Introduction
Major depressive disorder (MDD) is a highly prevalent chronic condition both in the USA and worldwide, and it is estimated that one in six people will develop the disorder during their lifetime (Howard et al., Reference Howard, Adams, Clarke, Hafferty, Gibson, Shirali and McIntosh2019). The prevalence of MDD appears to be increasing over the past 25 years and age at first onset has been decreasing (Hasin et al., Reference Hasin, Sarvet, Meyers, Saha, Ruan, Stohl and Grant2018; Sloan & Sandt, Reference Sloan and Sandt2006). MDD is an important public health concern as it is associated with poor health, mortality, disability-years, functional impairment, and cognitive and social functioning, especially in the older population. Although first onset of MDD is less common in older adults compared to younger adults, with the first depression episode typically occurring before age 40 (Park et al., Reference Park, Hahn, Hwang, Kim, Jun, Lee and Park2014; Sloan & Sandt, Reference Sloan and Sandt2006), MDD (either late-onset or recurrent MDD) in older adults is fairly common and can lead to serious adverse consequences especially due to aging-related physical and cognitive impairment (Fiske, Wetherell, & Gatz, Reference Fiske, Wetherell and Gatz2009). Given the rapid growth of older populations (Anderson, Goodman, Holtzman, Posner, & Northridge, Reference Anderson, Goodman, Holtzman, Posner and Northridge2012), it has become particularly important to identify those at risk for MDD episodes in order to reduce the personal and societal economic burden associated with the condition. Once identified, health care professionals can provide early, targeted interventions for those at risk for MDD by monitoring their symptoms before they develop MDD and ensuring they receive adequate treatment, which will be critical for reducing the burden of the disease in older adults. This is especially important, as compared to younger and middle-aged adults, older individuals with MDD are less likely to seek psychiatric treatment (~30% for 65+ v. ~45% for 35–54 years) (Mackenzie, Reynolds, Cairney, Streiner, & Sareen, Reference Mackenzie, Reynolds, Cairney, Streiner and Sareen2012).
Numerous risk factors have been associated with MDD and the magnitude of association may differ across the lifespan (Emerson et al., Reference Emerson, Small, Merrill, Chen, Torres-Gil and Siddarth2018; Kendler, Gardner, & Prescott, Reference Kendler, Gardner and Prescott2002, Reference Kendler, Gardner and Prescott2006). For instance, familial risk is related more strongly to early-onset MDD (Kendler, Gatz, Gardner, & Pedersen, Reference Kendler, Gatz, Gardner and Pedersen2005). Furthermore, these associations may vary based on study design as a result of differences in study population, study sampling, diagnostic classification for MDD, and data source (e.g. surveys v. medical records). Nevertheless, well-documented MDD risk factors include genetics [the estimated heritability is between 30% and 40% (Power et al., Reference Power, Tansey, Buttenschon, Cohen-Woods, Bigdeli, Hall and Lewis2017)], neurobiological factors (e.g. dysregulation of neurotransmitter systems such as serotonin), physical illness (e.g. cardiovascular diseases), and social determinants of health (SDoH; e.g. childhood abuse, lifetime adverse events, and lack of physical activities) (Sekhon, Patel, & Sapra, Reference Sekhon, Patel and Sapra2021). SDoH is defined as aspects of social environment that affect a wide range of health, functioning, and quality-of-life risk and outcomes (Andermann, Reference Andermann2016; Koh, Piotrowski, Kumanyika, & Fielding, Reference Koh, Piotrowski, Kumanyika and Fielding2011). Some examples of individual-level SDoH are socioeconomic status (SES), education, income, housing status, and social support networks (Singh et al., Reference Singh, Daus, Allender, Ramey, Martin, Perry and Vedamuthu2017). In MDD, the impact of SDoH is well documented: higher SES, the most commonly studied SDoH, has a protective impact on MDD, mainly due to the fact that people with higher SES are less likely to have certain adverse life events (e.g. trauma), health behaviors that are linked to adverse health, and have better healthcare access (Albert, Reference Albert2016; Assari, Reference Assari2017; Averina et al., Reference Averina, Nilssen, Brenn, Brox, Arkhipovsky and Kalinin2005; Gibbs & Rice, Reference Gibbs and Rice2016; Kim & Chen, Reference Kim and Chen2011; Liang et al., Reference Liang, Gong, Wen, Guan, Li, Yin and Wang2012; McClintock & Bogner, Reference McClintock and Bogner2017; Shittu et al., Reference Shittu, Issa, Olanrewaju, Mahmoud, Odeigah and Sule2014; Tanner, Martinez, & Harris, Reference Tanner, Martinez and Harris2014).
Beyond commonly studied SDoH (SES, income, and education), recent research has examined the role of more diverse SDoH variables, such as social support, on depression and found a strong contribution: depressed individuals with poorer social support and/or loneliness have worse outcomes in terms of symptom recovery or remission, and functional outcomes (Wang, Mann, Lloyd-Evans, Ma, & Johnson, Reference Wang, Mann, Lloyd-Evans, Ma and Johnson2018). A study of MDD using the UK Biobank found optimal sleep duration and lower screen time were protective against depressed mood (Sarris et al., Reference Sarris, Thomson, Hargraves, Eaton, de Manincor, Veronese and Firth2020). Choi et al. reported that a higher level of physical activity was associated with a reduced risk of depression across all levels of genetic vulnerability (Choi et al., Reference Choi, Zheutlin, Karlson, Wang, Dunn, Stein and Smoller2020). While SDoH (e.g. social support and adverse life events) in general plays a significant role in MDD at all ages, the degree of importance of specific types of SDoH may differ by age. For instance, SES and education play a stronger role in younger age groups (Kendler et al., Reference Kendler, Gatz, Gardner and Pedersen2005). However, the role of SDoH variables that act as a buffer for aging-related risk factors (e.g. cardiovascular diseases and cognitive impairment) is stronger in older adults and includes close social network, bereavement and living situation (Fiske et al., Reference Fiske, Wetherell and Gatz2009; Litwin, Stoeckel, & Schwartz, Reference Litwin, Stoeckel and Schwartz2015).
Despite the extensive literature on the associations between SDoH and mental health conditions, prior studies have typically analyzed each SDoH variable separately. However, these variables may interact with each other to contribute to the disease, and thus it is important to analyze different SDoH variables in mutually controlled models. In a population-based study using electronic health records (EHR) data, for example, higher SES and minority status (i.e. being other than non-Hispanic White) were associated with a lower risk of mood disorder, but the effect of minority status differed depending on SES, potentially due to issues such as healthcare access and literacy among individuals with lower SES (Wi et al., Reference Wi, St Sauver, Jacobson, Pendegraft, Lahr, Ryu and Juhn2016). While a few studies have considered interactions among SDoH, these studies mostly investigated basic demographic characteristics (e.g. age, gender, race/ethnicity) and only a small number of other SDoH (e.g. education).
In the current study, we utilized data from the Mayo Clinic Biobank (MCB), including a health questionnaire with over 30 SDoH variables and linked EHR data that were used to identify participants with newly diagnosed MDD at Mayo Clinic in older age (50–89 years old at the time of enrollment in the MCB). We aimed to investigate multiple SDoH simultaneously to identify the most influential SDoH contributing to the development of MDD in older adults. Because the MCB sample is relatively homogeneous with regard to SES (~50% with college degrees or higher), self-reported race/ethnicity (~90% White), and geographic distribution, the findings may not generalize to all populations (Olson et al., Reference Olson, Ryu, Johnson, Koenig, Maschke, Morrisette and Cerhan2013, Reference Olson, Ryu, Hathcock, Gupta, Bublitz, Takahashi and Cerhan2019). Nevertheless, this study is an important step toward understanding the SDoH factors that impact MDD in the older adult populations that the MCB sample represents, which can subsequently be evaluated in other populations.
Methods
Study design and participants
This cohort study utilized data from Mayo Clinic patients who enrolled in the MCB. The design and governance of the MCB is described elsewhere (Hathcock et al., Reference Hathcock, Kirt, Ryu, Bublitz, Gupta, Wang and Olson2020; Olson et al., Reference Olson, Ryu, Johnson, Koenig, Maschke, Morrisette and Cerhan2013, Reference Olson, Ryu, Hathcock, Gupta, Bublitz, Takahashi and Cerhan2019). Briefly, the MCB started to enroll adults (age 18 or older) in April 2009 and ended active enrollment in March 2016. With some exceptions (i.e. volunteers who self-selected to participate without a study invitation), participants were largely selected through medical visits to primary care departments at Mayo Clinic. At consent, participants provided biological samples, completed a questionnaire, and provided permission for researchers to search their full EHR from all clinical visits (including past and future data) for studies approved by the MCB. This study was reviewed and approved by Mayo Clinic Institutional Review Board (IRB) and Mayo Clinic Biobank Access Committee.
At the time of pulling EHR data for the current study (6 April 2020), baseline survey data were available for a total of 41 174 participants who were 50–89 years old at the time of their biobank enrollment. We selected participants over 50 years of age at enrollment to study the role of SDoH in older adults, but excluded participants over 90 years old because they are unlikely to represent the general population in this age group [individuals with very poor physical/cognitive health, which are common in the oldest age group, are unlikely to travel to the clinic to enroll (Takahashi et al., Reference Takahashi, Ryu, Olson, Anderson, Hathcock, Haas and Cerhan2013), even if they were able to provide informed consent to participate in the biobank]. Of those eligible, 10 938 (27%) participants had a known history of depression prior to the baseline survey completion, either documented in the EHR and/or self-reported on the enrollment questionnaire. Participants having at least one MDD-related ICD9/10 code in their EHR were considered as having a prior history of MDD in the EHR (see the Primary outcome section below). Self-reported depression was identified by a baseline survey question asking if a participant had been diagnosed with depression. Because our intent is to examine SDoH as potential risk factors for future MDD diagnosis, we excluded patients with a history of MDD and used the data for the remaining 30 236 participants to quantify variable importance of SDoH for the risk of MDD in older adults.
Although the MCB's recruitment strategy aimed to enrich for participants having comprehensive EHR, the MCB consists of participants with a wide range of EHR coverage. However, over 70% of the participants had clinic visits in at least 3 out of 5 years prior to consent or live in Mayo Clinic catchment areas (Olson et al., Reference Olson, Ryu, Hathcock, Gupta, Bublitz, Takahashi and Cerhan2019). The study cohort has a median length of prior EHR records of 12.4 years (25th–75th percentiles: 4.2–30.6 years). To assess the impact of EHR coverage, we conducted a sensitivity analysis using only data from a subset of participants (N = 11 716) that are included in the Mayo Clinic Primary Care Panel (PCP; i.e. receiving regular primary care at Mayo Clinic).
Primary outcome
The primary outcome of interest was a new MDD diagnosis since the time of biobank survey completion (index date). As described above, participants with a known history of depression (determined from the EHR or self-report) were excluded from the analysis. However, not all patients with an early or prior history of MDD may have been excluded because of either participants' failure to report or recall the disease which may have occurred many years before, or incompleteness of EHR to capture episodes from the past. Therefore, we label the main outcome as ‘new episode of MDD’, as opposed to ‘incident MDD’. Participants were followed up from index date until the last follow-up date (death date, the date of first MDD diagnosis, or 6 April 2020, whichever comes first). MDD was defined based on having at least one MDD-related ICD9/10 code, using an initial list of ICD9/10 codes mapped to phecodes for MDD [296.2 and 296.22, available from https://phewascatalog.org/phecodes (He et al., Reference He, Ortiz, Marshall, Mendelsohn, Curtis, Barr and Kim2019; Wei et al., Reference Wei, Bastarache, Carroll, Marlo, Osterman, Gamazon and Denny2017)], with minor modification [adding dysthymic disorder (ICD9:300.4), depressive type psychosis (ICD9: 298.0), and atypical depressive disorder (ICD9: 296.82)]. The complete list of ICD9/10 codes is presented in online Supplementary Table S1.
Primary predictors
The main goal of this study was to quantify the relative importance (RI) of SDoH variables in order to identify the most influential variables for the risk of new episodes of MDD in older adults. We selected, a priori, several SDoH variables collected from self-reported health questionnaires administered at the time of biobank enrollment, including (a) perceived level of social activity (low, medium, high); (b) six questions from ENRICHD Social Support Instrument (ESSI; someone available to listen, give advice, show love/affection, help with daily chores, provide emotional support, to trust/confide) (Vaglio et al., Reference Vaglio, Conard, Poston, O'Keefe, Haddock, House and Spertus2004); (c) general health behaviors (e.g. smoking status); (d) physical activities (e.g. exercise); and (e) environmental variables (e.g. secondhand smoking). In addition, we also considered several demographic variables (e.g. age, gender, race/ethnicity, education attainment, and marital status). Age at time of enrollment in the biobank and gender information were extracted from EHR, while the rest of the SDoH data were collected from the survey. The survey questions are listed in online Supplementary Table S2. The ESSI questions measure different aspects of social support that are correlated. For a secondary analysis, we also calculated a perceived social support score using five of the aforementioned six ESSI questions (omitting ‘someone to help with daily chores’) using a previously established approach (Gan et al., Reference Gan, Xiong, Song, Xiong, Yu, Gao and Chen2019). Scores of the five questions were summed (ranging from 5 to 25), and dichotomized to determine the degree of social support (low v. high): Low social support was defined as a total score ⩽18 and a score ⩽3 (none, little, or some of the time) for at least two questions (Gan et al., Reference Gan, Xiong, Song, Xiong, Yu, Gao and Chen2019).
Statistical analysis
Descriptive statistics [median (25th–75th percentile) for continuous variables and percentage for categorical variables], were used to characterize the study sample. For most variables, the percentage of missing information was <1% with some exceptions such as exercise questions (4% missing). The main goal of the analysis was to quantify the RI of SDoH variables when analyzing 30 variables simultaneously. Analysis limited to participants with complete data (which would exclude ~20% of the participants) may lead to biased results, and thus we first imputed missing SDoH data using Multiple Imputation by Chained Equation (MICE) within a random forest framework (Shah, Bartlett, Carpenter, Nicholas, & Hemingway, Reference Shah, Bartlett, Carpenter, Nicholas and Hemingway2014) with five repetitions, using the R package mice v3.10-0. Following imputation, the univariate association between each SDoH variable and the risk of MDD was tested using a Cox regression model adjusting for age (using a quadratic spline) and gender in each of the five imputation replicates. For each SDoH variable, the model parameter estimates and test statistics [hazard ratio (HR), 95% confidence interval (CI) and associated p values] from the five repetitions were aggregated using ‘Rubin's Rules’, implemented in the R package miceadds v3.10–28.
To quantify the RI of each SDoH variable for predicting MDD, we used Cox proportional hazards models with gradient boosting machine (GBM) approach (Natekin & Knoll, Reference Natekin and Knoll2013). The analysis was performed for each imputation replicate and the median of RIs from the five imputation repetitions was used to identify the most influential variable. The GBM models were constructed using the R package gbm v2.1–8 with 80% of the data used as the training dataset, with 25 000 trees, fivefold cross-validation, 100% bag fraction, and two-way interactions included. Using the final fitted model, the RI of each SDoH variable was calculated using a feature importance ranking measure on quantifying the ‘flatness’ of the effects of each variable on the risk of MDD, assessed by partial dependence plots (PDPs) (Greenwell, Boehmke, & McCarthy, Reference Greenwell, Boehmke and McCarthy2018) using the R package pdp v0.7-0. Relative ‘flatness’ was defined by the standard deviation of predicted partial dependent function over the data range of each SDoH variable, with a higher score implying greater RI.
After quantifying the RI of each SDoH variable, potential interaction effects between the most influential variables and the rest of the SDoH were tested using Cox regression models, adjusting for age and gender. We also conducted a sensitivity analysis by repeating the entire analysis using only data from participants who were included in the PCP at the time of biobank enrollment. All analyses were repeated using an aggregated social support question (dichotomized), instead of using the five separate ESSI social support questions described above.
Results
Cohort characteristics
After excluding participants who had a prior history of depression identified via either EHR or self-report, a total of 30 236 patients aged 50–89 years at the time of enrollment were included in the study. The study cohort had a median age at the index date of 67 years, was about half female, mostly white (93%), non-Hispanic (98%), and US born (95%). Over 50% had a 4-year college degree or higher (Table 1). Low social connection was reported by 11% of the participants for the level of social activity and 16% for social support (Table 2). Roughly 6% of the participants reported having little to no time with someone they trust and confide in (online Supplementary Table S3). During the follow-up (median follow-up duration: 6.7 years), 2073 (6.8%) participants had at least one diagnosis code for MDD.
Table 1. Basic characteristics of the study participants and univariate association results (adjusted for age and gender) between each characteristic and risk of major depressive disorder
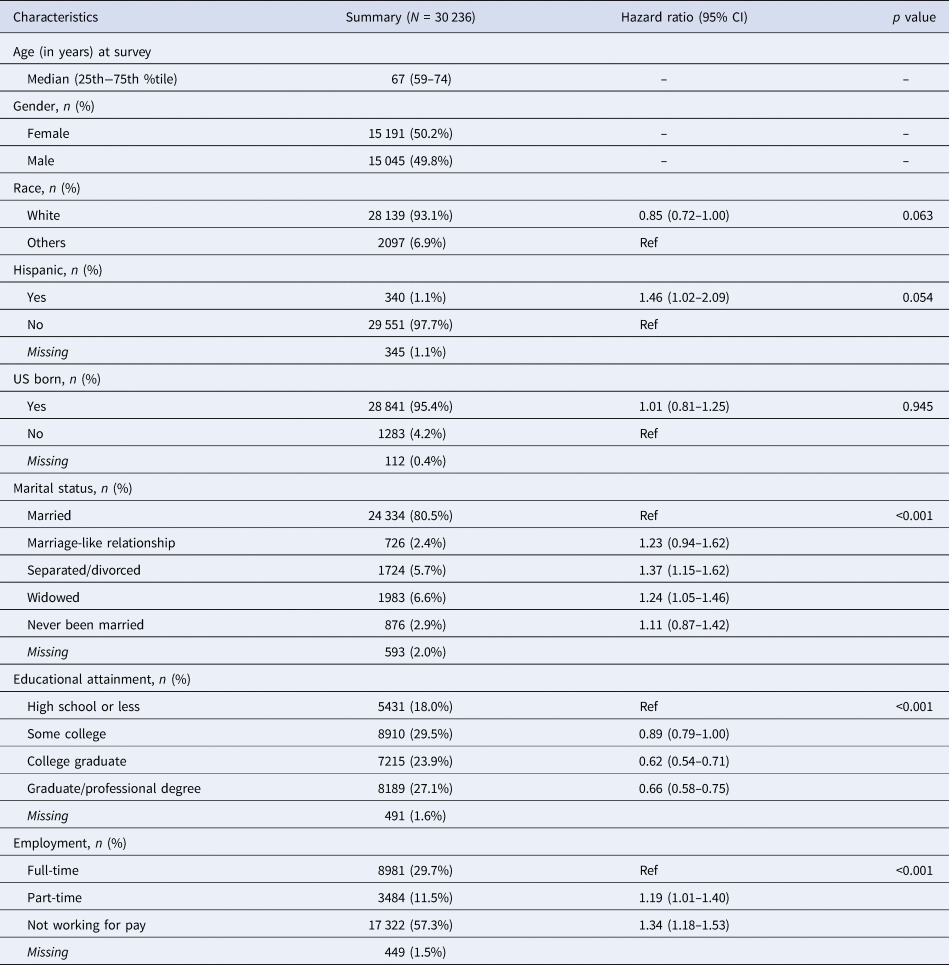
Table 2. Univariate association results (adjusted for age and gender) between social connection (activity and support) questions and risk of major depressive disorder in the study cohort
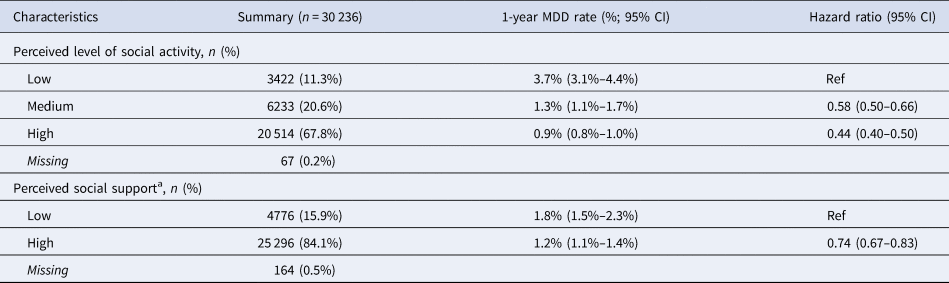
a Perceived low social support is a composite score for measuring perceived social support, using five ENRICHD Social Support Instrument (ESSI) questions (someone to listen, someone to give advice, someone for love, someone for emotional support, and someone to trust and confide).
Univariate associations between SDoH and MDD risk
Participants in their 60s had the lowest rate of new diagnoses of MDD and the risk increased with advancing age. MDD risk was higher among women than men [HR = 1.37 (95% CI 1.25–1.49)]. Most of the SDoH variables (collected at the index date, prior to MDD diagnosis) were associated with the risk of MDD (Tables 1 and 2, and online Supplementary Table S3). For instance, after adjusting for age and gender, a higher level of social activity was associated with a reduced risk of MDD [HR = 0.44 (95% CI 0.40–0.50) when comparing participants having high level v. low level; see Table 2 and Fig. 1]. Similarly, participants with high social support also had a lower risk of MDD compared to those with low support [HR = 0.74 (95% CI 0.67–0.83)], although the effect size was smaller than for social activity. Similar findings were observed in the sensitivity analysis restricted to the subset of the cohort consisting of participants who were included in the Mayo Clinic PCP (i.e. those who received usual medical care at Mayo Clinic) at the time of biobank enrollment (online Supplementary Table S3).

Fig. 1. Kaplan–Meier plot for developing major depressive disorder, by perceived level of social activity.
Relative importance of SDoH on MDD risk
Among the 30 SDoH variables considered (including age and gender), the most influential variable for the risk of a new episode of MDD was the level of social activity (median RI = 0.17; Fig. 2), followed by age (median RI = 0.14). Overall, MDD risk after age 60 years increased with age, which may indicate late-onset MDD. Higher level of social activity was associated with a lower risk of MDD (Fig. 3). ESSI social support questions had a much smaller influence (median RI scores <0.03; online Supplementary Fig. S1). A separate analysis showed that the influence of social support (as a composite score, rather than using individual ESSI variables) was also small compared with the effect of the level of social activity (data not shown). In a sensitivity analysis restricted to participants who received usual medical care at Mayo Clinic (PCP cohort), the relationship of the level of social activity to MDD risk was also strong (although age had a stronger influence in this sub-cohort) and effect sizes were similar (online Supplementary Figs. S1 and S2).
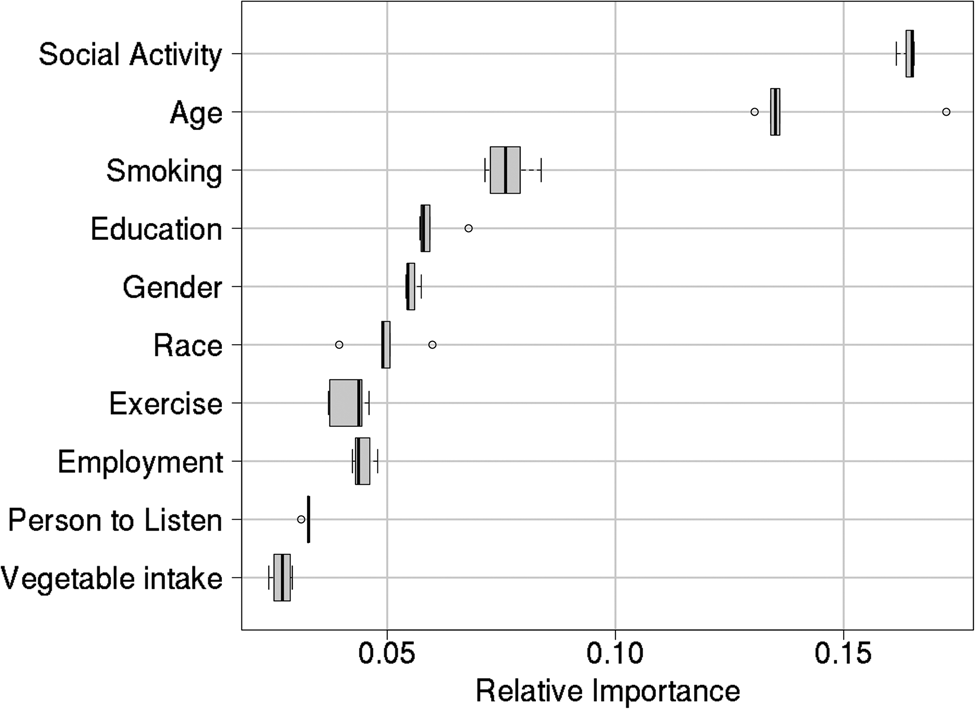
Fig. 2. Relative influence of the top 10 social determinants of health variables for the risk of major depressive disorder.

Fig. 3. Relationship of age (left panel: comparing to the median age of the cohort) and perceived level of social activity (right panel: comparing with low perceived level of social activity [0–5]) with the risk of major depressive disorder.
Interaction between the level of social activity and other SDoH
To assess whether the most influential SDoH variable for the risk of a new episode of MDD (level of social activity) interacted with other SDoH to contribute MDD risk, we tested for interaction effects between the level of social activity and other SDoH, adjusting for age and gender. None of the other SDoH variables interacted with the level of social activity (all interaction p values ⩾0.05), implying that the influence of level of social activity on MDD risk was independent of age (interaction p = 0.42), gender (interaction p = 0.36), and social support (e.g. interaction p = 0.75 for the availability of someone to trust and confide in). The results were similar for the PCP cohort (online Supplementary Table S4).
Discussion
This study quantifies the RI of various SDoH to the risk of a new episode of MDD in older adults. In addition to age (a known risk factor for MDD), perceived level of social activity was the SDoH most closely correlated with a new diagnosis of MDD. The effect of level of social activity was independent of other SDoH such as age, gender, and social supports. Further studies are needed for replication and to assess whether these findings reflect SDoH being a consequence of depression or a cause of depression. Given the lack of diversity in the study population, further studies are needed to determine if the findings also hold for more diverse populations, such as other ethnic groups. However, given that the level of social activity can be assessed via a single question, it could be easily implemented in routine clinical practice as a means of screening older adults for MDD risk followed by more detailed mental health assessments of individuals with low level. Assessing patients' perceptions about their level of social activity (or related psychological states such as loneliness) is important because it may be difficult for primary care clinicians to identify patients with few social connections (Due, Sandholdt, Siersma, & Waldorff, Reference Due, Sandholdt, Siersma and Waldorff2018). This aspect is particularly important in the COVID-19 pandemic era where social isolation and depressive symptoms have become more prevalent (Bu, Steptoe, & Fancourt, Reference Bu, Steptoe and Fancourt2020; Vahratian, Blumberg, Terlizzi, & Schiller, Reference Vahratian, Blumberg, Terlizzi and Schiller2021).
A large volume of literature demonstrates the importance of SDoH as risk factors for mental health conditions including depression. Fiske et al. suggested that different SDoH variables contribute to depression over the life span: for instance, high education plays a protective role for depression in young adults. However, social connection such as engagement and a close social network emerge as protective factors for depression in the elderly, which is likely because these factors act as a buffer for aging-related risk factors (e.g. physical/cognitive impairment and cardiovascular disease) that are specific to older adults (Fiske et al., Reference Fiske, Wetherell and Gatz2009). As an example, Roy et al. reported that adverse effects of living alone (an important SDoH in the elderly) on psychological stress were not present among older adults with greater social participation (Roy et al., Reference Roy, Levasseur, Dore, St-Hilaire, Michallet, Couturier and Genereux2018). The importance of social connections is further supported by a study based on adults aged 57–85 years, in which social disconnectedness (e.g. small social network, infrequent social interaction) predicted higher subsequent perceived social isolation (e.g. loneliness, lack of support), which in turn predicted higher depression symptoms (Santini et al., Reference Santini, Jose, Cornwell, Koyanagi, Nielsen, Hinrichsen and Koushede2020). Our finding that the level of social activity (an aspect of social connection) is the most influential SDoH in older adults is in line with these findings.
Several studies have reported associations between social activity and mental health conditions. Participation in social activities may protect against depression in elderly patients, due to stimulating bodily systems, and reinforcing life-long patterns of attachment (Lee & Kim, Reference Lee and Kim2014). However, the association may differ by types of activity and culture. A study based on older adults from 10 European countries showed that social activity was associated with depressive symptoms, but the association direction and strength depended on the types of social activities, with participation in religious organizations having greater benefits than other forms of social activities (e.g. volunteer work), which may be partly because religious participation may provide a coping mechanism and prevent social isolation (Croezen, Avendano, Burdorf, & van Lenthe, Reference Croezen, Avendano, Burdorf and van Lenthe2015). However, a longitudinal study based on older Asian adults showed that attending religious services was related to an increase in depressive symptoms among those who were not depressed at baseline, whereas participating in social gatherings with friends and neighbors was associated with a decrease in depressive symptoms (Min, Ailshire, & Crimmins, Reference Min, Ailshire and Crimmins2016). Flatt et al. also emphasized the importance of considering different types of social activities in relation to cognitive health and general well-being in older adults (Flatt et al., Reference Flatt, Hughes, Documet, Lingler, Trauth and Albert2015). Therefore, inconsistent results regarding the association between social activity and mental health may be related to differences in types of social activities and cultural context. As a measure of social activity, we used the perceived level of social activity that incorporates an individual's own evaluation, which is less likely to be affected by the types of activity, frequency, and study setting.
This study has several strengths and limitations. As a strength, our study used data from the MCB; a large portion of this cohort receive primary care at Mayo Clinic and thus have comprehensive EHR data (over 25 years since 1994) available for research (Olson et al., Reference Olson, Ryu, Hathcock, Gupta, Bublitz, Takahashi and Cerhan2019). In addition, our study used both longitudinal EHR and biobank-collected survey data that included SDoH-related questions in addition to medical history. Because SDoH information is not routinely collected in clinical care and therefore not available in EHR, these data provide a unique opportunity to study the role of SDoH on various health outcomes including mental health conditions.
Our study also has several limitations. First, the cohort may not represent the local population because of selection bias that results from enrollment into the MCB. On average, the older participants (50+) are likely in poorer health than their age-matched counterparts from the general population because recruitment was largely based on medical appointments, but might be healthier in the oldest age group because individuals with very poor physical/cognitive health, which is common in this age group, are unlikely to travel to the clinic to enroll (Takahashi et al., Reference Takahashi, Ryu, Olson, Anderson, Hathcock, Haas and Cerhan2013). Because such selection bias might pose the greatest threat to this oldest age group, we excluded biobank participants who were 90 years or older from the analysis. Second, the current study used ICD-9/10 diagnostic billing codes from structured EHR data as the source of case ascertainment, as opposed to other standard approaches such as standardized interviews (First, Reference First, Cautin and Lilienfeld2015). Therefore, misclassification of MDD (especially false negatives) based on ICD codes may be high. Additionally, it is well understood that mental health conditions including depression are generally under-coded in EHR. The concordance between clinical major depression diagnoses and independent assessments is fair to modest (Townsend, Walkup, Crystal, & Olfson, Reference Townsend, Walkup, Crystal and Olfson2012). Also, patients who receive medical care at Mayo Clinic can also seek medical care, including psychiatric care, from other medical centers where the current study was unable to use the data. Nevertheless, EHR-based case ascertainment facilitates efficient large-scale studies compared to traditional approaches and has been used successfully in studies of numerous complex traits including psychiatric disorders (Chen et al., Reference Chen, Lee, Castro, Minnier, Charney, Stahl and Smoller2018; Li, Chen, Ritchie, & Moore, Reference Li, Chen, Ritchie and Moore2020; Smoller, Reference Smoller2018). Third, our study sample did not capture the period when depression prevalence is highest, before age 40 years. As a consequence, some participants included in our study, despite having no clinically diagnosed MDD in their EHR and no self-reported depression at the index date, may still have had a history of depression that was missed due to incomplete EHR and recall bias in self-report. Therefore, our findings may partly reflect the consequences of depression, rather than risk factors for depression, as it is possible that some participants reporting a low level of social activity may already have been experiencing depressive symptoms. Fourthly, there are other factors such as medical comorbidities, cognitive impairment, and activities of daily living that are associated with depression and therefore may have affected the study findings. However, this information was not evaluated in the biobank questionnaire (the source of the SDoH data in this study) and thus was not included in our study. Lastly, our study results may not be generalizable to a more diverse population in terms of race/ethnicity and education, and our study may not have had sufficient statistical power for assessing the importance of some SDoH variables that had low frequencies in our sample including ethnic/racial minority ancestry. As another example, educational attainment is a well-known strong SDoH associated with numerous health outcomes. However, its importance was not strong compared to social activity in our study of older adults. Although it is possible that education may not be as influential on depression in later life, it is also possible that our study lacked statistical power to detect the effect of education due to the overall high level of educational attainment in the study cohort (18% of the MCB participants with high school degree or lower, compared to 34% of the 2010 US population).
In conclusion, our study identified perceived level of social activity as the most influential SDoH variable in older adults. As this variable is easily measurable (as a single question) and its influence is independent of demographic characteristics and other SDoH variables, it could be easily implemented in clinical care to identify patients with an elevated risk of depression who could then be targeted for early intervention.
Supplementary material
The supplementary material for this article can be found at https://doi.org/10.1017/S0033291721004566.
Acknowledgements
Mayo Clinic Biobank is supported by the Mayo Clinic Center for Individualized Medicine. This work was supported by the National Institute of Mental Health (R01 MH121924).
Conflict of interest
The authors have no conflicts of interest with regard to this study. Dr Jyotishman Pathak is co-founder of Iris OB Health Inc., and has equity ownership. Dr John Mann receives royalties from the Research Foundation for Mental Hygiene for commercial use of the C-SSRS. Dr Myrna M Weissman has received research funding from NIMH, Brain and Behavior Foundation, Templeton Foundation and has received book royalties from Perseus Press, Oxford Press, and APA Publishing and received royalties on the social adjustment scale from Multihealth Systems. None of these represent a conflict of interest.








