Maternal stress exposure and mental health problems during pregnancy are well-established risk factors for adverse child development and psychopathology, suggesting that developmental origins of later mental health begin even before birth (Glover, Reference Glover2011; Van den Bergh et al., Reference Van den Bergh, Mulder, Mennes and Glover2005, Reference Van den Bergh, van den Heuvel, Lahti, Braeken, de Rooij, Entringer, Hoyer, Roseboom, Räikkönen, King and Schwab2020). Substantial evidence indicates that stress exposure, maternal anxiety, and depression during pregnancy increase the risk for negative mental health outcomes in offspring across the life span (Betts et al., Reference Betts, Williams, Najman and Alati2014; Lafortune et al., Reference Lafortune, Laplante, Elgbeili, Li, Lebel, Dagenais and King2021; O’Donnell et al., Reference O'donnell, Glover, Barker and O'connor2014; Madigan et al., Reference Madigan, Oatley, Racine, Fearon, Schumacher, Akbari and Tarabulsy2018). Delineating pathways from prenatal maternal stress exposure to child outcomes, while accounting for ongoing maternal mental health, may be important for understanding psychological mechanisms of risk and resiliency. Prior research has shown that it is not only exposure to a stressful event in utero, but mothers’ subjective psychological response to the stressor, that can have meaningful and differential influences on child outcomes (Simcock et al., Reference Simcock, Elgbeili, Laplante, Kildea, Cobham, Stapleton, Austin, Brunet and King2017). This calls for rigorous, prospective research designs that consider connections between prenatal stress, perinatal maternal mental health problems, and early risk factors for developmental psychopathology risk in young children. The current study focuses on the associations between prenatal maternal exposure to a natural disaster and subsequent maternal mental health problems with infant temperament, an early indicator of developmental psychopathology (see Stifter & Dollar, Reference Stifter, Dollar and Cicchetti2016 for a review).
Prenatal stress exposure is associated with increased risk for maternal perinatal mental health symptoms including depression, anxiety, and posttraumatic stress (Brock et al., Reference Brock, O’Hara, Hart, McCabe, Williamson, Laplante, Yu and King2014; Harville et al., Reference Harville, Xiong and Buekens2010; Tees et al., Reference Tees, Harville, Xiong, Buekens, Pridjian and Elkind-Hirsch2010), which are associated with mental health risk in offspring (Chen et al., Reference Chen, Chen, Shi, Jiang, Li, Zhou and Chan2020; Lin et al., Reference Lin, Xu, Huang, Jia, Zhang, Yan and Zhang2017). The developing fetus is particularly vulnerable to environmental influences, including maternal psychopathology and exposure to stressful life events (Glover, Reference Glover2011; Van den Bergh et al., Reference Van den Bergh, Mulder, Mennes and Glover2005). In utero exposure to maternal psychological distress has long been associated with adverse socioemotional outcomes in offspring (DiPietro et al., Reference DiPietro, Voegtline, Pater and Costigan2018; Korja et al., Reference Korja, Nolvi, Grant and McMahon2017). Prenatal maternal stress, depression, anxiety, and posttraumatic stress symptoms have been associated with increased risk for infant negative emotional reactivity and lower self-regulation capacity (Bosquet Enlow et al., Reference Bosquet Enlow, Kullowatz, Staudenmayer, Spasojevic, Ritz and Wright2009, Reference Bosquet Enlow, Kitts, Blood, Bizarro, Hofmeister and Wright2011; Bush et al., Reference Bush, Jones-Mason, Coccia, Caron, Alkon, Thomas and Epel2017; Erickson et al., Reference Erickson, Gartstein and Dotson2017; Korja et al., Reference Korja, Nolvi, Grant and McMahon2017) which are both associated with later psychopathology risk (Clauss & Blackford, Reference Clauss and Blackford2012; De Pauw & Mervielde, Reference De Pauw and Mervielde2010; Rapee, Reference Rapee2014; Sayal et al., Reference Sayal, Heron, Maughan, Rowe and Ramchandani2014). Thus, maternal mental health problems that develop following exposure to a stressor in pregnancy may be one psychological mechanism that increases the risk for adverse infant socioemotional outcomes.
The fetal programming hypothesis provides a framework for understanding the pathways through which prenatal stress and subsequent maternal psychological responses influence fetal development and later mental health risk (Barker, Reference Barker1995; Seckl & Holmes, Reference Seckl and Holmes2007; see review Van den Bergh et al., Reference Van den Bergh, van den Heuvel, Lahti, Braeken, de Rooij, Entringer, Hoyer, Roseboom, Räikkönen, King and Schwab2020). Maternal distress and associated fluctuations in glucocorticoids may be passed from the mother to the fetus in utero, influencing offspring neurodevelopment and later stress reactivity (Kapoor et al., Reference Kapoor, Dunn, Kostaki, Andrews and Matthews2006; Weinstock, Reference Weinstock2005). In postnatal phases, this may manifest behaviorally and physiologically through measures of emotional reactivity and regulation in offspring (Bush et al., Reference Bush, Jones-Mason, Coccia, Caron, Alkon, Thomas and Epel2017; Van den Bergh et al., Reference Van den Bergh, van den Heuvel, Lahti, Braeken, de Rooij, Entringer, Hoyer, Roseboom, Räikkönen, King and Schwab2020).
The broad definition, conceptualization, and measurement of prenatal stress has created significant challenges to effectively studying its influences on offspring development. In current literature, measures of prenatal “stress” include exposure to a range of potentially stressful or traumatic events, objective hardship experienced, subjective distress or perceived stress, maternal mental health symptomology (i.e., anxiety, depression), or biological stress response functioning (e.g., cortisol). As Doyle and Cicchetti (Reference Doyle and Cicchetti2018) noted, this current conceptualization of prenatal stress often combines potential mediating or moderating processes with external stressors, which contributes to the complexity in understanding effects on development. Additionally, the causal effects of prenatal stress can be difficult to test in humans due to cross-sectional and correlational designs, confounding personal risk factors such as prior mental health history, and the heritability of maternal personality, mood, and other temperament characteristics. Sudden-onset natural disasters provide a unique opportunity to study a stressor that is independent of personal characteristics. They also offer a quasi-experimental design through which prospective, longitudinal effects of sudden-onset stress exposures, experienced at varying levels of severity, can be studied across a large geographic region. As such, natural disaster studies can help disentangle the effects of objective exposure to a stressor from subjective responses to it in pregnant women (King et al., Reference King, Dancause, Turcotte-Tremblay, Veru and Laplante2012). We aimed to examine the cascade of effects beginning from disaster-related hardships experienced by the mother during pregnancy to the development of maternal mental health problems and subsequent infant socioemotional outcomes.
Research groups have studied the longitudinal impact of prenatal maternal stress on child behavioral development in the context of several natural disasters, including the 1998 Quebec Ice Storm (King et al., Reference King, Dancause, Turcotte-Tremblay, Veru and Laplante2012; Laplante et al., Reference Laplante, Brunet and King2016; Walder et al., Reference Walder, Laplante, Sousa-Pires, Veru, Brunet and King2014), 2008 Iowa Floods (Nylen et al., Reference Nylen, O’Hara and Engeldinger2013; Yong Ping et al., Reference Yong Ping, Laplante, Elgbeili, Hillerer, Brunet, O'Hara and King2015), 2011 Queensland Flood (King et al., Reference King, Kildea, Austin, Brunet, Cobham, Dawson, Harris, Hurrion, Laplante, McDermott, McIntyre, O’Hara, Schmitz, Stapleton, Tracy, Vaillancourt, Dancause, Kruske, Reilly and Yong Ping2015; McLean et al., Reference McLean, Cobham, Simcock, Kildea and King2019; Simcock et al., Reference Simcock, Elgbeili, Laplante, Kildea, Cobham, Stapleton, Austin, Brunet and King2017), and the 2012 Superstorm Sandy in the New York metropolitan area (Finik & Nomura, Reference Finik and Nomura2017). A recent meta-analysis found modest but statistically significant effects of prenatal maternal stress from the experience of natural disasters on children’s cognitive, behavioral, motor, and socioemotional development (Lafortune et al., Reference Lafortune, Laplante, Elgbeili, Li, Lebel, Dagenais and King2021). In the context of disasters, researchers have assessed the effects of both the severity of disaster-related exposure or objective hardship (e.g., losing one’s belongings, lack of power/electricity, being evacuated, threat of death/injury, etc.) and subjective reactions (e.g., emotional distress, perceived stress, or posttraumatic stress symptoms) on children’s socioemotional outcomes. For example, higher levels of maternal posttraumatic stress symptoms, but not objective hardship, were associated with more difficult infant temperament characteristics, including increased fussiness, dullness, and need for attention in 6-month-old infants exposed to the 1998 Quebec Ice Storm in Canada (Laplante et al., Reference Laplante, Brunet and King2016) and 2005 Hurricane Katrina in the United States (Tees et al., Reference Tees, Harville, Xiong, Buekens, Pridjian and Elkind-Hirsch2010). However, research from a separate natural disaster study focusing on mothers affected by the 2012 US Atlantic Superstorm Sandy found conflicting results: objective hardship, but not maternal posttraumatic stress symptoms, predicted greater infant emotional reactivity and dysregulation (Buthmann et al., Reference Buthmann, Ham, Davey, Finik, Dana, Pehme, Zhang, Glover and Nomura2019). Alternatively, in a study of mothers exposed to the 2011 Australian Queensland Flood, researchers found that when mothers reacted with high subjective distress (operationalized as a composite score of posttraumatic stress and peritraumatic distress questionnaires) to low levels of objective hardship exposure, their infants displayed the highest levels of difficult activity-reactivity temperament traits (Simcock et al., Reference Simcock, Elgbeili, Laplante, Kildea, Cobham, Stapleton, Austin, Brunet and King2017). This highlights the importance of mothers’ subjective response to a stressor above and beyond the level of hardship experienced for influencing infant outcomes. Despite some conflicting evidence, the recent meta-analysis found that both maternal objective hardship and subjective distress had significant effect sizes (rs ∼ 0.07) on children’s socio development, including temperament (Lafortune et al., Reference Lafortune, Laplante, Elgbeili, Li, Lebel, Dagenais and King2021).
There are theoretical reasons to believe that maternal subjective distress should have greater effects on the unborn child than objective hardship. The stress model of Lazarus and Folkman (Reference Lazarus and Folkman1984) would suggest that the more severe the objective level of exposure to a potential stressor, the greater the subjective distress. A tenet of models of fetal programming (Barker, Reference Barker1990; Kwon & Kim, Reference Kwon and Kim2017) and the developmental origins of health and disease (DOHaD) (Gluckman et al., Reference Gluckman, Hanson and Buklijas2010) is that it is the distress that should activate the mother’s hypothalamic-pituitary-adrenal axis and secretion of glucocorticoids to the placenta which then programs the fetus, for better or for worse (Sandman et al., Reference Sandman, Davis and Glynn2012). Thus, the research that finds that objective hardship has significant effects, while subjective distress does not, is somewhat counterintuitive and suggests that mechanisms other than glucocorticoid transmission may be involved. The 2021 meta-analysis found that effect sizes were greater for objective hardship from the Quebec ice storm than for that from floods, which could be due to seasonal temperatures and effects of the cold. Furthermore, some studies, including Project Ice Storm, measure subjective distress in terms of symptoms associated with posttraumatic stress disorder; the fact that traumatic stress disorder symptoms tend to be associated with lower, rather than higher, levels of cortisol (Meewisse et al., Reference Meewisse, Reitsma, de Vries, Gersons and Olff2007), and the importance of having increasing levels of cortisol as parturition approaches, suggests that more research is required to better understand the specific roles of various components and mechanisms of maternal hardship and stress responses in fetal programming from natural disasters (St-Pierre et al., Reference St-Pierre, Laplante, Dawson, Kildea, King and Vaillancourt2018).
Existing literature has examined a developmental cascade of effects from prenatal stress exposure to maternal psychological reactions which then affect infant outcomes. The pathway from objective hardship to maternal mental health across pre- and postnatal periods may be a key mediating pathway to understanding individual variability in offspring risk and resilience (Hentges et al., Reference Hentges, Graham, Plamondon, Tough and Madigan2019; Moss et al., Reference Moss, Simcock, Cobham, Kildea, Elgbeili, Laplante and King2017). In addition to fetal programming theories, alternative hypotheses such as interpersonal models of stress transmission (Hammen et al., Reference Hammen, Shih and Brennan2004) and continuation of stress or mental health problems into the postpartum period (Hentges et al., Reference Hentges, Graham, Plamondon, Tough and Madigan2019) offer additional perspectives on how maternal stress and mental health influence child outcomes. Examining such pathways calls for prospective research designs that measure maternal and child outcomes over time following prenatal stress exposure.
The present study aims to integrate existing knowledge on the relations between prenatal stress and child outcomes by examining how objective hardship from a natural disaster during pregnancy prospectively influences infant temperament (negative affect, positive affect/surgency, orienting/regulating capacity) via maternal mental health symptoms (anxiety/depression and posttraumatic stress symptoms). Severe flooding from Hurricane Harvey significantly impacted Houston, Texas and surrounding areas in late August 2017 and had devastating material and financial impacts including displacing approximately 30,000 residents, costing over $125 billion in damages and killing approximately 88 people (Blake & Zelinsky, Reference Blake and Zelinsky2018). After the storm, women who were pregnant, or had been pregnant at the time of Hurricane Harvey, were recruited for the study. Mothers reported on their objective hardship resulting from the disaster as well as their subjective distress (conceptualized in this study as mental health symptoms of anxiety/depression and posttraumatic stress) at a baseline and postpartum assessment. Women also reported on offspring temperament at a postpartum assessment.
The current study examined pathways to infant temperament development from prenatal exposure to disaster-related objective hardship through maternal mental health symptoms (anxiety/depression and posttraumatic stress). Building on prior research (Buthmann et al., Reference Buthmann, Ham, Davey, Finik, Dana, Pehme, Zhang, Glover and Nomura2019; Laplante et al., Reference Laplante, Brunet and King2016; Moss et al., Reference Moss, Simcock, Cobham, Kildea, Elgbeili, Laplante and King2017; Tees et al., Reference Tees, Harville, Xiong, Buekens, Pridjian and Elkind-Hirsch2010), we hypothesized that maternal mental health symptoms would mediate the association between disaster-related objective hardship and infant temperament. Specifically, we hypothesized that greater exposure to objective hardship would predict higher levels of maternal mental health symptoms, which would in turn be associated with more difficult infant temperament characteristics (higher negative affect, lower positive affect/surgency, lower orientating/regulatory capacity).
Method
Study design and recruitment
This project is part of the Harvey Mom Study, a prospective longitudinal study investigating the effects of perinatal maternal stress associated with the 2017 Hurricane Harvey and subsequent flooding in Houston, Texas on early child development. Eligibility criteria for the Harvey Mom Study included women who were 18 years of age or older at the time of recruitment and: (1) lived in the greater Houston area during Hurricane Harvey (August 25, 2017); (2) were pregnant during Hurricane Harvey or became pregnant within 6 months after Hurricane Harvey; and (3) were English-speaking. Women who were pregnant with multiples were excluded. Recruitment began after receiving ethical approval from the University of Houston’s Institutional Review Board in February 2018 and continued through August 2018. For the present study, mothers exposed to Hurricane Harvey prior to conception were excluded.
Recruitment strategies included the distribution of flyers throughout the community, with a special emphasis on health clinics, pregnancy clinics, Women, Infants, and Children centers, social media engagement through Facebook advertisements, and postings in local mother groups and local news articles. Written, online informed consent was obtained from all eligible women for all study procedures. Data were collected and managed using REDCap electronic data capture tools hosted and supported by the Women and Children’s Health Research Institute at the University of Alberta. Mothers received compensation (Amazon gift cards) for participating in all study assessments. After removing all suspected bots and fraudulent participants, 1,017 women met eligibility criteria and completed baseline surveys (see Supplementary Figure 1) in the overall sample.
Assessment schedule
Mothers completed online research assessments at three separate time points. At the baseline assessment , mothers completed questionnaires about demographic information, objective hardship related to Hurricane Harvey, and their current mental health symptoms including posttraumatic stress and anxiety/depression symptoms. The initial baseline questionnaires were completed on average at 7.9 months after Hurricane Harvey (range = 5.7–11.9 months), which is comparable to starting points of prior studies examining prenatal stress in the context of large-scale disasters (Simcock et al., Reference Simcock, Elgbeili, Laplante, Kildea, Cobham, Stapleton, Austin, Brunet and King2017). Mothers were then randomized to a 4-day expressive writing intervention or control activity after which they completed a 2-month follow-up of mental health symptoms. Intervention effects were not observed for maternal mental health outcomes, as reported recently (Paquin et al., Reference Paquin, Bick, Lipschutz, Elgbeili, Laplante, Biekman and Olson2021). Mothers were invited to complete an additional online assessment when their infants reached 6 months of age. At this postpartum assessment, mothers reported on their infants’ development and temperament and on their own current levels of anxiety and depression symptoms, using the same measures from the baseline assessment. Infants ranged from 4.9 to 11.9 months of age at the postpartum assessment (M = 7.3 months, SD = 1.1); however, 81% of infants were in the range of 4.9–8.0 months of age. The variation in age at the postpartum assessment was due to participants who completed the surveys early (due to RedCap technical errors) or later than intended (due to continued follow-up for completion of surveys).
In the present study, our primary objective was to examine associations between disaster-related objective hardship, subsequent maternal mental health, and infant temperament. To maximize recruitment, eligible mothers could enroll in the study at any time during the recruitment window regardless of if they were currently pregnant or had already given birth. In 114 cases, mothers completed the baseline assessment and postpartum assessment within a 2-week period. As maternal assessments specifically asked about mental health symptoms that occurred over the past 2 weeks, these cases were excluded due to the likely overlap in symptom reporting across time points. The final sample size for analyses was N = 527. The average time between baseline and postpartum assessments was 100.6 days (SD = 73.2). See Table 1 for additional descriptive data on time variables and Supplementary Figure 1 for descriptions of sample size and exclusions at each time point.
Table 1. Descriptive statistics for demographic and key study variables (N = 527)
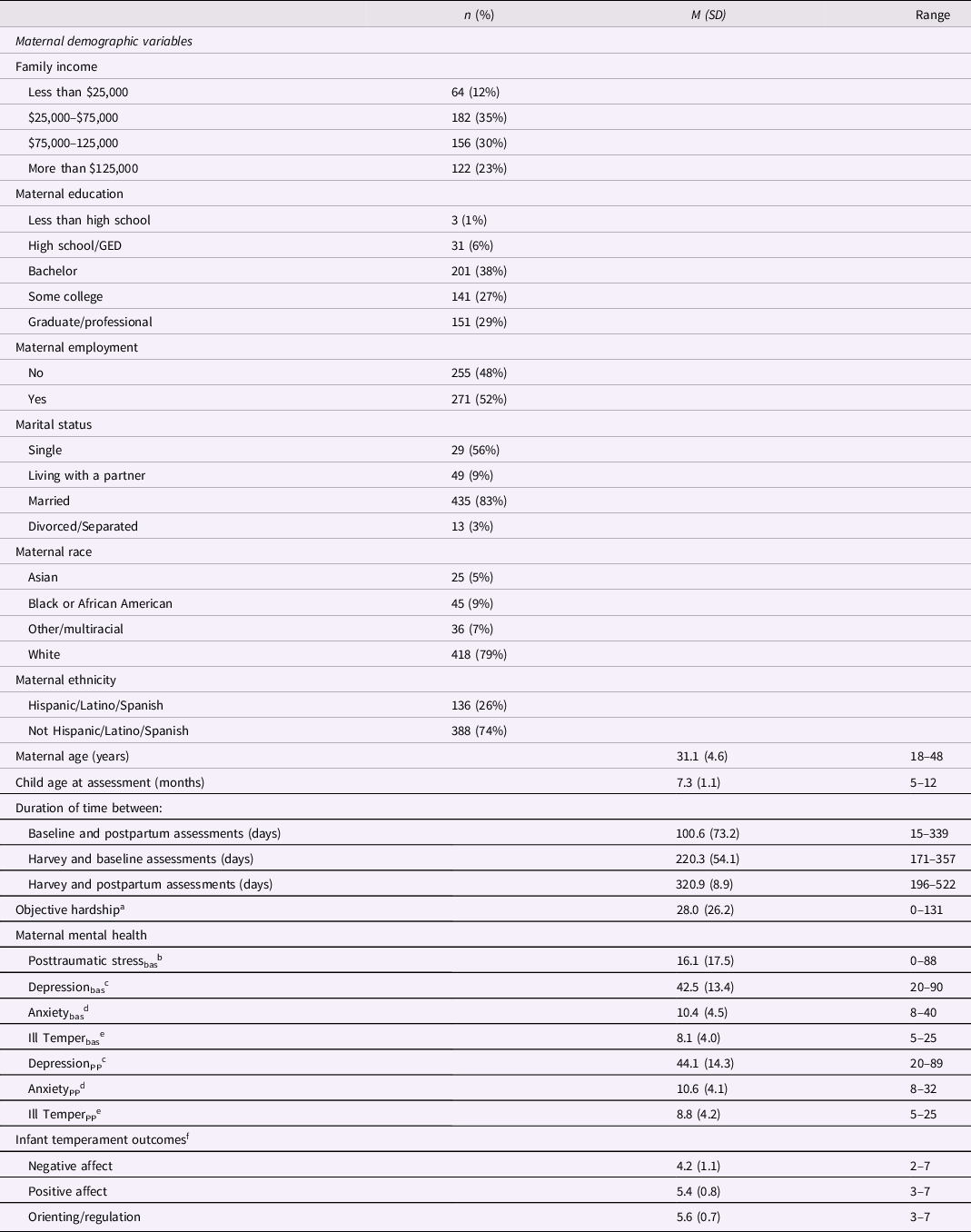
Notes. aUntransformed scores are used for objective hardship descriptive statistics. bImpact of Event Scale-Revised (IES-R). Scores on the IES-R ≥ 33 indicate clinically significant PTSD symptoms. cInventory of Depression and Anxiety Symptoms (IDAS) General Depression subscale. dIDAS Panic subscale. eIDAS Ill-Temper subscale. fInfant Behavior Questionnaire-VSF subscales. Bas = baseline assessment. PP = postpartum assessment.
Sample characteristics
Mothers reported their demographic information at the baseline assessment (Table 1). Of the mothers included in this sample, 42% (n = 221) of the sample were exposed to Hurricane Harvey during the third trimester, 28% (n = 148) during the second trimester, and 29% (n = 154) during the first trimester. At the baseline assessment, 13% of mothers were still pregnant.
Attrition analyses
We tested differences in baseline demographic characteristics between mothers that completed postpartum assessments and those who had missing data due to attrition. Mothers that completed the postpartum assessment reported higher income X 2 (3,1017) = 8.93, p = .03, and education levels, X 2 (3, 1017) = 19.90, p < .001, lower objective hardship from Harvey, t(617) = −3.76, p < .001, and lower depression t(657) = −2.33, p = .02, anxiety, t(573) = −3.30, p = .001, and posttraumatic stress, t(657) = −2.72, p = .01, symptoms at baseline than mothers who did not complete the postpartum assessment. There were no statistically significant differences in ethnicity, X 2 (1, 1017) = 1.71, p = .19, employment status, X 2 (1, N = 1,017) = 0.62, p = .43, or race, X 2 (3, 1013) = 5.95, p = .11.
Measures
Sociodemographic factors and pregnancy factors
Sociodemographic factors including maternal age, education level, family income level, maternal employment, marital status, race, and ethnicity were collected via maternal report online at baseline. Maternal education was reported on a five-point scale ranging from 1 (less than High school education) to 5 (Graduate/Professional degree). Family income was reported on a nine-point scale ranging from 1 (less than $10,000) to 9 (above $200,000). Mothers reported their ethnicity as Hispanic or Non-Hispanic, and racial background as White, Asian, Black, Other, or Multiracial. Due to small sample sizes across Asian, Black, and Other/Multiracial race categories, racial background was collapsed across these categories into one group (People of color) for further analyses. Stressful life events were assessed by the Life Events Questionnaire (Sarason et al., Reference Sarason, Johnson and Siegel1978). Timing of prenatal exposure to Hurricane Harvey (trimester and days since conception) was calculated from reported due dates and dates of birth. Mothers reported their infants’ birth weight, gestational age, current age, and sex at the postpartum assessment.
Infant temperament
The Infant Behavioral Questionnaire Revised Very Short Form (IBQ-VSF; Putnam et al., Reference Putnam, Helbig, Gartstein, Rothbart and Leerkes2014), a widely used parent-report measure of infant temperament, was administered at the postpartum assessment. The IBQ-VSF has been validated in samples of infants from 3 to 12 months of age. Ten participants who completed the IBQ when their child was older than 12 months, were excluded from analyses (see Supplementary Figure 1). The IBQ consists of 37 items and three subscales including Negative Affect (NEG; sadness, distress to limitations, fear, and falling reactivity), Positive Affect/Surgency (PAS; approach, vocal reactivity, high-intensity pleasure, smiling and laughter, activity level, perceptual sensitivity), and Orienting/Regulating Capacity (ORC; low-intensity pleasure, cuddliness, duration of orienting, and soothability). Mothers reported on the frequency of infant behaviors over the past week on a seven-point Likert scale from 1 (never) to 7 (always). Consistent with established scoring guidelines, items that were coded 0 (does not apply) were treated as missing. A mean score was calculated for each scale based on the original conceptualization of each factor (Putnam et al., Reference Putnam, Helbig, Gartstein, Rothbart and Leerkes2014). Higher scores on a given subscale indicated that mothers reported higher levels of that temperament domain. Each subscale demonstrated adequate internal consistency (Cronbach’s alphas were as follows: PAS = .73, NEG = .80, ORC = .79). In prior research, the IBQ-VSF has demonstrated adequate test-retest reliability, internal consistency, and interrater agreement (Putnam et al., Reference Putnam, Helbig, Gartstein, Rothbart and Leerkes2014) and established reliability in samples that vary on race and socioeconomic status (Leerkes et al., Reference Leerkes, Su, Reboussin, Daniel, Payne and Grzywacz2017).
Maternal mental health symptoms
Posttraumatic stress symptoms
The 22-item Impact of Event Scale-Revised (Weiss, Reference Weiss2007; IES-R), a well-validated measure of posttraumatic stress symptoms, was administered at baseline to assess disaster-related trauma symptoms. Mothers reported on their distress related to the flood over the past 7 days on items with a 5-point Likert scale from 0 (not at all) to 4 (extremely). The 22-item IES-R includes three subscales of posttraumatic stress symptoms including avoidance, intrusion, and hyperarousal (Weiss, Reference Weiss2007). Higher scores on each of these subscales indicate higher levels of posttraumatic stress symptoms. Summed scores on each of these subscales were used as measured indicators of the posttraumatic stress latent variable. Internal consistency across subscales was high (Cronbach’s alphas = .92–.95).
Maternal anxiety/depression symptoms
Maternal anxiety/depression symptoms were measured with an abridged version of the Inventory of Depression and Anxiety Symptoms (IDAS-II; Watson et al., Reference Watson, O’Hara, Simms, Kotov, Chmielewski, McDade-Montez, Gamez and Stuart2007) at baseline and the postpartum assessment. The IDAS-II was designed to broadly assess symptom dimensions underlying depression and anxiety disorders (Watson et al., Reference Watson, O’Hara, Naragon-Gainey, Koffel, Chmielewski, Kotov, Stasik and Ruggero2012). Symptoms were rated for the preceding 2 weeks on a five-point Likert scale from 0 (not at all) to 4 (extremely). In consultation with one of the original authors of the IDAS-II, Michael O’Hara, the IDAS-II was shortened to 40 items reflecting 4 of the 10 factors from the original principal factor analysis of the IDAS-II that was conducted in a sample of postpartum women (Watson et al., Reference Watson, O’Hara, Simms, Kotov, Chmielewski, McDade-Montez, Gamez and Stuart2007): 20 depression items, 9 anxiety/panic items, 5 ill temper items, as well as 6 reverse-coded items reflecting well-being. Subscales for each of these factors were created as sum scores. Higher subscale scores indicate higher levels of depression, anxiety/panic, or ill temper symptoms. The Depression, Anxiety/Panic, and Ill Temper scales have shown strong intercorrelations, factor loadings, and associations with depression and anxiety diagnoses in previous psychometric research (Watson et al., Reference Watson, O’Hara, Simms, Kotov, Chmielewski, McDade-Montez, Gamez and Stuart2007). Irritability (measured here through the Ill Temper scale), is a common symptom in individuals with depression and anxiety disorders (Fava et al., Reference Fava, Rush, Alpert, Carmin, Balasubramani, Wisniewski, Trivedi, Biggs and Shores-Wilson2006, Reference Fava, Hwang, Rush, Sampson, Walters and Kessler2010), and an important indicator of depressed mood in postpartum women (Williamson et al., Reference Williamson, O'Hara, Stuart, Hart and Watson2015). Items related to irritability are included in several well-validated measures of depression (i.e., Beck Depression Inventory, Zung Self-Rating Depression Scale). Thus, we selected the Depression, Anxiety/Panic, and Ill Temper subscales as indicators for a latent variable of Anxiety/Depression. The IDAS-II and its subscales have excellent internal consistency, strong short-term stability, display excellent convergent validity and good discriminant validity in comparison to other self-report and interview-based measures of depression and anxiety (Watson et al., Reference Watson, O’Hara, Simms, Kotov, Chmielewski, McDade-Montez, Gamez and Stuart2007). For the current sample, internal consistency across time points was high (Cronbach’s alphas = .93–.95).
Hurricane Harvey-related objective hardship
Mothers’ flood-related objective hardship was reported retrospectively at baseline using a questionnaire similar to that used by our team in previous disaster-related prenatal maternal stress research (King et al., Reference King, Kildea, Austin, Brunet, Cobham, Dawson, Harris, Hurrion, Laplante, McDermott, McIntyre, O’Hara, Schmitz, Stapleton, Tracy, Vaillancourt, Dancause, Kruske, Reilly and Yong Ping2015; King & Laplante, Reference King and Laplante2005) that was modified specifically for Hurricane Harvey. Items were written in objective terms and assessed four key dimensions of flood exposure: threat (e.g., personal injury), loss (e.g., loss of personal income), scope (e.g., days were you without electricity), and change (e.g., time spent in a temporary shelter). Although most questions assessed hardship that occurred at the time of the flood, some questions may have captured the continued stress that mothers experienced after the storm, such as financial stress or displacement. A committee of researchers assigned items to categories and assigned point values to items and to their possible responses to reflect relative weights of hardship following discussions until consensus was reached. Each dimension was made to have a possible total of 50 points such that total scores could range from 0 to 200, and higher scores indicated higher levels of flood-related hardship. The objective hardship variable was negatively skewed; thus, data were square root transformed for statistical analyses.
Covariates
Pearson correlations, t tests, and ANOVAs were used to identify maternal and child factors that might influence infant outcomes. Variables that were associated with each temperament outcome at p < .10 were included as covariates in subsequent mediation models. The following variables were considered as potential covariates: number of stressful life events since the child was born, maternal age, timing of prenatal exposure to Hurricane Harvey, pregnancy status at baseline assessment (0-not pregnant, 1-pregnant), maternal education, family income, ethnicity (0-Hispanic, 1-Non-Hispanic), race (0-People of color, 1-White), child sex (0-male, 1-female), birth weight, gestational age, child age at assessment. The writing intervention group was also considered as a covariate (0-Expressive Writing, 1-Control Writing, 2-No Writing Control). The following covariates met inclusion criteria for primary analyses: race, pregnancy status, and child age. Socioeconomic factors were not correlated with infant outcomes; however, they were significantly correlated with maternal mental health variables. Thus, to control for variability in the effects of the hurricane by socioeconomic status, income and maternal education were included as covariates of maternal mental health mediator variables. Additionally, maternal anxiety/depression reported at the time of the postpartum assessment was included to control for any statistical effect of concurrent maternal mood on mothers’ report of infant temperament. Time-related covariates that accounted for the number of days between Hurricane Harvey and the date of data collection for each participant at each time point were also included. Associations between all potential covariates, maternal mental health variables, and infant outcomes are presented in Supplementary Table 1.
Data analytic plan
As a part of preliminary analyses, we computed descriptive statistics and bivariate correlations in R (version 3.5, R Core Team, 2021) using the jmv package (Selker et al., Reference Selker, Love and Dropmann2020). To examine the indirect and direct effects between flood-related objective hardship, maternal mental health symptoms, and infant temperament outcomes, structural equation modeling was conducted in Mplus 8.5 software (Muthén & Muthén, Reference Muthén and Muthén2017).
Measurement modeling was conducted first to construct separate latent variables for maternal posttraumatic stress and anxiety/depression. Model fit was examined with subscales used as the indicator for each variable. After establishing adequate fit for each latent variable, results of these measurement models were used to inform specification of structural model. We relied on factor and residual correlations, chi-square corresponding p-value, and commonly used fit statistics (including RMSEA, CFI, TLI, SRMR) to evaluate model fit. Next, a structural model was specified to investigate the direct and indirect effects (via baseline maternal anxiety/depression and posttraumatic stress) between objective hardship and infant temperament. As shown in Figure 1, objective hardship was modeled to predict the mediators (baseline maternal anxiety/depression and posttraumatic stress), and outcomes (infant negative affect, positive affect, orienting/regulatory capacity). Residuals associated with latent variable mediators at the same time point (anxiety/depression and posttraumatic stress symptoms) were allowed to covary (Preacher & Hayes, Reference Preacher and Hayes2008). Consistent with best practices, residual covariances were also estimated between identical measurements across time (Marsh et al., Reference Marsh, Morin, Parker and Kaur2014). Missing data were handled with full information maximum likelihood. Model fit was evaluated using established goodness of fit criteria for reasonably fitting models (RMSEA < .06; CFI > .90; TLI > .90, SRMR < .08) and for well-fitting models (RMSEA < .05; CFI > .95; TLI > .95, SRMR < .05; Hu & Bentler, Reference Hu and Bentler1999).

Figure 1. Standardized path coefficients for the structural model from maternal objective hardship to infant temperament. Bolded lines represent significant direct and indirect paths. Dashed lines represent non-significant paths. * p < .05, ** p < .01, *** p < .001. Statistically significant indirect effects were observed through Objective hardship → Posttraumatic stress → Orienting/Regulation, 95% CI [.009, .133], and Objective hardship → Anxiety/Depressionbas → Anxiety/DepressionPP → Negative Affect, 95% CI [.018, .079]. Dep = IDAS General Depression scale, Anx = IDAS Panic scale, Tem = IDAS Ill Temper scale. Int = IES-R Intrusion scale, Hyp = IES-R Hyperarousal scale, Avo = IES-R avoidance scale. Bas = baseline assessment. PP = Postpartum assessment. The covariates are not shown in the figure.
To address the primary study hypotheses, we examined the indirect effects of objective hardship on infant temperament outcomes through maternal posttraumatic stress and anxiety/depression symptoms at the baseline assessment, while controlling for mothers’ anxiety/depression symptoms at the postpartum assessment. Secondary post hoc analyses examined the indirect effects of objective hardship on infant temperament through mothers’ anxiety/depression symptoms at the baseline and postpartum assessments. Bootstrapped bias-corrected confidence intervals (5000 iterations) were used to estimate indirect effects (Preacher & Hayes, Reference Preacher and Hayes2004) and mediation was inferred if the 95% confidence intervals for the indirect effects did not include zero (Hayes, Reference Hayes2015). Following Hayes and Rockwood (Reference Hayes and Rockwood2017) recommendations for modern mediation analysis, both mediators (baseline anxiety/depression and posttraumatic stress) were included in one parallel multiple mediator model. Fully standardized estimates of indirect effects are reported in Table 3 and indicate the magnitude of the indirect effect in terms of standard deviations of the dependent and independent variables (Miočević et al., Reference Miočević, O’Rourke, MacKinnon and Brown2018). Proportion of total effect mediated is also reported for significant indirect effects.
Results
Bivariate analyses
Table 2 includes Pearson-product correlations between key study variables and sociodemographic variables. There were significant associations between objective hardship and all infant temperament outcomes such that greater objective hardship predicted higher infant negative affect (r = .09, p = .05), positive affect (r = .10, p = .02), and orienting regulatory capacity (r = .10, p = .03). Objective hardship was significantly correlated with higher total maternal posttraumatic stress (r = .48, p < .001), depression (r = .38, p < .001), anxiety/panic (r = .25, p < .001), and ill temper (r = .30, p < .001) symptoms at baseline, and with depression (r = .27, p < .001), and anxiety/panic (r = .22, p < .001), and ill temper (r = .20, p < .001) symptoms at the postpartum assessment. Maternal depression and ill temper at baseline were correlated with infant negative affect (r = .11, p = .01, r = .10, p = .02 respectively), but not with infant positive affect or orienting regulatory capacity. Baseline maternal posttraumatic stress symptoms were positively correlated with infant negative affect (r = .10, p = .03), positive affect (r = .09, p = .03), and orienting/regulatory capacity (r = .12, p = .01). At the postpartum assessment, all three measured Inventory of Depression and Anxiety Symptoms (IDAS) subscales were significantly correlated with infant negative affect (depression, r = .18, p < .001; anxiety/panic, r = .13, p = .002; ill temper, r = .17, p < .001) but not with infant positive affect or orienting regulatory capacity.
Table 2. Bivariate correlations between key study variables and covariates
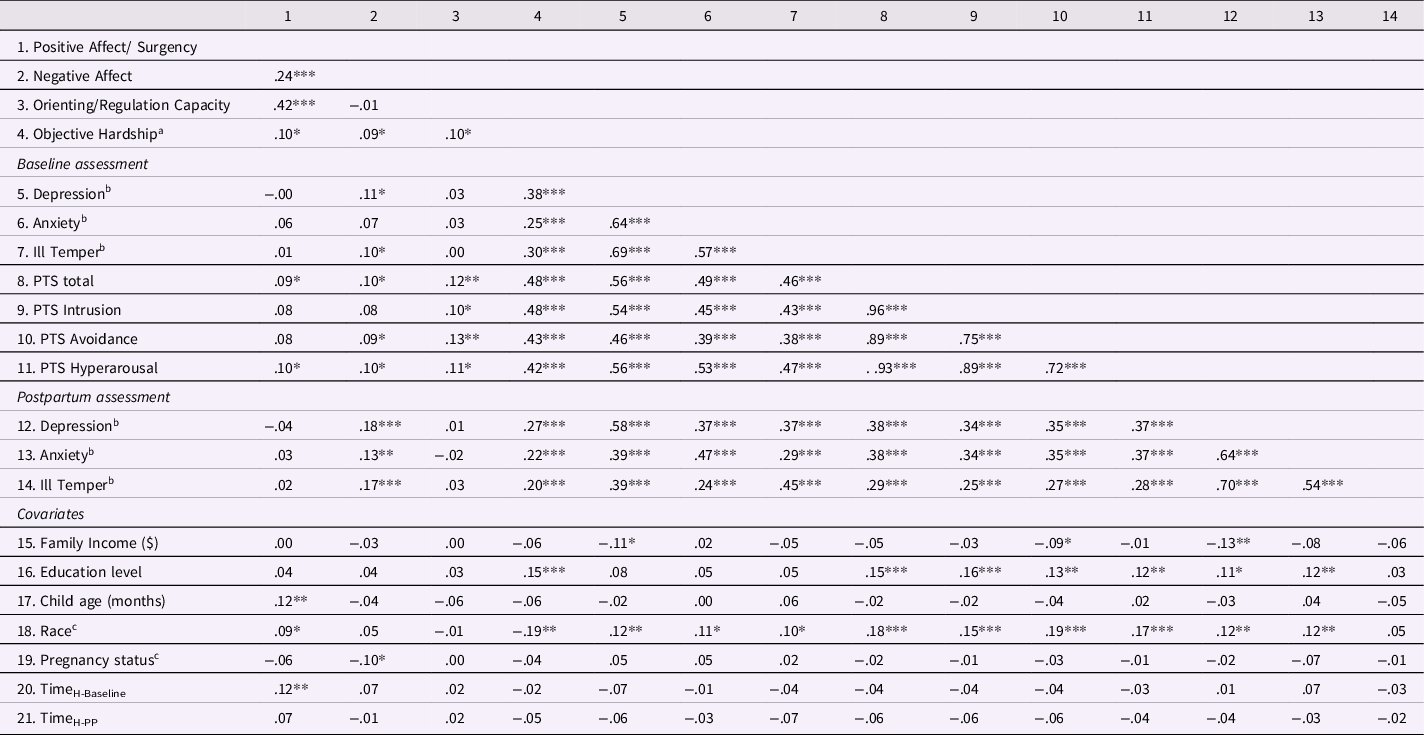
Notes. *p < .05, **p < .01, ***p < .001, Subscale averages are used for Negative Affect, Orienting/Regulation Capacity, Positive Affect/Surgency. Subscale sum scores are used for maternal mental health variables. aTransformed scores are used for objective hardship. bmeasured with Inventory of Depression and Anxiety Symptoms subscales. cpoint biserial correlation coefficients used for binary variables; race: 0-White, 1-People of color; Pregnancy status: 0-Not pregnant at baseline, 1-Pregnant at baseline. PTS = posttraumatic stress symptoms measured with IES-R. Time variables are calculated as the number of days between Harvey (Aug 25, 2017) and the assessment date of completion for each participant. PP = Postpartum assessment.
Table 3. Parameter estimates for direct effects of disaster-related objective hardship and maternal mental health on infant temperament
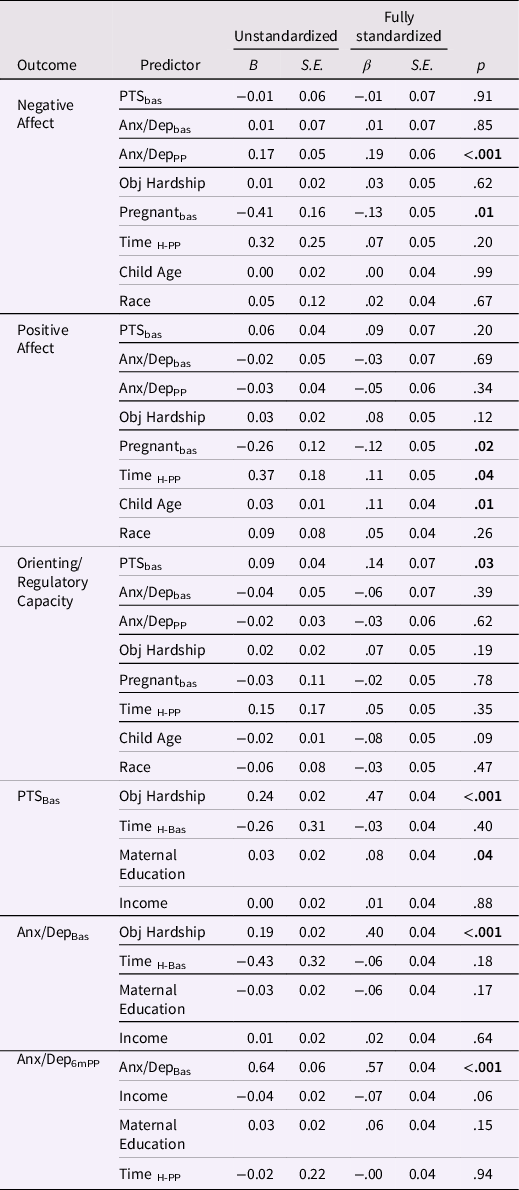
Note. Unstandardized and standardized parameter estimated are reported. Significant direct paths are bolded. SE = standard error. Bas = baseline assessment. PP = postpartum assessment. PTS = Posttraumatic Stress symptoms. Anx/Dep = Anxiety/Depression symptoms. Time variables measured days from Hurricane Harvey to participant assessment date. Race: 0-White, 1-People of color; Pregnancy status: 0- Not pregnant at baseline, 1-Pregnant at baseline.
Measurement model
A measurement model was estimated with posttraumatic stress and anxiety/depression latent variables included together. A one factor anxiety/depression latent variable was estimated from the three measured IDAS subscales (general depression, anxiety/panic, ill temper) at each time point. The IDAS scales have been shown to define a single underlying psychopathology factor rather than separate anxiety and depression factors (Watson et al., Reference Watson, O’Hara, Simms, Kotov, Chmielewski, McDade-Montez, Gamez and Stuart2007), and thus were modeled as a single factor. A posttraumatic stress latent variable was estimated from the three subscales of the Impact of Event Scale-Revised (IES-R) according to a previous conceptualization of the measure in a community sample with varying levels of traumatic stress symptoms (Creamer et al., Reference Creamer, Bell and Failla2003). Covariances were estimated between identical measurements across time (i.e., same IDAS subscales at baseline and postpartum assessments; Marsh et al., Reference Marsh, Morin, Parker and Kaur2014) and maternal mental health variables at the same time point (baseline posttraumatic stress and anxiety/depression). The measurement model demonstrated a good fit, χ2 (21) = 67.50, p < .001, RMSEA = .07, CFI = .99, TLI = .98, SRMR = .03. All factor loadings of the measured variables on the latent variables were statistically significant (all p values < .001, see Figure 1).
Structural model for testing mediated effects
The structural model was estimated as shown in Figure 1. Maternal education and income were included as covariates of maternal anxiety/depression and posttraumatic stress symptoms. Time between Hurricane Harvey and assessment date was included as a covariate for all mental health and infant temperament variables. Maternal race, pregnancy status at baseline, and child age were included as covariates of infant temperament outcomes. The model also controlled for maternal anxiety/depression symptoms at the postpartum assessment. The structural model showed a good fit to the data, χ2 (117) = 201.23, p < .001, RMSEA = .04, CFI = .98, TLI = .97, SRMR = .04. Unstandardized and standardized estimates of direct effects are shown in Table 3. Standardized estimates of significant direct effects are also shown in Figure 1.
Results of the structural model indicated significant total effects (direct + indirect) between objective hardship and infant positive affect (β = .10, p = .04) and orienting/regulatory capacity (β = .10, p = .03) but not negative affect (β = .70, p = .09).
The direct effects between objective hardship and infant temperament outcomes were no longer significant after accounting for associations with maternal mental health and covariates (see Table 3). Objective hardship was significantly associated with higher levels of maternal anxiety/depression (β = .40, p < .001) and posttraumatic stress symptoms (β = .47, p < .001) at the baseline assessment. Greater maternal posttraumatic stress symptoms at baseline were associated with higher infant orienting and regulatory capacity scores (β = .14, p = .03) but not infant negative affect (β = −.01, p = .91), or positive affect (β = .09, p = .20) at the postpartum assessment. Maternal anxiety/depression symptoms at baseline did not significantly predict any infant temperament outcomes (see Table 3). Maternal anxiety/depression symptoms at the postpartum assessment were significantly associated with higher infant negative affect (β = .19, p = .001) at the same assessment, but were not associated with infant orienting and regulatory capacity (β = −.02, p = .73) or positive affect (β = −.04, p = .43).
Indirect effects
Standardized estimates for the bootstrapped bias-corrected 95% confidence intervals estimated with 5000 samples for the indirect effects of objective hardship on infant temperament outcomes through baseline maternal posttraumatic stress and anxiety/depression are summarized in Table 4. There was a significant indirect path from objective hardship to orienting and regulatory capacity through posttraumatic stress (95% CI [.01, .13]) indicating that higher objective hardship was associated with higher maternal posttraumatic stress symptoms, which in turn were associated with greater infant orienting/regulatory capacity. Standardized indirect effects indicate that a one standard deviation increase in objective hardship resulted in an increase of .07 standard deviations in orienting/regulatory capacity scores via maternal posttraumatic stress. The indirect effect through posttraumatic stress accounted for 68% of the total effect of objective hardship on infant orienting/regulatory capacity. None of the 95% confidence intervals for the indirect effects from objective hardship to negative affect and positive affect through posttraumatic stress and baseline anxiety/depression were considered statistically significant (95% confidence intervals included zero). Primary mediation analyses focused on indirect pathways through baseline maternal mental health symptoms (reported prior to infant temperament) to establish temporal precedence.
Table 4. Indirect effects of objective hardship through maternal mental health symptoms on infant temperament outcomes
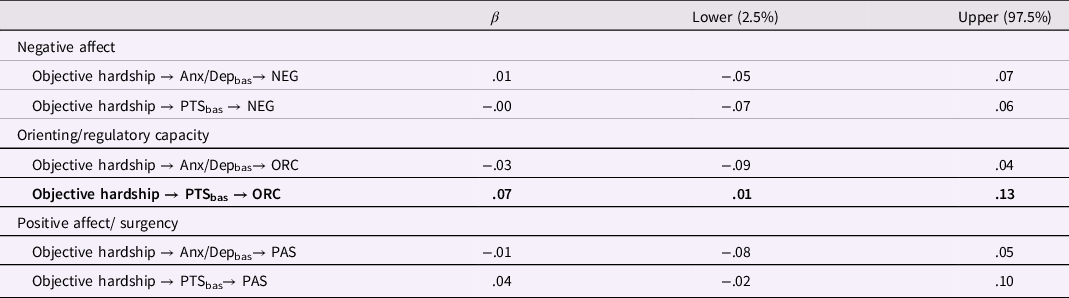
Notes. Standardized results for the estimates and bias-corrected 95% confidence intervals estimated with 5000 bootstrap samples for the indirect effects. Statistically significant indirect paths (95% confidence internals that do not include zero) are bolded. Objective hardship = Harvey Objective Hardship Scale. NEG = Negative Affect. ORC = Orienting/Regulatory Capacity.
PAS = Positive Affect/Surgency. Anx/Depbas = Anxiety depression at baseline. PTSbas = posttraumatic stress symptoms at baseline.
In post hoc analyses, we explored indirect pathways through concurrent maternal anxiety/depression reported at the postpartum assessment. Specifically, indirect pathways from objective hardship to infant negative affect were tested given the significant association between maternal anxiety/depression at the postpartum assessment and infant negative affect. Indirect pathways to positive affect and orienting regulatory capacity were not examined due to a lack of association with maternal anxiety/depression at the postpartum assessment. The indirect effect from objective hardship to negative affect through maternal anxiety/depression at baseline and then through anxiety/depression at the postpartum assessment was significant, 95% CI [.02, .08]. The indirect effect from objective hardship to negative affect only through maternal anxiety/depression at the postpartum assessment was not significant, 95% CI [−.004, .04]. Taken together, this suggests that maternal anxiety/depression at the baseline or postpartum assessments was not an independent mediator of the association between objective hardship and infant negative affect, but that the cascading effect of maternal anxiety/depression across the two time points (baseline and postpartum assessments) partially explained this association. This indirect effect through maternal anxiety/depression at baseline and postpartum assessments accounted for 53% of the total effect of objective hardship on infant negative affect. Higher objective hardship was associated with higher maternal anxiety/depression at baseline, which predicted higher maternal anxiety/depression at the postpartum assessment, which in turn was associated with higher infant negative affect scores.
Discussion
In this study, the associations among prenatal maternal objective hardship, maternal mental health symptoms, and infant temperament outcomes were examined in a sample of mothers who were exposed to Hurricane Harvey during pregnancy. Mediation analyses were used to address study hypotheses that exposure to prenatal objective hardship from a natural disaster would be indirectly associated with infant temperament through higher levels of maternal mental health symptoms. Our findings suggest that maternal mental health symptoms may be an indirect mechanism linking prenatal disaster exposure with specific offspring temperamental characteristics.
Notably, we found that higher levels of objective hardship predicted higher levels of infant orienting/regulatory capacity via higher maternal posttraumatic stress symptoms. In contrast to our hypotheses, we did not find indirect effects from objective hardship to the other two temperament scales (positive affect/surgency and negative affect) through maternal posttraumatic stress symptoms in the full model accounting for covariates (infant age, race, pregnancy status, concurrent maternal anxiety/depression symptoms). Differences in findings between orienting/regulation versus negative affect and positive affect/surgency may be related to interactions amongst temperament traits. Regulation includes the capacity to modulate emotional affect and reactivity, and psychometric studies of the Infant Behavior Questionnaire have shown an inverse relationship between orienting/regulation and negative affect (Castro Dias et al., Reference Castro Dias, Costa, Pinto and Figueiredo2021; Leerkes et al., Reference Leerkes, Su, Reboussin, Daniel, Payne and Grzywacz2017). Thus, infants of mothers with higher posttraumatic stress symptoms and higher orienting/regulation capacity may also exhibit patterns of lower negative affect and reactivity. The lack of association with negative affect and positive affect/surgency could also be explained by unmeasured factors such as parenting, biological correlates, or potential protective factors that exerted buffering effects.
Interestingly, more disaster-related objective hardship was indirectly related to higher levels of infant orienting/regulation capacity via increased maternal posttraumatic stress symptoms. Higher levels of regulation and orienting are considered adaptive temperamental traits and precursors to better effortful control in early childhood (Hill-Soderlund & Braungart-Rieker, Reference Hill-Soderlund and Braungart-Rieker2008). Although surprising that greater maternal stress was linked with a positive outcome, prior research has observed associations between higher maternal subjective distress and higher levels of engagement in orienting (Lin et al., Reference Lin, Crnic, Luecken and Gonzales2014) and cooperation-manageability (Simcock et al., Reference Simcock, Elgbeili, Laplante, Kildea, Cobham, Stapleton, Austin, Brunet and King2017) behaviors in infants. Our results contrast with findings in extant literature that greater maternal pregnancy stress and postpartum stress are associated with lower regulation in offspring (Bush et al., Reference Bush, Jones-Mason, Coccia, Caron, Alkon, Thomas and Epel2017; Buthmann et al., Reference Buthmann, Ham, Davey, Finik, Dana, Pehme, Zhang, Glover and Nomura2019). Orienting behaviors are fundamental to the development of self-regulation and measure infants’ capacity to direct attention toward or away from distressing objects in the environment (Ruff & Rothbart, Reference Ruff and Rothbart2001). One explanation for this finding is that the neurodevelopmental adaptions from exposure to prenatal stress in utero may have primed infants to be more attentive to their environment, suggesting a potential adaptive strategy to both attend to or disengage from stressors (Sandman et al., Reference Sandman, Davis and Glynn2012).
The observed indirect effect via maternal posttraumatic stress symptoms indicates that higher levels of orienting/regulation were not fully explained by just exposure to increased hardship from a stressor, but that the variability in mothers’ subjective responses, either in pregnancy or postpartum (87% of mothers had given birth by baseline) also explained the development of increased orienting/regulation capacity in infants. These findings may be understood in the context of the predictive-adaptive-response model (Gluckman et al., Reference Gluckman, Hanson and Spencer2005; Sandman et al., Reference Sandman, Davis and Glynn2012), which suggests that under certain conditions, exposure to stress in utero may confer an adaptive advantage if offspring experience stress later in development compared to a more favorable postnatal environment. Prior research has shown that the congruence and stability between the prenatal and postnatal environments may be important in preparing infants to survive and thrive early in development (Sandman et al., Reference Sandman, Davis and Glynn2012). However, as there were both pregnant and postpartum mothers at the time of mental health assessment, it could not be determined if the observed effects of maternal mental health were specific to either time period. The overall pattern of results remained the same when including only the mothers who had given birth at baseline, but unfortunately, the sample size of the mothers pregnant at baseline group was too small to allow for direct comparison. These findings suggest that it is not only the exposure or hardship experienced in utero that predicted later child socio development, but also the effects of that hardship on mothers’ subjective response and subsequent mental health symptoms that play a role in early temperament development.
This finding may also be understood in the context of existing parental posttraumatic stress literature. In our sample, assessment of posttraumatic stress symptoms at the baseline assessment was at least 6 months after the hurricane; although posttraumatic stress symptoms are to be expected in the first days and weeks after a disaster, there could be genetic and/or pre-existing characteristics that are associated with individuals who experience persistent posttraumatic stress symptoms in response to trauma (Pitman, Reference Pitman2006; Shin et al., Reference Shin, Bush, Milad, Lasko, Brohawn, Hughes, Macklin, Gold, Karpf, Orr, Rauch and Pitman2011; VanElzakker et al., Reference VanElzakker, Felicione, Staples-Bradley, Panic, Dubois, Lasko, Shomstein, Pitman, Orr and Shin2020). For example, 5–6 months following the 1998 Quebec ice storm, greater maternal posttraumatic stress symptoms were associated with lower, not higher, diurnal maternal cortisol (King et al., Reference King, Mancini-Marïe, Brunet, Walker, Meaney and Laplante2009). This finding is further extended in other literature demonstrating associations between parental posttraumatic stress disorder and low offspring cortisol levels (Yehuda & Bierer, Reference Yehuda and Bierer2008). These studies suggest a possible biological mechanism of intergenerational transmission of traumatic stress via alterations in cortisol levels. Our finding that the association between baseline posttraumatic stress symptoms and infant orienting and regulatory control is similar whether the posttraumatic stress symptoms are assessed during pregnancy or in the post partum period supports the idea that there is something unique about mothers who have persistent posttraumatic stress symptoms. The biological mechanisms of intergenerational transmission of traumatic stress are likely complex and beyond the scope of this paper, however, they may help explain differences in mothers who have persistent posttraumatic stress symptoms who then pass on some of those characteristics to their children.
Primary results did not find significant indirect effects through maternal anxiety/depression at baseline on any infant temperament outcome. However, post hoc analyses indicated a significant serial indirect effect from objective hardship to infant negative affect when maternal anxiety/depression at baseline and postpartum assessments were included (objective hardship → anxiety/depressionbas → anxiety/depressionPP → negative affect). This echoes existing research that has established links between maternal depression and increased infant negative affect (e.g., Feldman et al., Reference Feldman, Granat, Pariente, Kanety, Kuint and Gilboa-Schechtman2009; McMahon et al., Reference McMahon, Barnett, Kowalenko, Tennant and Don2001; Spry et al., Reference Spry, Aarsman, Youssef, Patton, Macdonald, Sanson, Thomson, Hutchinson, Letcher and Olsson2020; Whiffen & Gotlib, Reference Whiffen and Gotlib1989), and recent models that suggest cascading effects of maternal depression on negative affect across the first year of life (Rigato et al., Reference Rigato, Stets, Bonneville-Roussy and Holmboe2020). Increased maternal depression and infant negative affect are both associated with behavioral problems later in childhood (Cents et al., Reference Cents, Diamantopoulou, Hudziak, Jaddoe, Hofman, Verhulst and Tiemeier2013; Lawson & Ruff, Reference Lawson and Ruff2004). Our findings for negative affect are also consistent with Lin et al. (Reference Lin, Xu, Huang, Jia, Zhang, Yan and Zhang2017) who observed that temperament development was more strongly associated with postnatal maternal mental health problems than with prenatal mental health problems. Links between maternal anxiety and depression and infant negative affect may be understood in the context of both potential behavioral (e.g., postnatal parent-child interactions) and physiological (e.g., neuroendocrine, epigenetic) mechanisms. These results may also point to an underlying genetic component related to increased anxiety, depression, and negative affect.
We did not observe indirect effects of objective hardship to positive affect/surgency and orienting/regulatory capacity via maternal depression/anxiety symptoms. There is some evidence that anxiety and depression exhibit effects in different directions on positive affect/surgency (Simcock et al., Reference Simcock, Elgbeili, Laplante, Kildea, Cobham, Stapleton, Austin, Brunet and King2017). Anxiety and depression symptoms were estimated as a single latent variable, and although the constructs were highly correlated in this sample, it is possible they exerted separate effects on infant temperament traits that were not captured in this model.
A limited number of studies have systematically examined the effects of both prenatal and postnatal stress exposure on child temperament and typically only included postnatal stress, such as life events, as a covariate when studying prenatal stress. Similar to Laplante et al. (Reference Laplante, Brunet and King2016), our analytic sample only included women exposed to a natural disaster prenatally, however, the longitudinal design of the present study allowed us to also examine maternal mental health symptoms that continued into the postnatal period. Differences between the present study and other prenatal stress studies (Bush et al., Reference Bush, Jones-Mason, Coccia, Caron, Alkon, Thomas and Epel2017; Buthmann et al., Reference Buthmann, Ham, Davey, Finik, Dana, Pehme, Zhang, Glover and Nomura2019; Laplante et al., Reference Laplante, Brunet and King2016; Tees et al., Reference Tees, Harville, Xiong, Buekens, Pridjian and Elkind-Hirsch2010) may be explained by different measures and timing of pre- and postnatal stress; existing work has shown that different types of maternal stress (i.e., objective hardship, subjective distress, anxiety, depression, posttraumatic stress symptoms) are differentially associated with child outcomes (Lafortune et al., Reference Lafortune, Laplante, Elgbeili, Li, Lebel, Dagenais and King2021). Our results also contribute to developmental cascade models that have tested several potential mechanisms of maternal transmission of prenatal stress for child outcomes (Hentges et al., Reference Hentges, Graham, Plamondon, Tough and Madigan2019; Moss et al., Reference Moss, Simcock, Cobham, Kildea, Elgbeili, Laplante and King2017). Taken together, we recognize the importance of examining different measures of maternal stress across the pre- and postnatal period to better understand how they shape children’s temperamental development and risk for psychopathology. This work also highlights the potential intergenerational effects of prenatal stress and persistent mental health symptoms into the postnatal period for infant socio development. In line with developmental psychopathology principles of multifinality, there are many pathways to the later development of psychopathology in children such that different domains of temperament may be associated with different psychopathology outcomes across development (Cicchetti & Rogosch, Reference Cicchetti and Rogosch1996). Thus, different domains of perinatal maternal psychopathology may pose differential risk and protective factors for developmental psychopathology trajectories in offspring.
Limitations, strengths, and future directions
The study has several limitations to note. Infant temperament was only assessed through maternal report; multiple informants or observational measures may have provided different results in the assessment of temperament. Mothers’ report of infant temperament may have been biased by their own mental health symptoms, however, we controlled for concurrent maternal anxiety/depression symptoms and recent research found little empirical evidence for systematic bias in mothers’ report of early temperament from their current or past anxiety/depression symptoms (Olino et al., Reference Olino, Guerra-Guzman, Hayden and Klein2020). We did not account for pregnancy-specific anxiety, which has also been shown to be associated with infant temperament (Erickson et al., Reference Erickson, Gartstein and Dotson2017) and may have been exacerbated by the storm and related stressors. Due to the original study design and the feasibility of collecting data after the storm, many of the mothers had already given birth before completing the baseline assessments. Only a small percentage of the sample was still pregnant at baseline (13%), limiting the ability to compare or draw specific conclusions about maternal mental health during pre- and postnatal periods. The sample included in the current analyses may not be representative of the whole sample as the final sample reported higher income and education, however income and education were included as covariates in final analyses. Additionally, only anxiety/depression symptoms were collected at the postpartum assessment, while maternal posttraumatic stress symptoms were not assessed at this time point.
There are also several limitations to note with the reporting of objective hardship. It is possible that mothers’ reporting of their hardships related to the flooding from Hurricane Harvey could have been biased due to retrospective reporting which was at least 7 months after the storm, or to whether they had been pregnant or not at the time of reporting. On the other hand, the items on the HOSS were designed to be as objective as possible and to leave little room for interpretation. Using a very similar scale, prior research has found that women’s reports of their objective hardship 6 years after the Quebec ice storm were not significantly different from their levels reported at baseline (Nguyen et al., Reference Nguyen, Jones, Elgbeili, Monnier, Yu, Laplante and King2018); this is likely due to the exceptional nature of the events and to the frequent retelling of one’s experiences. Only for the few women who were still pregnant when they completed the HOSS more than 7 months after the disaster is it possible that their responses failed to include flood-related hardships that endured or occurred much later and could still have been considered “prenatal” exposure. Additionally, the objective hardship measure assessed flood-related hardships that could have occurred after they gave birth and could include both prenatal and postnatal hardships, especially for those women in their final months of pregnancy at the time of the flooding. Future work should examine the trajectory of maternal mental health and stress reactions from prenatal to postnatal period and how these patterns influence temperament outcomes.
The present study has several strengths. Testing associations between perinatal maternal stress and infant outcomes in the context of a natural disaster presents the opportunity for a quasi-experimental study that helps to control for individual-level confounds inherent to correlational research designs. Mothers in the Houston area all experienced the same stressor of Hurricane Harvey but to different degrees of exposure, providing the opportunity to study the dose-response effects of exposure rather than simply the presence/absence of the stressor or the cumulative effect of several unrelated life events. Existing studies of prenatal stress assess numerous types of stressors, however many may be related to personal attributes of the mother, such as interpersonal conflicts or loss of employment, making it hard to disentangle the independent impact of the stressor vs maternal factors. Natural disasters occur independent of maternal characteristics, making it ideal to study the differential effects of exposure to a stressful event versus maternal factors. The present study included a prospective mixed design and large sample size which allowed us to utilize advanced statistical methods to model the within-subject data. This study builds on prior studies of natural disasters as a prenatal stressor, by examining indirect associations between prenatal stress and infant temperament in a larger sample that included variation across socioeconomic status, race, ethnicity, and stress exposure.
Future research should continue to assess children’s socioemotional and behavioral problems in this Hurricane Harvey-exposed cohort across development to investigate long-term outcomes of prenatal stress. Additionally, there is evidence that postnatal caregiving plays an important role in potentially buffering the negative effects of prenatal stress exposure and maternal posttraumatic stress that should be further examined (Austin et al., Reference Austin, Christl, McMahon, Kildea, Reilly, Yin and King2017; Diab et al., Reference Diab, Isosävi, Qouta, Kuittinen and Punamäki2018; Kaplan et al., Reference Kaplan, Evans and Monk2008). It is also important to consider the underlying neurobiological development and functioning of offspring in utero and across early development to further understand how maternal experiences shape infant outcomes.
Conclusion
This study examined prospective associations between maternal objective hardship and mental health symptoms across the perinatal period with infant temperament in a cohort of women exposed to Hurricane Harvey during pregnancy. Our study found evidence for differential pathways to specific infant temperament outcomes through increases in maternal mental health symptoms. Unexpectedly, disaster-related objective hardship was indirectly related to increased infant orienting/regulatory capacity via maternal posttraumatic symptoms, suggesting a potentially adaptive response to increased hardship and posttraumatic stress symptoms. Results support a potential psychological mechanism for the intergenerational transmission of stress that could be indicative of an unexpected adaptive calibration to stress experienced in perinatal periods. On the other hand, more severe maternal objective hardship predicted more negative affect in infancy via a cascade through perinatal maternal anxiety and depression. These results advance knowledge of early temperamental traits that may promote resiliency after exposure to varying levels of stress. This is important as understanding potential strengths, rather than only deficits related to developmental adaptions to stress (Ellis et al., Reference Ellis, Bianchi, Griskevicius and Frankenhuis2017) can improve education, policy, and interventions to fit the needs and potentials of stress-exposed children and youth.
Supplementary material
The supplementary material for this article can be found at https://doi.org/10.1017/S0954579423000160
Acknowledgements
Many thanks to the Harvey Mom Study families who participated in this research. The authors would like to thank Griselda Barcenas and Rosalva McPherson for their support with participant recruitment and data management, David Cornish for help with online participant recruitment, and Shana Rimmer and Rick Watts with the Women and Children’s Health Research Institute at the University of Alberta for REDCap management.
Funding statement
The Canadian Institutes of Health Research permitted to use funds from grant PJT-148903 to support this research, and funds from Canadian Institutes of Health Research Grant 151029 to DMO supported this research.
Conflicts of interest
None.








