Introduction
A lot of recent research efforts have been devoted to prodromal and first-episode symptoms of schizophrenia spectrum disorders; however, the long-term outcome and handling of these complex disorders also deserve attention. Recovery from schizophrenia is possible and approximately 40% of individuals affected have positive outcomes in occupational and social domains (Jääskeläinen et al., Reference Jääskeläinen, Juola, Hirvonen, McGrath, Saha, Isohanni, Veijola and Miettunen2013). Although the associated stigma has not subsided sufficiently from society or the health care system, the concept of recovery from schizophrenia has evolved and is finding growing acceptance (Slade et al., Reference Slade, Leamy, Bacon, Janosik, Le Boutillier, Williams and Bird2012; Norman et al., Reference Norman, Li, Sorrentino, Hampson and Ye2017). Recovery-oriented approaches have been recognised as best suited for psychiatric rehabilitation in severe mental disorders (Xu et al., Reference Xu, Lay, Oexle, Drack, Bleiker, Lengler, Blank, Müller, Mayer, Rössler and Rüsch2018).
The concept of recovery style provides an important approach to understand how individuals handle psychosis (Espinosa et al., Reference Espinosa, Valiente, Rigabert and Song2016). It has been proposed that people recovering from psychosis adopt one of two distinct recovery styles: either they ‘seal-over’ by avoiding the psychotic experience, not seeing it as a part of themselves or they ‘integrate’ by incorporating the psychotic episode into their identity (McGlashan et al., Reference McGlashan, Docherty and Siris1976; Reference McGlashan, Wadeson, Carpenter and Levy1977). Recovery style has been demonstrated to influence treatment engagement and illness status (Tait et al., Reference Tait, Birchwood and Trower2003).
‘Sealing-over’ recovery style is associated with insecure identity and little resilience (Drayton et al., Reference Drayton, Birchwood and Trower1998; Tait et al., Reference Tait, Birchwood and Trower2004). These individuals more often have negative experiences in early attachment as well as current social difficulties. This might explain why these patients seek less contact with services and have a higher rate of involuntary measures (Tait et al., Reference Tait, Birchwood and Trower2004; O'Donoghue et al., Reference O'Donoghue, Lyne, Hill, O'Rourke, Daly, Larkin and O'Callaghan2011). A weaker therapeutic alliance was observed to be more frequent in patients with a sealing-over recovery style (Cavelti et al., Reference Cavelti, Homan and Vauth2016). ‘Sealing-over’ recovery style was also associated with more predominant negative symptoms and more overall illness severity. Higher levels of thought disorders may interfere with the patient's capability to understand experiences and predicted rather avoidant coping strategies (Cavelti et al., Reference Cavelti, Homan and Vauth2016).
‘Integration’ is the more favourable recovery style. In presence of the same severity of illness, an integrative recovery style may indicate higher service engagement (Tait et al., Reference Tait, Birchwood and Trower2003; Vender et al., Reference Vender, Poloni, Aletti, Bonalumi and Callegari2014). In patients with severe mental illness in community services and long-term secure services, not recovery style but insight directly influenced the type of treatment service. However, insight was closely related to recovery style (Fitzgerald, Reference Fitzgerald2010). A moderator role of recovery style between internalised stigma and emotional distress was found in people with persecutory delusions. People with ‘integration’ recovery styles, even if feeling stigmatised, tend to be more resilient to depression (Espinosa et al., Reference Espinosa, Valiente, Rigabert and Song2016). Nevertheless, in individuals with recent onset of psychosis and post-traumatic stress disorder syndrome, a trend towards an integrative coping style was found (Mueser et al., Reference Mueser, Lu, Rosenberg and Wolfe2010).
To identify these distinct recovery styles, two instruments have been developed for research purposes and clinical use. The ‘Integration Sealing over Scale’ (ISOS, McGlashan, Reference McGlashan1987) is an extensive semi-structured clinical interview requiring rating by a clinician. The ‘Recovery Style Questionnaire’ (RSQ; Drayton et al., Reference Drayton, Birchwood and Trower1998) has been developed as a short self-report version of the ISOS. Initial psychometric evaluation of the RSQ by the developers showed good internal consistency, test–retest reliability, face- and criterion-related validity with the ISOS (Drayton et al., Reference Drayton, Birchwood and Trower1998). Sound psychometric parameters were also reported by others (Modestin et al., Reference Modestin, Caveng, Wehrli and Malti2009; Poloni et al., Reference Poloni, Callegari, Buzzi, Aletti, Beranzini, Vecchi and Vender2010; Nasillo et al., Reference Nasillo, Santos, Arrufat and Obiol2013).
However, efforts of further scale validation have been scarce (Cavelti et al., Reference Cavelti, Kvrgic, Beck, Kossowsky and Vauth2012) and a factorial validity assessment of the RSQ has so far never been conducted to the best of our knowledge (Grinter, Reference Grinter2012). Furthermore, a German instrument to measure recovery style in psychosis is needed. Therefore, the aim of this study was to psychometrically re-evaluate the RSQ during the process of developing a German version of the questionnaire.
Methods
Participants
The participants were recruited from psychiatric inpatient and outpatient treatment units. Patients included were (a) aged between 18 and 65, (b) had a diagnosis of a schizophrenia spectrum disorder according to ICD-10, (c) gave written informed consent and (d) able to understand the German language sufficiently. Exclusion criteria were (a) severe cognitive impairment with serious impairment or inability to communicate, (b) seriously impaired judgement and reality testing as in the case of an acute psychotic episode.
Procedures
Data were collected at the Department of Psychiatry and Psychotherapy at the Medical University of Vienna and a collaborating public mental health centre in Vienna. Recruitment was done by psychiatric residents or psychiatric consultants. Patients received detailed information about the study and were able to ask questions concerning the project. Those willing to participate signed informed consent. The presence of psychotic symptoms and medical data were asked for, and the questionnaires mentioned below were administered.
Instrument
The RSQ (Drayton et al., Reference Drayton, Birchwood and Trower1998, see Table 1) consists of 39 items divided into 13 subscales each comprising three separate questions (see Table 2). The patient rates each item with either ‘agree’ or ‘disagree’. Using a coding frame, each answer is identified as either ‘sealing-over’ (1 point) or ‘integration’ (2 points). Each of the 13 subscales is rated separately (3–4 points ‘sealing-over’ and 5–6 points ‘integration’) and finally a formula is used to calculate the overall percentage of integration: (RSQ overall percentage = number of scales with overall rating of integration/13 × 100%). From the RSQ overall percentage, the following categories are built: 0–17% = 6 sealing-over, 18–33% = 5 tends towards sealing-over, 34–49% = 4 mixed picture, sealing-over predominates, 50–67% = 3 mixed picture, integration predominates, 68–82% = 2 tends towards integration, 84–100% = 1 integration. The initial scale development paper (Drayton et al., Reference Drayton, Birchwood and Trower1998) reported good psychometric properties with Cronbach's α of 0.73, test–retest reliability of 0.81 and suggested two recovery styles (i.e. sealing-over and integration) composed of 13 factors, without reporting a factor analysis.
Table 1. Items of the Recovery Style Questionnaire with valid answers (n) and item-total correlation r it
a Inverted items, bold: item-total correlation ⩾0.20, items selected via model modification after confirmatory factor analysis.
Table 2. Definitions of domains of the Recovery Style Questionnaire and Cronbach's α values
a Poor but acceptable Cronbach's α ⩾ 0.5.
b Good Cronbach's α ⩾ 0.7.
Translation and back translation
The RSQ was translated into German according to the guidelines of the WHO (Sartorius and Janca, Reference Sartorius and Janca1996). One of the authors (A.U.) is a German and English native speaker and works as a psychiatrist. She translated the English original version into German and then an English back-translation was done by a German–English professional translator. The English back-translation was reviewed and checked for consistency by one of the authors of the original English version (M.B.; Drayton et al., Reference Drayton, Birchwood and Trower1998).
Validation
As recommended by Guadonoli and Velicer (Reference Guadagnoli and Velicer1988) and Costello and Osborne (Reference Costello and Osborne2005), about 150 cases were planned to be appropriate when performing a factor analysis on the 39-item RSQ. The correlation coefficient should become an adequate estimator of the population correlation coefficient when sample sizes reach this level. To establish test–retest reliability with a power of 0.80 and an α of 0.05, assuming that at least 10% of the sample agrees with the item and considering the possibility that occasionally items might be missing, we found a sample of 30 patients to be suitable to fill out the questionnaire again after a couple of weeks. For the assessment of convergent and discriminant validity, other instruments with related or distinguishing constructs were administered. The Internalised Stigma of Mental Illness inventory (ISMI) (Ritsher et al., Reference Ritsher, Otilingam and Grajales2003; German Version: Sibitz et al., Reference Sibitz, Friedrich, Unger, Bachmann, Benesch and Amering2013) was developed to measure internalised stigma. The 27-item scale consists of the subscales alienation, discrimination experience, social withdrawal, stereotype endorsement and resistance. The German version of the ISMI showed good psychometric properties (Sibitz et al., Reference Sibitz, Friedrich, Unger, Bachmann, Benesch and Amering2013). The well-established Positive and Negative Syndrome Scale (PANSS) (Kay et al., Reference Kay, Fiszbein and Opler1987) was used. The Illness Concept Scale (KK-Scale) (Linden et al., Reference Linden, Nather and Wilms1988) is a German questionnaire, also named ‘Krankheitskonzept Skala’ (KK-Scale). It consists of 29 items and was designed for schizophrenic patients. The scale assesses patients’ illness-related attitudes. Chronbach's α and retest–test reliability were moderate (Linden et al., Reference Linden, Nather and Wilms1988). The 28-item Rogers Empowerment Scale (Rogers et al., Reference Rogers, Chamberlin, Ellison and Crean1997) measures empowerment in five different dimensions: self-esteem and self-determination, power v. feeling powerless, autonomy, optimism and control over the future, justified anger. The scale demonstrated excellent reliability and validity in large samples (Rogers et al., Reference Rogers, Ralph and Salzer2010). The revised version of the self-esteem scale by Rosenberg (Reference Rosenberg1965) is a ten-item self-rating instrument measuring positive and negative feelings about the self. It has been validated in German language and showed good psychometric properties (Von-Collani and Herzberg, Reference Von-Collani and Herzberg2003). The well-established WHOQOL-BREF is a 26-item short version of the WHOQOL-100 instrument with satisfactory internal consistency (WHO, 1996). It entails the dimensions physical well-being, psychological well-being, social relations and the environment.
Statistical analysis
The statistical analysis was calculated using the software packages SPSS® 24 and AMOS® 24. Descriptive statistics are presented in absolute numbers and percentages. Internal consistency of the RSQ was calculated and corrected for dichotomous variables by the Kuder–Richardson Formula 20 (Kuder and Richardson, Reference Kuder and Richardson1937). A Cronbach's α coefficient >0.70 was considered acceptable. Pearson correlation coefficient was used to evaluate test–retest reliability. Additionally, split-half reliability was calculated with the Spearman–Brown coefficient. The convergent and discriminant validity were examined with correlational analyses of the RSQ overall percentage score with other constructs.
A confirmatory factor analysis was performed to test the fit of our data to a 13-factor model deriving from the original 13-subscale structure of the English RSQ with 39 dichotomous items (Drayton et al., Reference Drayton, Birchwood and Trower1998). The acceptability of the model was judged by following recommended standards: χ 2 ratio to degrees of freedom (χ 2/df) < 2.00, Comparative Fit Index (CFI), Normed Fit Index (NFI) and Tucker–Lewis Index (TLI) > 0.90 and the root mean square error of approximation (RMSEA) values of 0.06 or less for a good fit and 0.08 or less for a reasonable fit (Bentler, Reference Bentler1990; Backhaus et al., Reference Backhaus, Erichson, Plinke and Weiber2006; Schreiber, Reference Schreiber2008; Moosbrugger and Kelava, Reference Moosbrugger and Kelava2012). To compute fit indices in the CFA, estimates of standardised regression weights were used because the weight gives information about the implication that each item should preferably have. They can be interpreted like effect sizes following the effect size classification by Cohen (Reference Cohen1988).
Results
Sample characteristics
Of 251 persons approached, 94 declined to participate, 16 dropped out because they did not meet the inclusion criteria and three patients did not complete the RSQ. The study sample comprised 138 participants, 56 of them missed at least one RSQ item. Therefore, only 82 cases could be included into some of the calculations (e.g. internal consistency). In Table 3, socio-demographic and illness-related data of the sample are shown. Overall, 74 men (53.6%) and 64 women (46.4%) aged between 19 and 69 years (M 36.4, s.d. ± 11.3) were included. Ninety-one persons (65.9%) were diagnosed with paranoid schizophrenia (WHO, 1993) (ICD-10: F20.0), three (2.2%) with hebephrenic schizophrenia (ICD-10: F20.1), one (0.7%) with undifferentiated schizophrenia (ICD-10: F20.3), three (2.2%) with residual schizophrenia (ICD-10: F20.5), four (2.9%) with schizotypal disorder (ICD-10: F21), three (2.2%) with persistent delusional disorder (ICD-10: F22), two (1.5%) with acute polymorphic psychotic disorders (ICD-10: F23.1) and 31 (22.5%) with schizoaffective disorder (ICD-10: F25). Most participants had been suffering from a psychosis of the schizophrenic spectrum for several years (M 15.1, s.d. ± 15). The patients were moderately to severely ill (PANSS M 72.9, s.d. ± 12.6) and demographic characteristics reflected the typical adverse effects of this illness: 110 participants were unmarried (79.7%) and more than half (n = 52, 52.9%) lived alone. Nearly half of all participants (n = 65, 47.1%) received invalidity pension and only three people had a paid work.
Table 3. Socio-demographic and illness-related data
Standard deviation s.d.
Out of 138 participants, the mean RSQ overall percentage of integration in our sample was 66.12% (s.d. ± 17.43), representing the category ‘mixed picture, integration predominates’. The majority of participants showed either a ‘mixed picture where integration predominates’ (n = 38, 27.0%), ‘tends towards integration’ (n = 46, 32.6%) or ‘integration’ (n = 28, 19.9%). Few participants showed either ‘mixed picture where sealing-over predominates’ (n = 21, 14.9%), ‘tend towards seal-over’ (n = 4, 2.8%) or ‘sealing-over’ (n = 1, 0.7%) (see Fig. 1).
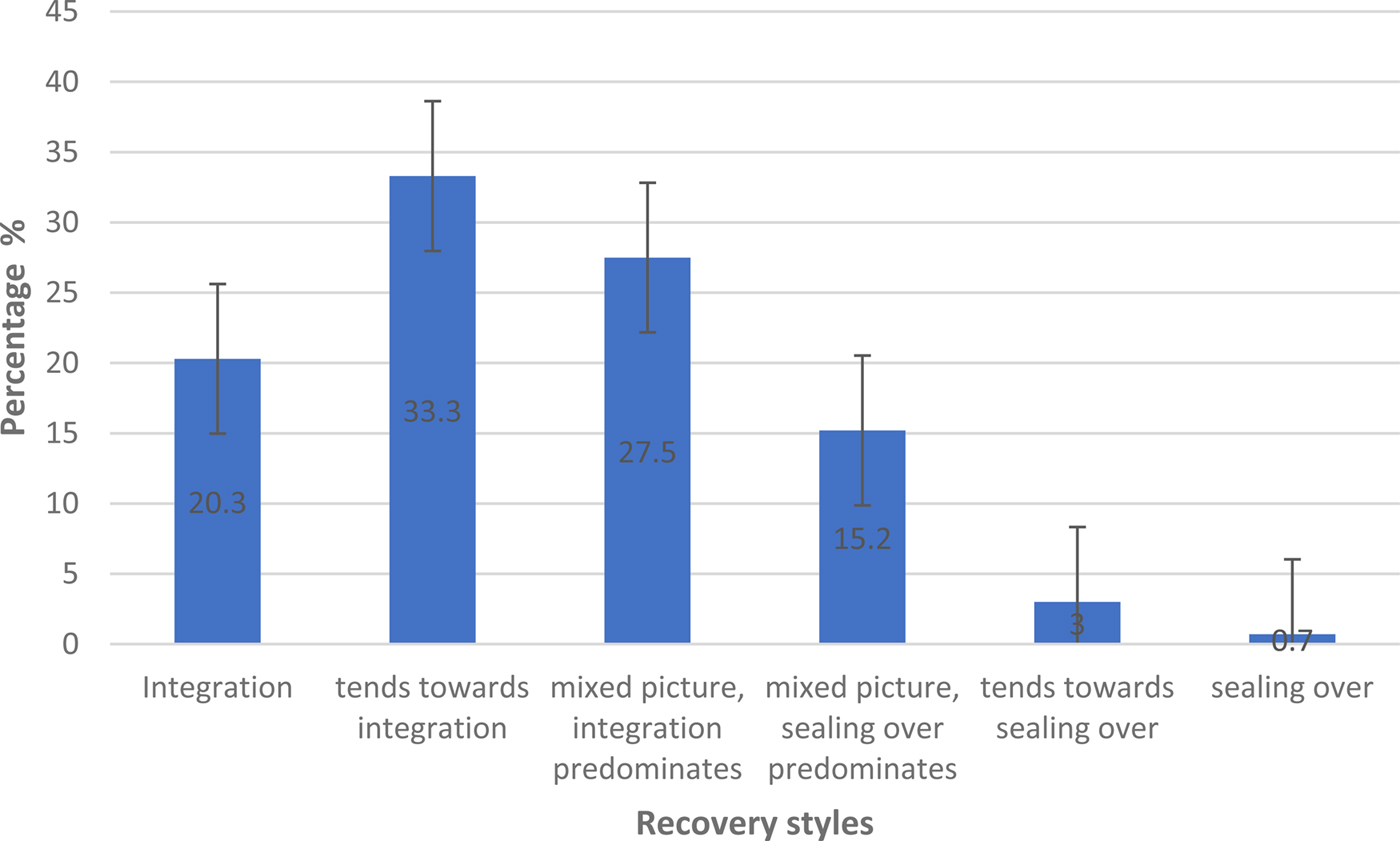
Fig. 1. Distribution of recovery styles, percentages with standard errors, N = 138.
Reliability
Eighty-two questionnaires with no missing items were included for internal consistency. An acceptable Cronbach's α of 0.741 was achieved. Most of the subscales performed below an acceptable range (see Table 1). The test–retest coefficient for the RSQ overall per cent scores (n = 24) was r = 0.502 for 52.17 days with a significance of p = 0.01 (two-tailed). The split-half reliability for the 39 RSQ items yielded a Spearman–Brown coefficient of 0.686 with n = 82.
Descriptive statistical evaluation of items
The RSQ consists of 39 items, 17 items were inverted during questionnaire development (Drayton et al., Reference Drayton, Birchwood and Trower1998). Table 1 shows the formulation of each individual item. It was found that the proportion of integrative answers is lower for items with negative formulations. The 17 negatively poled items were answered by 38.0% of the participants with integrative patterns, while the 22 positively poled items of 65.8% were given an integrative answer. Respondents rejected items like item 23, ‘My illness has had little effect on my life’ or item 4 ‘I am not interested in my illness’. In addition, separation powers were calculated for the individual items (see Table 1). The power of separation indicates how well a single item distinguishes persons with a ‘sealing-over’ and an ‘integrative recovery style’. Corrected separations r it of ⩽0.20 were considered too low. Only 22 items showed satisfactory values. For example, item 19, ‘I can manage the problems caused by my illness, alone’ was not clearly distinguishable between the two types of recovery styles.
Convergent and discriminant validity
The convergent and discriminant validity were examined with correlations of the RSQ overall percentage score with other constructs. The RSQ was positively correlated with psychological quality of life (r = 0.323; p < 0.01) and showed an overlap with following concepts: resistance on the internalised stigma scale (r = 0.389; p < 0.01), empowerment (r = 0.422; p < 0.01) and specifically optimism on the empowerment scale (r = 0.428; p < 0.01). There was a positive relationship between the recovery style and the construct of self-esteem, on the self-esteem scale (r = 0.324; p < 0.01) and self-esteem on the empowerment scale (0.381; p < 0.01). A negative association of the RSQ with alienation on the internalised stigma scale was found (−0.309; p < 0.01) (see Table 4).
Table 4. Correlation of the RSQ overall percentage with different scales, (n = 92, listwise)
a Values under 0.01 were considered highly significant.
b Values under 0.05 were considered significant.
Confirmatory factor analysis
The results of the confirmatory factor analysis are displayed in Supplementary Table 1. The χ 2 test was significant (p < 0.001, χ 2 = 1080.604, 624 df) and the χ 2/df of 1.732 demonstrated good model fit, but other indices showed poor model fit with CFI of 0.586, NFI of 0.414 and a TLI of 0.508. The RMSEA of 0.095 indicated reasonable model fit.
Model modification
The fit to the proposed model was partially poor. In order to ameliorate the model, a post hoc model modification was done. It is good practice to assess the fit of each construct and its items individually to determine particularly weak items. Items with low corrected item total correlations (r it ⩽ 0.20, see Table 1 and Supplementary Table 2) indicate very high levels of error. These items were removed from the model step by step (Hooper et al., Reference Hooper, Coughlan and Mullen2008). Path coefficients for each item derived from the CFA were also comparable with the results of the item-total correlations (see Supplementary Table S1 and Supplementary Fig. S1). Model modification revealed a one-factor model consisting of 11 items with acceptable fit to the data (see Fig. 2; Supplementary Table S2). χ 2/df of 1.562 and CFI of 0.936, NFI of 0.847 and a TLI of 0.910 demonstrated good model fit. The RMSEA of 0.083 indicated reasonable but better model fit. The remaining items with the best parameters were marked in bold in Table 1.
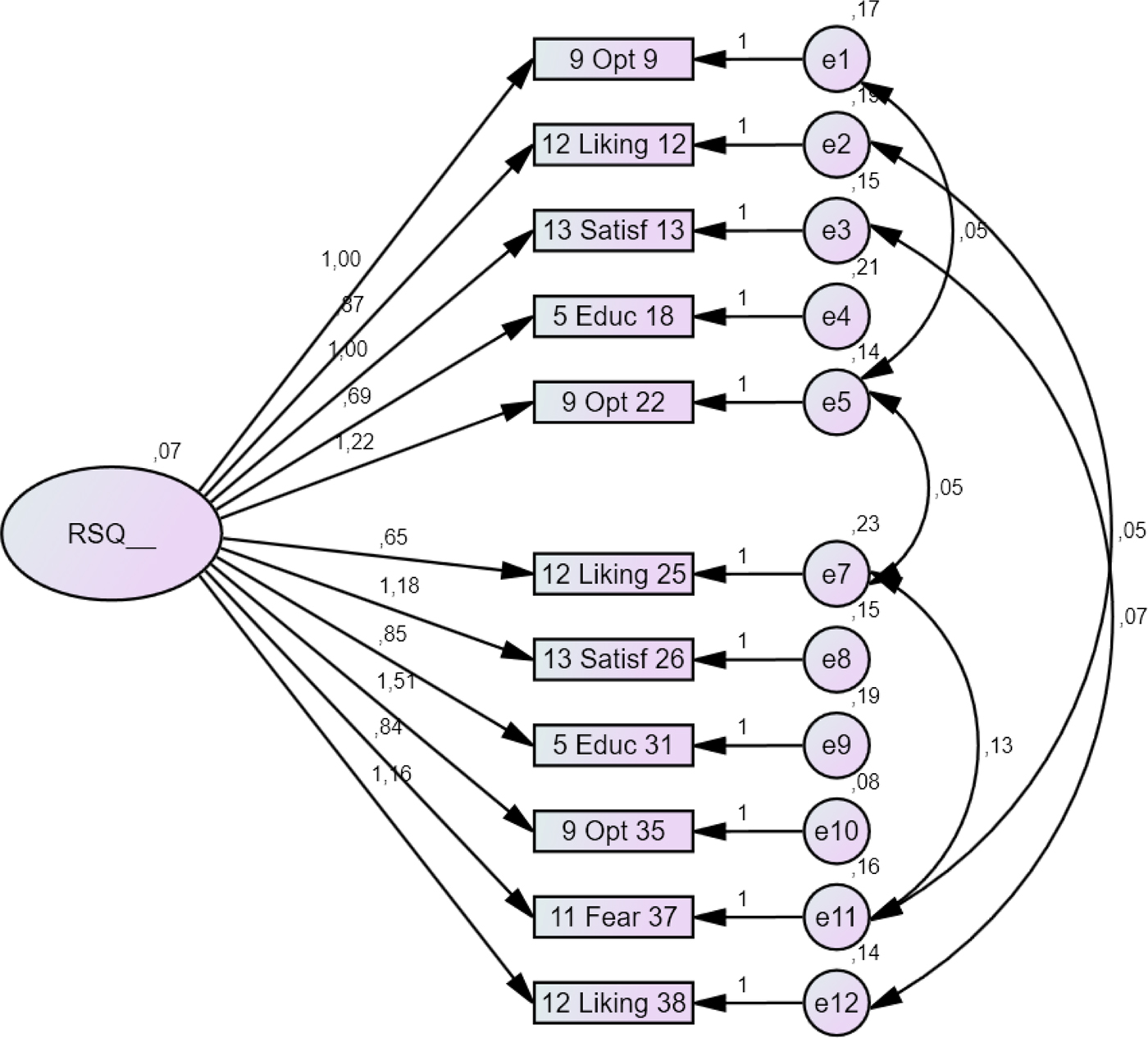
Fig. 2. Path diagram of the confirmatory factor analysis of an alternative one-factor model (11 items) with observed and latent variables, left number of rectangle refers to the number of subscale and right number indicates item number; n = 82.
Discussion
The aim of the present study was the validation of the RSQ. Overall, the reliability of the RSQ scale was acceptable. Confirmatory factor analysis revealed that the 13-factor model originally proposed was not replicated in the present sample. The RSQ was modified based on item-total correlations and path coefficients, the confirmatory factor analysis of the resulting model showed adequate fit to the data.
Internal consistency of the RSQ showed an acceptable value at Cronbach's α = 0.741, similar to the original paper where internal consistency was α = 0.73 and other validation papers reporting values from α = 0.73 (Poloni et al., Reference Poloni, Callegari, Buzzi, Aletti, Beranzini, Vecchi and Vender2010) to α = 0.78 (Modestin et al., Reference Modestin, Caveng, Wehrli and Malti2009; Grinter, Reference Grinter2012). However, the internal consistency of most of the subscales was below an acceptable value, which could be expected because each subscale consists only of three items. The test–retest reliability was moderate with a correlation of r = 0.502 which translates to only about half of all responses being identical when asked again a second time after a couple of weeks. A previous study has also reported a test–retest reliability correlation coefficient of r = 0.50 for the RSQ (Poloni et al., Reference Poloni, Callegari, Buzzi, Aletti, Beranzini, Vecchi and Vender2010), whereas the test–retest reliability for 1 month of the original validation was r = 0.81 (Drayton et al., Reference Drayton, Birchwood and Trower1998).
The sample size of 56 participants in the original study was small with a low proportion of female participants (26.8%) (Drayton et al., Reference Drayton, Birchwood and Trower1998). In comparison, our study included 138 participants with a balanced gender distribution. In the original paper, only people diagnosed with schizophrenia according to ICD-10 criteria were included. The present sample consisted of a broader diagnostic spectrum with 65.9% diagnosed with paranoid schizophrenia, 2.2% with hebephrenic schizophrenia, 0.7% with undifferentiated schizophrenia, 2.2% with residual schizophrenia, 2.9% with schizotypal disorder, 2.2% with persistent delusional disorder, 1.5% with acute polymorphic psychotic disorders and 22.5% with schizoaffective disorder. The age at onset of illness and the duration of illness were quite similar in both studies but the number of admissions was higher in our investigation with 5.9 hospital stays on average compared with three admissions in the original paper. The present sample was moderately to markedly ill with a mean PANSS score of 72.9 (s.d. 12.6) (Leucht et al., Reference Leucht2014). Therefore, the larger sample with a broader range but more severe disorders could have influenced the results.
In summary, the confirmatory factor analysis performed on our data yielded a poor-to-moderate model fit to the original 13-subscale structure with 39 items of the RSQ (Drayton et al., Reference Drayton, Birchwood and Trower1998). To our knowledge, this is the first study to examine the factor structure of the RSQ by means of factor analysis. In the original paper by Drayton (Reference Drayton, Birchwood and Trower1998), no factor analysis was conducted. The basis for the formation of 13 subscales was the ISOS (McGlashan et al., Reference McGlashan, Docherty and Siris1976), an observer report measure requiring the interviewer to assess the patient over 13 concepts pertaining to illness-related attitudes. The RSQ was designed as a short self-report assessment with three questions assigned to each concept presented in the ISOS and therefore a face validity with the ISOS was stated. The criterion-related validity with the ISOS was good achieving similar results for the RSQ (r = 0.92; Drayton et al., Reference Drayton, Birchwood and Trower1998). However, most subscales did perform below an acceptable reliability. The evaluation of the questionnaire is not based on a sum score of the 39 items. Each subscale consisting of three items is rated separately and an overall percentage is calculated which refers to an either integrative or sealing-over recovery style. The 13-scubscale structure did disappoint and this might distort the results. Furthermore, 17 out of 39 items showed disappointing separation power. It seemed that more than a third of negatively worded questions (17 items) were more likely to be answered in a non-integrative pattern. Reversing a proportion of items is often used to reduce the effects of response styles by changing the direction of the item. Although this is an established practice, there is no consensus about its effectiveness (van Sonderen et al., Reference Van Sonderen, Sanderman and Coyne2013). Ebesutani et al. (Reference Ebesutani, Drescher, Reise, Heiden, Hight, Damon and Young2012) found that non-reverse-worded items were associated with superior psychometric properties relative to the reverse-worded items. Often it makes questions more complex and more difficult to understand. Questions like RSQ item 2 ‘My illness is not a part of my personality’ or item 4 ‘I am not interested in my illness’ may not be well read and understood by respondents. Especially patients suffering from schizophrenia for years often have impaired cognitive functioning with thought disorders. They may lack sufficient attention to carefully read and understand the questions, this might influence the truth of the given answers. In contrast, the dichotomous answer format of the RSQ may be beneficial for this patient group due to a dichotomous thinking style often found in patients with psychotic disorders (Peters et al., Reference Peters, Moritz, Schwannauer, Wiseman, Greenwood, Scott, Beck, Donaldson, Hagen, Ross, Veckenstedt, Ison, Williams, Kuipers and Garety2014).
The concept of recovery style was related to the construct of resistance to internalised stigma measured with the ISMI (Ritsher et al., Reference Ritsher, Otilingam and Grajales2003). This is consistent with recent findings where recovery style was shown to have a moderator role between internalised stigma and depression in people with persecutory delusions (Espinosa et al., Reference Espinosa, Valiente, Rigabert and Song2016). Recovery style was also found to overlap with the concept of empowerment and optimism. Recovery style provides an important approach to understand how individuals handle psychosis in a psychological dimension. The RSQ is continued to be used in recovery-oriented research (Modestin et al., Reference Modestin, Caveng, Wehrli and Malti2009; O'Donoghue et al., Reference O'Donoghue, Lyne, Hill, O'Rourke, Daly, Larkin and O'Callaghan2011; Vender et al., Reference Vender, Poloni, Aletti, Bonalumi and Callegari2014; Espinosa et al., Reference Espinosa, Valiente, Rigabert and Song2016) and clinical practice. The ISOS, which is essentially the same construct, is still applied, too (Modestin et al., Reference Modestin, Caveng, Wehrli and Malti2009; Cavelti et al., Reference Cavelti, Homan and Vauth2016). Recovery style has been shown to affect symptoms, treatment and outcome in schizophrenia (McGlashan et al., Reference McGlashan1987; Modestin et al., Reference Modestin, Soult and Malti2004; Reference Modestin, Caveng, Wehrli and Malti2009; Cavelti et al., Reference Cavelti, Homan and Vauth2016).
Strengths and limitations
The study provides a comprehensive and independent psychometric evaluation of the RSQ. To the authors’ knowledge, it is the first study to investigate the factor structure of the RSQ and to compare the underlying construct with an independent concept of stigma internalisation (ISMI). Although the sample size of the present study is relatively small, it is acceptable for factor analytical procedures and it is so far the largest sample to investigate psychometric properties of the RSQ. The composition of the present sample could be a limitation. Patients were in part recruited at an outpatient clinic where mainly patients with a chronic progression of schizophrenia are often repeatedly treated on a rather long-term basis over years. These patients are usually very advanced in their expertise about psychotic experiences and are, in the majority of cases, stabilised due to the extensive treatment and support. This limits the examined population to those who were in treatment at the time of assessment, and it is not known how results might have differed in a ‘real-world’ population of those who are partly out of treatment or completely on their own without support. The influence of duration of illness on recovery style is unclear and further studies are warranted to determine how transition from sealing-over to integration can best be promoted.
Conclusions
The use of the RSQ in clinical practice might be inspiring and helpful, especially for treatment planning. The RSQ does cover several topics that are clinically relevant, with items such as ‘I have a medical illness’ and ‘My illness had a strong impact on my life’ insight and the impact the illness has on patients’ lives is reflected. Yet, addressing and discussing topics such as showing interest in one's illness, believing in one's influence on the course of the illness and accepting help and support within the therapeutic relationship might facilitate the acceptance of the illness and further the recovery process. The use of the RSQ in mental health practice might provide the therapist and the patient with an indication of areas in need of enhanced therapeutic discussion and support. First, the RSQ can be a helpful tool for measuring the integration of the recovery concept on the consumer side. Second, identifying patients with sealing-over recovery styles might enable professionals to provide more intensive support to those at risk for poorer service engagement. Anyway, considering the results of the present study pointing to statistical and conceptual shortcomings, the RSQ cannot be recommended for use in recovery-oriented research in its original version (Drayton e t al., Reference Drayton, Birchwood and Trower1998). Therefore, a short version with better psychometric properties is proposed for research use but further scale validation is needed.
Supplementary material
The supplementary material for this article can be found at https://doi.org/10.1017/S2045796018000471
Acknowledgements
The authors acknowledge the assistance and help of all people who contributed to the study.
Financial support
This research received a grant from Jubiläumsfonds of the Austrian National Bank (ÖNB – Österreichische Nationalbank) project number 12034.
Conflict of interest
None.
Ethical standards
The study was approved by the ethics committee of the Medical University of Vienna (Nr. 455/2005). The authors assert that all procedures contributing to this work comply with the ethical standards of the committee of the Medical University of Vienna in accordance with the Helsinki Declaration of 1975, as revised in 2008.
Availability of data and materials
The data that support the findings of this study are available for qualified researchers from, but restrictions for academic and not-commercial use apply to the availability of these data. Data are however available from annemarie.unger@meduniwien.ac.at upon reasonable request.








