‘Long before the child develops his inner resources for overcoming dangers he is dependent upon his parents to satisfy his needs, to relieve him of tension, to anticipate danger, and to remove the source of a disturbance. This is the situation of the infant. To the infant and very young child the parents are very powerful beings, magical creatures who divine secret wishes, satisfy the deepest longings, and perform miraculous feats.’ (Reference FraibergFraiberg 1959: p. 12)
The influence of parent–child interaction on the child's development across different domains is becoming increasingly well understood. It is recognised that emotional and psychological difficulties later in life often have roots in early experiences, including the experience of the parent–child relationship. The parent has an important regulatory role for the child, who has not yet developed their own capacity for emotion regulation. However, when a parent is experiencing difficulties, the capacity to fulfil this regulatory role may be impaired. For example, depressed mothers have been observed to show fewer positive facial expressions and less sensitivity towards their infants (Reference Herrera, Reissland and ShepherdHerrera 2004). Infants will alter their behaviour in response to the behaviour of a depressed mother (Reference Manian and BornsteinManian 2009) and, in turn, infants of depressed mothers are at increased risk of developing negative affective states (Reference Tronick and ReckTronick 2009). With regard to the longer term, a meta-analysis by Reference Fearon, Bakermans-Kranenburg and van IjzendoornFearon and colleagues (2010) found that childhood attachment problems were associated with increased risk of other emotional and psychological difficulties, such as externalising behaviour and problems at school. The most recent research has indicated that maternal depression in the first years of a child's life has an impact on the neural basis of empathy in pre-adolescence (Reference Pratt, Goldstein and LevyPratt 2017).
In the UK, it is estimated that perinatal mental health problems cost £8.1 billion for each one-year cohort of births, and that 72% of this cost relates to their adverse effects on the child (Reference Bauer, Parsonage and KnappBauer 2014). There is an increasing emphasis on early intervention in practice, research and policy; and there are an increasing number of interventions aimed at supporting the parent–infant relationship. Parent–infant psychotherapy (PIP), the subject of the review by Reference Barlow, Bennett and MidgleyBarlow and colleagues (2015) in this month's Cochrane Corner, is one such intervention. PIP is a psychodynamic approach with its origins in the work of Selma Fraiberg (Reference Fraiberg, Adelson and ShapiroFraiberg 1975) (Box 1). It aims to address difficulties in the parent– infant relationship (e.g. sleep problems, eating difficulties, ‘excessive’ crying) and contribute to an improvement in parent and infant mental health. PIP is recommended alongside other interventions in the ‘1001 Critical Days’ manifesto (Reference Leadsom, Field and BurstowLeadsom 2013), which is a cross-party manifesto aiming to highlight and support early intervention with a focus on the first 1001 days (2.75 years) of a child's life. The manifesto maps parent–infant services onto the four-tier strategic model used by child and adolescent mental health services (CAMHS), and PIP is recommended at tier 3 as a specialised service for families experiencing high levels of stress (Fig. 1).
BOX 1 Parent–infant psychotherapy and ‘ghosts in the nursery’
‘Ghosts in the nursery’ is a phrase coined by Reference Fraiberg, Adelson and ShapiroFraiberg and colleagues (1975) to describe the way in which a parent's view of their infant may be ‘haunted’ by the parent's relationship experiences, including their experience of their own parents. Parent–infant psychotherapy involves a parent–infant psychotherapist working directly with the parent and infant dyad with the aim of making connections between the parent's experiences of early relationships and the parent's current relationship to the infant, with the aim of directly improving the present parent–child relationship.
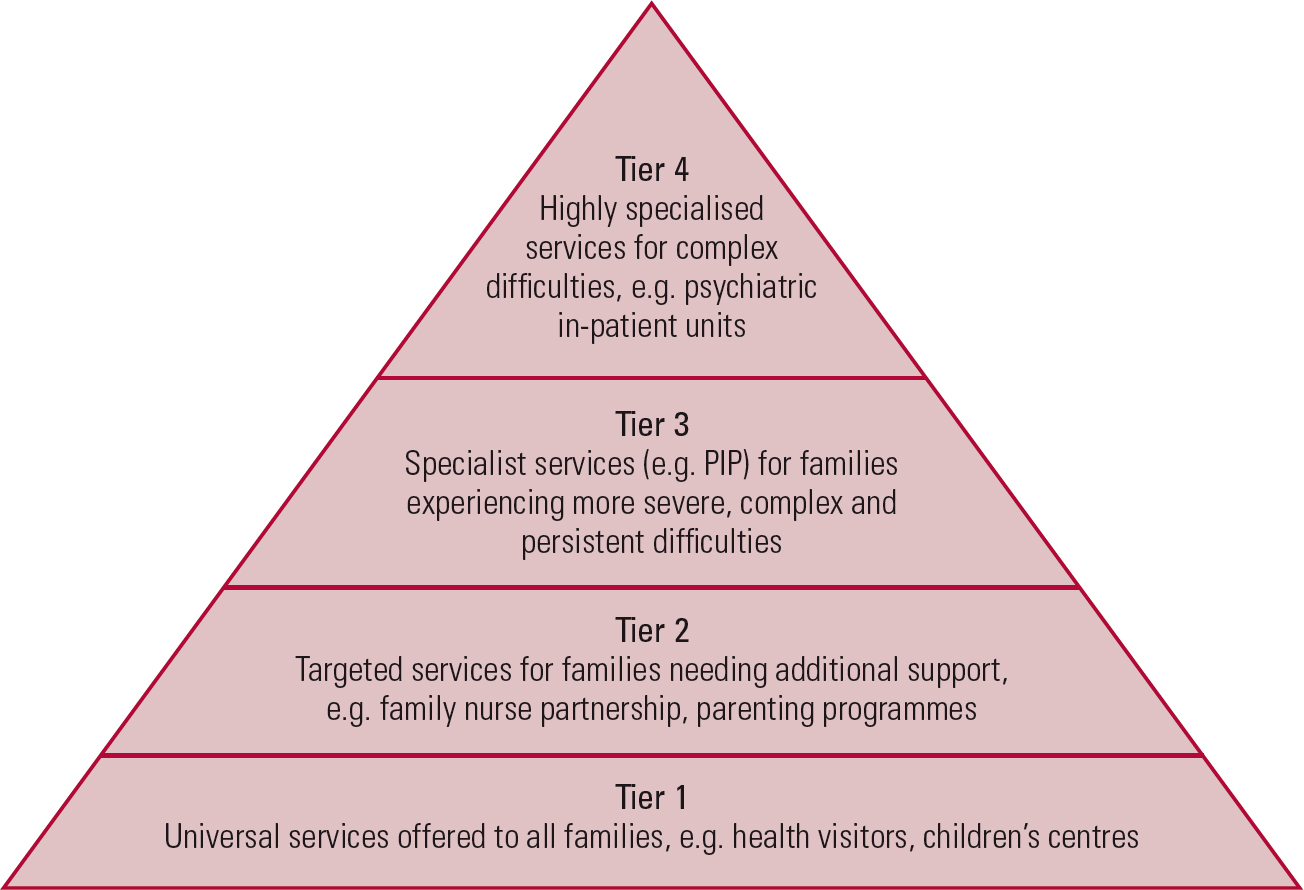
FIG 1 Parent–infant services mapped onto the child and adolescent mental health services fourtier strategic model as outlined in the ‘1001 Critical Days’ manifesto; PIP, parent–infant psychotherapy (after Reference Leadsom, Field and BurstowLeadsom et al, 2013).
Barlow and colleagues conducted their review to examine the effectiveness of PIP in improving parental and infant mental health, and the parent–infant relationship. It also aimed to identify components of PIP that were associated with more effective outcomes and moderators of the effectiveness of interventions (e.g. programme duration). This review is welcome as it is the first systematic review of PIP.
The review
Method
Barlow and colleagues searched electronic databases, hand-searched reference lists and contacted experts in the field in order to identify potentially relevant studies. Randomised controlled trials (RCTs) and quasi-randomised controlled trials (quasi-RCTs) that compared a PIP intervention with a control condition were included in the review. Studies that used a second treatment group were also included. Four primary outcomes were assessed: parental mental health; parent–infant relationship/interaction; infant emotional well-being; and adverse effects. Meta-analysis was undertaken using a random-effects model. For dichotomous outcome data risk ratios (RRs) were presented and for continuous outcome data standardised mean differences (SMDs) were presented.
Results
Eight studies with a total of 846 randomised participants were included. The mean age of the infants was under 24 months at the start of the study. The range of clinical groups included mothers with a diagnosis of depression, mother– infant dyads in prison, and mothers with concern about the mother–infant relationship. Across the eight studies, participants were reported to be of a range of ethnicities. Participants were recruited by various methods, including referrals from mental health professionals and self-referral. In all of the studies the intervention was directed at mothers. Studies were conducted in a variety of settings, including the home, clinic and women's prisons.
All studies included delivery of a PIP intervention; however, delivery varied from one study to another. Duration varied from a total of 8 sessions (two 2-h sessions on one day a week for 4 weeks) (Reference Sleed, Baradon and FonagySleed 2013) to between 46 and 49 sessions scheduled on a weekly basis (Reference Cicchetti, Rogosch and TothCicchetti 2006). Three of the eight studies used manualised programmes (Reference Cicchetti, Rogosch and TothCicchetti 1999, Reference Cicchetti, Rogosch and Toth2006; Reference Sleed, Baradon and FonagySleed 2013). One study delivered PIP in a group context (Reference Sleed, Baradon and FonagySleed 2013). Treatment fidelity was reportedly maintained across all studies by using highly trained and supervised therapists to monitor delivery.
Four studies compared PIP with a treatment-as-usual (TAU) control (Reference Lieberman, Weston and PawlLieberman 1991; Reference Cicchetti, Rogosch and TothCicchetti 1999; Reference Salomonsson and SandellSalomonsson 2011; Reference Sleed, Baradon and FonagySleed 2013). Two studies compared PIP with an alternative intervention (Reference Robert-Tissot, Cramer and SternRobert-Tissot 1996; Reference Cohen, Muir and LojkasekCohen 1999). One study was a three-arm trial comparing PIP with TAU and another intervention (Reference Cicchetti, Rogosch and TothCicchetti 2006). One study was a four-arm trial comparing PIP with TAU and two other interventions (Reference Cooper, Murray and WilsonCooper 2003).
Reporting of results
For parent–infant psychotherapy v. control, the evidence did not favour PIP or control for the incidence of parental depression (RR = 0.74, 95% CI 0.52 to 1.04, 3 studies, 278 participants, low-quality evidence) or parent-reported levels of depression (SMD = −0.22, 95% CI −0.46 to 0.02, 4 studies, 356 participants, low-quality evidence). In addition, the evidence did not show a difference for maternal sensitivity, child involvement or maternal positive engagement. However, the evidence favoured PIP over control for secure attachment (RR = 8.93, 95% CI 1.25 to 63.70, 2 studies, 168 participants, very low-quality evidence), with fewer infants with an avoidant attachment style, fewer infants with disorganised attachment and a higher proportion of infants moving from insecure to secure attachment. With regard to the additional primary outcomes (i.e. adverse effects) and secondary outcomes, there were no differences between PIP and control in any of the meta-analyses.
Quality of the evidence
The authors used the Grading of Recommendations, Assessment, Development, and Evaluation (GRADE; www.gradeworkinggroup.org) approach to assess the overall quality of the data. This included an analysis of the risk of potential bias in the design or execution of the study, using the ‘risk of bias’ assessment tool (Reference Higgins and GreenHiggins 2011). The risk of bias across the studies resulted in downgrading of the evidence for parental depression and secure or disorganised infant attachment to low or very low quality.
Barlow and colleagues conclude, ‘Although […] PIP is a promising model in terms of improving attachment security in high-risk families, there were no significant differences compared with no treatment or treatment-as-usual for other parent-based or relationship-based outcomes, and no evidence that PIP is more effective than other methods of working with parents and infants’ (p. 2). On this basis the authors point to the need for further research.
Discussion
The most striking observation is the lack of robust evidence for PIP. Although the review found that a PIP intervention was more likely to lead to better attachment outcomes, the supporting evidence was of low quality.
Challenges of real-world research
Intervention studies can be placed on a continuum from efficacy to effectiveness (Table 1). Efficacy studies investigate an intervention in an ideal and controlled setting, whereas effectiveness studies investigate an intervention under real-world circumstances. The studies included in the review sit along the efficacy–effectiveness continuum; however, the meta-analysis of the findings as a study of PIP interventions measures effectiveness. Thus, many of the factors that compromised the quality of the evidence can be explained by the real-world context in which the studies were carried out. For example, Barlow and colleagues recognise that there was clinical and statistical heterogeneity, particularly with regard to the comparisons made in the studies. For example, some studies had a TAU control group, whereas others compared PIP only with a different intervention (e.g. psychoeducation, cognitive–behavioural therapy).
TABLE 1 Differences between efficacy and effectiveness intervention studies
What are the implications for researchers?
Further research is needed to address limitations of the existing research, particularly the low quality of its evidence and the risk of bias. The real-world context poses some challenges to this: for example, it is impossible to eliminate performance bias as therapists and participants will always be aware of the type of intervention taking place. However, there are some ways in which the quality of the research could be improved: for example, the use of core outcome measures would make comparison between studies more reliable. Importantly, as Reference RamchandaniRamchandani (2015) points out, there is an ethical responsibility to participants to ensure that research trials are conducted in such a way that the findings can be reliably used to inform planning and provision of services.
Unfortunately, the review was not able to elucidate modifying factors associated with more effective outcomes. Therefore, further research could usefully contribute by exploring the effect of variables such as type of PIP, duration, content, target populations and settings.
Although referred to as ‘parent–infant psychotherapy’, in all of the included studies the intervention was directed at mothers. Further research could usefully consider how the intervention and the outcomes may differ with father–infant dyads, parent–infant triads and same-sex parents. Furthermore, research has demonstrated (e.g. Reference Smith, Domenech Rodriguez and BernalSmith 2011) that the most effective psychotherapy interventions are those with the greater number of adaptations in relation to recipients’ cultural backgrounds; therefore, it would be beneficial to consider the differences in parenting across cultures and whether there is a need for cultural adaptation of PIP.
Research into the effectiveness of early intervention programmes also needs to consider longer-term outcomes and whether any benefits are sustained over time. Three of the studies included in the review contributed follow-up data at 6–12 months (Reference Cohen, Muir and LojkasekCohen 1999; Reference Cooper, Murray and WilsonCooper 2003; Reference Cicchetti, Rogosch and TothCicchetti 2006) and 5 years (Reference Cooper, Murray and WilsonCooper 2003). Some other studies did attempt to gather follow-up data, but this was not possible because of sample attrition. Given the limited follow-up data, there is scope for further research into the effectiveness of early intervention programmes to explore longer-term outcomes and whether any benefits are sustained over time.
Recent evidence
The review makes reference to five ongoing studies with the potential to contribute to the evidence base for the effectiveness of PIP. Results of two of these have since been published. One is an RCT by Reference Goodman, Prager and GoldsteinGoodman and colleagues (2015) comparing perinatal dyadic psychotherapy with TAU plus depression monitoring by telephone. Across both groups, maternal self-esteem increased significantly and depression and anxiety decreased significantly. Although this would suggest some potential for PIP, TAU with monitoring by phone showed equal benefit. The other, an RCT by Reference Fonagy, Sleed and BaradonFonagy and colleagues (2016), compared PIP with TAU and found that PIP led to improvements in mothers’ psychological well-being and representations of the parent–infant relationship. However, there was no difference between PIP and TAU for effect on infant development or attachment status. At the time of writing, a further two of the five studies have been completed but not yet publishedFootnote a,Footnote b and one is ongoing.Footnote c Taken at face value, these results appear to support the findings of the current review. However, further exploration is necessary.
What are implications for practitioners, commissioners and policy makers?
In interpreting these apparently somewhat disappointing results, it is important to note that where the control was TAU it does not mean that the participants in this group received ‘no treatment’; rather, participants were able to access the services usually available. In addition, as the authors of the review point out, no evidence of an effect is not the same as evidence of no effect. In other words, although the results of the review did not find strong evidence in support of PIP, it is possible that this is at least in some part due to its low statistical power. Thus, the statistics do not provide the whole picture and other factors should also be taken into account when making decisions about treatment provision.
A pertinent related issue is whether different types of intervention may be differentially effective for parents with different needs, including attachment needs. For example, Reference Bakermans-Kranenburg, Juffer and van IjzendoornBakermans-Kranenburg and colleagues (1998) compared different types of parent–infant video feedback intervention and concluded that the effectiveness of the intervention was associated with the attachment needs of the parent. However, the studies included in the Cochrane review did not explore this and it was therefore beyond the scope of the review.
PIP appears to be a promising model, but caution must be exercised, as the review did not provide conclusive evidence to suggest that PIP is more effective than other interventions. None of the studies included any cost information, so it was not possible to examine the cost-effectiveness of the interventions.
Conclusions
As none of the studies included in Barlwo and colleagues review was of more than low quality, further research will have an important impact on the confidence in the estimates of the effects of the interventions and may change these estimates. As it stands, the review provides cautious support for PIP. Further research will hopefully elucidate the active components of PIP.





eLetters
No eLetters have been published for this article.