A diet rich in fruits and vegetables reduces the risk of chronic diseases such as hypertension, CHD and stroke( Reference Boeing, Bechthold and Bub1). However, in countries like the UK(2) and the USA(Reference Kim, Moore and Galuska3), the majority of children do not eat the recommended quantities of fruits and vegetables, although fruit consumption tends to be higher than vegetable consumption. In Australia, less than 5 % of children meet vegetable intake guidelines, although 72 % meet fruit guidelines(4). Although dietary behaviour is regarded as a modifiable risk factor, it has proven difficult to modify. At an individual level, some interventions (e.g. repeated exposure) can increase fruit or vegetable intake, but effects can be small and tend to diminish over time(Reference Appleton, Hemingway and Saulais5–Reference Nekitsing, Blundell-Birtill and Cockroft7). At a population level, low fruit and vegetable intake has been largely stable in Australia over the past 20 years(Reference Magarey, Daniels and Smith8). This suggests that new approaches to dietary intervention are necessary. Early childhood, particularly the first 1000 d, is a window of opportunity to establish healthy dietary preferences(Reference Birch and Doub9–Reference Hetherington12), as food preferences are formed in infancy and track into adulthood(Reference Beckerman, Alike and Lovin10–Reference Birch, Savage and Ventura15). In particular, breast-feeding and the introduction of complementary foods can set taste preferences and shape attitudes towards food(Reference De Cosmi, Scaglioni and Agostoni11).
The flavour and composition of breast milk can vary according to the mother’s diet(Reference De Cosmi, Scaglioni and Agostoni11,Reference Barends, Weenen and Warren13,Reference Mastorakou, Ruark and Weenen16–Reference Spahn, Callahan and Spill18) , and this variety is thought to provide a flavour bridge for the infant, helping them to learn to accept variations in flavours and accustoming the infant to particular tastes(Reference Beckerman, Alike and Lovin10,Reference De Cosmi, Scaglioni and Agostoni11,Reference Birch, Savage and Ventura15,Reference Mastorakou, Ruark and Weenen16) . Infants who are fed with formula are not exposed to the same variations in flavour(Reference De Cosmi, Scaglioni and Agostoni11,Reference Mennella14,Reference Harris and Coulthard17) . Longer duration of any or exclusive breast-feeding is associated with higher fruit and vegetable intake in childhood(Reference de Lauzon-Guillain, Jones and Oliveira19–Reference Santos, AssuncAo and Matijasevich23), although associations with fruit intake are less consistent(Reference de Lauzon-Guillain, Jones and Oliveira19,Reference Okubo, Miyake and Sasaki24,Reference Specht, Rohde and Olsen25) . However, there is a great deal of variation in breast-feeding practices during the first 6 months, with some mothers exclusively breast-feeding, some supplementing with formula and/or complementary foods and some breast-feeding for less than 6 months or not at all(Reference Moss, Dobson and Tooth26). Due to the focus in research on exclusive breast-feeding(Reference Fonseca, Ribeiro and Andreoli20,Reference Santos, AssuncAo and Matijasevich23,Reference Specht, Rohde and Olsen25) , or failure to report on exclusive and mixed breast-feeding separately(Reference de Lauzon-Guillain, Jones and Oliveira19,Reference Perrine, Galuska and Thompson22) , there is little information about whether these varying breast-feeding practices are associated with fruit and vegetable consumption in childhood.
The introduction of complementary foods is another opportunity to lay the foundation for healthy eating, as infants begin to learn tastes and textures(Reference De Cosmi, Scaglioni and Agostoni11–Reference Barends, Weenen and Warren13). In the UK, there is a move towards a vegetables-first approach to weaning(Reference Chambers27,Reference Chambers, Hetherington and Cooke28) , recognising that infants are born with a preference for sweet and salty flavours but must learn to accept the bitter flavours present in many vegetables(Reference Beckerman, Alike and Lovin10,Reference Barends, Weenen and Warren13) . However, evidence to support this recommendation is lacking as many studies on the process of introducing complementary foods include the age of introduction(Reference de Lauzon-Guillain, Jones and Oliveira19,Reference Okubo, Miyake and Sasaki24,Reference Cooke, Wardle and Gibson29) , but not the infant’s first complementary food.
The aim of the present study was to investigate whether feeding practices during infancy were associated with fruit and vegetable consumption during childhood, over and above maternal fruit and vegetable consumption, which is one of the strongest predictors of child diet(Reference Nekitsing, Blundell-Birtill and Cockroft7,Reference Cooke, Wardle and Gibson29,Reference Jones, Moschonis and Oliveira30) due to observational learning from parents and availability of food within the home. Specifically, the research questions were (1) whether practices such as supplementing breast-feeding with solids and/or formula make a difference to fruit and vegetable consumption (frequency and variety), compared with exclusive breast-feeding to 6 months; (2) whether breast-feeding was associated with higher frequency and variety of fruit and vegetable consumption in childhood; and (3) whether feeding fruits or vegetables as the first complementary food was associated with higher frequency and variety of fruit and vegetable consumption in childhood.
Methods
Study design and participants
Participants for the present study were drawn from the Mothers and their Children’s Health study (MatCH)(Reference Mishra, Moss and Loos31), which is a sub-study of the Australian Longitudinal Study on Women’s Health (ALSWH)(Reference Lee, Dobson and Brown32). In 1996, a random sample of women who were representative of the Australian population were selected from the database of Australia’s universal health care system. Participants in ALSWH have completed written surveys approximately every 3 years. In 2016/2017, women in the ALSWH cohort born in 1973–1978 were asked to complete written surveys on their three youngest children aged under 13 years as part of MatCH. The eligibility criteria for MatCH were (1) consented to be contacted about sub-studies; (2) not reported infertility; and (3) not died or withdrawn (n 5799). As dietary change is rapid before 24 months of age(Reference Birch and Doub9) and eating patterns are dynamic, the present study included children aged 2–12 years (n 5471) with complete data on infant feeding and covariates (N 4981). The study received ethics approval from the University of Newcastle and The University of Queensland, and mothers provided written informed consent.
Measures
Explanatory variables
Feeding practices to 6 months were assessed in MatCH by questions adapted from the Australian National Infant Feeding Survey(33). Mothers were asked: if their child had ever received breast milk, and if so at what age this ceased; if their child had ever had infant formula and if so at what age; and at what age their child started eating solids, semi-solid and complementary foods. Based on these questions, children were classified as: breastfed less than 6 months or never (i.e. predominantly formula fed); breastfed to 6 months and supplemented with formula and/or complementary foods; or breastfed exclusively to 6 months (i.e. no formula or solids before 6 months). First complementary food was assessed by asking mothers, ‘What was the very first complementary or solid food you introduced?’ and providing a list of 16 options, as well as a free-text ‘other’ option and a ‘Can’t remember’ option. Answers were categorised as cereal, fruit, vegetables or other (e.g. meat, eggs).
Outcome variables
Child fruit and vegetable consumption was measured in MatCH using items from the Children’s Dietary Questionnaire (CDQ)(Reference Magarey, Golley and Spurrier34). Mothers were asked how frequently (0, 1, 2, 3, 4 or 5 or more times) the child ate fruit (‘Fresh, canned, stewed or dried, e.g. juice at breakfast and afternoon tea and apple at lunch is three times’) and vegetables (‘raw or cooked, e.g. salad in sandwich and vegetables for dinner is twice’) in the past 24 h. They were also asked how many different (0, 1, 2, 3, 4, 5+) vegetables (raw or cooked) and fruits (fresh, canned, stewed or dried) their child had in the past 24 h. The CDQ has been rigorously evaluated, provides a valid assessment of dietary patterns and is suitable for epidemiological studies(Reference Magarey, Golley and Spurrier34,Reference Golley, Bell and Hendrie35)
Covariates
Child-related covariates were taken from MatCH and were selected based on research showing fruit and vegetable intake can vary by age and sex(Reference Cooke, Wardle and Gibson29,Reference Bell, Ullah and Olds36) . Mothers reported the sex of the child. The child’s age was calculated from the return date of the survey and the child’s date of birth. Maternal-related covariates were taken from the ALSWH survey completed closest to MatCH and were selected based on research showing parental consumption is one of the strongest predictors of child fruit and vegetable intake(Reference Cooke, Wardle and Gibson29,Reference Jones, Moschonis and Oliveira30) , and that fruit and vegetable availability can be influenced by demographic factors, such as parental education, financial resources and area of residence(Reference de Lauzon-Guillain, Jones and Oliveira19,Reference Cooke, Wardle and Gibson29,Reference Bell, Ullah and Olds36) . Maternal fruit consumption was measured by asking mothers, ‘How many pieces of fresh fruit do you usually eat per day?’ Responses were categorised as 0–1 pieces, 2–3 pieces, and 4 or more pieces. Maternal vegetable consumption was measured by asking mothers, ‘How many serves of vegetables do you usually eat each day?’, and categorised as 0–1 serves, 2–3 serves, and 4 or more serves. Highest maternal educational qualification was categorised as up to Year 12, trade/graduate certificate or university/higher university degree. Area of residence from postcodes in ALSWH was determined using the Accessibility/Remoteness Index of Australia (Aria+)(Reference Glover and Tennant37) and categorised as major city, inner regional or outer regional/remote/very remote. Difficulty managing on income was categorised as easy, not too bad, difficult sometimes and difficult all the time/impossible.
Statistical analyses
Statistical analysis was conducted using SAS version 9.4 (SAS Institute Inc.). Initial descriptive statistics were calculated for the overall sample, along with means for the outcome variables by categories of the explanatory variables. An a priori power analysis was calculated for the funding application for the overall MatCH study, which projected that with 3500 mothers, a family level variable that explained 20 % of the variance in the outcome of interest would have power of 0·77 for a one-child family and 0·97 for a two-child family.
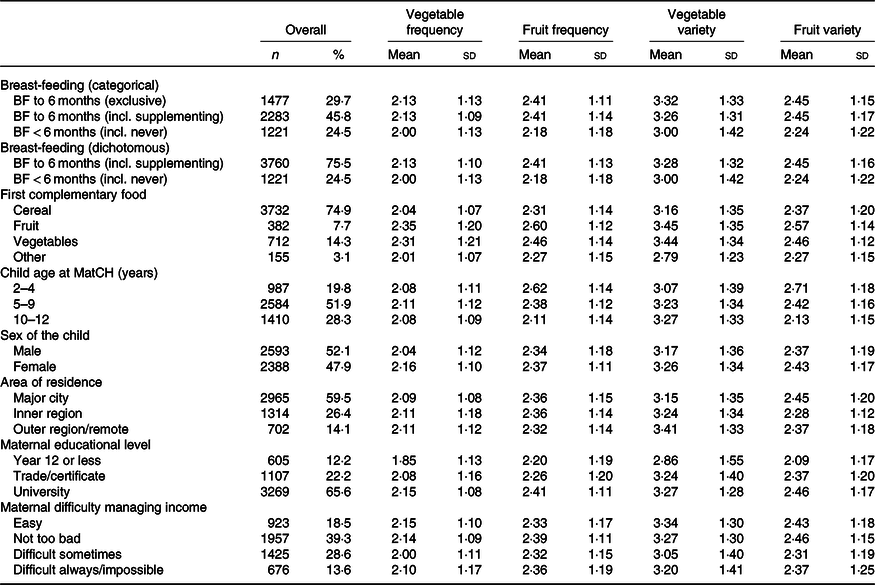
Forest plots were used to examine the means and 95 % CI for fruit and vegetable frequency and variety for children who were exclusively breastfed and those who were supplemented. The supplemented group was separated out as a sensitivity analysis to check that these two groups could be combined for analysis (Research Question 1).
To investigate whether breast-feeding practices and first complementary food were associated with the outcome variables, over and above maternal fruit and vegetable consumption (Research Questions 2 and 3), a series of linear regression models was run, using generalised estimating equations to account for clustering of children within mothers. (Note that due to the wide range of ages among the children and evidence that fruit and vegetable consumption differ by age(Reference Cooke, Wardle and Gibson29,Reference Golley, Hendrie and McNaughton38) , moderation analyses by age were conducted in univariate regression models. However, moderation analyses were all statistically non-significant at P < 0·05, suggesting stratification by age was not necessary.) The first model included breast-feeding and complementary feeding practices, the second model added maternal fruit and vegetable consumption, the third model added child covariates and the final model added maternal covariates. This series of models was repeated for each of the four outcome variables.
Results
Demographic characteristics
In the overall sample, 3·9 % of children (n 193) were never breastfed, 15·0 % (n 745) were breastfed for 3 months or less, 8·2 % (n 410) stopped breast-feeding at 6 months and 67·3 % (n 3351) were breastfed for more than 6 months. Complementary foods were introduced at 6 months for 46·3 % (n 2304) of children, at 5 months for 23·8 % (n 1183) and at 4 months for 20·9 % (n 1039). One-third of children (34·0 %, n 1695) never had formula. Of those who did, half (50·9 %, n 1673) first drank formula before 3 months.
Demographic characteristics are in Table 1. The majority of children were breastfed to 6 months (75·5 %). The first complementary food for most children was cereal (74·9 %), with only 22 % given fruits or vegetables. The majority of children lived in major cities (59·5 %) and had a mother with a university education (65·6 %). On average, children were aged 7·36 (sd 2·90) years. In the last 24 h, on average children ate vegetables 2·10 (sd 1·11) times and fruits 2·35 (sd 1·14) times and ate 3·21 (sd 1·35) different vegetables and 2·40 (sd 1·18) different fruits.
Table 1. Demographic characteristics of mothers and children and fruit and vegetable consumption by each demographic characteristic (n 4981)
(Mean values and standard deviations; numbers and percentages)
BF, breastfed; incl., including; MatCH, Mothers and their Children’s Health Study.
Supplementing v. exclusive breast-feeding
The means for children who were supplemented and children who were exclusively breastfed were identical for vegetable frequency, fruit frequency and fruit variety (three-category variable, Figs. 1–4). Mean vegetable variety was slightly higher for children who were exclusively breastfed (mean = 3·32) compared with children who were supplemented (mean = 3·26); however, the overlapping CI indicated this difference was not statistically significant and in practical terms the difference was not meaningful. This suggested that supplementing with formula and/or complementary foods before 6 months was not associated with any differences in childhood fruit and vegetable frequency and variety, compared with exclusive breast-feeding (Research Question 1).
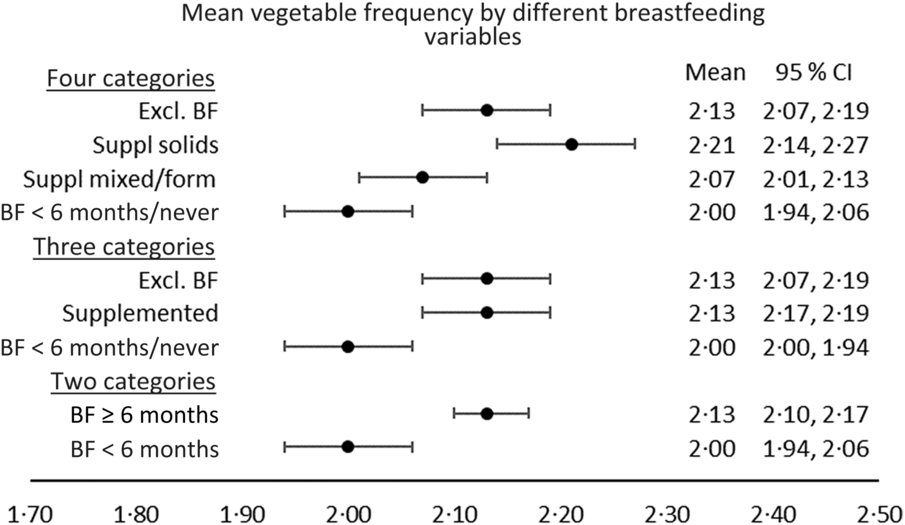
Fig. 1. Mean values and 95 % confidence intervals for vegetable frequency, by different categorisations of breast-feeding. Excl. BF, exclusively breastfed; Suppl solids, supplemental solids; Suppl mixed/form, supplemental mixed/formula; BF, breastfed.
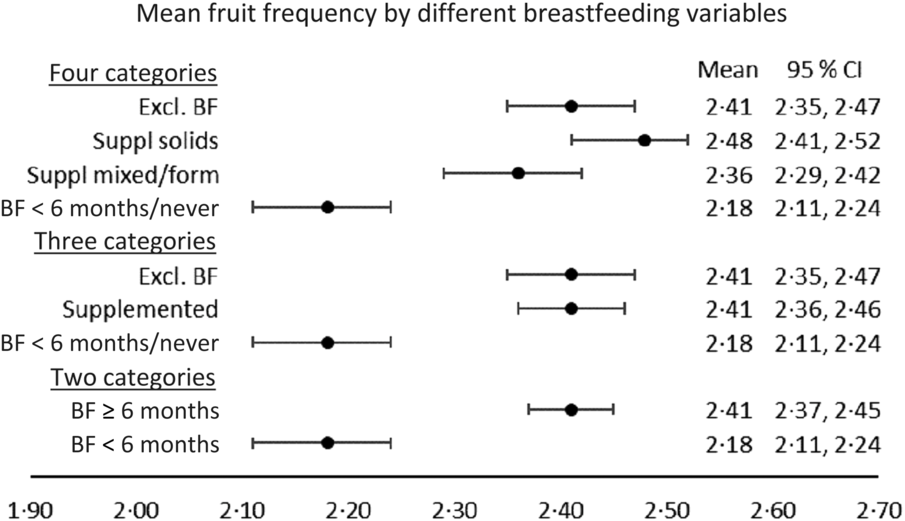
Fig. 2. Mean values and 95 % confidence intervals for fruit frequency, by different categorisations of breast-feeding. Excl. BF, exclusively breastfed; Suppl solids, supplemental solids; Suppl mixed/form, supplemental mixed/formula; BF, breastfed.
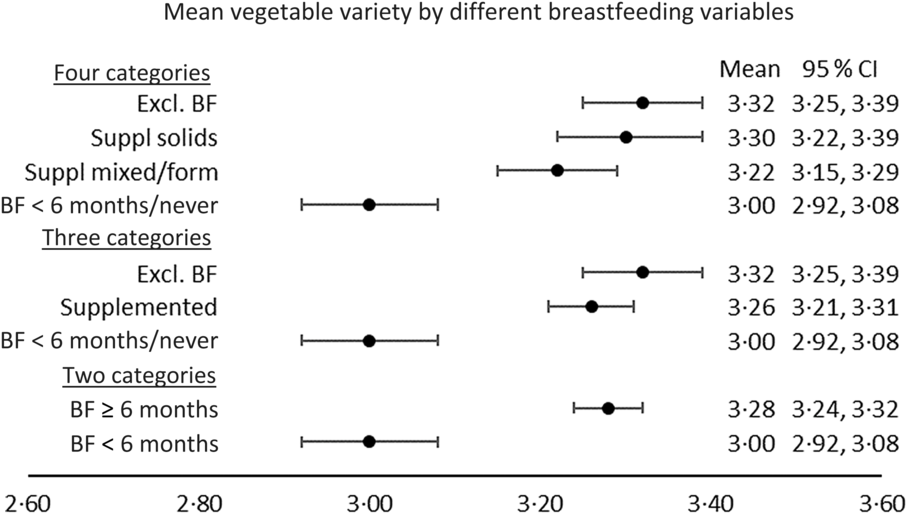
Fig. 3. Mean values and 95 % confidence intervals for vegetable variety, by different categorisations of breast-feeding. Excl. BF, exclusively breastfed; Suppl solids, supplemental solids; Suppl mixed/form, supplemental mixed/formula; BF, breastfed.
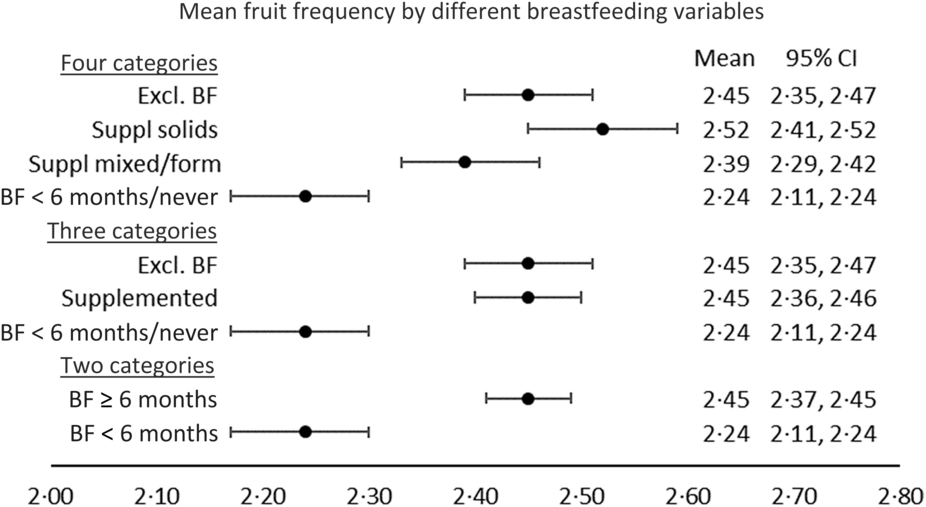
Fig. 4. Mean values and 95 % confidence intervals for fruit variety, by different categorisations of breast-feeding. Excl. BF, exclusively breastfed; Suppl solids, supplemental solids; Suppl mixed/form, supplemental mixed/formula; BF, breastfed.
As a sensitivity analysis, the children who were supplemented were separated into those supplemented with complementary foods and those supplemented with formula or with both formula and complementary foods (four-category variable, Figs. 1–4). Means were slightly higher on every variable for children supplemented with complementary foods than children supplemented with formula or with both formula and complementary foods. However, the CI for the two groups overlapped on every variable except vegetable frequency, and differences in the means were small, suggesting there was no evidence for differences between the two groups of children who were supplemented. The two groups of children who received 6 months of breast milk (the group that was exclusively breastfed and the group that was supplemented) were combined for the remaining analyses (two-category variable, Figs. 1–4).
A series of regression models (Tables 2 and 3) found that first complementary food was more consistently associated with the frequency and variety of fruit and vegetable consumption in childhood, compared with breast-feeding (Research Questions 2 and 3), with results for each outcome variable detailed below.
Table 2. Associations between feeding practices in infancy and the frequency of vegetable and fruit intake in childhood (n 4981)
(Linear regression coefficients and 95 % confidence intervals)
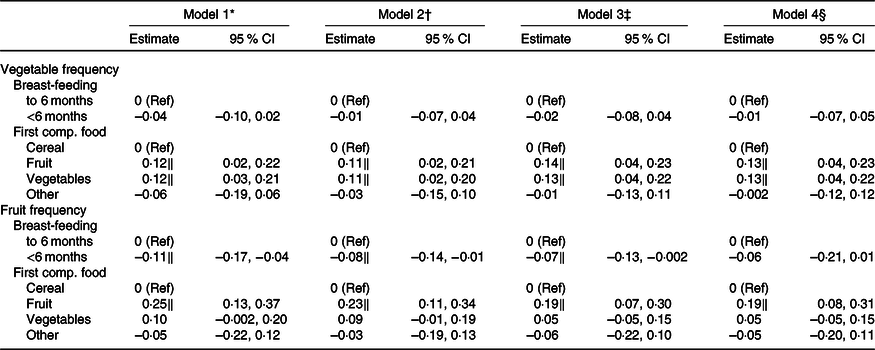
Ref, reference; comp., complementary.
* Model 1 included only breast-feeding and first complementary food.
† Model 2 added maternal fruit and vegetable consumption.
‡ Model 3 added the child’s age and sex.
§ Model 4 added area of residence, as well as maternal educational level and difficulty managing on income.
‖ Values indicate that the CI does not contain 0.
Table 3. Associations between feeding practices in infancy and the variety of vegetables and fruit consumed in childhood (n 4981)
(Linear regression coefficients and 95 % confidence intervals)
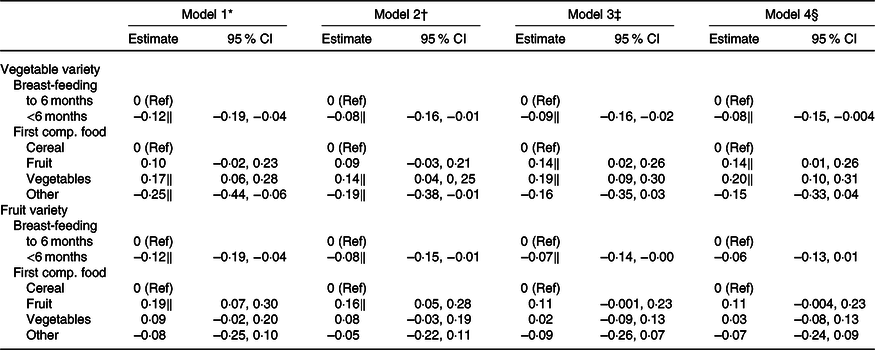
Ref, reference; comp., complementary.
* Model 1 included only breast-feeding and first complementary food.
† Model 2 added maternal fruit and vegetable consumption.
‡ Model 3 added the child’s age and sex.
§ Model 4 added area of residence, as well as maternal educational level and difficulty managing on income.
‖ Values indicate that the CI does not contain 0.
Frequency of vegetable consumption
Breast-feeding duration was not associated with the frequency of childhood vegetable intake (Table 2), but first complementary food was, even after accounting for maternal diet and child and maternal covariates. Children who were given fruits or vegetables as their first complementary food ate vegetables more frequently on average than children given cereal.
Frequency of fruit consumption
Being breastfed for less than 6 months was associated with lower frequency of childhood fruit intake compared with being breastfed for 6 months, although the magnitude of the effect reduced after accounting for maternal diet and child covariates (Table 2). First complementary food was also associated with frequency of childhood fruit intake, even after accounting for maternal diet and child and maternal covariates. Children given fruit (but not vegetables) as their first complementary food ate fruit more frequently on average than children given cereal.
Vegetable variety
Being breastfed for less than 6 months was associated with less vegetable variety in childhood compared with being breastfed for 6 months, even after accounting for maternal diet and child and maternal covariates (Table 3). First complementary food was also associated with vegetable variety, even after accounting for maternal diet and child and maternal covariates. Children who were given vegetables (but not fruit) as their first complementary food ate a wider variety of vegetables on average than children who were given cereal.
Fruit variety
Being breastfed for less than 6 months was associated with less fruit variety in childhood compared with being breastfed for 6 months, although the magnitude of the effect reduced after controlling for maternal diet and child covariates (Table 3). Children who were given fruit as their first complementary food ate a wider variety of fruits on average than children who were given cereal; however this association reduced in magnitude once child covariates were added to the model.
Discussion
The aim of the present study was to investigate the associations between feeding practices in infancy and the frequency and variety of fruit and vegetable consumption in childhood. It found that breast-feeding to 6 months was associated with greater vegetable variety in childhood, compared with being breastfed for less than 6 months or never. Associations with fruit frequency and variety attenuated after adjustment for demographic characteristics. First complementary food was a more consistent predictor of fruit and vegetable consumption. Compared with having cereal as a first complementary food, having fruits or vegetables was associated with more frequent consumption of fruits and vegetables in childhood as well as a greater variety of vegetables, although it was not associated with fruit variety. Additionally, there were no real differences in the frequency and variety of fruit and vegetable consumption between children who were exclusively breastfed to 6 months and children who were breastfed to 6 months and supplemented with formula and/or complementary foods. These findings have important implications for infant feeding guidelines.
In our study, being breastfed for 6 months was associated with children eating a wider variety of vegetables in childhood, compared with children who were breastfed for less than 6 months or never breastfed. Breast-feeding was not associated with vegetable frequency, and initial associations with fruit frequency and variety attenuated after adjustment for demographic covariates. This is inconsistent with studies that have found breast-feeding is associated with higher fruit and/or vegetable intake in childhood(Reference de Lauzon-Guillain, Jones and Oliveira19,Reference Fonseca, Ribeiro and Andreoli20,Reference Perrine, Galuska and Thompson22–Reference Specht, Rohde and Olsen25,Reference Cooke, Wardle and Gibson29) . However, some categorisations of breast-feeding duration differed from ours, as did the age range of the children, some studies did not include maternal fruit and vegetable intake, and breast-feeding became statistically non-significant in some multivariable models. An experimental study(Reference Maier-Noth, Schaal and Leathwood39) found that breast-feeding was not associated with the frequency of vegetable consumption rated by mothers, but it was associated with consuming more of a new vegetable and being more willing to taste offered vegetables in an experimental setting. This supports our finding that breast-feeding was associated with higher vegetable variety but not frequency and provides some support for the hypothesis that breast-feeding accustoms children to a greater variety in tastes, compared with formula feeding(Reference Beckerman, Alike and Lovin10,Reference De Cosmi, Scaglioni and Agostoni11,Reference Birch, Savage and Ventura15–Reference Harris and Coulthard17) . Our findings suggest longer duration of breast-feeding is associated with greater receptiveness to variety. Future research should test this in samples that include a higher percentage of children who were never breastfed. It also suggests that future research may benefit from incorporating broader measures of fruit and vegetable intake than just frequency, such as variety and willingness to taste new vegetables.
In our study, there was no difference in the frequency and variety of fruit and vegetable consumption in childhood between children who were exclusively breastfed to 6 months, and children who received 6 months of breast milk and were supplemented with formula and/or solids. Exclusive breast-feeding to 6 months is recommended by the WHO(40). However, some country-based guidelines differ. For example, guidance in Australia and Britain suggest introducing complementary foods at about 6 months based on cues for developmental readiness(41,42) , which occurs between 4 and 6 months(Reference Fewtrell, Wilson and Booth43). Our findings suggest that it may be appropriate to introduce complementary foods prior to 6 months(Reference Schwartz, Scholtens and Lalanne44), and public health messages could inform parents on signs of developmental readiness(Reference Schwartz, Scholtens and Lalanne44,45) . However, these findings are specific to future fruit and vegetable intake and advantaged areas of high-income countries and may not apply to other childhood outcomes (e.g. cognition), or to disadvantaged communities.
In our study, first complementary food was a more consistent predictor than breast-feeding of future fruit and vegetable frequency and vegetable variety. This is consistent with the view that complementary feeding, but not breast-feeding, is essential to acceptance of a wider range of food(Reference Harris and Coulthard17), although to maintain the effects vegetables need to be part of the ongoing family diet(Reference Hetherington12,Reference Birch, Savage and Ventura15) . Exposure to vegetables was generally more strongly associated with vegetable-related outcomes, and vice versa for fruit. As it seems more difficult to encourage children to eat more vegetables than to eat more fruits, these findings support policy initiatives encouraging a vegetables-first approach to weaning(Reference Chambers27,Reference Chambers, Hetherington and Cooke28) . This may require updating infant feeding guidelines and targeted public health messages, as the most common first food given to infants in many countries is cereal(Reference Hetherington12,Reference Chambers27,Reference Chambers, Hetherington and Cooke28,Reference Caton, Ahern and Hetherington46) .
Our study had several strengths. These included a large national sample, inclusion of a novel explanatory variable (i.e. first food) and inclusion of key covariates, such as maternal diet. The present study also had several limitations. The sample included a higher percentage of children who received 6 months of breast milk than reported in other Australian studies: 75·5 % compared with 42–62 %(33,47–49) . This is probably due to the high proportion of mothers in our study with a university education (65·6 %), which may affect the generalisability of the findings. Duration of breast-feeding and first complementary food were retrospectively recalled; however, our previous work has found that breast-feeding to 6 months was recalled with more than 90 % accuracy when comparing measures in MatCH with measures in ALSWH, which were completed within 3 years of the child’s birth(Reference Moss, Dobson and Tooth26). First complementary food was not asked in ALSWH so we were unable to cross-check this variable; however, we did include a ‘Can’t remember’ option in the list of potential first foods, and children where this option was selected were not included in the analysis. The CDQ did not include fruit and vegetable quantities or typical consumption (rather than consumption in the last 24 h), which would have been useful for the analysis and should be considered for future research. Finally, while parents provide the food environment for the child, both parents and children can be influenced by community- and macro-level factors, such as the media, food availability, cultural norms and food policy(Reference Beckerman, Alike and Lovin10,Reference Scaglioni, De Cosmi and Ciappolino50) . While consideration of these factors was beyond the scope of the present study, we acknowledge the importance of the wider context in dietary assessment.
Conclusion
Infancy is an important window of opportunity for dietary intervention, as feeding practices can shape food tastes and preferences and may influence fruit and vegetable intake later in life. We found stronger evidence for the role of complementary feeding than for breast-feeding on childhood vegetable and fruit intake. Our findings suggest that guidance to parents on infant feeding could encourage a vegetables-first approach or at the least encourage the provision of fruits and vegetables rather than cereal at the early stages of the weaning process.
Acknowledgements
The research on which this paper is based was conducted as part of the Australian Longitudinal Study on Women’s Health by the University of Queensland and the University of Newcastle. We are grateful to the Australian Government Department of Health for funding and to the women who provided the survey data. We are also grateful to Dr Megan Ferguson for constructive and expert feedback on the draft manuscript, and to Colleen Loos for excellent data management.
ALSWH is funded by the Australian Government Department of Health. MatCH is funded by the National Health and Medical Research Council (NHMRC) project grant (APP1059550). G. D. M. is supported by an NHMRC Principal Research Fellowship (APP1121844). The funders had no role in the design, analysis or writing of this article.
K. M. M. and G. D. M. designed the present study and devised the research questions (G. D. M., A. J. D. and L. T. designed the overall MatCH and ALSWH studies). G. D. M., A. J. D. and L. T. supervised data collection and management of MatCH and ALSWH. K. M. M. analysed the data and wrote the manuscript. G. D. M., A. J. D. and L. T. assisted in interpreting results and provided critical input on draft manuscripts. All authors read and approved the final manuscript.
The authors declare that there are no conflicts of interest.










