In many countries the oldest age groups have the highest suicide rates (Reference Manton, Blazer and WoodburyManton et al, 1987; Reference De LeoDe Leo, 2001). Suicide frequencies differ with regard to age, and the suicide rate of the very old population (80 years and over) has not followed the declining trend of that of the old (65-79 years) (Reference Erlangsen, Bille-Brahe and JeuneErlangsen et al, 2003). However, the reasons for these differences are unknown. Psychiatric disorder, especially affective disorder, is strongly associated with suicide among the elderly (Reference Henriksson, Marttunen, Isometsä, Pearson and ConwellHenriksson et al, 1996; Reference Conwell, Lyness and DubersteinConwell et al, 2000; Reference Harwood, Hawton and HopeHarwood et al, 2001; Reference Waern, Runeson and AllebeckWaern et al, 2002). Duberstein et al (Reference Duberstein, Conwell and Conner2004) found a peak in the suicide risk during the active period of psychiatric disorders for older individuals. Nevertheless, the suicide risk associated with psychiatric hospitalisation may vary between the old and the very old population groups.
The aim of our study was to investigate the suicide risk associated with psychiatric hospitalisation and whether it varies with regard to age among elderly people.
METHOD
The study population consisted of everyone aged 50 years or above living in Denmark during the period 1994-1998. Information on each individual was available through data registers. As each person in Denmark has a unique personal identifier which is registered in various administrative registers, data from different registers can be linked on an individual basis (Reference FrankFrank, 2000). Demographic data on gender, age and dates of immigration and emigration were derived from the Register of Population Statistics (Eurostat, 1995). The Registry of Causes of Death (Reference Juel and Helweg-LarsenJuel & Helweg-Larsen, 1999) provided information on suicides and other causes of deaths, and data on psychiatric hospitalisations were obtained from the Danish Psychiatric Central Register (Reference Munk-J⊘rgensen and MortensenMunk-Jørgensen & Mortensen, 1997). The latter contains exact dates and diagnoses for the entire population on all full-time admissions to psychiatric hospitals from 1969 onwards.
The observation period was 1 January 1994 to 31 December 1998. People who reached the age of 50 years or migrated to Denmark during this period entered the study population at the time of these events. Emigrants were right-censored at the date of leaving the country. The event of interest was completed suicide, which was defined according to ICD-10 criteria (World Health Organization, 1992). Deaths due to other causes during the study period were censored at date of death.
Time-varying covariates
Four time-varying covariates were included in the analyses. The variable on current age of each person included in the study was grouped into three categories: middle-aged (50-64 years), old (65-79 years) and very old (≥80 years). This variable was updated whenever someone changed age group. Another covariate denoted the current hospitalisation status of each individual, categorised as not hospitalised, previously hospitalised and currently hospitalised. This variable was updated on the date when an individual was hospitalised or discharged. Information on previous hospitalisation prior to the start of the study was limited to the coverage of the Danish Psychiatric Central Register, which dates back to 1969. Similar to hospitalisation status, a third variable was created, which reflected whether the patient had been diagnosed with an affective disorder or another type of psychiatric disorder during hospitalisation. Last, a covariate covered the time since last admission or discharge at any given point during the study period.
Event-history analysis
We applied event-history analysis by fitting proportional hazard models. This method allows us to calculate the relative risk for the different levels of the analysed factors and at the same time control for compositional changes. In the case of two covariates x and y, the proportional hazard models can be written as:
where m i (t) is the risk that individual i will complete suicide at time t and g(t) is the baseline, where t represents the time since entry into study. Since current age was included as a time-varying covariate, the baseline was fixed to the value of zero throughout the observation time. The coefficient a jk is estimated for specific combinations of level j of variable x and level k of variable y. For instance, variable x could denote current age while variable y could be current hospitalisation status of individual i at time t. A 54-year-old person who at time t is in a psychiatric hospital would be included in the analysis with covariate x having the value 'middle-aged' and covariate y having the value 'currently hospitalised'. Whenever an individual experienced a change of status the value of the respective covariate was updated. In the above example there are 6 (3×2) possible combinations of the covariates' values, which are all logically sound. One of these combinations is set as the reference group and the suicide risk of each of the other combinations is calculated relative to this reference group. The risks are based on estimates of a jk . For further details on the method, see Hoem (Reference Hoem1993, Reference Hoem1997). The differences in suicide risks were analysed in separate models for men and women and we calculated the 95% confidence intervals of the estimates.
Data management was carried out using the SAS system package (SAS Institute, 2001) and proportional hazard estimates were obtained using the AML software program (see Reference Lillard and PanisLillard & Panis, 2000). Both programs were operated on a UNIX platform at Statistics Denmark (Sun Microsystems, 1999).
RESULTS
In all, 1 978 527 persons (918 452 men and 1 060 075 women) were included in the study. The study population was observed during 8.3 million person-years: 3.8 million person-years for men and 4.5 million person-years for women (Table 1). During the 5 years of the study, 2323 persons (1494 men and 829 women) died by suicide.
Table I Distribution in person-years of the study population during the period 1994-1998 according to psychiatric hospitalisation
| Study population | |||||||
|---|---|---|---|---|---|---|---|
| All (person-years) n(%) | Previous hospitalisation 1 (person-years) n(%) | Currently hospitalised (person-years) n(%) | Previously or currently hospitalised (person-years) n(%) | ||||
| Men | |||||||
| 50-64 years | 2 199 611 (58.1) | 117 422 (64.7) | 1374 (55.8) | 118 796 (64.6) | |||
| 65-79 years | 1 276 106 (33.7) | 54895 (30.2) | 799 (32.4) | 55 694 (30.3) | |||
| 80+ years | 311 512 (8.2) | 9238 (5.1) | 291 (11.8) | 9530 (5.2) | |||
| All (50+ years) | 3 787 228 (100) | 181 556 (100) | 2464 (100) | 184 020 (100) | |||
| Women | |||||||
| 50-64 years | 2 227 421 (49.5) | 153 859 (51.9) | 1953 (46.1) | 155 812 (51.8) | |||
| 65-79 years | 1 621 604 (36.1) | 109 173 (36.8) | 1636 (38.6) | 110 809 (36.8) | |||
| 80+ years | 647 241 (14.4) | 33 629 (11.3) | 648 (15.3) | 34276 (11.4) | |||
| All (50+ years) | 4 496 266 (100) | 296 661 (100) | 4237 (100) | 300 898 (100) | |||
1. Person-years in the study period for those who had been hospitalised at least once since 1969.
As shown in Table 2, the percentage of very old people who died by suicide was higher than would be expected from the percentage of people in this age group in the study population (see Table 1), especially for men. However, only a small proportion of very old people who completed suicide had at some point been hospitalised. Although approximately 37% and 61% respectively of the middle-aged men and women who took their own lives had been in a psychiatric hospital at some point since 1969, only 12% and 22% of very old men and women had been hospitalised.
Table 2 Suicides among all men and women in Denmark aged 50 years and over during the period 1994-1998, and psychiatric hospitalisations
| Suicides during observation period (1994-1998) | |||||||
|---|---|---|---|---|---|---|---|
| All n (%) | Previous 1 hospitalisation n (%) 2 | Current hospitalisation n (%) 2 | Previous and current hospitalisation n (%) 2 | ||||
| Men | |||||||
| 50-64 years | 720 (48.2) | 239 (33.2) | 24 (3.3) | 263 (36.5) | |||
| 65-79 years | 525 (35.1) | 114 (21.7) | 15 (2.9) | 129 (24.6) | |||
| 80+ years | 249 (16.7) | 25 (10.0) | 4 (1.6) | 29 (11.6) | |||
| All (50+ years) | 1494 (100) | 378 (25.3) | 43 (2.9) | 421 (28.2) | |||
| Women | |||||||
| 50-64 years | 361 (43.5) | 192 (53.2) | 27 (7.5) | 219 (60.7) | |||
| 65-79 years | 318 (38.4) | 130 (40.9) | 20 6.3) | 150 (47.2) | |||
| 80+ years | 150 (18.1) | 29 (19.3) | 4 (2.7) | 33 (22.0) | |||
| All (50+ years) | 829 (100) | 351 (42.3) | 51 (6.2) | 402 (48.5) | |||
1. Suicides among people who had been hospitalised at least once since 1969.
2. Percentage of all suicides in that age group.
Table 3 sets out the relative suicide risk with regard to hospitalisation status. The suicide risks were calculated relative to middle-aged people who had never been admitted to hospital with a psychiatric diagnosis (since 1969). People with a history of psychiatric hospital admission have - regardless of age and gender - significantly higher suicide risks than people with no such history. The highest risks are found among people currently admitted to psychiatric hospital. Middle-aged women who were currently hospitalised had an almost 200-fold higher suicide risk than those never hospitalised. People who had never been hospitalised experienced an increasing risk relative to increasing age; however, this trend was reversed in those who had been in psychiatric hospital. This opposing trend was particularly pronounced among women. Consequently, when the distribution of risks was compared within each age group, the increase in risk associated with hospitalisation was smaller among the very old than among the younger age groups. Being previously hospitalised increased the suicide risk by a factor of 4 (12.3/3.3) and 5 (12.6/2.8) among very old men and women, respectively, compared with a factor of 9 (9.2/1) and 18 (18.2/1) among middle-aged men and women. Very old people currently hospitalised experienced a 19-fold (62.5/3.3) and 32-fold (90.1/2.8) higher risk compared with never-hospitalised men and women respectively. The corresponding risk among the middle-aged group increased by a factor of 82 and 199 for men and women, respectively. It should be taken into account that very few of those aged 80 years or over completed suicide while they were in hospital. Nevertheless, the interaction effect between age and psychiatric hospitalisation was highly significant (P<0.0001).
Table 3 Suicide risks by age for men and women never, previously or currently hospitalised with a psychiatric diagnosis, 1994-1998
| Age group (years) | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| 50-64 | 65-79 | 80+ | |||||||||
| Risk | n (95% Cl) | Risk | n (95% Cl) | Risk | n (95% Cl) | ||||||
| Men | |||||||||||
| Never hospitalised | 1.0 1 | 457 | 1.5 | 396 (1.3-1.7) | 3.3 | 220 (2.8-3.9) | |||||
| Previously hospitalised | 9.2 | 239 (7.9-10.8) | 9.5 | 114 (7.7-11.6) | 12.3 | 25 (8.2-18.4) | |||||
| Currently hospitalised | 82.4 | 24 (55.1-123.1) | 85.3 | 15 (51.2-142.1) | 62.5 | 4 (23.5-166.1) | |||||
| Women | |||||||||||
| Never hospitalised | 1.0 1 | 142 | 1.6 | 168 (1.3-2.0) | 2.8 | 117 (2.2-3.6) | |||||
| Previously hospitalised | 18.2 | 192 (14.7-22.6) | 17.3 | 130 (13.6-21.9) | 12.6 | 29 (8.4-18.8) | |||||
| Currently hospitalised | 198.8 | 27 (131.9-299.8) | 184.8 | 20 116.8-292.4) | 90.1 | 4 (33.4-242.5) | |||||
1. Reference group.
Among those with a history of psychiatric hospitalisation, the highest relative suicide risk was found among those who at least once had been diagnosed with an affective disorder (Table 4). This seemed to be more pronounced among women than men. Again, the highest risk was found among those currently in hospital with a diagnosis of affective disorder, although the estimates are based on few suicides among the very old.
Table 4 Suicide risks by age and psychiatric diagnosis given during hospitalisation, 1994-1998
| Age group (years) | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| 50-64 | 65-79 | 80+ | |||||||||
| Risk | n(95%CI) | Risk | n(95%CI) | Risk | n(95%CI) | ||||||
| Men | |||||||||||
| Never hospitalised | 1.0 1 | 457 | 1.5 | 396 (1.3-1.7) | 3.3 | 220 (2.8-3.9) | |||||
| Previous affective disorder | 17.1 | 63 (13.1-22.3) | 18.6 | 54 (14.1-24.7) | 24.2 | 15 (14.5-40.4) | |||||
| Previous other disorder | 7.9 | 176 (6.7-9.4) | 6.6 | 60 (5.0-8.6) | 7.1 | 10 (3.8-13.3) | |||||
| Current other disorder | 177.3 | 15 (107.5-292.4) | 177.0 | 13 (97.6-320.9) | 78.5 | 1 (11.1-555.5) | |||||
| Current other disorder | 42.5 | 9 (22.0-81.8) | 35.3 | 2 (13.2-94.0) | 58.6 | 3 (19.0-180.7) | |||||
| Women | |||||||||||
| Never hospitalised | 1.0 1 | 142 | 1.6 | 168 (1.3-2.0) | 2.8 | 117 (2.2-3.6) | |||||
| Previous affective disorder | 32.7 | 70 (24.6-43.6) | 23.7 | 56 (17.4-32.3) | 18.4 | 16 (11.0-30.9) | |||||
| Previous other disorder | 14.5 | 122 (11.4-18.5) | 14.3 | 74 (10.8-18.9) | 9.0 | 13 (5.1-16.0) | |||||
| Current affective disorder | 340.0 | 22 (211.1-547.6) | 236.4 | 15 (136.5-409.4) | 112.8 | 2 (28.0-454.4) | |||||
| Current other disorder | 102.4 | 5 (50.2-208.6) | 130.4 | 5 (60.6-280.8) | 75.0 | 2 (18.7-301.3) | |||||
1. Reference group.
Figure 1 displays the risks of suicide, logarithm of the hazard, at different lengths of time following hospital admission or discharge. During the first week following an admission to or a discharge from a psychiatric hospital, significantly higher risks are found compared with people not in hospital or people who had been discharged for a long period, respectively. In the first week after discharge the suicide risk is significantly higher than during the subsequent weeks, for all age groups. Nonetheless, any time after a discharge is associated with a higher risk than for people never hospitalised. We found no significant difference in the risk pattern with regard to age.
DISCUSSION
This is the first study to examine the suicide risks associated with psychiatric hospitalisation among the whole older adult population of a country, using individual-level data and a longitudinal study design. Older people - including those aged over 80 years - admitted to psychiatric hospital were found to have a markedly higher suicide risk than those who had no record of admission to a psychiatric hospital since 1969. The time immediately after admission was associated with the highest increase in risk. However, only a small proportion of the very old people who took their own lives had previously been hospitalised with psychiatric disorders. In addition, we found an inverse interaction between age and psychiatric hospitalisation: people over the age of 80 years who were hospitalised experienced a lower increase in their risk of completing suicide than middle-aged and old people.
The elevated suicide risk after psychiatric hospitalisation among older people is in accordance with previous studies based on psychological autopsy studies (Reference Henriksson, Marttunen, Isometsä, Pearson and ConwellHenriksson et al, 1996; Reference Conwell, Lyness and DubersteinConwell et al, 2000; Reference Waern, Runeson and AllebeckWaern et al, 2002). Whereas those studies mainly employed cross-sectional data, our study adds further substance to the interpretation by using longitudinal data. Furthermore, our study is the first to distinguish between previously and currently hospitalised patients among the examined age groups. Although people currently hospitalised had significantly higher suicide risks than those previously hospitalised, the difference diminished with increasing age. A marked increase in suicide risk was found for the time shortly after discharge compared with the following weeks. Our findings confirm that this period is associated with elevated risks in late life, as has been found in studies on all age groups (Reference Qin, Agerbo and MortensenQin, 2003; Reference Hoyer, Olesen and MortensenHoyer et al, 2004). Clearly, this finding is very important in terms of preventive work.
The prevalence of depression is reported to increase with age among the elderly (Reference BlazerBlazer, 2000). It therefore seems surprising that only a small proportion of very old people who completed suicide had at some point been admitted to a psychiatric hospital. Also, the inverse interaction between psychiatric hospitalisation and age is unexpected. There may be several explanations for these findings. First, it might be that very old people in general are less affected by psychiatric disorders or that they may to a larger extent suffer from psychiatric disorders that are associated with lower suicide risk. An example of this is dementia. When assessing all patients aged over 50 years with dementia in psychiatric hospitals, we found that this group actually had a lower suicide risk than the general hospitalised population (a future research project aims to address this). Additional support for this finding is mentioned by Harris & Barraclough (Reference Harris and Barraclough1997) as well by Schneider et al (Reference Schneider, Maurer and Frolich2001). As dementia is expected to be more prevalent among very old people, this could explain the lower suicide risks among those hospitalised. Furthermore, it is likely that more cases of mood disorders are related to dementia among the very old, leading to a lower suicide risk. Second, it might be that affective disorders (including those leading to suicide) are more complicated to diagnose in very old people. Studies show that psychiatric disorders in elderly people are to some extent not identified or treated (Reference Purcell, Thrush and BlanchettePurcell et al, 1999; Reference S⊘rensenSørensen, 2001). In these age groups a depressed mood may be viewed as a part of the ageing process. Additionally, mood disorders at older ages may interact with organic disorders and thus complicate diagnostic interpretation (Reference BlazerBlazer, 2000). If depression among the very old is not identified and treated to the same extent as in younger age groups, this could lead to a higher suicidality among very old people who are not hospitalised. Third, the majority of very old people in Denmark are already living with some kind of healthcare assistance or in nursing homes (Reference Andersen-Ranberg, Schroll and JeuneAndersen-Ranberg et al, 2001). The very old population may thus to a larger extent be treated in other healthcare settings and not admitted to psychiatric hospitals. The increased frailty and proportion of severe somatic disorders among the very old (Reference Manton and GuManton & Gu, 2001; Reference Nybo, Gaist and JeuneNybo et al, 2001) may also prevent a psychiatric admission. Very old people with both somatic and psychiatric disorders are probably more likely to be admitted to general hospitals for treatment.
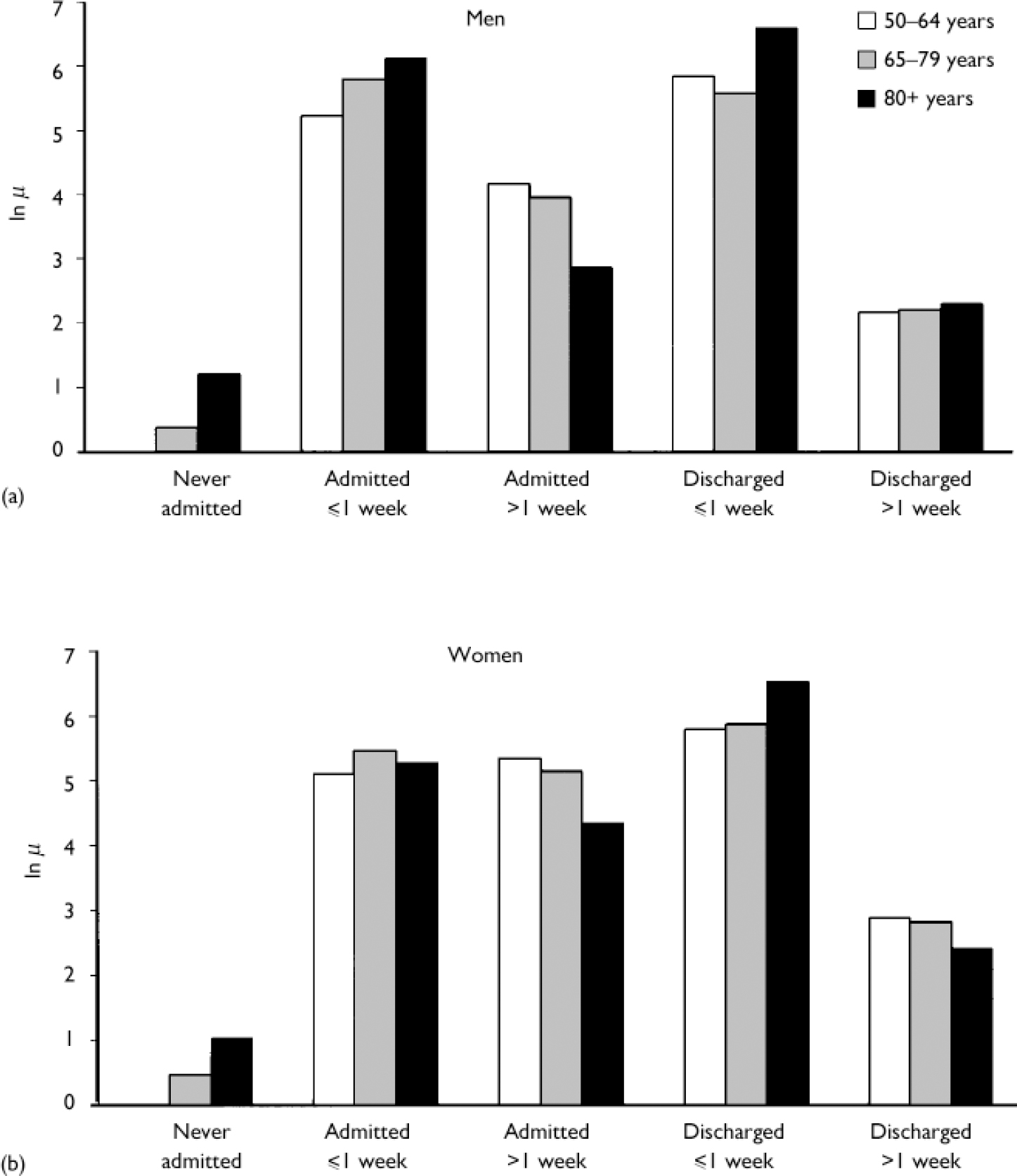
Fig. 1 Relative suicide risk by age and time since admission or discharge for (a) men and (b) women aged 50+ years in Denmark, 1994-1998; the reference group is never-admitted men and women aged 50-64 years.
Limitations
A limitation of our study is that the analyses were based on admissions to psychiatric hospitals, which serve as a proxy for severe psychiatric disorder. Our analyses do not include data on elderly people who might be treated by general practitioners at home or in nursing homes, nor data on people with unidentified or untreated psychiatric disorders. The proportion of psychiatric disorders in those who die by suicide may thus be even larger. However, it seems probable that elderly people with severe psychiatric disorders would be admitted to a psychiatric hospital.
Additionally, the data only cover psychiatric hospitalisation since 1969, not the entire life span of the study population. For immigrants to Denmark, no history of psychiatric hospitalisation was available for the time prior to immigration. Nevertheless, the number of immigrants among the elderly was small, so we do not expect this misclassification to influence the results substantially (less than 1% of the study population migrated to Denmark during the observation period).
Validity of suicide registration
In this study we solely include deaths registered as suicides. It is therefore imperative to consider the validity of the suicide registration. Schmidtke & Weinacker (Reference Schmidtke and Weinacker1991) have proposed that the 'dark number' of suicides, i.e. suicides that are not registered as such, is likely to be higher among elderly people than it is in younger age groups. It might be that other causes of death, such as those classified as 'undetermined', conceal actual suicides of older adults. If there is a misclassification problem we would expect suicides occurring during psychiatric hospitalisation and also among people previously hospitalised to be less frequently misclassified than suicides among people who had never been hospitalised. This would mean that the suicides among never-hospitalised persons might be slightly underrepresented. However, we assume that the effects are similar among all age groups and therefore this would not have any influence on the documented interaction. The risk patterns we observed seem realistic.
Strengths of the study
One strength of our study is that we investigated risks of suicide using very complete and detailed individual-level data covering an entire nation. This allowed us to calculate estimates of suicide risks for smaller population groups such as the very old. Furthermore, the prospective data collection implies that the data are gathered on an identical basis for people who die by suicide and those who do not. The availability of longitudinal data allowed us to model the event history of each individual by taking into account changes within the individual with respect to risk status, as well as changes in the composition of the population. The applied method is hence a step further towards an optimal approach for analysing the association between hospitalisation and subsequent suicide.
As data for the entire Danish population aged 50 years and over were analysed, the findings are 100% representative for all older adults in Denmark during 1994-1998. The results are to some extent limited to the context of Danish society or a society with similar healthcare facilities.
Implications
We found a clear increase in the suicide risks of very old people hospitalised with psychiatric diagnoses. However, only a small proportion of very old people who complete suicide have at some point been hospitalised. Also, the increase in risk experienced by this age group in association with psychiatric hospitalisation is lower than for younger age groups. An inverse interaction effect between age and admission to psychiatric hospital is noted. Further research is needed to determine if this is because the disorders in the very old population are of another type, not identified or treated in other healthcare settings (e.g. interacting with somatic disorders).
An important implication of our study, which should be taken into account when identifying target populations for new preventive measures, is that psychiatric hospitals are in contact with a relatively small proportion of very old people who die by suicide. However, for those who are admitted to a psychiatric hospital, a vital time for potential interventions is the weeks shortly after an admission or a discharge.
Clinical Implications and Limitations
CLINICAL IMPLICATIONS
-
▪ Only a small proportion of very old people who die by suicide have been hospitalised for psychiatric disorders.
-
▪ The weeks just after admission are associated with an elevated suicide risk in elderly people.
LIMITATIONS
-
▪ The data used for analyses included only psychiatric disorders that required hospitalisation.
-
▪ Since suicide is a relatively rare event, some of the estimates in our hazard models are based on only a few cases.
-
▪ If there were suicides not registered as such (i.e. misclassified), they are not included in the analyses.
Acknowledgements
We thank Dr Gunnar Andersson and Dr Vladimir Canudas Romo for their helpful comments. The project has received funding from the Danish Health Insurance Foundation and the Reference Group for Prevention of Suicide Attempts and Suicide. P.B.M. was supported by the Stanley Medical Research Institute, and the National Centre for Register-based Research is funded by the Danish National Research Foundation. The research project was approved by the Danish Data Protection Agency. The analysis was carried out with the kind cooperation of the National Centre for Register-based Research in Denmark.








eLetters
No eLetters have been published for this article.