Depression is a common psychiatric disorder and a major contributor to mortality and morbidity worldwide. Over the past decade in Sweden, work absence because of mental ill health has risen markedly and depression is a major factor. 1 Substantial societal costs are associated with the disorder, which affects up to 15% of the population at any one time and tends to be recurrent. Reference Sobocki, Jonsson, Angst and Rehnberg2 There are compelling reasons to investigate alternative treatments for depression. Although effective treatments exist, most people with the disorder never seek professional help. Among those that do, only half appear to benefit. Reference Forsell3 Adherence with medication is often poor and waiting times for cognitive–behavioural therapy (CBT) can be lengthy, resulting in more entrenched symptoms and a worse long-term prognosis. As general medical practitioners are frequently the main care providers for depression, treatment options that are non-stigmatising, have few side-effects and can readily be prescribed in community healthcare settings are needed.
Prescribed physical exercise has been proposed by many as an effective alternative treatment for depression and meta-analysis has demonstrated effect sizes ranging from −0.80 to −1.1. Reference Rethorst, Wipfli and Landers4 A recent Cochrane review of 32 randomised controlled trials (RCTs) concluded that exercise is moderately more effective than a control intervention for reducing the symptoms of depression. Reference Rimer, Dwan, Lawlor, Greig, McMurdo and Morley5 Several models have been proposed to explain the benefits of regular exercise on mood disorders. They include changes in core body temperature, increased serotonin synthesis and hippocampal cell proliferation Reference Dunn and Jewell6,Reference Bjornebekk, Mathe and Brene7 and reduced levels of proinflammatory cytokines. Reference Eyre, Papps and Baune8 Psychological theories suggest that distraction, mastery and improved self-efficacy also play a role. Reference Barbour, Edenfield and Blumenthal9 Internet-based interventions to promote health have expanded greatly over the past decade. Reference Cuijpers, van Straten and Andersson10 Such interventions have the advantage of being able to reach individuals without access to conventional treatment. This includes people living in rural or remote areas and individuals with mobility issues. Like exercise, internet-based therapy may also help to reduce patient waiting times for treatment. CBT is considered a first-line treatment for depression with strong empirical support. Reference Cuijpers, van Straten, Andersson and van Oppen11 CBT can be made available via the internet in the form of guided self-help. Internet-based CBT (ICBT) engages patients in structured programmes of care through online modules with limited online message support from a qualified therapist. Several RCTs have assessed the effectiveness of ICBT on depression. Reference Moritz, Schilling, Hauschildt, Schroder and Treszl12,Reference Wagner, Horn and Maercker13 A recent review concludes that internet-based psychological treatments can be equally effective in treating mild to moderate depression as face-to-face CBT. Reference Andersson, Cuijpers, Carlbring, Riper and Hedman14
Physical exercise for depression is currently recommended in Sweden and ICBT-interventions continue to grow. However, it remains unclear which treatment option is most effective and how each compares with conventional treatments routinely prescribed in clinical practice. The aim of the present study, therefore, was to compare the effectiveness of regular physical exercise and ICBT to standard treatments for mild to moderate depression in a population of Swedish adults. The primary outcome of interest was self-rated depression. As mood disorders frequently have an impact on work performance, a secondary aim was to assess change in self-rated work capacity. In this paper, we present results from assessments taken at baseline (pre-treatment) and 3 months (post-treatment). The study is registered with the registry of clinical trials in Stockholm county (KCTR study ID: KT20110063).
Method
Study design
We conducted a RCT to assess the short-term effectiveness of three treatments for depression. As our primary focus was on the relative effectiveness of exercise and ICBT compared with treatment as usual (TAU), the latter group was considered a control equivalent. Each intervention lasted 12 weeks with assessments of depression and self-rated work capacity taken at baseline (pre-treatment) and post-treatment, 3 months later. The participants represent a cross-section of patients currently treated for depression in clinical practice because in addition to the three 12-week interventions, one-third of all patients were taking antidepressants (primarily selective serotonin reuptake inhibitors (SSRIs)) prior to and during the trial. An ethics committee at the Karolinska Institute approved the study (Dnr 2010/1779-31/4).
Patient recruitment
Patients were recruited via primary care facilities located in six county councils in Sweden (Stockholm, Skåne, Västra Götaland, Kronoberg, Blekinge and Västmanland). The selection of regions was deliberate and helped ensure that the sample included participants from different regions varying in population size and composition. Patients aged 18 years and over who scored >9 on the Patient Health Questionnaire (PHQ-9) Reference Kroenke, Spitzer and Williams15 were invited to participate in the trial. Recruitment began in February 2011 and the last participants ended their treatment in March 2013. Exclusion criteria were: age (<18 years), severe somatic illness, a primary alcohol or drug use disorder, or a psychiatric diagnosis that required specialist treatment (such as psychosis). Following an initial consultation with their primary healthcare provider, suitable patients were referred to a research nurse who administered the baseline questionnaires and confirmed eligibility by conducting a thorough patient interview that included a psychiatric diagnostic assessment using standardised tools (described below). Before the study began, the research nurses were trained by a psychiatrist to interview patients and administer the questionnaires in a consistent manner. After obtaining informed consent, patients were randomised to one of the three treatment conditions by an independent clinical research organisation; the Karolinska Trial Alliance, where individual patients were treated as the ‘unit’ of randomisation. The blocks were unknown to the researchers, and a computer generated the group allocation. This procedure ensured that researchers responsible for the baseline and post-treatment assessments were masked to the patient's group allocation. Data on the number of patients who were invited to participate in the study but declined is unknown. It was not feasible for the primary care centres involved in the study to collect these data. In total, 946 patients met the inclusion criteria for the trial, agreed to participate and were included in the baseline analyses.
Participant characteristics
Baseline characteristics of the study sample are shown in Table 1. Most of the participants were women (73%) with a mean age of 43 years (s.d. 12, range 18–71) and 78% of the sample was employed or studying at baseline. Unemployment rates at baseline among men and women were 27% and 20%, respectively, approximately three times higher than the national average for 2011. 16 Based on the Mini-International Neuropsychiatric Interview (MINI), Reference Sheehan, Lecrubier, Sheehan, Amorim, Janavs and Weiller17 concurrent depressive and anxiety disorders were most common (67%), however, some participants, exclusively, had either depression (8%) or an anxiety disorder (20%). Table 1 shows the primary diagnoses of all participants, based on the MINI assessment. A total of 68% of participants reported moderate to severe physical pain and believed that their daily activities were adversely affected by their health condition. Daily tobacco use was high (28% of men, 18% of women) and the proportion of hazardous alcohol users exceeded the national average. Reference Kallmen, Wennberg, Leifman, Bergman and Berman18 As noted, one-third of all participants in the trial were taking antidepressants during the 12-week intervention. The percentage within each group at baseline was: 31% in the physical exercise and ICBT groups, respectively, and 24% in the TAU group. The proportions were not significantly different (P>0.07). The use of other medications (such as contraceptives, statins, thyroid drugs) during the trial was minimal.
TABLE 1 Primary diagnosis and baseline characteristics of the study sample (%)
| Participant characteristic | Men (n = 257) |
Women (n = 689) |
|---|---|---|
| Gender | 27 | 73 |
| Age, years | ||
| 18–34 | 30 | 30 |
| 35–49 | 37 | 36 |
| 50–71 | 33 | 33 |
| Born in Sweden | 76 | 81 |
| Main diagnosis (MINI) | ||
| Depression and anxiety | 65 | 68 |
| Depression only | 10 | 8 |
| Anxiety only | 20 | 20 |
| Subthreshold affective disorder | 5 | 4 |
| Education | ||
| Primary school | 5 | 3 |
| Technical school | 16 | 11 |
| Secondary school (year 12) | 27 | 23 |
| Post-secondary 2 years | 18 | 19 |
| Tertiary | 35 | 44 |
| Work status: employed or studying | 73 | 80 |
| Health status | ||
| Daily activities affected | 37 | 41 |
| Moderate or severe pain | 66 | 69 |
| Highly worried | 44 | 37 |
| Sick leave | ||
| 8–30 days | 22 | 31 |
| 1–12 months | 19 | 17 |
| Alcohol use | ||
| Hazardous drinker | 29 | 11 |
| Regular binge drinker | 23 | 9 |
| Daily tobacco user | 28 | 18 |
MINI, Mini-International Neuropsychiatric Interview.
Post-treatment assessment
All patients were contacted 3 months after commencing treatment by a research nurse (masked to group allocation) to arrange a post-treatment interview. In total 69% of the interviews were conducted at the patient's health clinic; 31% of the interviews were made by telephone. A short version of the baseline questionnaire was completed at follow-up (the MINI and AUDIT Reference Saunders, Aasland, Babor, de la Fuente and Grant19 were not included), along with a brief exit survey to assess patient satisfaction with the trial. Patients who did not complete a post-treatment questionnaire were contacted by telephone on two separate occasions with a reminder. Those who did not respond to the second reminder were offered the possibility to complete the survey online (n = 17) or a short version of the survey by telephone (n = 38). The flow of patients through the trial is summarised in Fig. 1.

Fig. 1 Flow chart of participants' progress.
PHQ-9, Patient Health Questionnaire; MINI, Mini-International Neuropsychiatric Interview; MADRS, Montgomery–Åsberg Depression Rating Scale; WAI, Work Ability Index; AUDIT, Alcohol Use Disorders Identification Test; ICBT, internet-based cognitive–behavioural therapy; TAU, treatment as usual.
Measures
Screening
We used the PHQ-9 and the MINI. The PHQ-9 assesses the presence of nine key criteria for depression during the past 2 weeks (such as pleasure doing things, feeling down, difficulty sleeping). Reference Kroenke, Spitzer and Williams15 Patients rate the frequency of each symptom on a scale between 0 (not at all) to 3 (nearly every day). Total scores range from 0 to 27. The PHQ-9 is a valid instrument for diagnosing depressive disorders and scores above 9 have a reported sensitivity and specificity of 88% for major depression. Reference Kroenke, Spitzer and Williams15 The MINI Reference Sheehan, Lecrubier, Sheehan, Amorim, Janavs and Weiller17 is a short, structured clinical interview used to diagnose psychiatric disorders based on the DSM-IV. 20 The MINI was used primarily as a screening instrument to exclude patients who did not meet the study inclusion criteria but also to diagnose concomitant anxiety disorders. The complete MINI was performed.
Baseline assessment
The baseline assessment included the following. The EQ-5D was used to assess patient's overall health status. Reference Rabin and de Charro21 We report three key dimensions from the scale: main life activities, pain/discomfort and anxiety/depression. Each dimension is scored on a three-item scale indicating no problems, some problems or extreme problems. The Alcohol Use Disorders Identification Test (AUDIT) was used to assess the proportion of hazardous alcohol users and binge drinkers in the study. Reference Saunders, Aasland, Babor, de la Fuente and Grant19 We used the recommended cut-off scores of 8 for men and 6 for women to define hazardous drinking. Reference Bergman and Kallmen22 Binge drinking refers to the consumption of six or more standard drinks (or about 12 g of alcohol) on a single occasion. Participants who indicated binge drinking ‘every month’, ‘every week’ or ‘daily’, were coded as ‘regular binge drinkers’. Those indicating ‘never’ or ‘less than once per month’ were excluded from this definition. Tobacco use was assessed with a single question: ‘Do you smoke or use ‘snus’ daily?’ with two response alternatives, yes or no (snus is a smokeless tobacco product). A questionnaire was developed by the research group to record the type of antidepressant medication used during the past 2 weeks. It was completed by a research nurse at baseline (pre-treatment) and 3 months (post-treatment).
Primary and secondary outcomes
The primary outcome was the severity of depression, assessed using the Montgomery–Åsberg Depression Rating Scale (MADRS); Reference Montgomery and Åsberg23 a 10-item scale designed to be sensitive to changes in depressive symptoms following treatment. Higher scores indicate more severe depression; each item yields a score ranging from 0 to 6. Ten symptoms are rated: apparent sadness, reported sadness, inner tension, reduced sleep, reduced appetite, concentration difficulties, lassitude, inability to feel, pessimistic and suicidal thoughts. Total scores range between 0 and 60.
Our secondary outcome was self-rated work capacity. This was scored on a single 10-item Likert scale ranging from 0 (unable to work) to 10 (highest possible work capacity). The item was derived from the Work Ability Index (WAI) and is strongly correlated with the complete 24-item WAI (r = 0.87). Reference Ahlstrom, Grimby-Ekman, Hagberg and Dellve24
Interventions
Physical exercise
Patients in the physical exercise group were randomised to one of three conditions: ‘light exercise’, which consisted of yoga classes (or similar) with a focus on gentle stretching and controlled breathing; ‘moderate exercise’, an intermediate-level aerobics class; and ‘vigorous exercise’, a higher intensity aerobics/strength-training and balance class. All exercise sessions were 60 min duration and most included between 5 and 20 participants. Patients were requested to participate in the exercise classes three times per week for 12 weeks. The exercise sessions were undertaken at ‘Friskis och Svettis’ a modern fitness centre with multiple locations throughout Sweden. As an incentive to increase adherence, all patients were provided with free gym memberships for 12 weeks. Adherence was monitored through weekly face-to-face meetings with a qualified personal trainer and patients who failed to attend this meeting were contacted by the trainer with a telephone call and encouraged to continue the exercise intervention. Reminder text messages were sent to patients who could not initially be contacted by telephone. Patients completed on average one exercise session per week; that is, 12 out of the recommended 36 sessions – an adherence rate of 33%. There were no gender differences in exercise participation rates. As our main interest was the overall effect of the physical exercise intervention on depression data from the three intensity groups were analysed together. A forthcoming paper will report the effects of exercise intensity on treatment outcomes.
ICBT
Patients randomised to the ICBT condition received treatment through a secure website operated via the county council. Treatment involved the patient working through a self-help manual available online in the form of modules. The manual was mostly text based, but also included images and sound clips. Before commencing the treatment, all ICBT participants received a short telephone call from their assigned clinician (a psychologist) who explained the process. Initially, several online forms were completed to identify patient-specific mental health concerns and work-related problems. The basic modules completed during the first few weeks address problems related to depressive symptoms in general, such as inactivity and avoidance behaviours. Subsequent modules were patient specific and targeted different comorbid symptoms often seen in depression, such as worry, panic attacks, social anxiety, stress, insomnia and pain. Other patient-specific modules focused on problems related to the workplace and motivated the patient to return to work or find a new job. Throughout treatment, patient responses were monitored by the assigned clinician on a weekly basis so that high-risk individuals could receive additional help if necessary. Patients who did not use the service for 1 week or more were prompted by their clinician to continue the treatment (unless they had chosen to withdraw). Patients were able to contact a clinician directly or request additional support if needed. As with the physical exercise intervention, ICBT was offered free of charge. During the 3-month trial, patients logged into the website on average four times per week, sent 18 messages to their assigned therapist, received 17 messages and accessed 7.8 (s.d. = 5) online modules out of an expected 13 (an adherence rate of 60%). The average frequency of ICBT usage was higher among women across all measures (for example, women accessed the service 52 times over 12 weeks, compared with 40 times among men).
TAU
One-third of the participants received standard treatment for depression administered by their primary care physician who was responsible for determining the type of treatment. In many cases, this consisted of counselling with a CBT focus conducted for about 1 h. Patients attended on average 8.2 (s.d. = 6.4) face-to-face counselling sessions during the 12 week trial. A total of 25% of patients in this group received no recorded treatment.
Statistical analyses
Descriptive statistics (percentages) were calculated to describe participant characteristics at baseline, stratified by gender. Paired sample t-tests with Bonferroni corrections for multiple comparisons assessed within-group changes in depression and work capacity from baseline to 3-month follow-up. The overall effectiveness of the three interventions was assessed using analysis of covariance (ANCOVA) with baseline depression and work capacity scores entered as covariance factors in each model. This was considered necessary to control for the intercorrelation between baseline and follow-up scores that results when the same individuals complete a questionnaire twice. The strength of the intervention effect was assessed using the partial Eta-squared statistic (represented by the symbol η2). Partial η2 is the variance explained by a given variable after excluding the variance explained by other predictors. Effect sizes were interpreted using the following criteria: 0.01, small; 0.06, medium; and 0.14 or higher, a large effect size. Reference Richardson25 Pairwise comparisons (independent sample t-tests) determined which group differences were statistically significant at 3 months post-treatment. Mean differences between groups with 95% confidence intervals are reported. For comparison purposes, a multilevel model was also performed, where the individual and time (baseline to 3 months) were the units of analysis. Possible age effects were examined by stratifying the data as follows: 18–34 years (n = 283, 30%), 35–49 years (n = 346, 36.7%) and 50–71 years (n = 314, 33.3%). Two patients had no recorded age. All analyses were performed using SPSS version 20.0.
Results
Primary outcome
Table 2 shows the change in mean depression (MADRS) scores at baseline and 3-month follow-up stratified by gender. Figure 2 illustrates these changes over time. Level of depression reduced significantly from baseline to post-treatment in all three treatment groups. There was a main effect of group with a small effect size, indicating that the improvements in depression at 3 months were significantly larger in both the physical exercise group (mean difference 2.99, 95% CI 1.61–4.37, P<0.001) and the ICBT group (mean difference 2.83, 95% CI 1.47–4.19, P<0.001), respectively. The treatment effect of exercise and ICBT was approximately equal. The main effect of gender fell slightly below statistical significance (F(1,715) = 3.43, P = 0.06). When the data were stratified by age, results were comparable with the overall analysis (that is, favouring exercise and ICBT), with one partial exception. Among younger participants aged 18–34 years, the mean differences between treatment groups were not statistically significant (F(2,207) = 0.90, P = 0.40). Mean depression scores at post-treatment in this age group were 10.4 (exercise group), 10.4 (ICBT group) and 11.1 (TAU group). Post-treatment group differences were statistically significant among adults aged 35–49 years (F(2,254) = 6.58, P<0.01) and 50–71 years (F(2,241) = 5.17, P<0.01). Multilevel modelling produced comparable outcomes with the ANCOVA analyses. A subgroup analysis was conducted to exclude patients taking antidepressants at baseline. The results indicated outcomes equivalent to the total sample analyses (data not shown).
TABLE 2 Within- and between-group treatment effects on depression (Montgomery–Åsberg Depression Rating Scale)Footnote a
| Mean, s.d. | Within-group change, t (d.f.) |
Main effect of treatment group, ANCOVA | Effect size, partial η2 |
|||
|---|---|---|---|---|---|---|
| Group | Baseline | 3 Months | F (d.f.) | P | ||
| All participants | 11.5 (2,714) | <0.001 | 0.031 | |||
| Treatment as usual | 20.9 (7.5) | 13.8 (8.9) | 12.6 (226)Footnote * | |||
| Physical exercise | 22.2 (6.8) | 11.3 (7.9) | 18.8 (238)Footnote * | |||
| Internet-based cognitive–behavioural therapy | 21.5 (6.7) | 11.2 (7.3) | 19.2 (251)Footnote * | |||
| Men | 9.2 (2,191) | <0.001 | 0.088 | |||
| Treatment as usual | 21.5 (8.1) | 16.9 (10.6) | 4.1 (49)Footnote * | |||
| Physical exercise | 21.9 (6.7) | 10.8 (8.2) | 10.3 (75)Footnote * | |||
| Internet-based cognitive–behavioural therapy | 22.2 (5.4) | 12.7 (8.1) | 9.3 (68)Footnote * | |||
| Women | 5.6 (2,519) | <0.01 | 0.021 | |||
| Treatment as usual | 20.7 (7.3) | 12.9 (8.2) | 12.2 (176)Footnote * | |||
| Physical exercise | 22.4 (6.9) | 11.6 (7.7) | 15.6 (162)Footnote * | |||
| Internet-based cognitive–behavioural therapy | 21.3 (7.1) | 10.6 (6.9) | 16.8 (182)Footnote * | |||
a. Lower scores indicate less depressive symptomatology.
* Significant at P<0.001 (adjusted using Bonferroni correction).
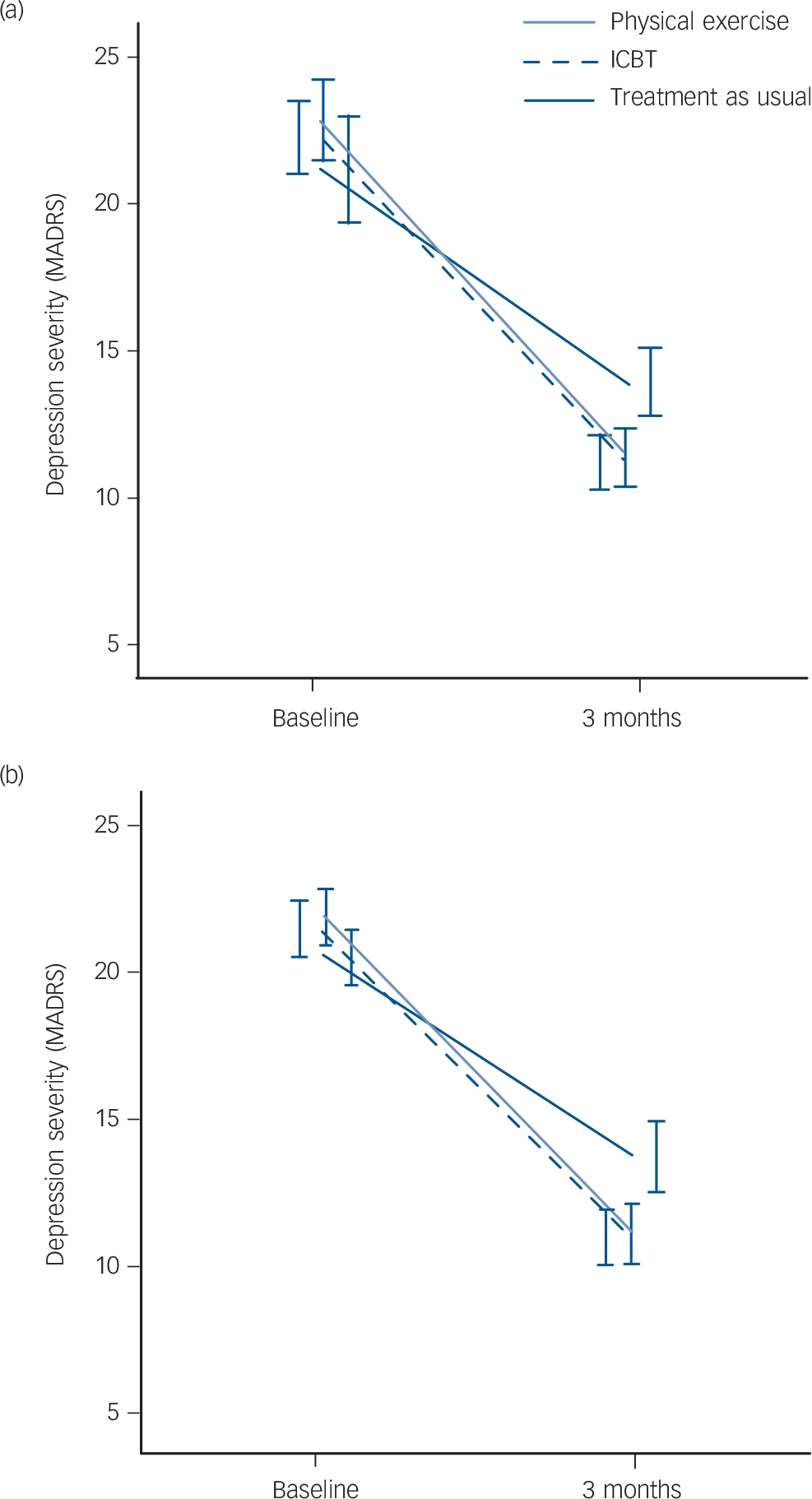
Fig. 2 Change over time in depression severity in (a) men and (b) women.
ICBT, internet-based cognitive–behavioural therapy; MADRS, Montgomery–Åsberg Depression Rating Scale.
Secondary outcome
Table 3 shows the change over time in self-rated work capacity scored on a single item scale ranging from 0 (no capacity) to 10 (highest possible capacity). Within-group improvements were found in all three treatments, but there were no differences between the three groups at 3 months. A gender difference was found, with men rating greater improvements in work capacity over time compared with women, but the effect size was small.
TABLE 3 Within- and between-group treatment effects on work capacityFootnote a
| Mean, s.d. | Within-group change, t (d.f.) |
Main effect of treatment group, ANCOVA | Effect size, partial η2 |
|||
|---|---|---|---|---|---|---|
| Baseline | 3 Months | F (d.f.) | P | |||
| Treatment group | 0.93 (2,639) | 0.39 | 0.003 | |||
| Treatment as usual | 5.68 (2.5) | 6.64 (2.6) | 5.28 (201)Footnote * | |||
| Physical exercise | 5.58 (2.4) | 6.69 (2.6) | 6.34 (209)Footnote * | |||
| Internet-based cognitive–behavioural therapy | 5.52 (2.5) | 6.84 (2.4) | 8.16 (230)Footnote * | |||
| Gender | 6.0 (1,640) | <0.05 | 0.009 | |||
| Men | 5.67 (2.4) | 6.43 (2.6) | 4.16 (183)Footnote * | |||
| Women | 5.56 (2.5) | 6.85 (2.5) | 10.92 (485)Footnote * | |||
a. Higher scores indicate greater work capacity.
* Significant at P<0.001 (adjusted using Bonferroni correction).
Response rates
Of the 946 patients who completed a baseline assessment, 740 (78.2%) participated in a post-treatment depression assessment. A smaller proportion of patients completed the work capacity survey (67.6%). A drop-out analysis revealed no differences in response rates based on age, gender, depression status, work capacity or alcohol use at baseline. However, more people who dropped out were not working at baseline (30%) compared with those who were employed (23%, P<0.03) and were patients assigned to TAU (14%) compared with ICBT (9%, P<0.01) or physical exercise (12%, P<0.02). The follow-up survey revealed that the majority of those who dropped out did so because of dissatisfaction with the randomisation outcome. Despite understanding that participation in the trial entailed a randomisation process, some patients were evidently disappointed when they did not receive their preferred treatment. A minority of patients withdrew because they felt the treatment regime was impractical and interfered with other activities. One patient relocated abroad and another could not be located.
Missing items on key variables ranged between 1% and 7% with one exception; 23% of items from the MADRS Question 2 (apparent sadness) were missing at follow-up. This occurred because Question 2 is based on an observational rating and about one-third of the MADRS follow-up interviews were conducted by telephone; consequently the question could not be rated. Otherwise, there were no discernible patterns associated with the missing data. As the first two items of the MADRS are highly correlated (r = 0.81) and logically related to each other, we used the last number carried forward (LNCF) method to impute these missing values. Separate analyses of the non-imputed MADRS data indicated almost identical results.
Discussion
Key findings and interpretation
In this study, all three interventions were associated with improvements in depressive symptoms at follow-up. However, the mean reduction in depression scores were significantly larger in the physical exercise and ICBT groups compared with TAU; an effect seen among both men and women. The overall treatment effect of exercise and ICBT was approximately equal. An age effect was observed; adults over 34 years responded more favourably to the exercise and ICBT interventions compared with TAU. A similar trend was found among younger adults (18–34 years), but the group differences were not significant at post-treatment. Work capacity improved over time but there were no group differences.
The clinical relevance of the observed improvements in depression are important to consider. Reference Montgomery and Åsberg23 Snaith et al Reference Snaith, Harrop, Newby and Teale26 propose a cut-off score of 20 points for moderate depression (with 7–19 points for mild severity). Mean MADRS scores at baseline ranged between 20.7 and 22.4 points, indicating that most participants were experiencing a ‘moderate’ depression at the initial assessment. At post-treatment (3 months), mean MADRS scores were reduced significantly in all three treatment groups to a level corresponding with ‘mild’ depression severity. Also relevant, is that among men randomised to TAU, the MADRS score (16.9) remained within the moderate category at follow-up, suggesting that men were less responsive than women to the interventions offered in usual care. In sum, the improvements seen in all three treatment groups were clinically meaningful, but patients in the exercise and ICBT groups improved significantly more than patients receiving TAU.
In addition to negative mood states, depression is associated with numerous functional impairments. Recently, there have been calls to include functional outcomes in studies investigating treatment effects on depression. Reference Greer, Kurian and Trivedi27 Perceived work capacity was assessed before and after treatment because it is an important indicator of a person's ability and willingness to work; a key functional outcome in this context. Self-rated work capacity improved equally in all three treatment groups at follow-up.
Our findings are broadly consistent with recent reviews supporting the mood-enhancing benefits of exercise on depression. A Cochrane review of 35 RCTs (1356 participants) comparing exercise with no treatment or a control intervention reported a pooled standardised mean difference of −0.62 (95% CI −0.81 to −0.42), indicating a moderate clinical effect of exercise. Reference Cooney, Dwan, Greig, Lawlor, Rimer and Waugh28 When compared with psychological or pharmacological treatment (12 studies), exercise was found to be equally but not more effective than usual care. Results from our investigation are also comparable with several controlled studies. In a multicenter trial involving 2322 patients treated for heart failure with a mild to moderate depression, Blumenthal et al Reference Blumenthal, Babyak, O'Connor, Keteyian, Landzberg and Howlett29 randomised participants to either 12 months of supervised/home-based aerobic exercise, or usual care for heart failure (with no planned exercise). Compared with usual care, aerobic exercise resulted in a modest but statistically significant reduction in mean depression scores at both 3- and 12-month follow-up. In an often cited study, Dunn et al explored dose–response relationships to exercise in 80 adults aged 20–45 years with mild to moderate depression. Reference Dunn, Trivedi, Kampert, Clark and Chambliss30 Participants were randomised to one of four supervised exercise treatment groups lasting 12 weeks, or a control condition. Of importance, the study showed that exercise by itself is effective in the treatment of depression, and that the amount of exercise needed is equivalent to consensus public health recommendations.
There is sound neurobiological and clinical trial evidence supporting the mental health benefits of exercise, yet some studies have failed to observe positive effects. In one of the largest trials of physical activity and depression conducted in primary care, Chalder et al randomised 351 adults aged 18–69 to either usual care plus a supported exercise intervention lasting 8 months, or to usual care alone. Reference Chalder, Wiles, Campbell, Hollinghurst, Haase and Taylor31 At 4-month follow-up (the primary outcome end-point) no differences in depression were observed between the physical activity and usual care groups. Moreover, there was no evidence of an intervention effect on mood at 8 and 12 months. There are notable similarities between the Chalder et al study and the present investigation; both were conducted in primary care settings and included a large number of adults voluntarily seeking treatment for depressive symptoms. However, there are also key differences that may explain the disparate results. In the present study, the aim was to supervise patients through a structured 12-week physical exercise regime. All exercise sessions were delivered in a standardised group setting for the duration of the trial. Adherence was encouraged and monitored through weekly contact with the patient's assigned trainer; a person known to the participants. In the Chalder et al study, the goal was to support an overall increase in physical activity. Participants were encouraged to engage in a range of physical exercises, but they were not supervised through a structured exercise programme. These key differences are relevant because recent research suggest that supervision of aerobic activity is a key predictor of successful treatment outcomes in depression trials. Reference Stanton and Reaburn32 Thus, it is possible that the higher level of support and monitoring offered to our patients encouraged more frequent exercise participation and, in turn, greater improvements in depression outcomes.
The other intervention assessed in this trial was internet-based CBT. A recent but growing body of evidence suggests that internet-based interventions can have beneficial effects on depression and several studies have reported outcomes comparable with those seen here. Reference Cuijpers, van Straten and Andersson10 To assess the effectiveness of ICBT delivered within routine care, Hedman et al conducted a cohort study (n = 1203) at a psychiatric out-patient clinic in Sweden. Reference Hedman, Ljotsson, Kaldo, Hesser, El Alaoui and Kraepelien33 The duration of the trial and the treatment delivery format were similar to the present one. However, treatment in the Hedman et al study focused solely on depression and was not individually tailored to address comorbid symptoms or work-related problems. As in the current trial, participants also had access to an online therapist who supervised progress, monitored suicidality and provided individual feedback on homework exercises (such as for behavioural activation). They found significant improvements in depression, and their effect size was somewhat smaller than in our study. Participants also reported improvements in sleep quality and reduced suicidal ideation; results that were maintained at 6-month follow-up. Recent ICBT studies have examined whether tailored v. standardised internet-based programmes have different effects on depression. In a RCT, Johansson et al found that both individually tailored and standardised ICBT were effective in reducing depressive symptoms and improving quality of life. Reference Johansson, Sjoberg, Sjogren, Johnsson, Carlbring and Andersson34 However, a subgroup analysis revealed that the tailored version was more effective in treating patients with more severe depression. Recent reviews report a strong correlation between the degree of support provided in ICBT trials and better mental health outcomes. Reference Johansson and Andersson35 For this reason, regular monitoring and online support was an integral component of the our ICBT intervention.
Although internet-delivered health interventions offer a number of potential benefits (timely access, reduced health service costs, reaching stigmatised groups, etc), some studies have reported no benefits compared with TAU, Reference Kivi, Eriksson, Hange, Petersson, Vernmark and Johansson36 and others have raised concerns about possible unintended consequences of internet-delivered mental health services. Reference Griffiths, Lindenmeyer, Powell, Lowe and Thorogood37 For example, it may be a poor substitute for face-to-face contact with a clinician in some instances. Providing an intervention via the internet for individuals living with a health problem they feel is stigmatised could also discourage the issue from being discussed beyond the relative anonymity of the internet, thus reinforcing the stigma. The findings presented in this study are promising, however, much of the supporting evidence for ICBT emanates from efficacy trials where the interventions have been delivered under optimal conditions. Studies of treatment effectiveness in ‘real-world’ settings remain scarce.
Strengths and limitations
To our knowledge, this is the largest effectiveness trial of physical exercise and ICBT for depression in primary care. The RCT design and the comparison of three treatment modalities in a single study are strengths of the investigation. The randomisation was performed remotely from where the RCT took place and participants were personally assessed in addition to making self-ratings. Research nurses responsible for follow-up assessments were masked to treatment allocation. The inclusion of patients using medication is both a strength and a weakness; it makes the intervention less ‘pure’ but increases the external validity of the findings.
Several limitations are acknowledged. Patients in the TAU group received on average 8.2 face-to-face counselling sessions with their primary care physician, which was a lower average frequency of treatment compared with the exercise and ICBT interventions. Consequently, we cannot exclude the possibility that the favourable outcomes associated with these interventions were at least partly attributable to more frequent engagement in treatment. Importantly however, usual care in this study was not a control group equivalent; most patients were actively engaged in treatment. As in previous studies, our main focus has been on the resolution of depressive symptoms. Although this is clearly important, from a clinical perspective, it could be argued that quality of life is a more appropriate measure of functional improvement following depression treatment. Other measures, such as psychosocial functioning are also important to consider. The single item used to assess work capacity may have been inadequate; factors such as absenteeism (days off work) and level of productivity while at work are relevant indicators of work ability that were not assessed here. Another study limitation is that we do not know how many patients were invited to participate in the trial but declined. It was not feasible for the primary care centres involved in the study, nor the researchers, to collect these data. Finally, we acknowledge that adherence to the physical exercise and ICBT interventions was suboptimal, despite ongoing monitoring, which may have lowered the potential treatment effects of these interventions.
Clinical implications and future research
Prescribed physical exercise at a frequency of at least once per week and therapist supported, individually tailored ICBT are more effective short-term treatments for mild to moderate depression than general clinical management in primary healthcare. Despite strong evidence supporting the use of exercise to treat mental health problems, and the availability of guidelines for exercise prescription, Reference Sundberg, Jansson, Edling and Wadman38,Reference Rethorst and Trivedi39 physical activity is rarely used as a treatment for depression in Sweden. According to data published in 2012, only 1 out of 1000 visits to primary care physicians resulted in the prescription of exercise. Reference Kallings40 The evidence supporting exercise for better mental health is substantial. We propose that physical activity should be more widely prescribed for depression in primary care settings. To date, over 1200 patients have received ICBT for depression through regular healthcare in Stockholm county. Reference Hedman, Ljotsson, Kaldo, Hesser, El Alaoui and Kraepelien33 This mode of treatment is increasing in other parts of Sweden. Our results are consistent with several studies demonstrating positive effects of supported internet treatments for depression. Future investigations of dose–response are needed for both physical exercise and ICBT interventions. Age and gender effects should be examined closely, and greater attention should be given to assessing the unintended consequences of internet-based treatments for depression.
Funding
The Regassa project has been financed by the Stockholm County Council, Sweden. M.H. is currently funded by a post-doctoral stipend from the Brain Foundation, Sweden.








eLetters
No eLetters have been published for this article.