Background
The complex behavioural, psychosocial, functional, and health sequelae associated with dementia make it a uniquely challenging condition to manage. As the condition progresses, neurodegeneration impacts cognition, mood, behaviour, and physical and social functioning, and can result in functional dependence and the need for full-time care (Patterson et al., Reference Patterson, Gauthier, Bergman, Cohen, Feightner and Feldman2001). Dementia increases the risk of motor vehicle accidents for those still driving, medication errors, financial difficulties, and getting lost, with the associated risk of severe injury and death (Rowe, Greenblum, & D’Aoust, Reference Rowe, Greenblum and D’Aoust2012; Sternberg, Wolfson, & Baumgarten, Reference Sternberg, Wolfson and Baumgarten2000). Persons living with dementia have a higher burden of chronic disease, with significantly higher rates of co-morbid conditions related to frailty, medication use, and health service utilization, than older adults without dementia (Gill, Camacho, & Poss, Reference Gill, Camacho, Poss, Bronskill, Camacho, Gruneir and Ho2011).
Family physicians typically refer up to 82 per cent of persons living with dementia to geriatric specialists for assessment and management (Pimlott et al., Reference Pimlott, Siegel, Persaud, Slaughter, Cohen and Hollingworth2006). In Canada, these specialist referral rates are unsustainable given the critical shortage of geriatricians (Hogan et al., Reference Hogan, Borrie, Basran, Chung, Jarrett and Morais2012) and the increasing numbers of individuals with dementia (Smetanin et al., Reference Smetanin, Kobak, Briante, Stiff, Sherman and Ahmad2009). Primary care must therefore assume much greater responsibility for dementia care. However, several studies have concluded that physicians lack confidence in managing dementia and find it more difficult to manage than other chronic diseases and conditions (Harris, Chodosh, Vassar, Vickrey, & Shapiro, Reference Harris, Chodosh, Vassar, Vickrey and Shapiro2009; Turner et al., Reference Turner, Iliffe, Downs, Wilcox, Bryans and Levin2004). It is well documented that family physicians lack knowledge about dementia, particularly as related to cognitive screening, differentiating types of dementia, and recognizing early signs and symptoms of cognitive impairment (Chodosh et al., Reference Chodosh, Petitti, Elliott, Hays, Crooks and Reuben2004; Dubois, Padovani, Scheltens, Rossi, & Dell’Agnello, Reference Dubois, Padovani, Scheltens, Rossi and Dell’Agnello2016; Prins, Hemke, Pols, & Moll van Charante, Reference Prins, Hemke, Pols and Moll van Charante2016) with the result that dementia often goes unrecognized (Bradford, Kunik, Schulz, Williams, & Singh, Reference Bradford, Kunik, Schulz, Williams and Singh2009; Feldman et al., Reference Feldman, Jacova, Robillard, Garcia, Chow and Borrie2008). Once dementia is diagnosed, primary care often lacks the resources needed to provide the comprehensive care required for the optimal management of this condition (Callahan, Hendrie, & Tierney, Reference Callahan, Hendrie and Tierney1995). Challenges experienced in providing dementia care have been associated with health care provider burnout (Duffy, Oyebode, & Allen, Reference Duffy, Oyebode and Allen2009; Kimura, Tamoto, Kanzaki, & Shinchi, Reference Kimura, Tamoto, Kanzaki and Shinchi2011).
Multidisciplinary care approaches and inter-agency partnerships for dementia care provide a significant opportunity to ameliorate the challenges that are associated with dementia care (Crooks & Geldmacher, Reference Crooks and Geldmacher2004; Johansson, Eklund, & Gosman-Hedstrom, Reference Johansson, Eklund and Gosman-Hedstrom2010; Pratt, Clare, & Kirchner, Reference Pratt, Clare and Kirchner2006; Venohr et al., Reference Venohr, Fine, Saunders, Tenney, Vahan and Williams2001). In particular, interprofessional approaches are aptly suited for dementia care, because the complex nature of patient and care partner biopsychosocial needs requires the input and expertise of a range of health care professionals. No one discipline has the expertise to singlehandedly manage the complex medical, cognitive, physical, and psychosocial issues associated with this disease (Grand, Caspar, & Macdonald, Reference Grand, Caspar and Macdonald2011). A randomized controlled trial comparing dementia care provided by a multidisciplinary collaborative team (led by a family physician and a geriatric nurse practitioner and consisting of geriatric specialists and psychologists) with non-collaborative care provided by a single provider found that collaborative care was associated with better treatment and better outcomes related to behavioural and psychological symptoms (Callahan et al., Reference Callahan, Boustani, Unverzagt, Austrom, Damush and Perkins2006). Other studies have demonstrated that collaborative team approaches to dementia care are associated with improved quality of care, adherence to best practice guidelines (Ganz et al., Reference Ganz, Koretz, Bail, McCreath, Wenger and Roth2010; Vickrey et al., Reference Vickrey, Mittman, Connor, Pearson, Della Penna and Ganiats2006), and patient satisfaction with care (Galvin, Valois, & Zweig, Reference Galvin, Valois and Zweig2014; Lee, Hillier, Heckman, et al., Reference Lee, Hillier, Heckman, Gagnon, Borrie and Stolee2014; Lee, Slonim, Hillier, Lu, & Lee, Reference Lee, Slonim, Hillier, Lu and Lee2018). One such collaborative team approach to dementia care is the Multispecialty INterprofessional Team (MINT) memory clinic care model (previously referred to as Primary Care Collaborative Memory Clinics) for which interprofessional team members are specially trained by having completed a comprehensive memory clinic training program in order to establish a memory clinic in their practice setting. This memory clinic will then serve the patients of all physicians in the practice group.
In Ontario, MINT memory clinics, of which there are currently more than 100, aim to build capacity for quality dementia care at a primary care level, while making efficient use of limited available specialist resources (Lee, Hillier, Molnar, & Borrie, Reference Lee, Hillier, Molnar and Borrie2017). MINT memory clinics operate at a primary care level. The clinics are led by family physicians, and at a minimum consist of trained family physicians, nurses, and social workers, but most frequently include other professionals such as pharmacists, occupational therapists, and representatives from local Alzheimer Societies and home care services, as available. Geriatricians, geriatric psychiatrists, and cognitive neurologists provide consultative support to these clinics for the most complex of cases. The patient’s own family physician refers persons with memory concerns or identified challenges in dementia care (e.g., managing medications, caregiver burden, or behaviours) to the MINT memory clinic for comprehensive assessment and care planning, and ongoing care in a shared-care approach.
All patients receive a standardized assessment in which they are assessed by various team members during the same appointment time. Prior to the appointment, patients and caregivers are mailed forms that need to be completed and brought with them to the assessment appointment. These forms include the Functional Activities Questionnaire (Teng et al., Reference Teng, Becker, Woo, Knopman, Cummings and Lu2010) and requests for information on medical, psychiatric, educational, and family history. As part of the team assessment, the MINT memory clinic family physician reviews medical information and completes a targeted physical examination as clinically indicated. Laboratory tests and diagnostic imaging (e.g., cranial computed tomography or magnetic resonance imaging) are ordered as relevant. The team nurse reviews patient information forms; obtains detailed medical and social history; assesses gait quality, weight, and orthostatic vital signs; administers cognitive tests; and completes brief language screening when indicated. The social worker assesses for depression, caregiver stress, behaviours, and risks associated with living with dementia using standardized assessments. The social worker also assesses the need for a home safety assessment and community supports. The team pharmacist reviews patient ability to manage medications and adherence, impact of medications on cognition, and potential for medication-related problems. In many clinics, occupational therapists perform some aspects of the nurse and/or social worker role that are within scope of practice. Outside of the clinic assessment appointment, if needed, occupational therapists may conduct home functional abilities assessments and home safety assessments. Representatives from community agencies and services provide a gateway to their respective services where appropriate. Team members have included the Alzheimer Society, home care services (as provided in Ontario by Home and Community Care, a government agency responsible for the administration of home care services and long-term care placement), Behavioural Supports Ontario (a community-based program aimed at supporting persons living with dementia who are experiencing responsive behaviours), and/or existing geriatric outreach services depending on locally available resources.
Following completion of the various assessments, all team members congregate to review results together and collaborate on preliminary problem formulation and management plan. A decision is made as to whether the complexity of the case requires consultation with one of the specialists supporting the clinic or a direct referral. While the team is meeting, patients and family members wait in a separate room and are offered refreshments. After the team has met, they meet all together with the patient and family members to clarify history and/or the need for further assessment, review findings and diagnosis, and together determine a plan of investigation and management. Immediately following the assessment, the team physician sends a brief message to the referring family physician summarizing the outcome of the assessment and recommendations. When needed, the MINT memory clinic physician consults with a specialist in geriatric medicine, geriatric psychiatry, or cognitive neurology, either by virtual case discussion or by direct patient referral. Post-assessment, arrangements are made for investigations, medication modifications, and community support and services, as relevant. Follow-up is arranged with the patient’s family physician and the MINT memory clinic at appropriate time intervals, depending on patient and caregiver needs and risks identified. A comprehensive report is prepared by the MINT memory clinic family physician to help referring physicians co-manage dementia care. This report outlines the history, cognitive test findings, assessment results, and detailed management plans. Ongoing management support is provided by the clinic team to the referring physician as well as to the patient and family.
The MINT memory clinic model differs from other specialist-led memory clinic care models operating in tertiary care settings, hospital-based specialized geriatric services or specialized psychiatry services, and geriatric research centres that operate at arm’s length from primary care and that focus on providing a consultation service with minimal provision of ongoing patient care (Jolley, Benbow, & Grizzell, Reference Jolley, Benbow and Grizzell2006; Luce, McKeith, Swann, Daniel, & O’Brien, Reference Luce, McKeith, Swann, Daniel and O’Brien2001; Van der Cammen, Simpson, Fraser, Preker, & Exton-Smith, Reference Van der Cammen, Simpson, Fraser, Preker and Exton-Smith1987). The MINT memory clinic care model is summarized in Figure 1 and is described in more detail elsewhere (Lee et al., Reference Lee, Hillier, Stolee, Heckman, Gagnon and McAiney2010; Lee & Hillier, Reference Lee and Hillier2016; Lee, Hillier, Molnar, et al., Reference Lee, Hillier, Molnar and Borrie2017; Lee, Slonim, Hillier, et al., Reference Lee, Hillier, McKinnon, Gregg, Fathi and Sturdy Smith2018; Lee, Hillier, & Weston, Reference Lee, Hillier and Harvey2014). MINT memory clinics work with the patient’s own family physician within a shared care management approach; proactive care plans help primary care provide high-quality dementia care. Aimed at providing comprehensive and patient-centred care, assessments within the memory clinic range in length from 1.4 hours for follow-up appointments to 2 hours for new assessments. This time commitment is in great contrast to the limited time that family physicians are able to provide within the context of typical busy family practice (Lee et al., Reference Lee, Hillier, Stolee, Heckman, Gagnon and McAiney2010; Lee, Hillier, Heckman, et al., Reference Lee, Hillier, Heckman, Gagnon, Borrie and Stolee2014). Within this synchronous team-based care model, all team members work in a coordinated manner to complete the assessment at the same visit and then work collaboratively to formulate a diagnosis and develop an integrated, individualized, and person-centred care plan. This differs from typical multidisciplinary approaches in which the patient is assessed by health care professionals from different disciplines at separate visits and each professional develops a separate care plan that may result in minimal, if any, integration of the services or the different disciplines involved.

Figure 1. MINT memory clinics: Core components and implementation details.
Throughout the course of the illness, MINT memory clinic members work with the patient’s own family physician to ensure that changing care needs are identified and met, such as optimizing medication use, identifying and managing risks, coordinating necessary community services, and managing specific issues that arise, such as responsive behaviours and escalating care needs. This team-based case management facilitates greater collaboration among care providers as team members work together to determine how best to meet patient needs (Salsbury et al., Reference Salsbury, Goertz, Vining, Hondras, Andresen and Long2018). Team-based approaches to case management are in contrast to individual case management, which involves coordination of care by an individual case manager. This type of case management is commonly used in dementia care and has been touted as an opportunity to provide persons living with dementia and their caregivers with information, individualized support, advocacy, and care planning and coordination to improve care and reduce health service utilization and costs (Callahan et al., Reference Callahan, Boustani, Unverzagt, Austrom, Damush and Perkins2006; Iliffe et al., Reference Iliffe, Wilcock, Synek, Carboch, Hradcová and Koch2019; Van Mierlo, Meiland, Van Hout, & Droes, Reference Van Mierlo, Meiland, Van Hout and Droes2014; Vickrey et al., Reference Vickrey, Mittman, Connor, Pearson, Della Penna and Ganiats2006; Walsh & Holton, Reference Walsh, Holton, Rowe and Papp-Paglicci2008). However, it has been suggested that individual case management may be cost prohibitive in some jurisdictions and may be limited in that it operates outside of the patient’s primary care circle, potentially fragmenting care as a result of the high turnover rate in dementia care case managers (Fortinsky, Kulldorff, Kleppinger, & Kenyon-Pesce, Reference Fortinsky, Kulldorff, Kleppinger and Kenyon-Pesce2009; Netting & Williams, Reference Netting and Williams1999).
MINT memory clinics are established following completion of a 5-day nationally accredited interprofessional education program. The program is delivered by members of the Centre for Family Medicine Family Health Team MINT Memory Clinic, in Kitchener, Ontario, which founded the first memory clinic in the province. Practice settings interested in developing a memory clinic select interested team members representing the various disciplines to work in the memory clinic, all of whom must complete the specialized training program. Practice settings without integrated interprofessional health care providers can create multidisciplinary teams through the development of partnerships with community agencies and services (Lee, Hillier, & Gregg, Reference Lee, Hillier and Gregg2019). Funding for the training has come from various sources over time including research agencies, non-profit organizations, and government agencies.
The training program consists of a standardized 2-day workshop, 1-day observership, and 2 days of individualized mentorship (Lee, Kasperski, & Weston, Reference Lee, Kasperski and Weston2011; Lee, Weston, & Hillier, Reference Lee, Weston and Hillier2013). A variety of topics related to dementia care are covered regarding the development and implementation of the MINT memory clinic care model, including how to implement standardized testing; assessment of driving fitness; assessment and management of mood, risk, and caregiver stress; medication optimization; non-pharmacological interventions; and communication with patients and families. Training also focuses on how to schedule and manage clinic flow and work collaboratively to complete the assessment. This evidence-based education program is rooted in current adult learning theory. The program supports active engagement of learners, role-modelling, situated learning experiences (i.e., learning occurs in the environment in which new knowledge is be applied), and opportunities to apply new learning in practice (Mann, Reference Mann2002; Yardley, Teunissen, & Dornan, Reference Yardley, Teunissen and Dornan2012). Following completion of the workshop, new clinic teams spend a day watching the training team conduct assessments. Clinic teams are then mentored over 2 days as they conduct assessments with the training team observing and providing advice and guidance. Annual continuing education sessions (“Booster Days”) provide ongoing opportunities for capacity building, support, and networking (Lee, Hillier, & Weston, Reference Lee, Hillier and Weston2020). Several studies have demonstrated the effectiveness of this training program in establishing MINT memory clinics and changing clinical practice related to dementia assessment and management (Lee et al., Reference Lee, Kasperski and Weston2011, Reference Lee, Weston and Hillier2013; Lee, Hillier, Heckman, et al., Reference Lee, Hillier and Weston2014).
There is some evidence that collaborative care approaches, such as the MINT memory clinic care model, result in enhanced health care provider satisfaction with their work (Barrett, Curran, Glynn, & Godwin, Reference Barrett, Curran, Glynn and Godwin2007; DiCenso et al., Reference DiCenso, Bourgeault, Abelson, Martin-Misener, Kaasalainen and Carter2010; Gaboury, Lapierre, Boon, & Moher, Reference Gaboury, Lapierre, Boon and Moher2011), increased awareness and understanding of the roles and scope of practice of other disciplines (Farris et al., Reference Farris, Cote, Feeny, Johnson, Tsuyuki and Brilliant2004), and improved working relationships (O’Brien, Martin, Heyworth, & Meyer, Reference O’Brien, Martin, Heyworth and Meyer2009). In general, little is known about whether collaborative interprofessional approaches to dementia care reduce the perceived challenges or impact attitudes associated with providing dementia care. Does working within an interprofessional collaborative care model impact the perception of challenges associated with dementia care, enthusiasm for dementia care, or perceptions of having a positive impact on the quality of life of persons living with dementia? Although enthusiasm and passion for dementia care have been identified as requisites for working this field (Evans et al., Reference Evans, Brooker, Thompson, Bray, Milosevic and Bruce2015), to the best of our knowledge, no research has been conducted in this area. The need to improve health care provider experience of care is evidenced by calls to modify the Institute of Healthcare Improvement’s Triple Aim approach to optimizing health system performance to a Quadruple Aim, which would include work life experiences as a system performance indicator (Bodenheimer & Sinsky, Reference Bodenheimer and Sinsky2014; Sikka, Morath, & Leape, Reference Sikka, Morath and Leape2015). Enhancing our understanding of the role of collaborative care approaches on perceived challenges and attitudes towards dementia care will serve to inform efforts to improve health care provider care experiences and to provide further support for the implementation of these types of care models.
The purpose of this study was to explore whether working within an interprofessional collaborative model of dementia care has an impact on health care professionals’ perceptions of the challenges and attitudes associated with providing dementia care and the level of collaboration among health professionals. This study explored collaborative dementia care within the context of MINT memory clinics (Lee, Hillier, Molnar, et al., Reference Lee, Hillier, Molnar and Borrie2017).
Methods
Participants
Participants for this study were memory clinic training program participants (n = 595) who completed the training program (workshop, observership day, and mentorship components) between September 2014 and January 2018. The program was delivered 21 times during this time period. Participants were either trained to establish 49 new MINT memory clinics located in Family Health Teams and Community Health Centres or completed the training program to join existing memory clinics. Training program participants included physicians, registered nurses, registered practical nurses and nurse practitioners, and allied health professionals, including social workers, pharmacists, occupational therapists, and various other disciplines including dieticians, physician assistants, Alzheimer Society representatives, mental health counsellors, and representatives from home care services and Behavioural Supports Ontario.
Pre-Program and Follow-up Surveys
We used a survey methodology in this study, specifically developing surveys for this study. The pre-program survey gathered information on participants’ perceptions of 11 common challenges experienced in various aspects of supporting persons living with dementia (rated on a 5-point scale: 1 = not at all challenging; 5 = extremely challenging). These challenges had been raised in discussions with previous training program participants and are supported by the literature in this area (Boustani, Schubert, & Sennour, Reference Boustani, Schubert and Sennour2007; Harris et al., Reference Harris, Chodosh, Vassar, Vickrey and Shapiro2009; Hinton et al., Reference Hinton, Franz, Reddy, Flores, Kravitz and Barker2007; Kaplan & Berkman, Reference Kaplan and Berkman2011). Respondents were also asked to rate the extent to which their care of patients with dementia in the previous 6 months had been collaborative (defined as involving frequent interactions and knowledge exchanges) with various disciplines involved in dementia care (rated on a 5-point scale: 1 = not at all collaborative; 5 = extremely collaborative). For questions related to dementia care challenges and collaboration with various disciplines, respondents were provided with a “not applicable” response choice. Respondents also rated the extent to which they thought they were able to have a positive impact on the quality of life of their patients living with dementia (5-point scale: 1 = not at all able; 5 = extremely able). This item was presented in a study using a 6-point Likert scale (Harris et al., Reference Harris, Chodosh, Vassar, Vickrey and Shapiro2009) and was modified in this study to be a 5-point scale. Five-point Likert scales are used in this study because they are commonly used to measure health-related perceptions and attitudes (Ho, Reference Ho2017). Five-point scales are simple to construct, easy to administer, and easily understood, and interpreting the results is straightforward (Ho, Reference Ho2017; Murphy & Davidshofer, Reference Murphy and Davidshofer2001).
Health provider attitudes toward dementia care were derived from the Utrecht Work Engagement Scale, a measure of work engagement and fulfillment (Schaufeli, Bakker, & Salanova, Reference Schaufeli, Bakker and Salanova2006). Question wording from this scale was modified from reference to “my job” to “my work with persons living with dementia”. Respondents rated how often (never; almost never = a few times a year or less; rarely = once a month or less; sometimes = a few times a month or less; often = once a week; very often = a few times a week; or always = every day) they felt enthusiastic about their work with persons living with dementia, felt that their work with persons living with dementia inspired them, and felt proud of the work that they do with persons living with dementia.
Emotional energy experienced by health professionals is considered a motivating force for establishing and maintaining therapeutic relationships; lack of emotional energy in this role has been associated with compassion fatigue and care provider burnout (Cocker & Joss, Reference Cocker and Joss2016; Figley, Reference Figley2002; Shimazu & Schaufeli, Reference Shimazu and Schaufeli2008; van Mol, Kompanje, Benoit, Bakker, & Nijkamp, Reference van Mol, Kompanje, Benoit, Bakker and Nijkamp2015). Based on this concept, we created a “battery” analogy to measure level of energy for dementia care (energized vs. drained), as dementia care can often be empowering, but at other times can be rather depleting. Respondents were asked to select the “battery level” (completely drained, 20%, 40%, 60%, 80%, completely energized) that most accurately reflected their energy levels associated with working with persons living with dementia during the previous 6 months. In the pre-program survey, respondents were asked to identify their discipline from a list provided; they were also given an “other” response choice in which to specify their discipline. They were also asked to provide the number of years that they have been employed in their current profession.
Questions presented in the pre-program survey were repeated in the follow-up survey. The surveys were pilot tested with four health professionals working in a MINT memory clinic with representation from various health disciplines. Pilot data were not retained for inclusion in this study. Revisions were made to the survey consistent with feedback received; revisions were made primarily to clarify wording. MINT memory clinic training program participants were invited to complete a survey prior to the training workshop. Follow-up surveys were administered 6 months following the launch of the newly established MINT memory clinics. For those participants joining existing memory clinics, the survey was administered 6 months following the completion of the training program. Both surveys were administered online (www.surveymonkey.com). Participants received an invitation to complete each survey via e-mail, in which a link to the survey was provided. Participants were provided with a 2-week time period in which to complete the surveys and were provided with two reminders via e-mail. Survey completion was anonymous. Participants created their own unique identification code that was used to match pre-program and follow-up surveys for analysis.
This study was approved by the Hamilton Integrated Research Ethics Board, McMaster University (REB #13-266).
Data Analysis
SPSS 25.0 (IBM Corp, 2018) was used to generate descriptive statistics (frequencies, means, standard deviations). We matched pre-program and follow-up surveys so that differences at an individual level could be examined. Survey matching was not possible in some instances in which respondents did not complete one of the surveys or failed to provide their identification code on one of the surveys. We explored differences between the pre-program and follow-up survey ratings of the challenges, attitudes, and level of collaboration associated with providing dementia care using two-tailed paired t tests. Differences in these outcome ratings and years in current profession among groups (physicians, nurses, and allied health professions and between those trained to establish new memory clinics and those trained to join existing clinics) were explored using non-parametric analysis of variance (Kruskal–Wallis Test). Where relevant, post-hoc pairwise comparisons using the Dunn–Bonferroni post-hoc method were used to test for differences in means between groups (Dunn, Reference Dunn1961). Between-discipline analyses were conducted between physicians, nurses, and allied health professionals. Given the lower number of individuals representing various disciplines such as social workers, pharmacists, occupational therapists, counsellors, and dietitians, these disciplines were grouped together as allied health professionals. For the purposes of describing the sample, nurses and social workers employed by the Alzheimer Society were differentiated from those employed by the primary care practice setting.
Given a desired statistical power level of 0.95, we required a sample size of 103, assuming a moderate effect size of 0.5. Power analysis was conducted using the G*Power 3.1 program (Faul, Erdfelder, Lang, & Buchner, Reference Faul, Erdfelder, Lang and Buchner2007). Cohen’s dz was calculated to measure the effect size of observed differences between pre-program and follow-up survey outcome scores (Cohen, Reference Cohen and Wolman1965); d = 0.2 was interpreted as a small effect size, 0.5 was interpreted as a medium effect size, and 0.8 was interpreted as a large effective size (Lakens, Reference Lakens2017). In Cohen’s dz the numerator is the mean difference within subjects and the denominator is the standard deviation of the within-subject change scores, making it appropriate to use with a within-subjects design (Cohen, Reference Cohen1988). The Bonferroni adjustment method (Chen, Feng, & Yi, Reference Chen, Feng and Yi2017) was used to control for familywise error rate; accordingly, significance for p values was set at < 0.002. Pearson’s correlation coefficient was used to measure the association between perceptions of ability to impact positive change in patients’ quality of life and perceptions of enthusiasm, inspiration, pride, and energy level for dementia care.
Results
A total of 552 pre-program surveys were completed, representing a 93 per cent response rate; 247 follow-up surveys were completed (44% response rate), of which 228 (92%) could be matched with pre-program surveys. Survey respondent characteristics are presented in Table 1. For matched pre-program and follow-up surveys, there was a relatively even distribution across the three discipline groups. In the matched survey sample (n = 228), the mean number of years in their current profession across all respondents was 12.6 years. In this sample, years in practice did not vary significantly (p = 0.143) among the three discipline groups. In the pre-program survey sample (n = 552), mean years in the current profession was significantly lower for allied health professionals (mean = 9.1) than for physicians (n = 12.9) and nurses (n =12.1), p = 0.001.
Table 1. Survey respondent characteristics
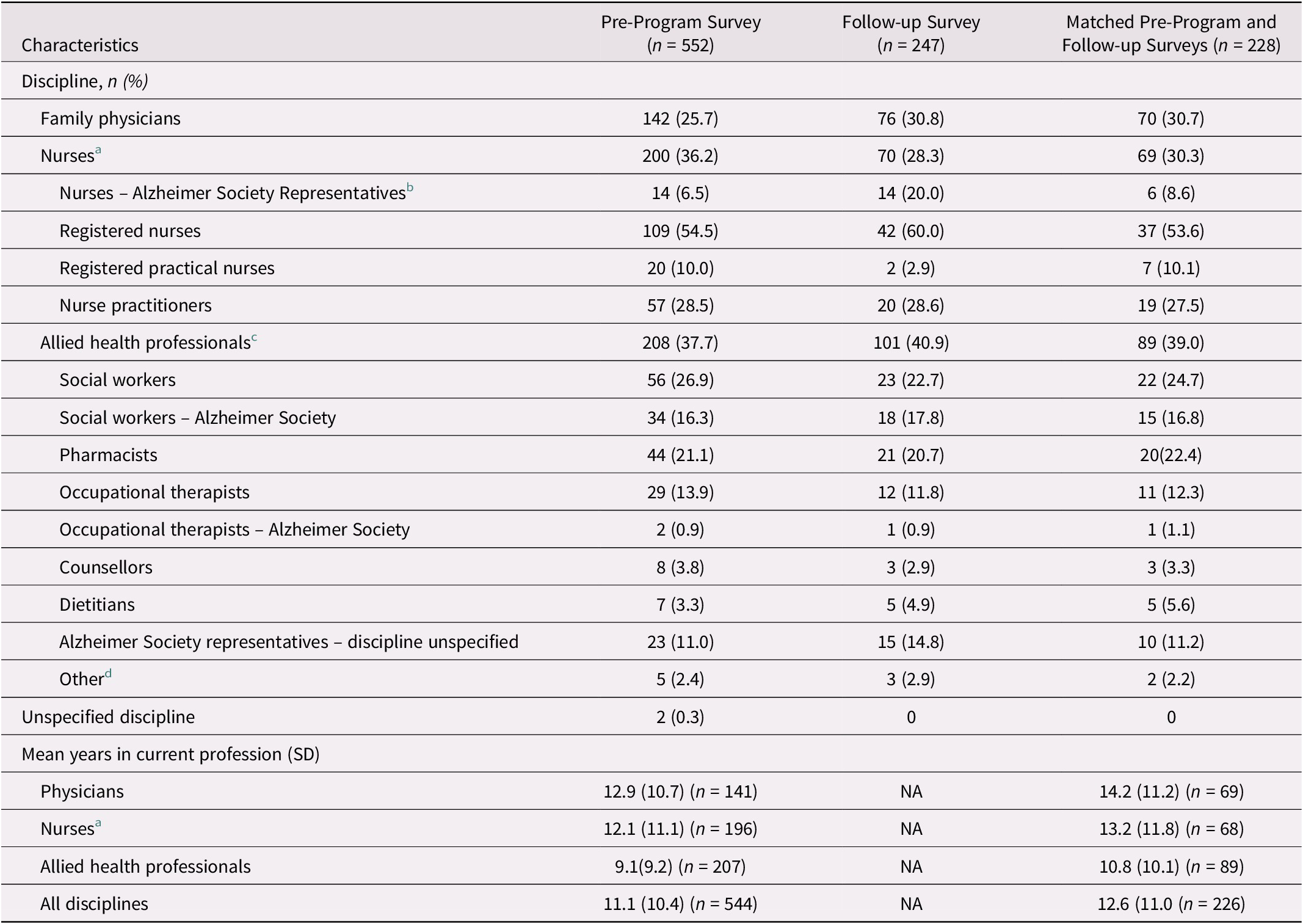
Note. Percentages may not sum to 100% because of missing values.
a Registered nurse/ registered practical nurse/ nurse practitioner; percentages specified for nurses who were Alzheimer Society representatives are based on the total number of nurses for each of the surveys.
b Percentages are based on the total number of nurses for each of the surveys.
c Percentages are based on the total number of allied health professionals for each of the surveys.
d Other disciplines included: Exercise physiologists, physical therapists, physician assistants, and speech-language pathologists.
SD, standard deviation.
As there were no significant differences in study outcomes among disciplines, or between those trained to establish new memory clinics and those trained to join existing clinics, results are presented across all respondents.
Challenging Aspects of Dementia Care
Prior to completing the memory clinic training program, mean ratings (on a scale of 1–5) of the level of perceived challenge associated with various aspects of dementia care ranged from 2.3 (developing a therapeutic alliance with caregivers and working collaboratively with other health professionals) to 3.6 (timely access to specialist support), reflecting that these activities were “a little” to “very” challenging (Table 2). At follow-up, mean challenge ratings (on a scale of 1–5) across the dementia care activities ranged from 1.8 (working collaboratively with other health care professionals) to 2.8 (access to specialist support), reflecting that these activities were now “a little” to “somewhat” challenging. Across all activities, there were statistically significant reductions in perceived level of challenge from pre-program to follow-up, with the exception of delivering bad news (p = 0.054). Effect sizes were moderate for managing the needs of persons living with dementia and caregivers, and for timely access to specialist support and community services, but were otherwise small.
Table 2. Pre-program and follow-up survey mean (SD) ratings of the level of challenge (5-point rating scale: 1 = not at all challenging; 5 = extremely challenging) associated with various aspects of dementia care
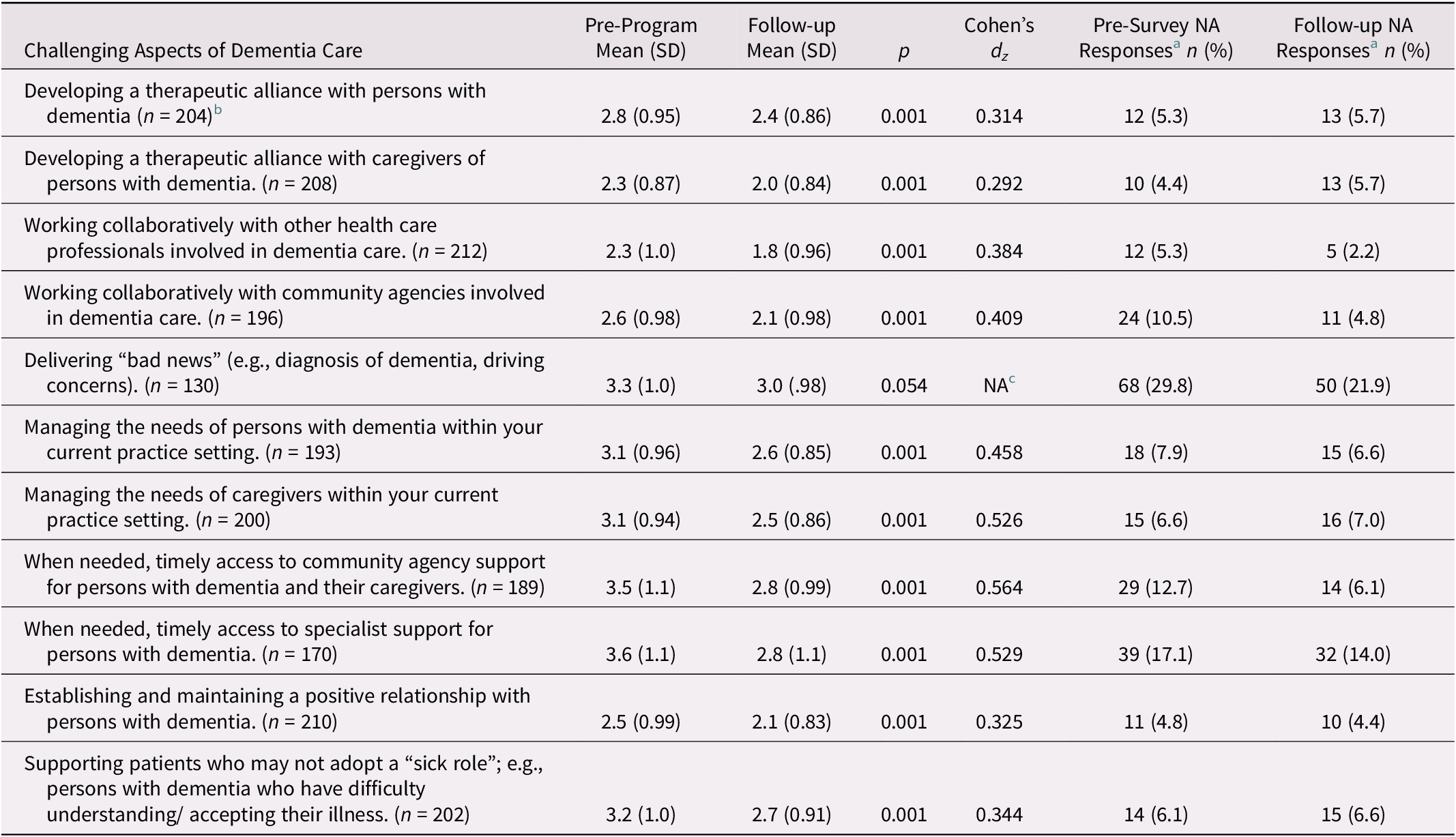
Note.
a Percentages are based on n = 228 (matched pre- and follow-up surveys).
b ns within parentheses represent the number of respondents completing each item.
c NA Cohen’s d was not calculated because difference is not statistically significant.
SD = standard deviation; NA = not applicable, if the activity was considered beyond the scope practice.
Attitudes Towards Dementia Care
Prior to completing the memory clinic training program, mean ratings (on a scale of 1–7) of the frequency with which respondents experienced enthusiasm, inspiration, and pride in their work in dementia care ranged from 5.0 to 5.2, reflecting that these were experienced “often” (at least once a week) (Table 3). At follow-up, mean ratings ranged from 5.7 to 5.9, reflecting that these were now experienced “very often” (several times a week). From pre-program to follow-up, there were statistically significant increases in the frequency with which participants experienced enthusiasm, inspiration, and pride in their work in dementia care; the effect sizes were moderate. Similarly, from pre-program to follow-up there was a significant increase in the extent to which respondents perceived themselves as being able to have a positive impact on the quality of life of their patients and caregivers; the effect size was moderate (Table 3). Related to the level of energy that respondents experienced for dementia care, prior to completing the memory clinic training program, mean ratings (ranging from 0%, completely drained to 100%, completely energized) of “battery level” (39.6%) reflected that respondents felt relatively drained by their work in dementia care (Figure 2). At follow-up, mean energy ratings (69.1%) were significantly increased (p = 0.001), indicating that participants were more energized to provide dementia care and a large effect size was observed (d = 0.980). All of these variables are positively correlated, so that as perceptions of ability to have a positive impact on the quality of life of patients increased, so did perceptions of enthusiasm, inspiration, pride, and energy levels (Table 4).
Table 3. Pre-program and follow-up survey mean ratings (SD) of various attitudes towards dementia care, n = 228
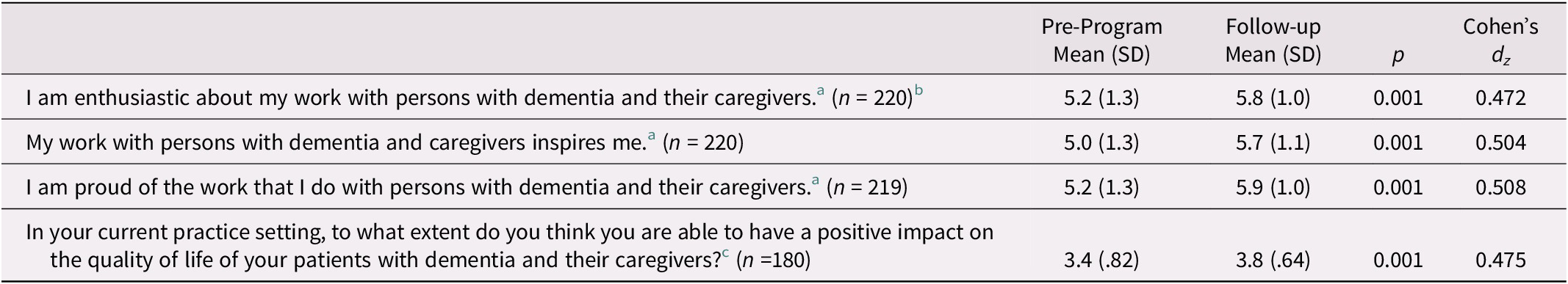
Note.
a 7-point rating scale: 1 = never; 2 = almost never (a few times a year or less); 3 = rarely (once a month or less); 4 = sometimes (a few times a month or less); 5 = often (once a week); 6 = very often (a few times a week); 7 = always (every day).
b Numbers in parentheses represent the number of respondents completing each item.
c 5-point scale: 1 = not at all able; 5 = extremely able.
SD = standard deviation.
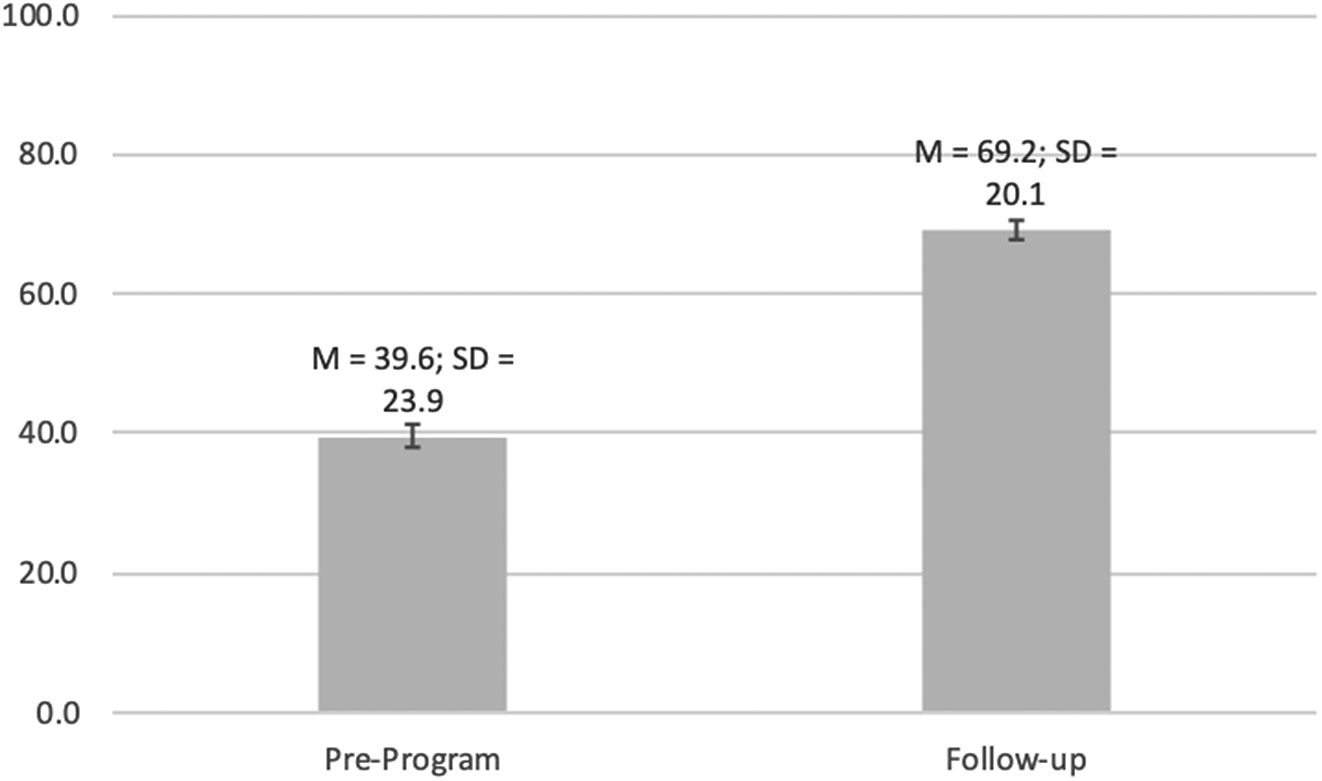
Figure 2. Mean ratings of level of energy for dementia care (n =221). 0 = completely drained; 100% = completely energized.
Table 4. Correlations between perceptions of ability to have a positive impact on the quality of life of patients and perceptions of enthusiasm, inspiration, pride, and energy level for dementia care, n = 228
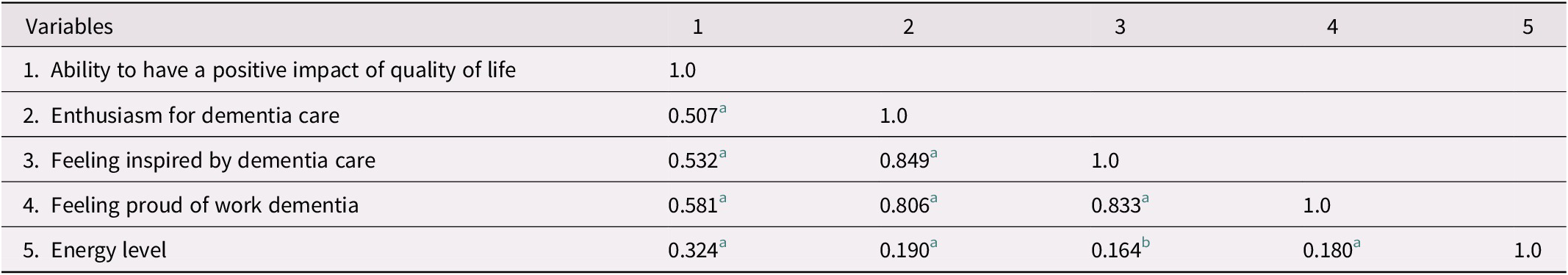
Note.
a p < 0.01
b p < 0.05
Level of Collaboration in Dementia Care
Prior to completing the memory clinic training program, mean ratings (on a scale of 1–5) of level of collaboration (defined as involving frequent interactions and knowledge exchanges) with various disciplines involved in dementia care ranged from somewhat collaborative for work with Behavioural Supports Ontario representatives (2.6) to very collaborative for work with nurses (3.9; see Table 5). At follow-up, mean ratings of level of collaboration with various disciplines involved in dementia care ranged from somewhat collaborative for work with Behavioural Supports Ontario representatives (2.8) and home care case managers (2.9) to extremely collaborative with nurses (4.5), social workers (4.5), and Alzheimer Society representatives (4.5). At follow-up, mean ratings of level of collaboration across all the disciplines, with the exception of home care case managers and Behavioral Supports Ontario representatives, were significantly increased, reflecting that respondents perceived more frequent interactions and knowledge exchanges with these disciplines for dementia care. Effect size was largest for collaboration with Alzheimer Society representatives, moderate for social workers and occupational therapists, and otherwise small for other disciplines.
Table 5. Mean (SD) ratings a of the level of collaboration b with various disciplines for dementia care, n = 228
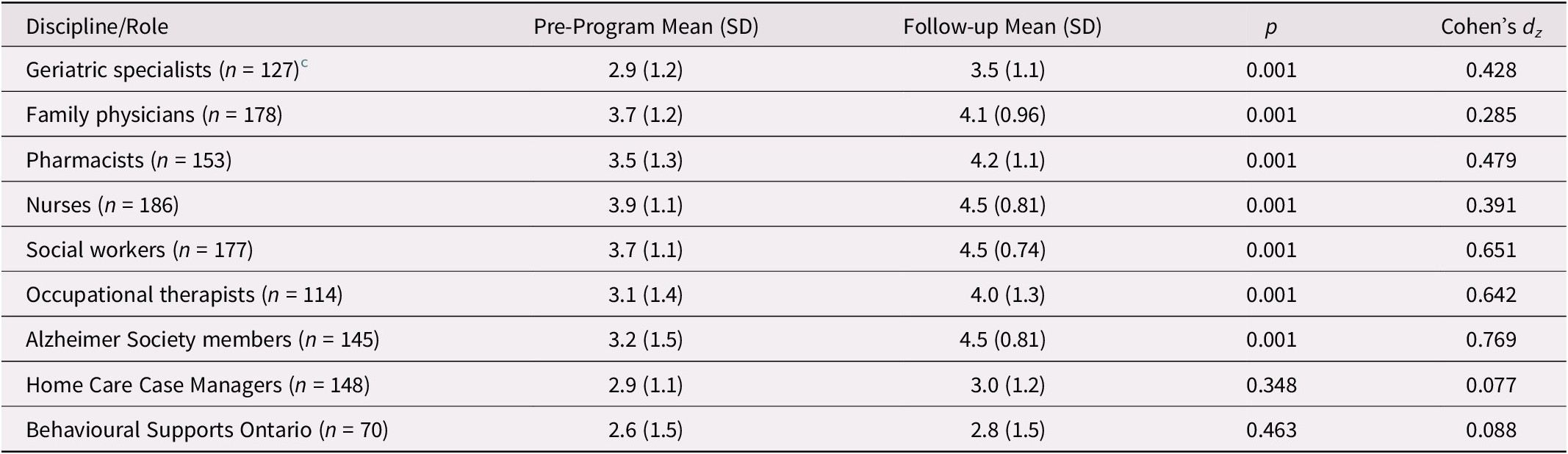
Note.
a 5-point rating scale: 1 = not at all collaborative; 5 = extremely collaborative.
b Defined as involving frequent interactions and knowledge exchanges with different care providers.
c The ns represent the number of matched pre-post ratings of level of collaboration for each discipline.
SD = standard deviation.
Discussion
This study demonstrated that working in an interprofessional collaborative model of dementia care can positively impact health professionals’ perceptions of the challenges and attitudes associated with providing dementia care and can improve collaboration among health providers in providing dementia care. Through their work in the MINT memory clinic model, participants perceived improved collaboration with community care supports (Alzheimer Society) and other health care professionals involved in dementia care. They also found it less challenging to provide most aspects of dementia care, perhaps because of increased and meaningful collaboration among interprofessional team members and the team-based case management approach used in this care model. Lastly, working within the MINT memory clinic model was associated with improved attitudes towards dementia care. Participants experienced increased enthusiasm, inspiration, pride, and energy for dementia care, and felt that they were better able to have a greater impact on quality of life of persons living with dementia and their caregivers. These findings are consistent with those of a phenomenological study exploring MINT memory clinic team member experiences with the provision of dementia care (Sheiban, Stolee, McAiney, & Boscart, Reference Sheiban, Stolee, McAiney and Boscart2018). In this study, team members described how working with others in this care model has led to personal and professional fulfillment, as it enabled them to have an important impact on the lives of persons living with dementia and found this work meaningful and motivating.
It is possible that some challenges associated with dementia care can be addressed by practice infrastructure supports and collaborative practice, as offered by the MINT memory clinic model. Working in a collaborative care model eases the challenges associated with working with other health professionals, community agencies, and specialists more than it eases those associated with working directly with persons living with dementia and caregivers. This is evidenced by the smaller effect size of follow-up survey differences in challenge ratings associated with aspects of direct care with persons living with dementia and caregivers. Limited change in challenges related to delivering bad news and forming therapeutic alliances with persons living with dementia may reflect challenges in communication and social interactions with persons living with dementia and caregivers, such as their reaction to difficult news, particularly if it affects their autonomy, such as suspension of driving license privileges (Adams & Gardiner, Reference Adams and Gardiner2005). No matter how well skilled health professionals become at delivering upsetting news, there are understandable negative reactions to bad news, no matter how well it is communicated. An important role for clinicians is to help patients ameliorate the suffering associated with bad news and its consequences (Rabow & McPhee, Reference Rabow and McPhee1999).
Prior to completing the memory clinic training program and working within MINT memory clinics, participants perceived their interactions with their primary care colleagues (family physicians, pharmacists, nurses, social workers) as being moderately collaborative and their interactions with geriatric specialists and community-based services (Alzheimer Society, home care, Behavioural Supports Ontario) as being less collaborative. After working in the MINT memory clinics for 6 months, participants perceived their work in dementia care to be more collaborative, particularly with representatives from the Alzheimer Society, but also with their own primary care colleagues (social workers, pharmacists, occupational therapists). This is evidenced by the moderate to large effect sizes in differences in collaboration ratings at follow-up. The lower effect sizes in differences in level of collaboration with geriatric specialists, family physicians, and nurses suggests that more work needs to be done to support collaborations with these disciplines. The lack of change in collaboration with representatives from home care services and Behavioural Support Ontario may reflect the relative lack of integration of these roles within the primary care practice setting. Opportunities to better integrate these services into the MINT memory clinic care model, ensuring meaningful contributions to the assessment process and care planning, may facilitate more collaborative interactions with these services. Previous research has demonstrated higher levels of involvement with community services when representatives from these services are fully integrated in the memory clinic as team members (Lee, Hillier, & Harvey, Reference Lee, Hillier and Weston2014; Lee, Lu, Hillier, Gregg, & Kaufman Carlin, Reference Lee, Lu, Hillier, Gregg and Kaufman Carlin2019).
A number of factors likely contributed to increased collaboration in the MINT memory clinics and reduced perceptions of dementia care as challenging. These factors may include the interprofessional nature of the memory clinic training program, the efficient standardized processes within the MINT memory clinic care model, and the team-based case management approach. It is likely that the interaction of the training and clinical practice within this care model contributed to changes in collaboration for dementia care. Interprofessional education has been identified as a prerequisite for collaborative dementia care (Cartwright, Franklin, Forman, & Freegard, Reference Cartwright, Franklin, Forman and Freegard2015; Dreier-Wolfgramm et al., Reference Dreier-Wolfgramm, Michalowsky, Austrom, van der Marck, Iliffe and Alder2017). A review of effective collaborative dementia care models highlighted the important role of interprofessional education in team-based approaches to facilitate collaborative care (Dreier-Wolfgramm et al., Reference Dreier-Wolfgramm, Michalowsky, Austrom, van der Marck, Iliffe and Alder2017). Learning together, health professionals develop shared goals for care and recognize each other’s knowledge, skills, and roles and their unique contributions to dementia care, which facilitates an increase in mutual trust and better preparation to work collaboratively in clinical practice (Cartwright et al., Reference Cartwright, Franklin, Forman and Freegard2015; Lee et al., Reference Lee, Weston and Hillier2013). Interprofessional education has been identified as a significant opportunity to build capacity for optimal, evidence-based dementia care; to foster early diagnosis; and to coordinate referrals to community services (Downs et al., Reference Downs, Turner, Bryans, Wilcox, Keady and Levin2006; Galvin et al., Reference Galvin, Valois and Zweig2014; Iliffe et al., Reference Iliffe, Wilcock, Griffin, Jain, Thune-Boyle and Koch2010). Evaluations of the MINT memory clinic training program and model of care have highlighted the importance of this interprofessional education training program to the establishment and implementation of the memory clinics (Lee et al., Reference Lee, Weston and Hillier2013; Lee, Hillier, Heckman, et al., Reference Lee, Hillier, Heckman, Gagnon, Borrie and Stolee2014). The memory training program includes education on effective teamwork and supports team building by requiring team members to work together on case study presentations and encouraging members of each discipline to contribute to their full scope of practice. Observership opportunities with the interprofessional training team serve to model and reinforce collaborative processes and care. Promotion of collaborative values in education programs can facilitate interprofessional collaboration (San Martin-Rodriguez, Beaulieu, D’Amour, & Ferrada-Videla, Reference San Martin-Rodriguez, Beaulieu, D’Amour and Ferrada-Videla2005). Moreover, at an individual level, willingness to collaborate in a team, a shared interest in care of the elderly, and respect for the unique and complementary contributions of each discipline to dementia care have been identified as key to the successful implementation of the memory clinics (Lee, Hillier, Heckman, et al., Reference Lee, Hillier, Heckman, Gagnon, Borrie and Stolee2014).
Collaboration within MINT memory clinics is facilitated by the structure of the clinics and clinic processes. Although the clinics are family physician led, there is a relatively flat hierarchy in which the physician is not necessarily the dominant decision maker. All team members work together to identify key issues and develop effective care plans to address identified issues. Limited power differentials, values that support collaborative practice over individualism, and interdependence among professionals are key to successful interprofessional collaboration in health care (San Martin-Rodriguez et al., Reference San Martin-Rodriguez, Beaulieu, D’Amour and Ferrada-Videla2005). Within the MINT memory clinic care model, all team members contribute to the success of the outcome and work at their maximum scope of practice. This serves to foster a synergistic method of working together. As a result, the burden of care may be less overwhelming and challenging for care providers than it is when they provide care independently, and they experience better satisfaction with the care that they provide.
The team-based case management approach used in the MINT memory clinic care model may also have contributed to improved collaboration and attitudes towards dementia care. There is generally a dearth of evidence on the effectiveness of team-based case management. Some evidence exists that suggests that this approach to case management results in high levels of patient satisfaction (Day et al., Reference Day, Demirkol, Tynan, Curry, Hines and Lintzeris2012), improved patient outcomes and reduced health service utilization (Aberg-Wistedt, Cressell, Lidberg, Liljenberg, & Osby, Reference Aberg-Wistedt, Cressell, Lidberg, Liljenberg and Osby1995), and increased job satisfaction, staff morale, and retention (Block, Wheeland, & Rosenberg, Reference Block, Wheeland and Rosenberg2014). In contrast to individual case management approaches that tend to operate external to the patient’s primary care circle (Van Mierlo et al., Reference Van Mierlo, Meiland, Van Hout and Droes2014; Walsh & Holton, Reference Walsh, Holton, Rowe and Papp-Paglicci2008), a primary care team-based management approach leverages existing primary care infrastructure and uses the expertise and strengths of each discipline to support the varied medical, functional, and psychosocial needs of persons living with dementia and their caregivers. These oftentimes complex and interrelated needs may be best addressed by health care teams working collaboratively in a coordinated and integrated way to develop effective care plans that are holistic and not solely medical in focus (Day et al., Reference Day, Demirkol, Tynan, Curry, Hines and Lintzeris2012). In doing so, no one health care professional, is left feeling helpless in responding to complex issues and may indeed feel able to have a greater impact on improving patient care and quality of life. As demonstrated in this study, various aspects of dementia care were perceived as less challenging and team members had a more positive attitude towards dementia care after working in a collaborative team. An interprofessional team approach also serves to overcome challenges experienced by persons living with dementia and caregivers related to accessing information about dementia, knowledgeable care providers, and community services (Prorok, Hussain, Horgan, & Seitz, Reference Prorok, Hussain, Horgan and Seitz2017). This is true of the MINT memory clinic model, as team members provide person-centred care for patient and caregiver dyads with care coordination and system navigation support offered throughout the disease process as needed (Lee, Hillier, et al., Reference Lee, Hillier, McKinnon, Gregg, Fathi and Sturdy Smith2018).
This study has demonstrated how interprofessional team-based approaches to dementia care in which assessment and care are provided in a synchronous, coordinated and integrative manner can improve how health professionals work together to provide dementia care and how they feel about providing dementia care. Job dissatisfaction in dementia care has been associated with feeling that one is unable to adequately manage dementia or have an impact on a person living with dementia and feeling unsatisfied with the quality of care provided (Vernooij-Dasssen et al., Reference Vernooij-Dasssen, Faber, Olde Rikkert, Koopmans, Van and Braat2009). In contrast, increased job satisfaction in dementia care has been associated with opportunities for skill development and training, personal growth, delivery of person-centred care and quality care, and confidence in one’s ability to provide quality care (Drebing, McCarty, & Lombardo, Reference Drebing, McCarty and Lombardo2002; Teri, Huda, Gibbons, Young, & van, Reference Teri, Huda, Gibbons, Young and Van2005; Vernooij-Dasssen et al., Reference Vernooij-Dasssen, Faber, Olde Rikkert, Koopmans, Van and Braat2009). Similarly, it has been shown that perceptions of the meaningfulness of one’s job impacts engagement in that job (May, Gilson, & Harter, Reference May, Gilson and Harter2004). Perceptions of the meaningfulness of one’s job is associated with rewarding interactions with coworkers and, conversely, when jobs are perceived as meaningless, people are more likely to experience burnout and detach themselves from their work (May et al., Reference May, Gilson and Harter2004). Working to one’s full potential and in service to others have also been associated with job meaningfulness (Lips-Wiersma & Wright, Reference Lips-Wiersma and Wright2012). Moreover, working within a patient centered approach that emphasizes the psychosocial aspects of dementia care can reduce the care burden experienced by physicians, as less emphasis is placed on their role in curing disease and greater emphasis is placed on helping persons living with dementia to live well with their disease (Apesoa-Varano, Barker, & Hinton, Reference Apesoa-Varano, Barker and Hinton2011). All of these characteristics are consistent with the MINT memory clinic care model, which emphasizes person-centred care, working to full scope of practice, and collaboration (Lee, Hillier, Molnar, et al., Reference Lee, Hillier, Molnar and Borrie2017). It has been demonstrated that the MINT memory clinic training program provides a significant opportunity for building knowledge, skill, and confidence in dementia care (Lee et al., Reference Lee, Weston and Hillier2013) and for improving the quality of dementia care provided (Lee, Hillier, Heckman, et al., Reference Lee, Hillier and Weston2014). The results of this study suggest that the MINT memory clinic care model provides primary care with a more effective and enjoyable way of addressing a condition that is traditionally difficult to manage, and in doing so, provides personal satisfaction that may reach to the root of why clinicians chose a career in health care. Indeed, it was dissatisfaction with the limitations imposed in traditional models of primary care dementia care that inspired the development of the MINT memory clinic care model.
This study provides further evidence of the positive impacts associated with the MINT memory clinic model. This care model has demonstrated efficient use of limited specialist resources by freeing specialists and their teams to focus on the management of the most complex cases while MINT memory clinics manage the majority of cases of dementia that may be less complex (Lee et al., Reference Lee, Hillier, Stolee, Heckman, Gagnon and McAiney2010; Lee, Hillier, Molnar, et al., Reference Lee, Hillier, Molnar and Borrie2017; Lee, Hillier, et al., Reference Lee, Slonim, Hillier, Lu and Lee2018). There is also evidence of high levels of satisfaction among referring physicians (Lee & Hillier, Reference Lee and Hillier2016) and positive patient and care partner experience with care (Lee, Slonim, et al., Reference Lee, Hillier, McKinnon, Gregg, Fathi and Sturdy Smith2018). Positive health system impacts have been demonstrated related to delayed time to first emergency department visit and hospitalization, reduced alternate level of care days, and delayed long-term care placement and associated cost savings (Health Innovations Group, 2019). Quality improvement in health care in Ontario is guided by the Quadruple Aim framework, which emphasizes the importance of improved patient experiences, better health outcomes, lower health care costs, and improved health care provider experience (Bodenheimer & Sinsky, Reference Bodenheimer and Sinsky2014). The findings from this study demonstrate that the MINT memory clinic care model improved health professionals’ experience of dementia care. Along with previously demonstrated improvements to patient experience of care (Lee, Slonim, et al., Reference Lee, Hillier, McKinnon, Gregg, Fathi and Sturdy Smith2018) and outcomes (Lee, Hillier, Heckman, et al., Reference Lee, Hillier and Weston2014; Lee, Hillier, Molnar, et al., Reference Lee, Hillier, Molnar and Borrie2017), and reduced health system costs (Health Innovations Group, 2019), this would suggest that the MINT memory clinic model is achieving the Quadruple Aim approach to optimizing health system performance (Bodenheimer & Sinsky, Reference Bodenheimer and Sinsky2014).
Limitations
The outcome measures in this study were self-reported; therefore, the extent to which care is indeed collaborative, as defined by frequent interactions and information sharing between health professionals, is not known. Alternative methodologies, such as chart audits and observational studies to assess frequency and type of interactions between team members and coordination of care are needed to increase our understanding of the nature and extent of collaboration within interprofessional teams in comparison with usual care or alternative models of dementia care. The pre-post study design may have introduced a response bias resulting from a perceived need to report differences in the expected direction. This bias is likely minimal, as there were no incentives for bias, because survey questions were non-leading and responses were anonymous. More rigorous methodologies, such as randomized control trials or study designs that provide control or comparison groups would allow for more meaningful conclusions to be drawn about the impact of collaborative care models on attitudes towards dementia care, particularly in light of the low response rate for the follow-up survey (44%). Given this low response rate, the follow-up survey results may not be representative of all participants. Response rates for follow-up surveys in our previous studies have varied from 36 per cent (Lee, Hillier, Heckman, et al., Reference Lee, Hillier and Weston2014) to 67 per cent (Lee et al., Reference Lee, Weston and Hillier2013) with a median of 54% (Lee, Hillier, & Gregg, Reference Lee, Hillier and Gregg2019). It is not entirely clear why follow-up survey response rates are low, but we suspect that this may reflect time constraints in busy family practice settings and low motivation to complete a survey for a program completed 6 months earlier. Low response rates for follow-up surveys are not unusual. A review of response rates for online follow-up surveys completed by health professionals found response rates ranging from 5 per cent to 62 per cent; response rates of 30–50 per cent were deemed “good”, and anything over 50 per cent, was deemed “excellent” (Silverman et al., Reference Silverman, Schrimshaw, Franks, Hirsch-Moverman, Ortega and El-Sadr2018).
This study explored how attitudes towards dementia care are influenced by work within an interprofessional collaborative care model. Pre-survey attitudes towards dementia care were fairly positive, perhaps reflecting a selection bias in that participants of the MINT memory clinic training program were self-selected based on their interest in care of the elderly. Selection bias may also have influenced follow-up survey results if less engaged and less satisfied participants did not respond to the second survey. However, this was not the case, as there were no statistically significant differences in ratings of enthusiasm, inspiration, pride, or energy level in the pre-survey between those who responded to the follow-up and those who did not. Energy for dementia care was measured to gather a sense of health professionals’ experience with care. Energy level as a psychological construct has not, to the best of our knowledge, been studied as related to attitudes towards provision of health care. However, intuitively, it makes sense that when health professionals feel depleted, they will have a less positive experience with care, similar to the concept of burnout, which is characterized by pessimism, loss of enthusiasm for clinical work, and low feelings of accomplishment (Shanafelt et al., Reference Shanafelt, Boone, Tan, Dyrbye, Sotile and Satele2012).
Future Directions
As it could be argued that health professionals’ positive experience with care within the MINT memory clinic model could be attributed to greater time allotted for dementia care, more research is needed to understand the nuances of positive experience with care and how these are manifested in dementia care, both in interprofessional care models, such as the MINT memory clinic care model, and in non-team-based care models. More research is also needed on the collaboration between memory clinic physicians and the specialists assigned to support the clinics. Early research has revealed that clinic physicians and specialists value their collaboration for dementia care and desire more opportunities for collaboration (Lee, Hillier, Locklin, Lumley-Leger, & Molnar, Reference Lee, Hillier, Locklin, Lumley-Leger and Molnar2019). Studies are currently underway to better understand the collaborative relationship between clinic physicians and specialists and how collaboration can be best fostered, supported, and sustained over time. More research is also needed on how team members work to the maximum scope of practice and synergistically together and how best to enhance and sustain positive attitudes towards dementia care over time. Generally, there is limited research on the role of interprofessional education on facilitating collaborative knowledge, skills, and practice (Jackson et al., Reference Jackson, Pelone, Reeves, Hassenkamp, Emery and Titmarsh2016). More research is needed on how interprofessional education can facilitate interprofessional collaborative practice for dementia care.
Conclusion
There is an urgent need for models of dementia care that build system capacity and efficiency and that improve health care provider experience with care, leveraging the large infrastructure of primary care in Canada and other countries to better meet the needs of our aging population. The MINT memory clinic care model provides one such dementia care model. This study provides some insights into the effect of the MINT memory clinic interprofessional approach to dementia care on health care professionals’ perceptions of the challenges and attitudes associated with providing dementia care and level of collaboration with other health professionals. Interprofessional team-based approaches, such as the MINT memory clinic model, can foster and support optimal dementia care through synergistic and collaborative working relationships, and can foster positive attitudes toward dementia care. This in turn will promote positive patient and care partner experience with care, as their care team will be engaged to provide patient-centred and well-coordinated care.










