The development of compact ECMO consoles and simpler circuits has made the transfer of patients supported with ECMO easier. However, there are still risks, including cannula dislodgement, console failure and bleeding.
The majority of patients requiring ECMO support will need to be transferred. This may only be to the operating room or the CT scan room within the hospital, or it may be from a referring centre to a unit able to provide ECMO support. It is possible for patients supported with ECMO to be moved from hospital to hospital, having been stabilized before transfer.
Some countries have set up networks based on a small number of high-volume centres working together to provide safe and efficient ECMO transfer. Clear guidelines and good communication between team members minimize the risk. All transfers require specific equipment, specially trained staff and planning to avoid potential mishap.
Planning
All transfers of patients on ECMO requires planning. Careful documentation is required and checklists are helpful.
Patients should be stabilized before transfer. This will require time. All lines should be secured. Non-essential medications should be interrupted. Replacement syringes must be prepared. Drugs and fluids that will need to be administered during transfer should be prepared and ready to be given when appropriate.
Emergency equipment should be checked before transfer. All batteries should be fully charged, and spares available when appropriate (power cables should accompany the patient).
Transfer team
Personnel included in the transfer of patients on ECMO vary from centre to centre. The team should be led by an intensive care doctor trained in the transfer of the critically ill patient. A person with intimate knowledge of the ECMO circuit, and trained in handling complications such as air embolism or circuit leakage, should accompany the patient at all times.
When retrieving patients not yet on ECMO, the doctor should have experience in cannulating and commencing ECMO support.
The team leader is responsible for the safety of team members and the patient during transfer. The team leader ensures communication between all team members to minimize the risk of complications.
Coordination at the ECMO centre is very important, ensuring that all runs smoothly. This includes being prepared for the team’s return.
Transfer equipment
Transferring a patient on ECMO requires much specialized equipment. Patients are usually attached to a ventilator, multiple pieces of monitoring equipment with associated connections and multiple infusion pumps with associated indwelling vascular lines. All are critical to life and cannot be disconnected.
Patients can be transferred on a critical care bed, with modifications to accommodate the equipment described above plus the components of the ECMO circuit and required gas cylinders.
A transfer trolley can be modified to accommodate the ECMO consoles, oxygenator and circuit (Figure 10.1). Newer ECMO consoles often have specially designed transfer trolleys with fixation for the motor, console, oxygenator and O2 cylinders. The extra weight needs to be taken into account, as this may limit the weight of the patient the trolley can support.
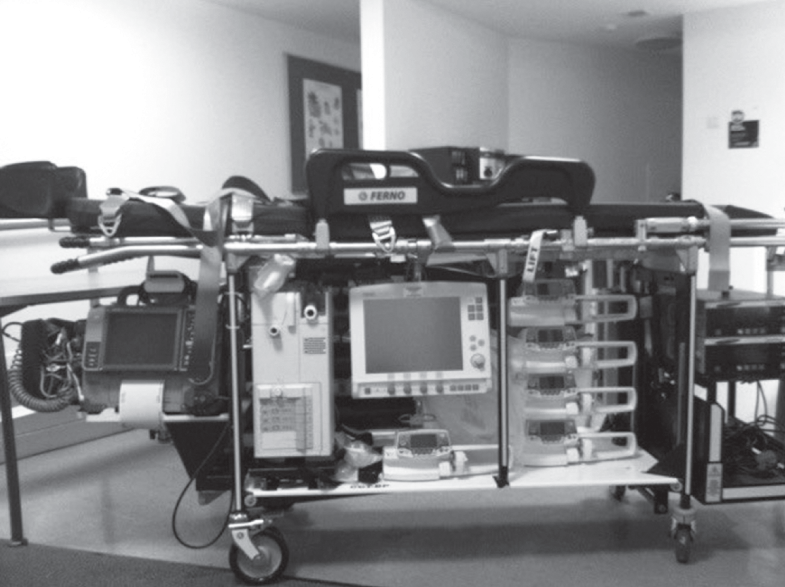
Figure 10.1 A transfer trolley modified to include ECMO consoles.
Appropriate mattresses are required in patients with a high risk of skin damage.
Replacement equipment is required in case of unexpected failure. This should include a back-up pump, driven either electrically or manually. A spare oxygenator and circuit are necessary.
Other resuscitation equipment such as suction systems and defibrillator are required.
Adequate power and an O2 supply are required for the duration of the transfer. This means that vehicles or aircraft may need to be modified to accommodate the extra gas requirements, or be able to deliver the proper current. In vehicles, all equipment has to be secured to protect staff and patients.
When planning to cannulate and commence the ECMO in another hospital, the team needs to have enough equipment to accommodate the needs of the patient, including a variety of cannulas. All the equipment should be ready at all times, and checklists used to ensure nothing is missing.
Checklists should be available to support the team. This includes a World Health Organization insertion checklist to be used before inserting the cannula.
Care during transfer
Patient vital signs should be monitored during transfer. This includes heart rate and rhythm, blood pressure, O2 saturation, end-tidal CO2, temperature and pupil reaction.
The ECMO circuit must be monitored; this includes circuit pressure, sweep gas and pump flow monitoring. All observations should be regularly documented. Portable devices allow monitoring of blood gases and coagulation during long transfers.
Transfer by air
The advantage of air transfer is reduced journey time. This is essential in some countries. Transfer by air is more expensive than by road, with helicopter usually being the most expensive form of transfer. Staff require special training.
The logistical and organizational requirements often mean that it is impractical if the planned journey is less than 2 h, as transferring between several vehicles is often required. Very few hospitals have an airstrip in their grounds, but many have a helipad close by.
Space is often limited, as well as the mode of entry to the cabin. Patients on ECMO may not fit through the door or in the cabin of an aircraft. Pressure bags should be available as the space in the cabin does not usually allow infusion by gravity. Acceleration, deceleration and frequent bumps during flight can all disturb the patient, equipment and infusions.
With altitude, gas will expand. This may affect a pneumothorax and other bubbles in the patient or the ECMO circuit. The endotracheal tube cuff should be filled with saline to avoid hyperinflation and tracheal damage. The balloon of a pulmonary artery catheter should be emptied. The altitude will affect the gas-exchange capacity of the membrane.
If using a helicopter, the noise level is very high. Auscultation is not possible. Audible monitoring appears silent. Conversation is impossible without aid. All patients should have earplugs.
The safety of the team is paramount, and flying should never be attempted if the pilot thinks it is inappropriate.
Key points
Transferring the patient on ECMO aims to ensure continuity of intensive care support during the whole journey.
Transferring on ECMO has risks and requires planning and communication.
Air transport is possible, but space is often limited and limiting.