1. Introduction
The pricing of marketised services remains ambiguous due to their unique features. This phenomenon is even more complex and intractable in healthcare services, where an inherent information asymmetry exists in their delivery. Hence, the pricing of hospital services warrants greater attention to ameliorate its structural complexity. However, the lack of consideration for pricing, particularly in hospital services, leads to deceptive and unfounded prices (Brown, Reference Brown2014). This enigmatic issue of hospital service pricing apparently grants considerable leeway for its perpetuation. Newhouse's (Reference Newhouse2002) restatement, ‘healthcare pricing is a conundrum’, reveals the complexity of pricing inherent in the system. The issue of healthcare pricing is complex and discriminatory, with significant variations observed for identical services, leading to a fractured healthcare market (Brown, Reference Brown2014). According to Thekkekara and Thiagarajan (Reference Thekkekara and Thiagarajan2019), this problem is multi-faceted and overwhelmingly intricate. Tompkins et al. (Reference Tompkins, Altman and Eilat2006) and Brown (Reference Brown2014) have indicated that the hospital pricing system is irrational and harmful. Rising costs are likely to hinder healthcare decision-making for both healthcare service providers, who may suffer a diminished reputation as excessively expensive, and patients, who may find services unaffordable. This has led health economics researchers to approach the issue of pricing from a multi-dimensional perspective, as evidenced by numerous studies (Harris, Reference Harris1979; Benz, Reference Benz1988; Bonnici, Reference Bonnici1992; Krishnan, Reference Krishnan2001; Waters and Hussey, Reference Waters and Hussey2004; Tompkins et al., Reference Tompkins, Altman and Eilat2006; Hsu, Reference Hsu2011; Brown, Reference Brown2014; Pandey and Raina, Reference Pandey and Raina2019; An et al., Reference An, Wang, Wu, Wang and Zhang2020). Furthermore, the fluctuation of costs for identical hospital services remains inadequately expounded upon (Park et al., Reference Park, Kim and Werner2015; Cooper et al., Reference Cooper, Craig, Gaynor and Reenen2018). Additionally, scholars have reiterated this pricing ambiguity (Babcock, Reference Babcock2019; Pandey and Raina, Reference Pandey and Raina2019). Therefore, a retrospective analysis of individual studies is necessary for knowledge synthesis and to pave the way for future research. The present study is a modest undertaking in relation to this issue.
Over the past five decades, reviews in this knowledge domain have been sporadic and scant. However, a review conducted three decades ago on issues related to healthcare service pricing suggested that pricing models should incorporate additional factors such as costs, competition and case mix (McKinney, Reference McKinney1990). In their study, Waters and Hussey (Reference Waters and Hussey2004) analysed costing and pricing methodologies for healthcare services purchased internationally. It is acknowledged that price-setting methods are influenced by provider and purchaser characteristics, payment systems for providers and the available information about costs, service volume and outcomes. A topic of contention among stakeholders and policymakers is the practice of cost-shifting in hospitals, which has been the subject of theoretical and empirical analysis (Frakt, Reference Frakt2011). The review concludes that while cost-shifting is present, it may not be consistent. An analysis by An et al. (Reference An, Wang, Wu, Wang and Zhang2020) has examined the effect of price reform policies on the economic performance of hospitals. Additionally, Pandey and Raina (Reference Pandey and Raina2019) conducted a systematic literature review on healthcare pricing, which revealed the various stages of evolution in healthcare pricing research.
Pandey and Raina's (Reference Pandey and Raina2019) recent review has neglected journal articles from prestigious databases such as Scopus and Web of Science. They focused on pricing for healthcare services that included the hospital, pharmaceutical, medical device, telemedicine and insurance sectors. It is our assertion that obtaining a complete understanding of the nuances of pricing hospital services is difficult when the synthesis of knowledge concerns various services that are structurally and operationally diverse. Therefore, we solely examine the pricing of hospital services in this review. Moreover, we address the consideration of pricing practices, strategies and methods that Pandey and Raina (Reference Pandey and Raina2019) neglected in their review. Therefore, there is a necessity for a comprehensive and methodical synthesis of evidence that is exclusively tailored to hospital service pricing. The existing literature is varied and disjointed, leaving a significant gap in knowledge that necessitates a detailed thematic review. Our objective is to address this gap by considering the literature from 1970 to February 2021 and formulating three questions to guide the direction of the review.
(1) How is hospital pricing of services portrayed in the literature?
(2) How has the literature addressed pricing objectives, strategies and practices for hospitals?
(3) What factors influence the pricing of hospital services?
This review provides several contributions to the literature. Firstly, it organises the varied and diverse results of primary research in this field of knowledge. Secondly, it elucidates the intricate and elusive nature of healthcare pricing. Thirdly, we analyse the pricing strategies and practices presented in the primary studies. We then collate the factors that affect hospital pricing. Finally, we suggest potential areas for further research in this field.
2. Methodology
A literature review is a crucial aspect of research that provides current information on a particular topic and justifies future studies of interest (Cronin et al., Reference Cronin, Ryan and Coughlan2008). This thematic synthesis follows the fivefold systematic review protocol proposed by Denyer and Tranfield (Reference Denyer, Tranfield, Buchanan and Bryman2009).
2.1 Formulation of research questions
We have developed three research enquiries to investigate how the current literature portrays the phenomenon of hospital service pricing and the factors that underpin it.
2.2 Search strategy
We conducted a literature search using electronic databases, including Scopus, Web of Science, ProQuest, Taylor and Francis Online, PubMed and Google Scholar. Our search terms consisted of ‘Hospital pricing’, ‘Pricing in Hospitals’, ‘Pricing Practices in hospitals’, ‘Price setting in hospitals’, ‘Pricing strategies in hospitals’, ‘Pricing of hospital services’ and ‘Pricing of services in hospitals’.
To avoid false matching, relevant keywords were used in the search process, with the search field limited to ‘Title, Abstract, Keywords’. The literature search was widened to cover from 1970 to 2021 to facilitate a deeper understanding of the thematic findings. The search was conducted in February 2021.
2.3 Selection process
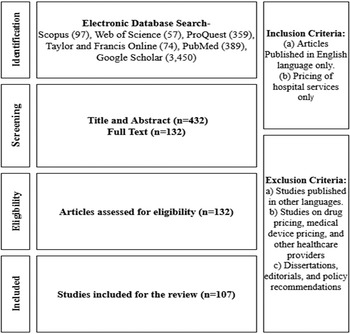
The online database search produced 97 outcomes in Scopus, 57 Web of Science articles, 359 search results in ProQuest, 74 documents on Taylor and Francis Online, 389 PubMed documents and 3,450 Google Scholar documents. The total retrieved publications were 4,426. After screening the titles and abstracts and eliminating duplicates, 432 records were considered. The primary author screened the shortlisted full texts and picked articles that addressed at least one of the research questions. The authors deliberated to create the final list. The full-text screening produced 132 documents. We included 107 articles for this review, excluding dissertations, editorials and policy recommendations. Figure 1 illustrates this process.
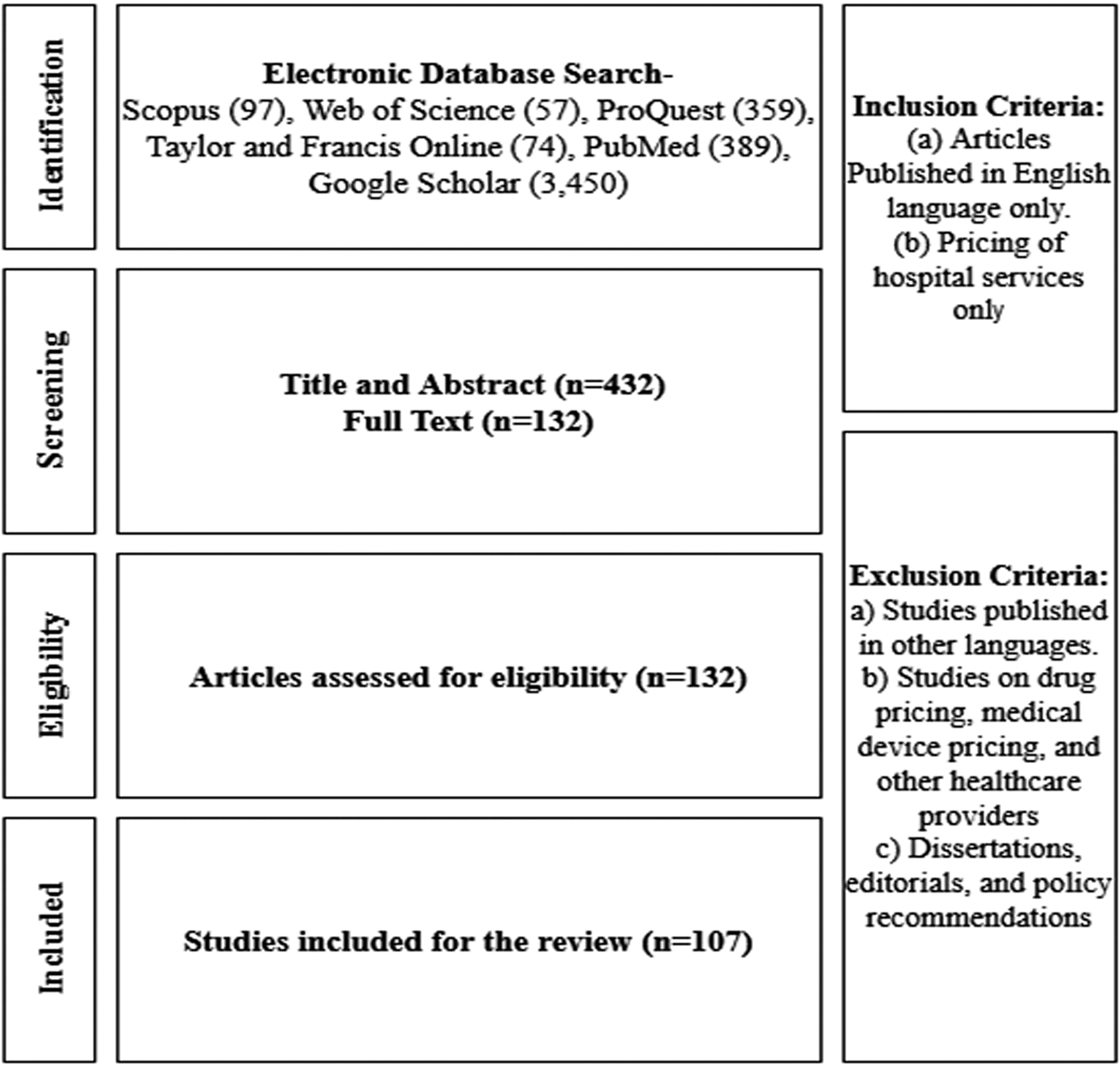
Figure 1. PRISMA 2020 flow chart.
Source: Current study.
All studies on hospital service pricing that met the inclusion criteria were selected for analysis. The review was limited to English-language articles and excluded studies on drug pricing, medical device pricing and pricing by other healthcare providers. Moreover, articles written in languages other than English were excluded. The articles retrieved were categorised based on the different themes identified during the search.
2.4 Data extraction, analysis and synthesis
The relevant data were extracted and recorded from selected articles in a pre-designed MS Excel template by the first author. The second author then cross-checked the data to ensure consistency and minimise potential loss (please refer to online supplementary file). The collected data were arranged in a custom table, which included the authors with their publication year, study title, study objectives/purpose, methodology, study location, key findings, inference and conclusion. The systematic extraction of data enabled the research team to analyse the crucial evidence from the literature. Both team members deliberated and moderated the obtained evidence in real-time. The extracted evidence was then reviewed again following thematic categorisation to improve accuracy in knowledge synthesis.
2.5 Reporting of results
The research adopted an interpretive and explanatory methodology in reviewing the main literature (Denyer and Tranfield, Reference Denyer, Tranfield, Buchanan and Bryman2009), to present the evidence and insights. A concise framework is provided in Table 1 to demonstrate the evidence synthesis in the subsequent section. The outcomes are presented in line with the guiding research inquiries.
Table 1. A snapshot of the thematic summary of the relevant manuscripts
Source: Current study.
Kindly change the year as 2017 instead of 2015
Kindly delete the in-text citation Eggleston et al. 2004
3. Findings
This section presents the review's findings, which are included in the study (please refer to the online supplementary file for details). The hospital service pricing issue has been scrutinised from various perspectives in academic literature. For example, Harris (Reference Harris1979), Brown (Reference Brown2014) and McKinney (Reference McKinney1990) note the elusiveness of hospital pricing. Meanwhile, Benz (Reference Benz1988) and Krentz and Jennings (Reference Krentz and Jennings1986) analyse the pricing goals of hospitals. Horowitz and Kleiman (Reference Horowitz and Kleiman1994) and Audibert et al. (Reference Audibert, Mathonnat, Pareil and Kabamba2007) provide an objective explanation of the pricing strategies employed by hospitals. Bonnici (Reference Bonnici1992) and Kleimenhagen et al. (Reference Kleimenhagen, Naidu and Pillari1994) discuss commonly observed pricing practices in hospitals. Oostenbrink and Rutten (Reference Oostenbrink and Rutten2006), Hsu (Reference Hsu2011), Raulinajtys-Grzybek (Reference Raulinajtys-Grzybek2014), Bahuguna et al. (Reference Bahuguna, Guinness, Sharma, Chauhan, Downey and Prinja2020) and Llewellyn et al. (Reference Llewellyn, Begkos, Ellwood and Mellingwood2020) investigate the precision of costing tools and methodologies utilised in price-setting by hospitals. Connor et al. (Reference Connor, Feldman and Dowd1998), Krishnan (Reference Krishnan2001), Ciliberto and Dranove (Reference Ciliberto and Dranove2006), Tenn (Reference Tenn2011), Haas-Wilson and Garmon (Reference Haas-Wilson and Garmon2011), Baker et al. (Reference Baker, Bundorf and Kessler2014) and Gowrisankaran et al. (Reference Gowrisankaran, Nevo and Town2015) have reflected upon the impact of organisational restructuring on pricing. Dranove et al. (Reference Dranove, Shanley and White1993), Propper (Reference Propper1996), Propper and Söderlund (Reference Propper and Söderlund1998), Melnick et al. (Reference Melnick, Keeler and Zwanziger1999), Moriya et al. (Reference Moriya, Vogt and Gaynor2010) and Wang and Chen (Reference Wang and Chen2017) provide insights into competition and concentration effects on hospital pricing. Harris (Reference Harris1979), Freisner and Rosenman (Reference Freisner and Rosenman2009), Melnick and Fonkych (Reference Melnick and Fonkych2008) and Moriya et al. examine related factors. Frakt (Reference Frakt2011), Robinson (Reference Robinson2011), Woodworth et al. (Reference Woodworth, Romano and Holmes2017), Wang and Chen (Reference Wang and Chen2017) and Cooper et al. (Reference Cooper, Craig, Gaynor and Reenen2018) have examined third-party reimbursements for hospital pricing practices, while Bai (Reference Bai2015) and Liu et al. (Reference Liu, Liu and Chen2000) have considered the regulatory implications of hospital pricing. Sheiner and Cutler (Reference Sheiner and Cutler1999) and Zuckerman et al. (Reference Zuckerman, Waidmann, Berenson and Hadley2010) discuss demand factors affecting hospital pricing, while Guerin-Calvert and Israilevich (Reference Guerin-Calvert and Israilevich2011) and Baker et al. (Reference Baker, Bundorf and Kessler2014) examine supply factors. A summary of the themes found in the manuscripts analysed as part of this study is presented in Table 1.
The research synthesis presents its findings in three sub-sections, organised by the guiding research questions. Section 3.1 addresses the elusive and intricate nature of hospital pricing. Section 3.2 examines the various pricing methods, practices and strategies deployed in hospital pricing. Lastly, section 3.3 explores the factors that impact the pricing of hospital services.
3.1 Elusiveness and complexity of hospital pricing
Hospital prices have been found to be illogical (Tompkins et al., Reference Tompkins, Altman and Eilat2006; Brown, Reference Brown2014), challenging to comprehend (Tengilimoglu and Dziegielewski, Reference Tengilimoglu and Dziegielewski2000) and intricate (Babcock, Reference Babcock2019; Pandey and Raina, Reference Pandey and Raina2019; Thekkekara and Thiagarajan, Reference Thekkekara and Thiagarajan2019). Harris (Reference Harris1979) hinted towards the lack of transparency on the criteria employed by hospitals for pricing, causing perilous and inadequately functioning price structures. Irrational hospital prices result in significant financial and health-related damages, and escalate costs excessively (Brown, Reference Brown2014). Hospital prices that do not correspond to the actual costs of providing healthcare services are opaque and exhibit significant inconsistencies (Brown, Reference Brown2014). McKinney (Reference McKinney1990) argues that service cost determination complexity is the main factor behind intricate pricing. Pricing can become laborious without sufficient information. Our views align with Krentz and Jennings (Reference Krentz and Jennings1986) in terms of the necessity to simplify pricing policies. In healthcare, price is considered as the fourth aspect of marketing, which serves as an offer to consumers (Leven, Reference Leven1984), representing the income and level of monetary reimbursement for the firm (McKinney, Reference McKinney1990; Tengilimoglu and Dziegielewski, Reference Tengilimoglu and Dziegielewski2000).
3.2 Hospital service pricing objectives, strategies and pricing practices
3.2.1 Pricing objective
The pricing strategy of hospitals varies depending on their purposes and objectives (Krentz and Jennings, Reference Krentz and Jennings1986). Krentz and Jennings (Reference Krentz and Jennings1986) identified several commonly used pricing objectives including profit maximisation, increasing market share, market skimming, maximising current revenues, target profit and promotional pricing. Establishing pricing objectives is a crucial and initial stage in the process of price development, regardless of the distinctive needs and resources available in hospitals (Benz, Reference Benz1988; Bonnici, Reference Bonnici1992). In the case of non-profit hospitals, the pricing objectives that financial managers aim to achieve are a reflection of their ambition to maximise net revenue, break even, generate target revenue and provide care for all patients requiring medical attention (Bauerschmidt and Jacobs, Reference Bauerschmidt and Jacobs1985). Benz's (Reference Benz1988) study acknowledges that an organisation's pricing objectives should align with its mission and goals and precede the pricing strategies of a hospital.
3.2.2 Pricing strategies
The importance of pricing indicates that pricing strategies are now a crucial element of any service delivery (Moore, Reference Moore1995). Increasing consumer price awareness, customer sophistication, deregulation and an expanding number of competitors have reignited interest in pricing strategies (McKinney, Reference McKinney1990). The healthcare sector has experienced a change in service pricing within the last decade. The three common pricing strategies are cost-oriented, demand-oriented and competition-oriented. The latter strategy can also be referred to as going-rate or imitative pricing (Krentz and Jennings, Reference Krentz and Jennings1986; McKinney, Reference McKinney1990). Various innovative pricing strategies have been discussed by scholars, including Illness Outcome Groups (IOGs) (Horowitz and Kleiman, Reference Horowitz and Kleiman1994), package pricing (Horowitz and Kleiman, Reference Horowitz and Kleiman1994; Tengilimoglu and Dziegielewski, Reference Tengilimoglu and Dziegielewski2000; Reinhardt, Reference Reinhardt2006; Tanwar et al., Reference Tanwar, Kumar and Mustafee2019) and reference pricing (Brown and Atal, Reference Brown and Atal2018; Nassiri et al., Reference Nassiri, Goodman and Mamani2020), marginal pricing and global budgets (Sutherland, Reference Sutherland2015; Malmmose et al., Reference Malmmose, Mortensen and Holm2018), pricing models for contracts (Teymourifar et al., Reference Teymourifar, Kaya and Ozturk2020), bundled payment pricing (Hellsten et al., Reference Hellsten, Chu, Crump, Yu and Sutherland2016) and cost accounting pricing models (Audibert et al., Reference Audibert, Mathonnat, Pareil and Kabamba2007; Thekkekara and Thiagarajan, Reference Thekkekara and Thiagarajan2019). Horowitz and Kleiman (Reference Horowitz and Kleiman1994) acknowledge that pricing strategies must reflect market competition realities and minimise financial risks for organisations. Therefore, if hospitals seek to progress in their pricing strategies, it is imperative that they focus more significantly on resolving operational, financial and information systems issues (Horowitz and Kleiman, Reference Horowitz and Kleiman1994).
3.2.3 Pricing practices
The service pricing literature frequently uses the terms ‘pricing strategies’ and ‘pricing practices’ interchangeably. As healthcare costs continue to rise, hospitals must have a defined strategic plan for analysing pricing practices. This requirement has been reiterated in the literature (Bonnici, Reference Bonnici1992; Kleimenhagen et al., Reference Kleimenhagen, Naidu and Pillari1994). Cross-subsidisation is the principal mechanism by which hospitals (David et al., Reference David, Lindrooth, Helmchen and Burns2014) subsidise unprofitable departments with profit-making departments. Mysterious within the literature, the pricing practice plays a critical role in compensating for inequities and distortions in existing health insurance coverage (Harris, Reference Harris1979). The literature provides anecdotal evidence of cross-subsidisation which is not thoroughly documented (David et al., Reference David, Lindrooth, Helmchen and Burns2014). Cross-subsidisation is defined by Harris (Reference Harris1979) as a kind of discriminatory pricing. This investigation reiterates that hospitals must deviate from the average cost pricing policy in a systematic way since it is not the most efficient pricing policy for them. Any optimal pricing policy should be based on marginal cost, co-payment rate, own price elasticity of demand, and the covariance between consumption and individual or social marginal utility of income. A study by Dittman and Morey (Reference Dittman and Morey1981) indicates that profit maximisation in a constrained hospital environment can cause cross-subsidisation.
Cost-shifting is a pricing strategy that has received extensive discussion in the literature on pricing (Dranove, Reference Dranove1988; Frakt, Reference Frakt2011; Robinson, Reference Robinson2011; Brown, Reference Brown2014, Malmmose et al., Reference Malmmose, Mortensen and Holm2018). This strategy involves using a differential pricing system to maintain profitability (Tompkins et al., Reference Tompkins, Altman and Eilat2006; Melnick and Fonkych, Reference Melnick and Fonkych2008). Research on cost-shifting within hospital settings has focused on price differences for insured and uninsured patients (Melnick and Fonkych, Reference Melnick and Fonkych2008; Woodworth et al., Reference Woodworth, Romano and Holmes2017). For cost-shifting to take place, the provider must have the ability to establish higher fees for some patients and lower fees for others (Freisner and Rosenman, Reference Freisner and Rosenman2009). A provider becomes restricted in doing so if an insurer decreases its reimbursement. However, providers shift costs solely when they cannot compensate their losses with cost or efficiency savings. The cost-shifting conduct is observable in hospitals that aim to maximise profits (Dranove, Reference Dranove1988). The practices have raised concerns among hospitals and insurance companies, although they are now less widespread than in past decades and not as significant a phenomenon of late (Frakt, Reference Frakt2011). It is important to note that the dynamic phenomenon of cost-shifting should not be confused with price discrimination, which is driven by differences in market power, as cost-shifting has a direct impact on prices charged (Frakt, Reference Frakt2011).
Cream-skimming is a practice that involves selecting patients based on characteristics other than their need for care and is well-documented in the literature (Newhouse, Reference Newhouse1984; Pauly, Reference Pauly1984; Matsaganis and Glennerster, Reference Matsaganis and Glennerster1994; Ellis, Reference Ellis1998; Barros, Reference Barros2003; Freisner and Rosenman, Reference Freisner and Rosenman2009; Berta et al., Reference Berta, Callea, Martini and Vittadini2010; Levaggi and Montefiori, Reference Levaggi and Montefiori2011; Cheng et al., Reference Cheng, Haisken-DeNew and Yong2015; Yang et al., Reference Yang, Chan, Cheng and Yong2020; Chen and Lang, Reference Chen and Lang2021; Kjøstolfsen et al., Reference Kjøstolfsen, Baheerathan, Martinussen and Magnussen2021). Cream-skimming involves selecting patients with lower-than-average costs in a prospective payment system such as a Diagnosis-Related Group (DRG), to maximise financial gains (Yang et al., Reference Yang, Chan, Cheng and Yong2020). Levaggi and Montefiori (Reference Levaggi and Montefiori2011) classify cream-skimming into horizontal and vertical categories. The limited evidence on cream-skimming practices highlights the need for further research to attain ample evidence.
3.3 Factors affecting the pricing of hospital services
The determinants influencing hospital service prices are shaped by the factors impacting the demand for care (Bonnici, Reference Bonnici1992). The drivers of patient's medical care demand are characteristically economic, incidence of illnesses and cultural-demographic factors (Feldstein, Reference Feldstein2005). Prices are also affected by internal and external factors. The internal factors comprise of the level of payer class, the level of uncompensated care due to lack of insurance and the adequacy of the underlying information systems/support. The external factors are the position of competitive costs, the total volume of services, the scope of the contract and the needs of the purchaser (Krentz and Jennings, Reference Krentz and Jennings1986). Heshmat (Reference Heshmat1989) has established a framework to achieve market-based pricing decisions, including pricing objectives, cost, demand analysis and competition. We have analysed the factors that affect the pricing of hospital services and will outline our findings in the following section.
3.3.1 Institutional factors
The hospital market is comprised of private for-profit, private not-for-profit and publicly owned and operated firms (Dranove, Reference Dranove1988; Duggan, Reference Duggan2000; Hsu, Reference Hsu2011). The pricing objectives differ depending on the hospital's ownership structure. For example, profit objectives can be attained by targeting either a return on investment or ‘satisfactory’ profit maximisation (Bonnici, Reference Bonnici1992), while non-profit objectives can be achieved by maximising net revenues (Heshmat, Reference Heshmat1992). Considerable emphasis has been placed on comprehending the pricing aims of non-profit healthcare facilities (Weisbrod, Reference Weisbrod1965; Bauerschmidt and Jacobs, Reference Bauerschmidt and Jacobs1985; Dranove, Reference Dranove1988; Heshmat, Reference Heshmat1992). A statistical analysis reveals that non-profit institutions charge more for their services than publicly owned hospitals (Hsia et al., Reference Hsia, Akosa Antwi and Weber2014). Additionally, for-profit hospitals charge more for interventions than any other facility (Hsia et al., Reference Hsia, Akosa Antwi and Weber2014). As public hospitals rely on tax funding to operate their services, pricing decisions are not vital for them.
Pricing practices for healthcare services are assessed according to the teaching and non-teaching status of hospitals, as evidenced by studies conducted by Newhouse (Reference Newhouse2003), White et al. (Reference White, Reschovsky and Bond2014), Burke et al. (Reference Burke, Khullar, Zheng, Frakt, Orav and Jha2019) and Kotwal et al. (Reference Kotwal, Abougergi and Wright2019). The findings suggest that teaching hospitals, which offer education and training for medical practitioners and treat complex cases, tend to be more costly than non-teaching establishments (Koenig et al., Reference Koenig, Dobson, Ho, Siegel, Blumenthal and Weissman2003; Hsu, Reference Hsu2011; Burke et al., Reference Burke, Khullar, Zheng, Frakt, Orav and Jha2019). Price variations also occur depending on the location where the service is provided. Prices differ depending on the services offered in various healthcare settings, including hospital outpatient departments. (Sledge et al., Reference Sledge, Tebes, Wolff and Helminiak1996; Hsu, Reference Hsu2011; Higgins et al., Reference Higgins, Veselovskiy and Schinkel2016; Babcock, Reference Babcock2019). Studies have shown that healthcare services provided in rural areas are generally less expensive than those in urban regions. However, in rural healthcare markets, prices can be higher due to lower patient volumes and increased overhead costs. Moreover, larger hospitals that offer numerous services may establish higher fees for their services in comparison to their smaller counterparts (Hsu, Reference Hsu2011). Therefore, the different fees for services can be attributed to variable pricing approaches based on the institutions' pricing goals.
3.3.2 Cost factors
To ensure efficient use of healthcare financial resources while maintaining price transparency, scholars have called for the development of strong cost accounting techniques (Tengilimoglu and Dziegielewski, Reference Tengilimoglu and Dziegielewski2000; Tompkins et al., Reference Tompkins, Altman and Eilat2006). Additionally, they have emphasised the importance of hospitals understanding their cost structures (Sutherland, Reference Sutherland2015). Much of the international evidence highlights the need for reliable cost-accounting techniques to support cost-based pricing (Raulinajtys-Grzybek Reference Raulinajtys-Grzybek2014). While Davis (Reference Davis1971) suggests that pricing should not always be based on costs, implementing a costing mechanism can facilitate transparent and efficient management of financial resources (Audibert et al., Reference Audibert, Mathonnat, Pareil and Kabamba2007). Additionally, such a mechanism is crucial for achieving revenue optimisation (Karaesmen and Nakshin, Reference Karaesmen and Nakshin2007). Therefore, there are current academic endeavours to implement costing methodologies comprising step-down approaches (Audibert et al., Reference Audibert, Mathonnat, Pareil and Kabamba2007) or bottom-up approaches (Sangwan et al., Reference Sangwan, Shankar, Sameer, Jagnoor, Pankaj and Rebecca2017; Thekkekara and Thiagarajan, Reference Thekkekara and Thiagarajan2019) and to construct cost models that encompass input expenses or service quantities to achieve the objective of cost-effectiveness in pricing (Tompkins et al., Reference Tompkins, Altman and Eilat2006). Activity-based costing in hospitals offers both value extraction and creation whilst enhancing healthcare service quality (Llewellyn et al., Reference Llewellyn, Begkos, Ellwood and Mellingwood2020).
Accurately measuring healthcare costs and gathering associated cost information is crucial for healthcare providers in both setting prices and arranging reimbursement (Krentz and Jennings, Reference Krentz and Jennings1986; Raulinajtys-Grzybek, Reference Raulinajtys-Grzybek2014). Hu (Reference Hu1971) studies the pricing behaviour of hospitals and uses maternity care as a case study to assess hospital costs. The provision of cost information for cost-plus pricing enables price setters to make informed decisions on resource allocation (Bahuguna et al., Reference Bahuguna, Guinness, Sharma, Chauhan, Downey and Prinja2020). Cost information comprises of fixed and variable costs, cost per care, costs related to outlier cases, costs specific to physicians, costs incurred per day of stay, payor-specific costs and so on (Horowitz and Kleiman, Reference Horowitz and Kleiman1994). Achieving pricing based on cost data is possible only when there is uniformity in cost calculation methods. However, cost-based pricing fails to consider the dynamics of a marketplace (Krentz and Jennings, Reference Krentz and Jennings1986).
3.3.3 Supply factors
Guerin-Calvert and Israilevich (Reference Guerin-Calvert and Israilevich2011) suggest that hospital prices are determined by both labour and non-labour factors associated with the supply of hospital resources. Provider service factors comprise of physicians providing specialty services at hospitals (Zuckerman et al., Reference Zuckerman, Waidmann, Berenson and Hadley2010) and physicians' practice type (Reschovsky et al., Reference Reschovsky, Hadley, Saiontz-Martinez and Boukus2011). Specialty physician services are a primary cost generator for hospital services (Feldstein, Reference Feldstein1970; Guerin-Calvert and Israilevich, Reference Guerin-Calvert and Israilevich2011). The rising costs of physicians have led to the proposal and development of pricing models to contain the expenses (Feldstein, Reference Feldstein1970) and to assess the impact of hospital–physician integration on costs (Baker et al., Reference Baker, Bundorf and Kessler2014). Various factors such as the structure of the healthcare delivery system, reimbursement systems, high consumer switching costs and differences in the training of physicians have been attributed to the increasing physician service prices (Sheiner and Cutler, Reference Sheiner and Cutler1999). Disagreements among medical professionals regarding treatments, financial incentives for physicians and the quantity of physicians in healthcare settings all have an impact on pricing for hospital physician services. Hospital costs also include the salaries and benefits of nurses, technicians and numerous other personnel (Guerin-Calvert and Israilevich, Reference Guerin-Calvert and Israilevich2011).
The provision of specialised clinical services by hospitals using high-tech services commands a higher price-cost margin, indicating an evident manifestation of price escalation (Dranove et al., Reference Dranove, Shanley and White1993). High and ever-increasing healthcare costs are mainly driven by ceaseless innovations in medical technologies for diagnosis and treatments (Bodenheimer, Reference Bodenheimer2005), invariably leading to price escalation. The pricing of hospital services is closely associated with the blend of services provided and the level and type of care offered by each hospital, thereby leading to regional variations in the costs of hospital services (Dranove et al., Reference Dranove, Shanley and White1993; Guerin-Calvert and Israilevich, Reference Guerin-Calvert and Israilevich2011).
3.3.4 Demand factors
The demand for healthcare services relies on a range of patient characteristics. Several quantitative studies have taken into account factors such as race, income, age, individual treatment preferences, marital status, education, employment and income levels. These characteristics influence demand and thus have an impact on healthcare pricing (Bonnici, Reference Bonnici1992; Sheiner and Cutler, Reference Sheiner and Cutler1999; Zuckerman et al., Reference Zuckerman, Waidmann, Berenson and Hadley2010; White et al., Reference White, Reschovsky and Bond2014). Moreover, scholars contend that specific geographical regions have comparatively weaker populations than others. The health status of a region's population can be evaluated based on various measurements, such as the percentage of smokers and individuals with hypertension, as well as rates of obesity, sedentary lifestyles, hospitalisation for hip fractures and incidences of heart attacks, strokes, gastrointestinal bleeding, surgeries for lung or colon cancers and myocardial infarction (Sheiner and Cutler, Reference Sheiner and Cutler1999; Zuckerman et al., Reference Zuckerman, Waidmann, Berenson and Hadley2010). The severity of a patient's health condition is a precursor to the level of care provided at hospitals and subsequently affects pricing.
The literature on hospital pricing of services based on case-mix has focused on payment reimbursements (Jencks et al., Reference Jencks, Dobson, Willis and Feinstein1984; Wiley, Reference Wiley1992; Oostenbrink and Rutten, Reference Oostenbrink and Rutten2006). For example, hospitals in developed countries have implemented prospective payment systems through DRGs that are based on the case-mix of patients. These classification systems have been found to lower healthcare costs (Lewis, Reference Lewis1984; Benz, Reference Benz1988; Corti et al., Reference Corti, Avossa, Schievano, Gallina, Ferroni, Alba, Dotto, Basso, Netti, Fedeli and Mantoan2018). Corti et al. (Reference Corti, Avossa, Schievano, Gallina, Ferroni, Alba, Dotto, Basso, Netti, Fedeli and Mantoan2018) have created a clinical group system that is risk-adjusted to account for variations in healthcare costs. Hof et al. (Reference Hof, Fügener, Schoenfelder and Brunner2017) posit that using case-mix to establish cost-efficiency highlights the uncertainty surrounding the price-setting protocols adopted by hospitals. This case-mix consists of a precise combination and number of patients, which, under the DRG pricing strategy, can potentially benefit healthcare facilities economically (Hof et al., Reference Hof, Fügener, Schoenfelder and Brunner2017).
3.3.5 Market structure
Hospitals demonstrate monopolistic market behaviour as they establish their prices by distinguishing their services on various parameters, including location, range of services, quality and level of sophistication (Dranove, Reference Dranove1988; Hsu, Reference Hsu2011). Scholars investigate how organisational changes, such as mergers and vertical integrations, impact the pricing of hospital services (Connor et al., Reference Connor, Feldman and Dowd1998; Melnick et al., Reference Melnick, Keeler and Zwanziger1999; Krishnan, Reference Krishnan2001; Haas-Wilson and Garmon, Reference Haas-Wilson and Garmon2011; Tenn Reference Tenn2011; Baker et al., Reference Baker, Bundorf and Kessler2014; Gowrisankaran et al., Reference Gowrisankaran, Nevo and Town2015). Connor et al. (Reference Connor, Feldman and Dowd1998) observe that merging hospitals horizontally and consequently changing their functions can lead to average cost savings, which, in turn, may have a dampening effect on the prices charged by such hospitals. Nonetheless, Tenn (Reference Tenn2011) verified an increase in inpatient prices post-merger. Anti-competitive mergers may cause prices for services to soar due to hospitals having increased market power (Baker et al., Reference Baker, Bundorf and Kessler2014). Prices for services in hospitals that have merged with different ownership types have increased, according to Melnick et al. (Reference Melnick, Keeler and Zwanziger1999). Therefore, mergers between hospitals can cause prices for the same services to be ambiguous compared to other hospitals. We found some evidence of vertical integration affecting hospital prices. However, Ciliberto and Dranove (Reference Ciliberto and Dranove2006) found no evidence of higher prices resulting from the vertical integration of hospitals. Baker et al. (Reference Baker, Bundorf and Kessler2014) demonstrated that hospitals which underwent vertical integration raised their service prices. Despite an increase in hospital prices and spending, the prices of physician services significantly reduced following vertical integration with physician practices (Baker et al., Reference Baker, Bundorf and Kessler2014).
Hospital concentration has no significant relationship with hospital service prices, according to Moriya et al. (Reference Moriya, Vogt and Gaynor2010). In contrast, Robinson (Reference Robinson2011) has found empirical evidence that hospitals in concentrated markets raise their prices to private insurers in case of payment shortfalls. The literature has evaluated the effect of competition on the pricing behaviour of for-profit and not-for-profit hospitals (Melnick et al., Reference Melnick, Zwanziger, Bamezai and Pattison1992, Reference Melnick, Keeler and Zwanziger1999). Non-price competitions based on factors such as the quality of care, features, amenities and location of hospitals contribute to the high cost of competing hospitals (Heshmat, Reference Heshmat1989). However, a shift from non-price to price competition has resulted in lower costs for hospitals (Melnick et al., Reference Melnick, Keeler and Zwanziger1999). The evolution of hospital market concentration has seen pricing become a key consideration (Keeler et al., Reference Keeler, Melnick and Zwanziger1999). The implementation of such a transition can potentially undermine the role of technology and specialised healthcare services in enhancing the quality of healthcare. It is worth noting, however, that the growth in productivity and advancements in technology must be assessed in the context of service pricing (Tengilimoglu and Dziegielewski, Reference Tengilimoglu and Dziegielewski2000; Tompkins et al., Reference Tompkins, Altman and Eilat2006). Based on the synthesis of literature, there is no clear consensus on the influence of market structures and strategic decisions on hospital pricing.
3.3.6 Pricing regulation
The healthcare sector is characterised by market failures, which necessitates the regulation of healthcare service pricing. One branch of literature on price regulation has investigated the impact of legislation on the fluctuation of hospital service charges (Liu et al., Reference Liu, Liu and Chen2000; Bai, Reference Bai2015; McClintock et al., Reference McClintock, Ye, Mahek, Benjamin and Steven2019). Thus, such regulations are involved in this pricing process. The literature on regulatory aspects of pricing presents evidence that healthcare providers do not strictly adhere to the regulated prices. For example, Liu et al. (Reference Liu, Liu and Chen2000) examined the impact of hospital pricing policies in China and identified that regulatory prices were inadequate in covering all the costs. Consequently, hospitals resorted to charging significantly more for services that used advanced technologies and drugs to offset the losses incurred by hospitals. Similarly, Bai (Reference Bai2015) evaluated the effect of the legislation on uninsured patients. The research uncovered that the legislation facilitated a decrease in prices payable by those without insurance. In a similar vein, McClintock et al. (Reference McClintock, Ye, Mahek, Benjamin and Steven2019) conducted a study that revealed how the extension of Medicaid under the Affordable Care Act (ACA) 2010 in the United States did not result in an increase of charges to private patients by safety net hospitals despite reimbursement reductions for those without insurance.
3.3.7 Third-party reimbursements
Price differences between insured and uninsured patients have been highlighted. Uninsured patients are charged higher prices and receive less comprehensive care (Reinhardt, Reference Reinhardt2006; Tompkins et al., Reference Tompkins, Altman and Eilat2006; Melnick and Fonkych, Reference Melnick and Fonkych2008; Robinson, Reference Robinson2011; Batty and Ippolito, Reference Batty and Ippolito2017). This indicates that a patient's ability to possess insurance affects the amount they are charged for hospital services and the level of healthcare services they receive at hospitals. A distinct pricing system is implemented for patients based on the third-party payer's identity (Reinhardt, Reference Reinhardt2006; Tompkins et al., Reference Tompkins, Altman and Eilat2006; Anderson, Reference Anderson2007; Bai and Andersen, Reference Bai and Andersen2018). Patients may be insured by public or private payers, resulting in dissimilar prices within and across hospitals depending on the contract type and the agreed-upon service costs between the payers and providers (Barros and Martinez-Giralt, Reference Barros and Martinez-Giralt2008; Bai and Anderson, Reference Bai and Anderson2016). Cooper et al. (Reference Cooper, Craig, Gaynor, Harish, Krumholz and Van Reenen2019) investigated the increase in insurer-negotiated physician prices for care rendered in hospitals, as well as the growth in hospital prices and found an increase in hospital prices. This highlights the need for policymakers to address hospital price hikes in the context of third-party reimbursement. Additionally, policymakers should tackle the issue of price disparities among insured and uninsured patients in hospitals.
Contracting. Contracting is the process of establishing agreements between hospitals and third-party entities. According to Oostenbrink and Rutten (Reference Oostenbrink and Rutten2006), reimbursement prices are determined by contracts between hospitals and insurers. Prior to negotiating contracts with third parties, hospitals first develop a pricing strategy (Barros and Martinez-Giralt, Reference Barros and Martinez-Giralt2008). Insurers, on the other hand, place significant importance on healthcare quality when establishing contracts with hospitals (Magid et al., Reference Magid, Murphy, Lankiewicz, Lawandi and Poulton2017). Price contracts may incorporate discounts on fees, case-based reimbursements, per diem reimbursements and capitated payments (Horowitz and Kleiman, Reference Horowitz and Kleiman1994; Wu, Reference Wu2009). Some literature suggests creating novel contract mechanisms and pricing strategies between private hospitals and governments (Teymourifar et al., Reference Teymourifar, Kaya and Ozturk2020). Contractual mechanisms can significantly enhance health system performance, especially when public hospitals face a reduction in capacity. In their 2012 publication, Robinson and McPherson discuss ‘centres-of-excellence contracting’, in which patients are directed towards hospitals that offer high-quality care at discounted rates in exchange for an increased volume of patients.
Reference pricing. Setting a reference price as the upper limit of charges to be reimbursed by the insurer is reference pricing, a recently originated phenomenon (Robinson and MacPherson, Reference Robinson and MacPherson2012; Brown and Atal, Reference Brown and Atal2018; Nassiri et al., Reference Nassiri, Goodman and Mamani2020). The literature on reference pricing centres around service prices, their link with insurer spending, as well as an analysis of the reference pricing payment system and its impact on patients, competing providers and insurers (Robinson and MacPherson, Reference Robinson and MacPherson2012; Brown and Atal, Reference Brown and Atal2018; Nassiri et al., Reference Nassiri, Goodman and Mamani2020). While reference pricing presents a promising payment system for shoppable healthcare services and incentivises patients to choose more economical options, it also has cost-reducing benefits for hospitals (Nassiri et al., Reference Nassiri, Goodman and Mamani2020). This pricing practice has led to a decline in total per-procedure expenditure for providers and subsequently impacts hospital pricing practices and their profitability. Nassiri et al. (Reference Nassiri, Goodman and Mamani2020) suggest that hospitals are viewed as value-based providers by insurers when they charge patients the reference price or less. This impacts the hospital's reputation and eventual profitability. The methodological reliability of reference pricing studies was assessed by Robinson et al. (Reference Robinson, Brown, Whaley and Bozic2015a, Reference Robinson, Brown, Whaley and Finlayson2015b) and Brown and Atal (Reference Brown and Atal2018). The impact of reference pricing was investigated on care outcomes, including the choice of care venue, overall costs and treatment complications, for procedures such as arthroscopy and colonoscopy (Robinson et al., Reference Robinson, Brown, Whaley and Bozic2015a, Reference Robinson, Brown, Whaley and Finlayson2015b). Future studies are needed to examine the effect of reference pricing schemes on pricing for hospital services.
4. Discussion
The pricing of hospital services is a multifaceted process influenced by an array of services provided by hospitals. Hospitals face significant pressure to offer services at affordable prices to ensure accessibility for patients. The issue of hospital pricing remains largely ignored and persists to this day. This study aimed to comprehend how hospitals establish their pricing decisions by surpassing prior research. The literature review revealed the factors that affect hospital pricing, pricing objectives, practices and strategies in the hospital context. Our findings attest to the fact that hospital service pricing can be examined from multiple perspectives, and that these are interconnected. For example, Keeler's et al. (Reference Keeler, Melnick and Zwanziger1999) study explored the interplay between competition, institutional factors and hospital pricing behaviour. The literature on pricing is limited during the period of 1970–1995 and its coverage is scant (Harris, Reference Harris1979; Leven, Reference Leven1984; Krentz and Jennings, Reference Krentz and Jennings1986; Benz, Reference Benz1988; McKinney, Reference McKinney1990; Bonnici, Reference Bonnici1992; Horowitz and Kleiman, Reference Horowitz and Kleiman1994). The pricing of hospital services is a multifaceted process and can be seen as both intricate (Thekkekara and Thiagarajan, Reference Thekkekara and Thiagarajan2019; Babcock, Reference Babcock2019; Pandey and Raina, Reference Pandey and Raina2019) and discriminatory (Harris, Reference Harris1979).
The study examined pricing goals (Bauerschmidt and Jacobs, Reference Bauerschmidt and Jacobs1985), tactics (McKinney, Reference McKinney1990; Horowitz and Kleiman, Reference Horowitz and Kleiman1994; Tengilimoglu and Dziegielewski, Reference Tengilimoglu and Dziegielewski2000), as well as prevalent pricing approaches, including cost-shifting (Tompkins et al., Reference Tompkins, Altman and Eilat2006; Melnick and Fonkych, Reference Melnick and Fonkych2008) and cross-subsidy (Dittman and Morey, Reference Dittman and Morey1981). Previous research has examined the effects of whether hospitals have teaching status or not on pricing (Burke et al., Reference Burke, Khullar, Zheng, Frakt, Orav and Jha2019), the care setting (Higgins et al., Reference Higgins, Veselovskiy and Schinkel2016), hospital size (Hsu, Reference Hsu2011), cost structures (Sutherland, Reference Sutherland2015; Llewellyn et al., Reference Llewellyn, Begkos, Ellwood and Mellingwood2020), DRG pricing (Corti et al., Reference Corti, Avossa, Schievano, Gallina, Ferroni, Alba, Dotto, Basso, Netti, Fedeli and Mantoan2018) and reference pricing (Nassiri et al., Reference Nassiri, Goodman and Mamani2020). Pricing literature for hospitals may be categorised according to institutional, cost, supply, demand, market structure, regulatory and third-party reimbursement factors. Recent pricing innovations in hospital services – such as case-mix pricing, reference pricing, bundled payments, global budgets, contractual mechanisms – were not previously anticipated within hospital service pricing. The latest pricing mechanisms provide possibilities for additional research, particularly within the context of developing countries.
Following Cronin et al.'s (Reference Cronin, Ryan and Coughlan2008) advice, this study reports methodological diversities in the literature. For example, Dranove (Reference Dranove1988) constructed an econometric model to illustrate how price determination, patient treatment costs, number of services provided and profit factors influence profit maximisation in hospitals. The findings of a panel data analysis (Hsu, Reference Hsu2011) suggest a direct link between hospital prices and the cost of operations, which are in turn influenced by the level of capacity utilisation and demand variability. Tanwar et al. (Reference Tanwar, Kumar and Mustafee2020) devised a pricing model to determine the optimal price in the face of cost uncertainty. Ciliberto and Dranove (Reference Ciliberto and Dranove2006) utilised a fixed regression model to examine the impact of vertical integration on the pricing of privately insured patients. Many studies have utilised secondary data sources for their empirical analysis, providing opportunities to explore alternative methodological approaches for studying hospital service pricing.
However, the main limitation of this study is the methodology employed for literature search, omitting substantial publications of grey literature like magazines and conference papers. Therefore, there is a possibility of missing significant information. Moreover, we observe disciplinary overlaps in the pricing of hospital services from a conceptual point of view. The pricing phenomenon is within the scope of social science, while its specific setting falls under medical science. These disciplinary attributes influence our understanding of the subtleties of hospital pricing. The hospitals' diverse and conflicting objectives, strategies and practices may have impeded the synthesis of relevant evidence from literature. The pricing literature's dynamic nature provides extensive evidence to recognise the intricate nature of the pricing phenomenon in hospitals.
5. Scope for future research
Based on the review, we have identified specific areas that require additional research and evidence to understand hospital pricing. Firstly, hospital service pricing is complex and obscure (Brown, Reference Brown2014). Therefore, more research on pricing methods is needed to increase the transparency of the pricing process. The World Health Organization's report, as outlined by Barber et al. (Reference Barber, Lorenzoni and Ong2019), elucidated pricing and payment systems applicable to developed nations. Consequently, additional study on pricing and payment systems in developing countries is necessary. Research on pricing in emerging economies such as India is inadequate. Future scholars are advised to concentrate on pricing mechanisms in low- and middle-income countries as well.
Secondly, the literature lacks an appropriate pricing strategy for hospitals, with pricing terms often used interchangeably. The ambiguity of terms such as ‘cost’, ‘price’ and ‘charge’ can lead to confusion. Additionally, there is an absence of clarity regarding ‘pricing practices’ and ‘pricing strategies’. Future researchers should focus on operationalising these terms to provide a clear structure and deeper understanding.
Thirdly, it is widely believed that unfulfilled healthcare requirements provide an opportunity for providers to engage in price skimming. However, there is insufficient evidence in the literature to demonstrate its occurrence. Therefore, investigating cream-skimming pricing practices could be a promising avenue for future research.
Fourthly, it is essential to conduct studies investigating the interplay between health insurance and hospital pricing practices for the development of appropriate policy frameworks and effective regulatory interventions. In addition, the role of technology in pricing hospital services is still up for debate. Proper scholarly intervention can aid in resolving this theoretical tension.
Lastly, comprehending the challenges confronted by hospitals in pricing is vital. This approach can only be achieved through engaging in discussions and conducting interviews with hospital managers or heads of hospitals.
No peer-reviewed studies have been found that explore hospitals' pricing practices. However, to achieve better pricing solutions, it is essential to comprehend pricing methods in hospitals. This can be achieved by employing qualitative methods such as interviews and focus group discussions with hospital managers and administrators.
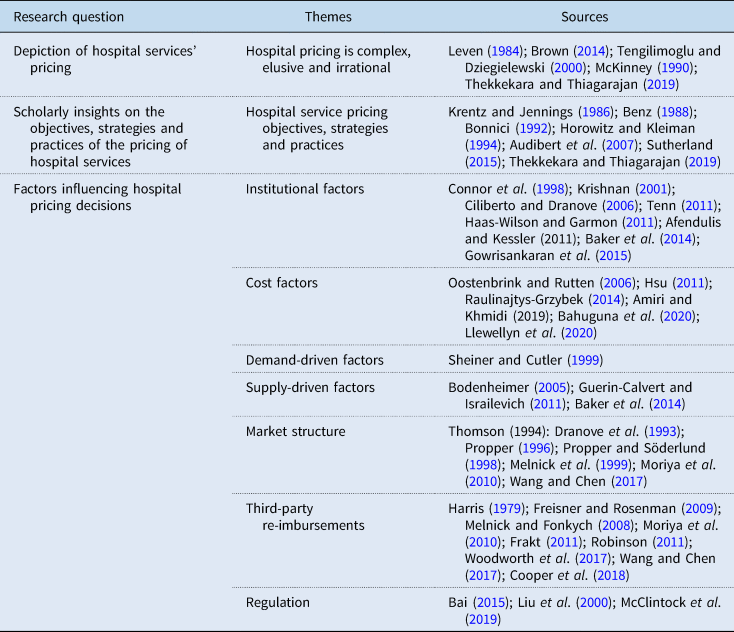
Additionally, we propose to conduct multiple research investigations into the factors that impact the pricing of healthcare services, as presented in Table 2.
Table 2. Tentative research questions
Source: Current study.
The research questions are aligned with the factors that impact hospital pricing to provide clear focus. Institutional factors, including locational specificity, ownership, size, operational structure and the extent of specialty services offered, are crucial in determining pricing practices within hospitals. Similarly, the validity of co-payment arrangements in health insurance policies is also under scrutiny due to increasing out-of-pocket expenses (Sugunan et al., Reference Sugunan, Pillai and George2023) in recent times.
The study has produced a conceptual diagram outlining the factors that affect hospital service pricing, as shown in Figure 2. The primary aim of this study was to uncover the factors that influence the pricing mechanism due to its perceived ambiguity and complexity. These factors include institutional, cost, demand and supply, market structure, regulatory requirements and third-party reimbursement.
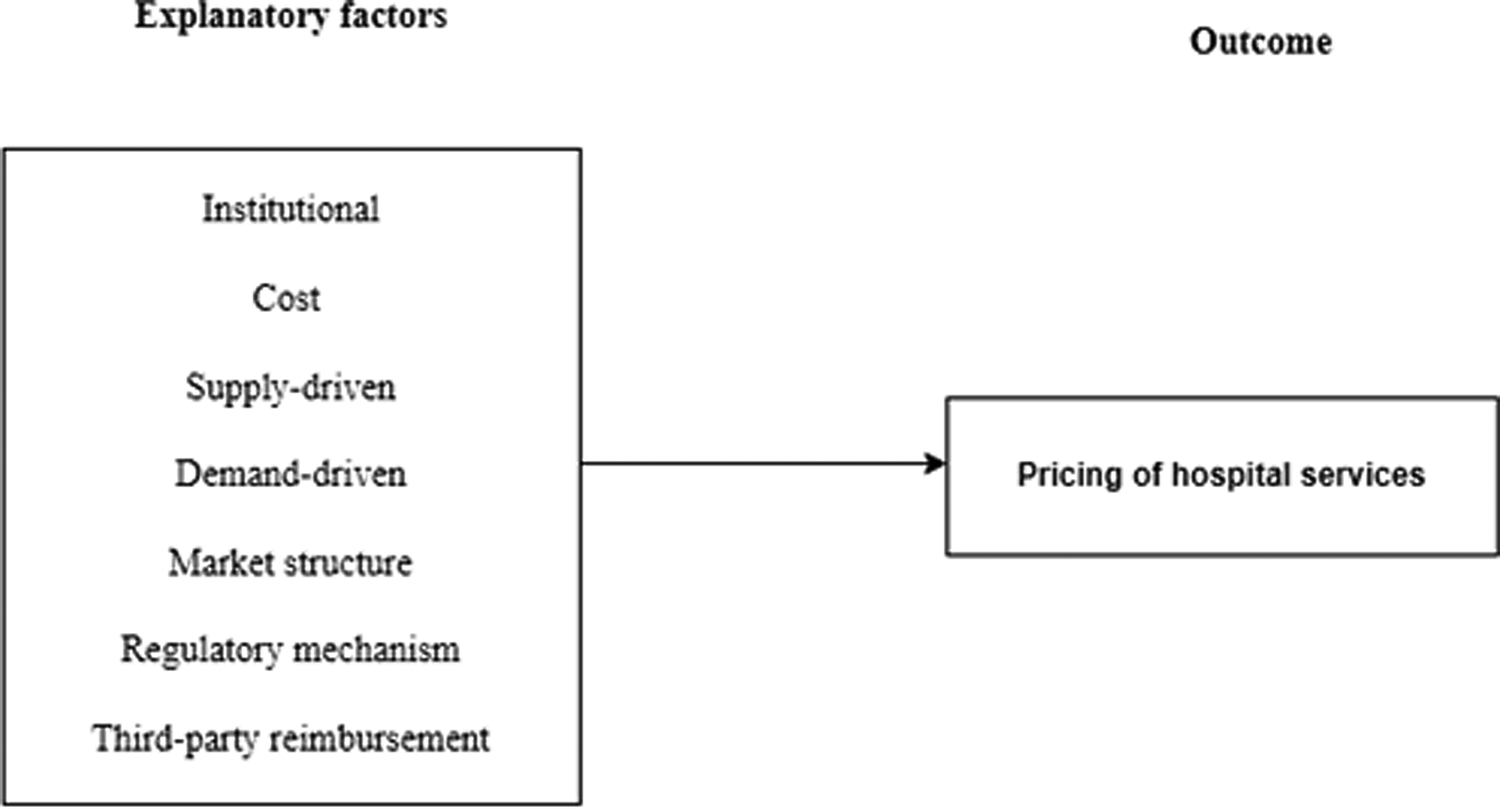
Figure 2. Factors influencing pricing of hospital services.
Source: Current study.
The literature review indicates that multiple factors influence hospital service pricing practices, demonstrating the inherent complexity of this area. This study has organised these factors into specific themes, as shown in Figure 3, to provide a clearer understanding of each individual dimension.
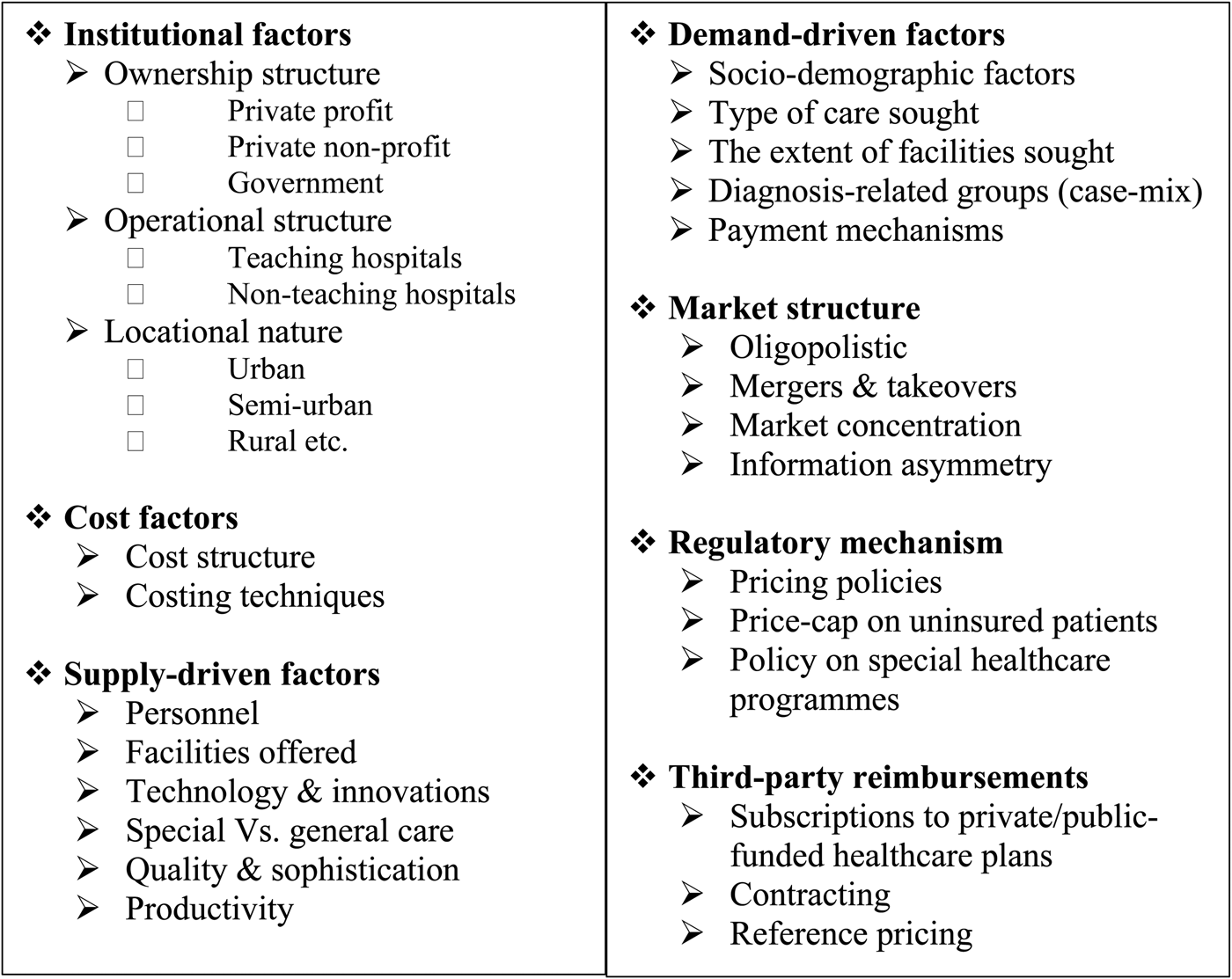
Figure 3. Dimensions of the factors influencing pricing for hospital services.
Source: Current study.
6. Conclusion
Prices impact the supply and demand of services, which ultimately affects the profitability of businesses. Despite its impact on profitability, there's a dearth of interest in service pricing in both theoretical and empirical contexts. The healthcare services market doesn't follow a traditional buyer and seller structure, making healthcare pricing complex for both patients and providers. Patients are insensitive to prices when seeking hospital services due to their necessity. From the healthcare providers' perspective, prices play a crucial role in determining the required resources and providing incentives for efficient, comprehensive and high-quality delivery of healthcare. The unquantifiable characteristics of services make their pricing challenging and distinct from that of tangible products. Pricing remains an underutilised management tool. Factors such as third-party payers or insurers' involvement, incomplete information and inadequate cost measurement processes impact the focus on pricing hospital services.
We have compiled the factors that underpin hospital pricing literature into five themes: institutional factors, costs, supply factors, demand factors, price regulation and third-party reimbursements. These factors amalgamate to affect pricing of hospital services. For example, reimbursement systems differ between private and public providers. Additionally, the literature documents pricing objectives and strategies. Furthermore, the study has revealed evidence of cream-skimming, cost-shifting and cross-subsidisation practices in hospitals. Our research suggests that service pricing in hospitals is context-dependent. There are no definitive pricing policies or ideal prices that align with a country's health system objectives. Despite the vast evidence on pricing, it is extensively fragmented, and a specific focus on pricing in low- and middle-income countries is necessary.
Supplementary material
The supplementary material for this article can be found at https://doi.org/10.1017/S1744133123000397.
Acknowledgement
The authors would like to thank Department of Commerce and Manipal Institute of Management, Manipal Academy of Higher Education, Manipal, Karnataka, India for providing the resources during the research period.
Financial support
No financial support was obtained for this study.
Competing interests
There are no conflicts of interest for this study.