Our recent study estimating the incidence of first-episode psychosis using population-based health administrative data (Anderson et al., Reference Anderson, Norman, MacDougall, Edwards, Palaniyappan, Lau and Kurdyak2018), and the subsequent response from Hogerzeil and van Hemert (Reference Hogerzeil and van Hemert2019), has opened the door for a productive discussion of the importance of contextualizing incidence estimates. In our original paper, we present findings which suggest that estimates derived from specialized psychiatric services may underestimate population-based estimates of psychotic disorders. The response from authors Hogerzeil and van Hemert make use of these findings, as well as their own prior work in this area, to propose a framework that more clearly delineates the relationship between study design elements and incidence estimates. The authors use a three-dimensional figure to describe these relationships, assigning each axis a domain of study design: accuracy of diagnosis, coverage of services and time frame of diagnosis. Changes to these design parameters will influence the volume of the cube, and correspondingly the size of the incidence estimate. We agree with Hogerzeil and van Hemert that this is a crucial consideration for measuring and interpreting incidence estimates, which has indeed been largely overlooked in the literature to date. Building on this model, we propose the use of standardized nomenclature which can further enhance our understanding and interpretation of incidence estimates and their relationship with a theoretical true population incidence (Anderson, Reference Anderson2013).
Framing incidence estimates
Incidence estimates are an integral component of etiological research, as they are used to inform our understanding of the risk of various exposures. In the case of psychotic disorders, they are also crucial for ensuring early intervention services are adequately resourced (Kirkbride et al., Reference Kirkbride, Jackson, Perez, Fowler, Winton, Coid, Murray and Jones2013). As such, accurate and well-defined incidence estimates have important social, scientific and public health implications (Anderson, Reference Anderson2019). To date, investigators have independently contextualized incidence estimates using a variety of categorizations and terminology (e.g. Anderson, Reference Anderson2013; Hogerzeil and Susser, Reference Hogerzeil and Susser2017; Jongsma et al., Reference Jongsma, Turner, Kirkbride and Jones2019). Standardizing our nomenclature around the surveillance of psychotic disorders is important for accurate comparison of estimates across geographic locations and over time (Anderson, Reference Anderson2019).
In our view, the framework proposed by Hogerzeil and van Hemert (Fig. 1), as well as the permutations of study design elements therein, result in at least four distinct types of incidence estimates:
(1) True incidence is the theoretical incidence in the entire population. As not all people with a psychotic disorder may present to health services, we expect the true incidence to be larger than incidence estimates obtained from clinical or health system data sources.
(2) Contact incidence is derived from contact with the health system for signs or symptoms of psychosis. These presentations may be captured in data sources as subthreshold symptoms and psychotic experiences, or as full psychotic disorder. The contact incidence will align with the true incidence when there is high diagnostic visibility, universal health care coverage and a policy-based emphasis on making mental health services available for people with severe mental illness, including the expansion of early diagnosis and treatment services for psychotic disorders (Goldner, Jones, and Waraich, Reference Goldner, Jones and Waraich2003).
(3) Diagnosed incidence is based on the number of people who receive a diagnosis of psychotic disorder from a clinician (Radigan et al., Reference Radigan, Gu, Frimpong, Wang, Huz, Li, Nossel and Dixon2019). We expect the diagnosed incidence to be lower than the contact incidence, given that contact incidence may include people with subthreshold psychotic symptoms and those who are misdiagnosed using non-standardized criteria.
(4) Treated incidence estimates are distinct from contact and diagnosed incidence, as it suggests that the person has engaged in some form of treatment (Goldner, Jones, and Waraich, Reference Goldner, Jones and Waraich2003). We expect treated incidence to yield the smallest estimate of incidence, typically requiring more stringent criteria be met.
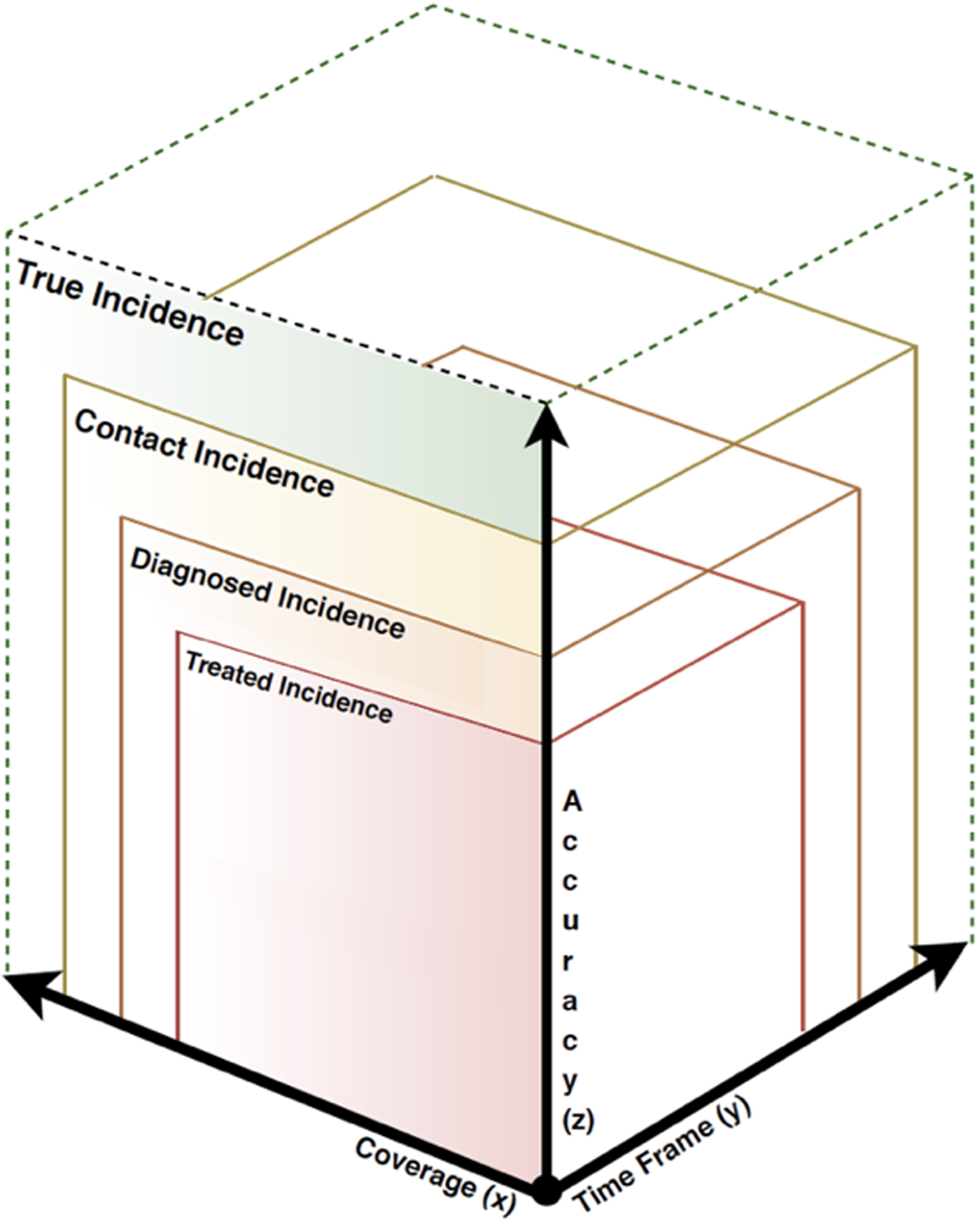
Fig. 1. Categorization of incidence estimates. Note: Volume represents the magnitude of an incidence rate. Figure adapted from Hogerzeil and van Hemert (Reference Hogerzeil and van Hemert2019).
These categorizations are gradational across the spectrum depending on the study design employed. As such, each design element highlighted on the three axes are important components of how close or far the incidence categories are from one another, and how closely they align with the true population incidence.
The case for context
A recent systematic review of the global incidence of psychosis (Jongsma et al., Reference Jongsma, Turner, Kirkbride and Jones2019) provides a useful tool to evaluate the contextualization of incidence estimates in the current literature. Included studies highlight the diversity of study designs used to estimate rates of psychosis, as well as the heterogeneity in incidence estimates across the globe.
The authors of this review categorized study design by combining information from two of the domains of study design found in Hogerzeil and van Hemert's framework, specifically coverage of services and time frame of diagnosis. The results of the meta-regression revealed study design was associated with substantial variations in incidence estimates – specifically, incidence rates were nearly 10-times higher in studies conducted using population registries compared with first contact studies. These results emphasize the substantial impact of study design on incidence estimates, and highlight a need to standardize and expand the ways in which we define and categorize incidence estimates.
In alignment with Hogerzeil and van Hemert, we propose that detailed descriptions of the relevant domains of study design should be reported by all studies measuring incidence – both for psychotic disorders specifically and for mental disorders more broadly – in addition to the use of standardized terminology reflecting the type of incidence estimated. This could be facilitated by the development of an extension to the reporting guidelines for observational studies, focusing on key elements for epidemiological studies reporting incidence and prevalence estimates. A standardized reporting guideline would improve transparency and enable knowledge users to contextualize and synthesize available evidence.
As epidemiologists interested in public mental health, we understand that context and comparison is a crucial aspect of interpretation. Furthermore, providing accurate and standardized estimates of disease are central to assessing the population impact of interventions. There is a need to provide greater clarity on important design elements, and to use specific and accurate nomenclature, when reporting the descriptive epidemiology of psychotic disorders.



