHWs in intervention delivery, were oftentimes cut short or canceled due to priority being placed on the CHWs’ completion of participant sessions and documentation. The OT noted that this lack of time to communicate with the CHWs hindered her ability to provide an adequate level of informed support and intervention individualization.
With regard to space, the CHWs raised no concerns about securing a central location for group sessions. However, some participants indicated that having closer venues for group meetings would have been preferable due to the lengthy travel requirements for those living in outlying communities and/or relying on public transportation. The stakeholders and project management team alike expressed frustrations with equipment, including technological complexity of the physical activity monitors that were given to participants; videoconferencing using study laptops, which was often impeded by unreliable Wi-Fi signals, thus requiring communication via phone; and necessity to share certain equipment and materials among multiple personnel.
Budgetary and personnel resources were closely linked. Limited funding hampered implementation feasibility by posing personnel challenges in meeting the deadline for intervention completion, which resulted in the CHWs having heavy caseloads. Accordingly, during implementation, we discovered the need for a third CHW intervener to ensure the full dosage of intervention delivery. Having a third intervener proved necessary after one of the CHWs required a short leave of absence, and when participant schedules did not align with the availability of the two primary interveners. Given budgetary constraints and shortages of Spanish-speaking personnel at AVPH, we allowed the supervising promotor to serve as a back-up intervener. Nevertheless, the AVPH administrator discussed difficulties with not having additional AVPH staff cross-trained as a back-up for the CHWs, which limited program flexibility.
Management feasibility
Managing the overall project and intervention from a distance without an onsite project coordinator was particularly challenging. For example, communication with community partners occurred primarily through long email chains and phone texts, sent from multiple study team members. AVPH stakeholders voiced frustration with this system, stating that the messages they received were overwhelming in number and were occasionally overlapping or contradictory. In response, communication was streamlined by splitting up responsibilities among our study team and limiting the number of sent messages. Bi-weekly phone check-ins with the AVPH administrator were also arranged to ensure the project was running smoothly for both AVPH and USC personnel. Importantly, the AVPH administrator brokered contact between the study team and administration at AVCC. The pre-established relationships with community partners greatly enhanced the ease of completing mandatory processes such as obtaining institutional agreements and human subject authorizations.
Discussion
The study findings uphold the viability of implementing a CHW/OT-led lifestyle intervention for rural-dwelling, late midlife Latinos. In support of the intervention’s scientific feasibility related to efficacy, a number of positive changes – typically reflecting large effect sizes – in psychosocial patient-centered outcomes were found including symptom severity, perceived impact of symptoms on daily activity, general well-being, satisfaction with social roles, satisfaction with social activities, and stress. Although there is some evidence demonstrating similar positive effects of lifestyle interventions led either by OTs or CHWs (Clark et al., Reference Clark, Azen, Zemke, Jackson, Carlson, Mandel, Hay, Josephson, Cherry, Hessel, Palmer and Lipson1997; Reference Clark, Jackson, Carlson, Chou, Cherry, Jordan-Marsh, Knight, Mandel, Blanchard, Granger, Wilcox, Lai, White, Hay, Lam, Marterella and Azen2012; Viswanathan et al., Reference Viswanathan, Kraschnewski, Nishikawa, Morgan, Honeycutt, Thieda, Lohr and Jonas2010), these results support adoption of a hybrid CHW-OT intervention approach.
Intervention recipients’ systolic blood pressure declined significantly, an outcome not routinely produced from Latino-tailored lifestyle interventions (Rosal et al., Reference Rosal, Ockene, Restrepo, White, Borg, Olendzki, Scavron, Candib, Welch and Reed2011; O’Brien et al., Reference O’Brien, Perez, Alos, Whitaker, Ciolino, Mohr and Ackermann2015). Because systolic hypertension increases with age, maintaining its level within healthy ranges becomes increasingly important for cardiovascular disease prevention in persons 50 years and older (Chobanian et al., Reference Chobanian, Bakris, Black, Cushman, Green, Izzo, Jones, Materson, Oparil, Wright and Roccella2003). Notably, the magnitude of systolic blood pressure reduction recorded in the present study was also clinically meaningful, as similar improvements have been associated with reduced risk of cardiac disease or mortality in medication-based trials (Chobanian et al., Reference Chobanian, Bakris, Black, Cushman, Green, Izzo, Jones, Materson, Oparil, Wright and Roccella2003). Though in a future trial plans will be made to test the precise mechanisms by which the intervention may have reduced blood pressure, it is postulated that participants’ reduced intake of sodium, saturated fat, and sugar played an important role (Hall, Reference Hall2009; Chen et al., Reference Chen, Caballero, Mitchell, Loria, Lin, Champagne, Elmer, Ard, Batch, Anderson and Appel2010; He et al., Reference He, Li and Macgregor2013). Moreover, intervention elements focusing on mental health, stress reduction, self-efficacy, and social support may have enhanced this effect, a possibility consistent with previous reports on the cardiovascular benefits of psychosocial interventions (Linden et al., Reference Linden, Stossel and Maurice1996; Rainforth et al., Reference Rainforth, Schneider, Nidich, Gaylord-King, Salerno and Anderson2007). Together, evidence points to the need to further explore lifestyle interventions that reach beyond a focus on diet and exercise and extend to psychosocial factors that may positively influence both physiological and mental well-being.
Other physiological parameters did not improve, and coronary heart and diabetes disease risk remained the same. These results are consistent with other CHW-led programs that have shown modest effects at best on cardiometabolic indicators (Rosal et al., Reference Rosal, Ockene, Restrepo, White, Borg, Olendzki, Scavron, Candib, Welch and Reed2011; De Heer et al., Reference de Heer, Balcazar, Wise, Redelfs, Rosenthal and Duarte2015). One explanation for these findings is that the 16-week intervention did not uniquely target any single disease or delve deeply into physical activity or diet, which is uncharacteristic of traditional lifestyle interventions. However, the intervention was designed to promote holistic wellness as recommended for rural healthcare efforts, in which multiple, targeted services are less practical or feasible (Chipp et al., Reference Chipp, Johnson, Brems, Warner and Roberts2008). In this regard, cardiometabolic parameters associated with certain diseases (eg, HbA1c levels) or specific health behaviors may be difficult to alter through a generalized intervention. Further investigation is warranted to determine the impact that adaptations made to improve the practicality of lifestyle interventions for implementation in a rural primary care context have on the intervention’s potential to produce desired health outcomes.
One aspect of ¡VMV! that proved unfeasible was use of the Vivofit activity monitor. The CHWs described the tracker as ‘too high-tech’ for the target population, resulting in only one participant utilizing it. In other CHW-led programs, incorporating strategies such as providing low-tech pedometers with a goal of 10 000 daily steps (Koniak-Griffin et al., Reference Koniak-Griffin, Brecht, Takayanagi, Villegas, Melendrez and Balcazar2015) or linking participants to community-based physical activity resources such as walking groups (De Heer et al., Reference de Heer, Balcazar, Wise, Redelfs, Rosenthal and Duarte2015) resulted in significantly increased physical activity. In planning the next iteration of ¡VMV!, our team will more appropriately tailor physical activity strategies to the target population.
Another possible reason for the lack of effect for cardiometabolic indicators is that the four-month program length was too short to affect changes in these parameters. For instance, in one prior study, significant changes in HbA1c levels were not observed until completion of a six-month, promotor-delivered, diabetes-focused program (Lujan et al., Reference Lujan, Ostwald and Ortiz2007). In a further study, Ockene et al. (Reference Ockene, Tellez, Rosal, Reed, Mordes, Merriam, Olendzki, Handelman, Nicolosi and Ma2012) reported improvements in weight and HbA1c following a lifestyle intervention for Latinos, although their program lasted a full year. Our preliminary findings justify consideration of an extended intervention and assessment period in a future clinical trial.
The process feasibility of ¡VMV! is promising. The desired number of intervention participants were efficiently recruited in a one-month time period with assistance from the primary care partners. Moreover, the study demonstrated 77% participant adherence to the program and 93% retention of individuals to the time of post-testing. These numbers are successful, given anecdotal reports of 50% no-show rates for general community programs at AVPH. ¡VMV! was delivered with high fidelity, though in future efforts the training workshop and CHW supervision meetings will be bolstered to address areas of concern. For instance, the CHW’s underutilization of motivational interviewing may be remedied by expanding the training component that is dedicated to introducing and utilizing the techniques. Nonetheless, the systematic assessment of intervention delivery fidelity featured in this pilot study reveals that the CHWs have full capacity to deliver the core components of a complex OT-CHW intervention with high fidelity.
Participants were extremely satisfied with ¡VMV!. Key stakeholders also found the program to be acceptable and worthy of adopting, but pointed out aspects that could be improved. For example, the OT and the AVPH administrator requested that in future efforts attempts be made to more fully integrate ¡VMV! into the ongoing services offered through patients’ primary care institutions (eg, establishing clear expectations for collaboration and reciprocal communication between the primary care and CHW-OT teams regarding treatment and outcomes). Interveners and participants alike experienced difficulties with Wi-Fi during the intervention. Because the Wi-Fi landscape continuously changes, verifying coverage before study initiation will be useful in future applications, and ‘offline’ solutions, such as using carbon copy paper to capture treatment notes instead of requiring CHWs to upload digital copies, need to be implemented when indicated.
Among all levels of the process evaluation, the team’s ability to improvise emerged as a common theme that facilitated implementation. Whether addressing adherence by allowing participants to make up missed treatment sessions or streamlining treatment documentation so that CHWs could complete their notes with less difficulty, the ability to undertake in-stream adaptations proved critical. In cases where the team was less adaptable, process feasibility suffered. As an example, because having prearranged groups for each CHW before initiating the intervention was adhered to, the time between pretesting and the first treatment session was unusually long (M=22 days). Indeed, the success of community-based participatory research hinges on the flexibility with which teams approach and execute process elements (Cook, Reference Cook2008).
The assessment of the resource feasibility and management feasibility of ¡VMV! revealed the need for slight reconfiguration of time and personnel. Travel time frequently presents an obstacle for rurally situated home health service providers and patients (Buzza et al., Reference Buzza, Ono, Turvey, Wittrock, Noble, Reddy, Kaboli and Reisinger2011), as was the case in this study. During planning stages, the amount of time required for CHWs to travel among participants’ homes was underestimated, resulting in a failure to anticipate how this would impact scheduling and caseloads. Future efforts will require strategizing with community partners to identify practical solutions to resource and management shortcomings, discussing strategies such as reducing intervener caseloads, increasing the number of telehealth sessions, and hiring an onsite project coordinator.
Strengths & limitations
This study had multiple strengths. The intervention features a pioneering collaboration between OTs and CHWs within primary care. Though each field of practice is independently emerging as a contributor to this healthcare context (Brownstein et al., Reference Brownstein, Hirsch, Rosenthal and Rush2011; Donnelly et al., Reference Donnelly, Brenchley, Crawford and Letts2013), their co-involvement as a partnered team brings an important, reciprocal skillset to the intervention equation that has not yet been studied. In addition, ¡VMV! is qualitatively distinct from other lifestyle interventions for rural-living Latinos (Brown et al., Reference Brown, Garcia, Kouzekanani and Hanis2002; Walker et al., Reference Walker, Pullen, Boeckner, Hageman, Hertzog, Oberdorfer and Rutledge2009; Fahs et al., Reference Fahs, Pribulick, Williams, James, Rovnyak and Seibold-Simpson2013; Hu et al., Reference Hu, Wallace, Mccoy and Amirehsani2014; Lilly et al., Reference Lilly, Bryant, Leary, Vu, Hill-Briggs, Samuel-Hodge, Mcmilin and Keyserling2014). It is based on a holistic approach to healthy lifestyle, thereby moving beyond the traditional focus on dietary intake and exercise to encompass pressing daily concerns such as social relationships, mental health, sleep, and stress management. Finally, including patients and all ranks of stakeholders in the development and implementation process of ¡VMV! (Schepens Niemiec et al., Reference Schepens Niemiec, Carlson, Martínez, Guzmán, Mahajan and Clark2015) provides a more realistic view of program roll-out in a real-life context.
Despite its strengths, the study also had several limitations. The pretest-posttest design did not include a control group, which leaves study results, particularly for the MYMOP2, susceptible to regression to the mean or other threats to causal inference. Long-term follow-up assessment was not included; however, the team is currently preparing a 12-month follow-up study of the same intervention participants. A small sample was drawn from one primary care facility. A future study will feature a multi-site trial with more participants to improve generalizability. Group session attendance was low in comparison to individualized sessions. A wider variety of locations and time slots for group sessions will be available to participants in a future trial to improve adherence. Use of deductive methods for content analysis of feasibility data – using predetermined thematic categories – limited the richness of data extracted from the interviews. More in-depth interviews with detailed qualitative analysis is warranted. Finally, change in self-reported health outcomes may have been over- or underestimated, owing to recall and social desirability biases.
Conclusion
The ¡VMV! lifestyle intervention is feasible to implement and shows potential to improve a variety of health and wellness outcomes in late middle-aged Latino patients from a rural community. This study is significant because it serves as a springboard to change clinical practice in primary care. Unlike other interventions, ¡VMV! combined the specialties of CHWs and OTs to encourage a hard-to-reach patient population to incorporate general healthy lifestyle changes into their daily routines. Although a number of challenges arose which can potentially be minimized through programmatic tweaks, this study demonstrated one way in which CHWs and OTs can effectively collaborate to address the health needs of underserved populations within rural primary care. Given the promise that ¡VMV! shows, and the health risks that present in rural-living Latinos, a future randomized controlled trial is warranted to further investigate the efficacy of this lifestyle intervention.
Acknowledgments
The authors would like to thank the participants and also Antelope Valley Partners for Health, Antelope Valley Community Clinic, and Southern California Clinical and Translational Science Institute for their support of this project.
Financial Support
This work was supported by the National Institutes of Health – National Center for Medical and Rehabilitation Research and National Institute for Neurological Disorders & Stroke (Schepens Niemiec, grant # K12 HD055929); and an internal award through the University of Southern California OS/OT Initiatives Program (Schepens Niemiec).
Conflicts of Interest
None.
Ethical Standards
The authors assert that all procedures contributing to this work comply with the ethical standards of the University of Southern California Institutional Review Board and with the Helsinki Declaration of 1975, as revised in 2008.









