Atrioventricular septal defects represent up to 5% of CHDs with an estimated occurrence of 0.19 in 1,000 live births. Reference Anderson, Ho, Falcao, Daliento and Rigby1–Reference Samanek4 Approximately 40 to 45% of children with Down syndrome) have CHD, and 45% of those have atrioventricular septal defect. Conversely, up to 50% of patients with atrioventricular septal defect have Down syndrome. 5
Previous studies have shown clinically relevant differences between atrioventricular septal defect patients with and without Down syndrome. Patients with Down syndrome most often have the complete form of atrioventricular septal defect. 5 Down syndrome patients with atrioventricular septal defect are more likely to have an earlier presentation and worsening evolution of the pulmonary vascular disease and respiratory complications compared to non-Down syndrome Patients. 5–Reference Yamaki, Yasui and Kado7 However, controversy exists about the impact of Down syndrome on the perioperative outcomes of atrioventricular septal defect patients. Studies have shown that Down syndrome is considered a risk factor for perioperative mortality and is associated with unfavourable outcomes. Reference Yamaki, Yasui and Kado7–Reference Reller and Morris9 In contrast, other reports demonstrated that the presence of Down syndrome is not a risk factor for adverse outcomes after surgical repair of atrioventricular septal defect. Reference Lange, Guenther, Busch, Hess and Schreiber10–Reference St Louis, Jodhka and Jacobs13
Therefore, in the current study, we aimed to use the National Inpatient Sample database to (a) Examine the trends of atrioventricular septal defect hospitalisation during the study period, (b) Determine the risk factors associated with perioperative mortality after complete surgical repair of atrioventricular septal defect in the first year of life, and (c) Evaluate the impact of Down syndrome on the outcomes after atrioventricular septal defect repair including cardiac (specifically pulmonary hypertension and arrhythmias), non-cardiac co-morbidities, procedures, length of hospitalisation, and resources utilisation.
Methods
Data source
This is a retrospective observational study using deidentified patient data from the National Inpatient Sample database during the period from 2000 to 2018. The National Inpatient Sample database is part of the Healthcare Cost and Utilization Project, which is collected by the Agency for Healthcare Research and Quality. The National Inpatient Sample database contains approximately 8 million hospital stays each year and randomly samples 20% of the discharges from the participating hospitals. 14 The collection of data is stratified to ensure equal representation of hospitals by geographic region, urban and rural location, teaching status, and hospital bed size. Procedure and diagnostic codes are recorded using the International Classification of Diseases. The International Classification of Disease, Ninth and Tenth Revisions, Clinical Modification were used to identify our patient population. The International Classification of Disease, Ninth Revision was used from January 2000 to September 2015 while the International Classification of Disease, Tenth Revision was used from October 2015 to December 2018.
Patient selection
The study was granted an exempt status from the Institutional Review Board given the use of a deidentified and publicly available database. Patients were included in the study if they were less than one year of age, had the diagnosis of atrioventricular septal defect (International Classification of Disease, Ninth and Tenth Revisions 745.60, 745.69, and Q21.2 and Q21.23, respectively), and had undergone complete surgical repair during the index hospitalisation. Patients were excluded from the study if there were > 1 year of age, had no surgical repair, and/or had any genetic diagnosis other than Down syndrome.
Identification of variables
The National Inpatient Sample database was queried for patients’ demographics and clinical characteristics. Demographic data included age, sex, race, primary payer, type of hospital (teaching versus non-teaching, urban versus rural), hospital bed size, and the region of the hospital. The main outcomes of interest included cardiac and non-cardiac co-morbidities, death prior to hospital discharge, length of hospital stay, and hospital charges. The total hospital charges were reported in United States of America dollars. The following ICD codes (758.0, Q90.0, Q90.1, Q90.2, and Q90.9) were used to identify patients with Down syndrome. Patients were divided into two groups: atrioventricular septal defect with versus without Down syndrome. Differences in demographics and clinical characteristics were examined between the two groups including cardiac morbidities (cyanosis, heart failure, pulmonary hypertension, arrhythmia, heart block, and cardiac arrest), respiratory, gastrointestinal, renal co-morbidities, and procedures (mechanical ventilation, extracorporeal membrane oxygenation support, tracheostomy, gastrostomy, and pacemaker implantation).
Statistical analysis
Data were analysed as appropriate, using mean and standard deviation for parametric continuous variables, median and interquartile range for nonparametric continuous variables, and frequencies (percentages) and proportions for categorical variables. We compared the survivors and non-survivors using appropriate statistical analysis; the Mann–Whitney U-test for continuous characteristics and chi-squared or Fisher’s exact tests for categorical characteristics. Trends in atrioventricular septal defect admissions and mortality over the study period years were assessed for significance using the Jonckheere–Terpstra test. We used a logistic regression model to examine the factors associated with mortality after atrioventricular septal defect surgical repair. SPSS 25 (SPSS Inc., Chicago, IL) was used for statistical analysis.
In accordance with the Healthcare Cost and Utilization Project data use agreement, cells with values of 1–10 are not published. P < 0.05 was considered significant. Data can be weighted such that the results can be extrapolated as representative of the entire inpatient population. Data weighting was developed essentially to obtain trend analysis; however, it can also be utilised for all analyses per the Agency for Healthcare Research and Quality Healthcare Cost and Utilization Project. Unweighted counts were used for all statistical analyses except trend assessments, where nationally weighted estimates were used.
Results
During the study period, 86,234,583 infants’ records were reviewed from 2000 to 2018. Out of 2,318,706 admissions with CHD diagnosis in the first year of life, 61,101 (2.6%) had atrioventricular septal defect. The incidence of hospitalisations in infants with atrioventricular septal defect ranged from 4.5–7.4/year during the study period. There was a predominance of the female sex in patients with atrioventricular septal defect (53.3 versus 46.7%, p < 0.001). The white race was pre-dominant (43%) followed by Hispanic (17%), p < 0.001. Medicaid was the primary payer insurance in (47.6%) versus private insurance in (45.8%) p < 0.001. Seasonal variations in patients’ discharges existed throughout the year (Table 1).
Table 1. Demographics and characteristics of all atrioventricular septal defect patients (n = 61,101).
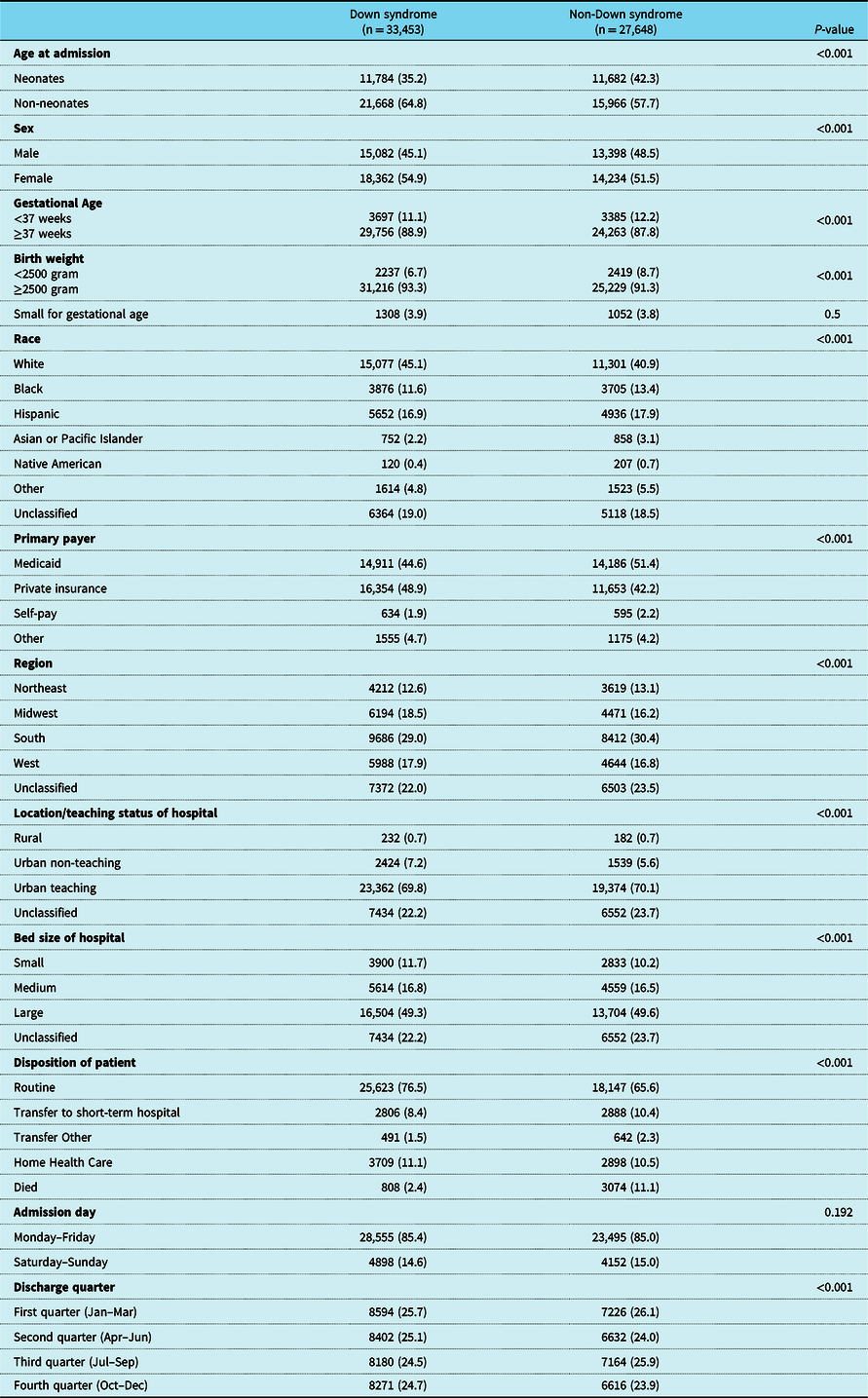
Data are expressed in frequency (%); chi-square or Fisher’s exact tests were used for analysis.
Atrioventricular septal defect with versus without Down syndrome
The diagnosis of Down syndrome was present in 33,453 (54.7%) patients. Trends in atrioventricular septal defect hospitalisation in patients with versus without Down syndrome during the study period are demonstrated in Figure 1. Down syndrome was associated with the female sex (54.9 versus 45.1%, p < 0.001). The White and Hispanics were the most associated races with Down syndrome. Regional distribution differences existed between patients with and without Down syndrome. Table 1 illustrates the demographics and patients’ characteristics of atrioventricular septal defect patients with versus without Down syndrome.
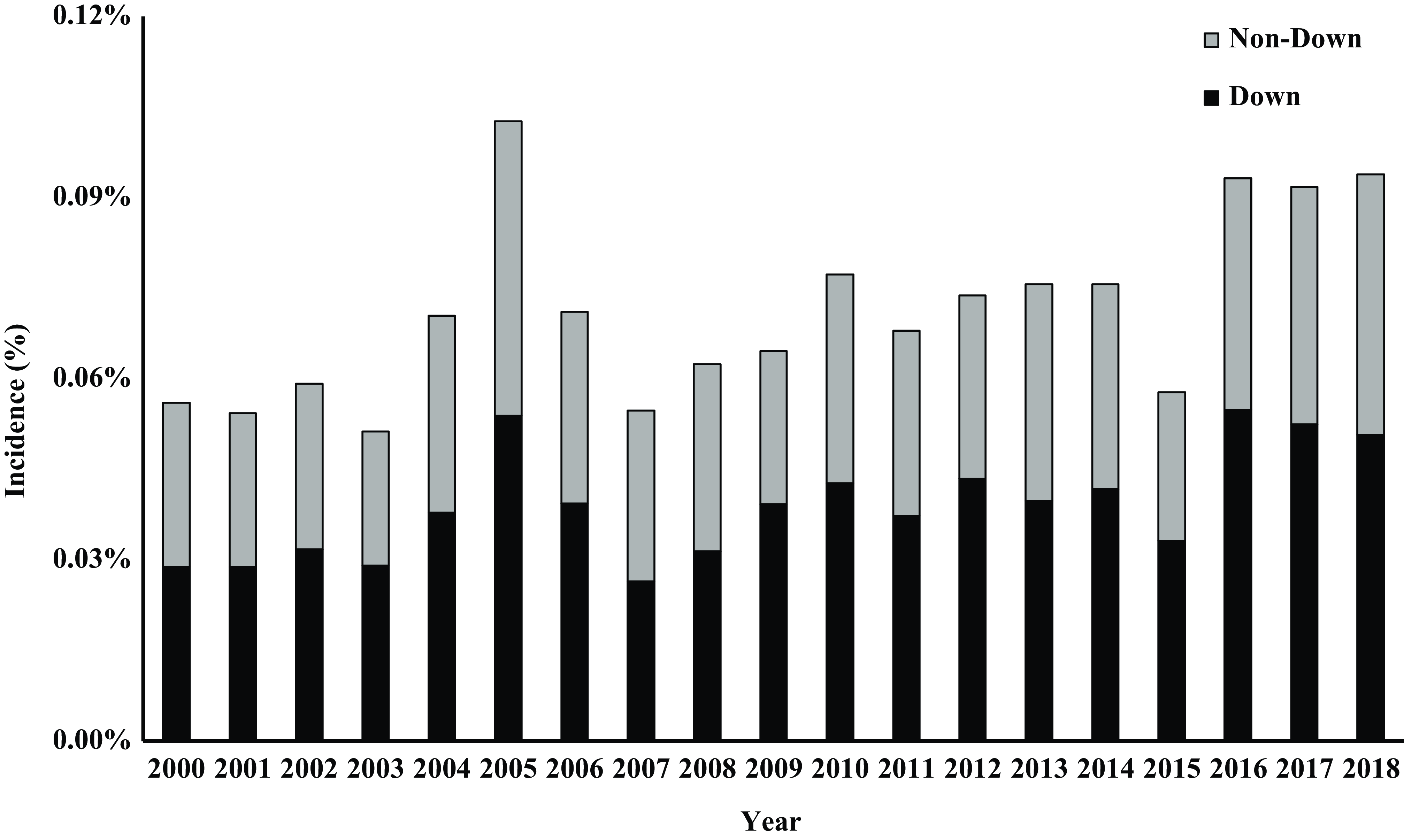
Figure 1. Trends in atrioventricular septal defect hospitalisation during the study period from 2000 to 2018 comparing patients with versus without Down syndrome.
Association with other CHDs
Isolated atrioventricular septal defects and those associated with simple lesions (secundum atrial septal defects, patent ductus arteriosus, and additional ventricular septal defects) were reported in 35,569 (58.2%) patients. Double outlet right ventricle, coarctation of the aorta, tetralogy of Fallot, and pulmonary atresia were the most common CHDs associated with atrioventricular septal defect in 6.9, 5.7, 4.3, and 4.2%, respectively. The association between atrioventricular septal defect and tetralogy of Fallot was more frequent in Down syndrome patients (5 versus 3.4 %, p < 0.001) while the association between atrioventricular septal defect and all other forms of CHDs was more frequent in the non-Down syndrome group (Table 2).
Table 2. Association of atrioventricular septal defect with other CHDs in patients with versus without Down syndrome.
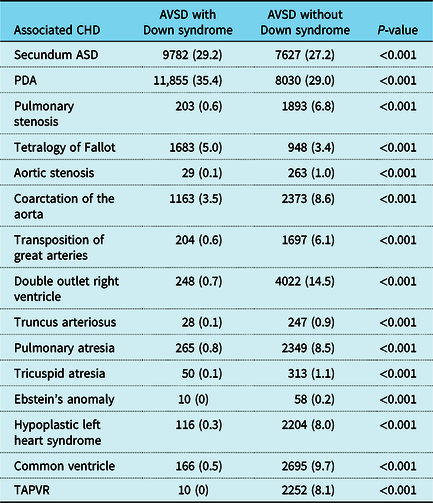
TAPVR = total anomalous pulmonary venous return; PDA = patent ductus arteriosus; ASD = atrial septal defects.
Data are expressed in frequency (%); Chi-square or Fisher’s exact tests were used for analysis.
Cardiac and non-cardiac co-morbidities and intervention
Atrioventricular septal defect patients with Down syndrome developed more frequent heart failure but less cyanosis, and less respiratory failure compared to non-Down syndrome atrioventricular septal defect patients (28.3 versus 22%, 0.6 versus 0.9%, 14.4 versus 16.9%, p = 0.01, < 0.001, and < 0.001, respectively). The development of pulmonary hypertension was more frequent in Down syndrome patients (4.8 versus 2.7%, p < 0.001). Cardiac arrhythmias and cardiac arrest tend to occur more frequently in non-Down syndrome patients [11.2 versus 6.6% OR 0.56 (0.53–0.59), p < 0.001] and [2.8 versus 1.0%, OR 0.37 (0.32–0.41), p < 0.001], respectively Table 3.
Table 3. Clinical outcomes in AVSD patients with versus without Down syndrome during the study period (2000–2018).
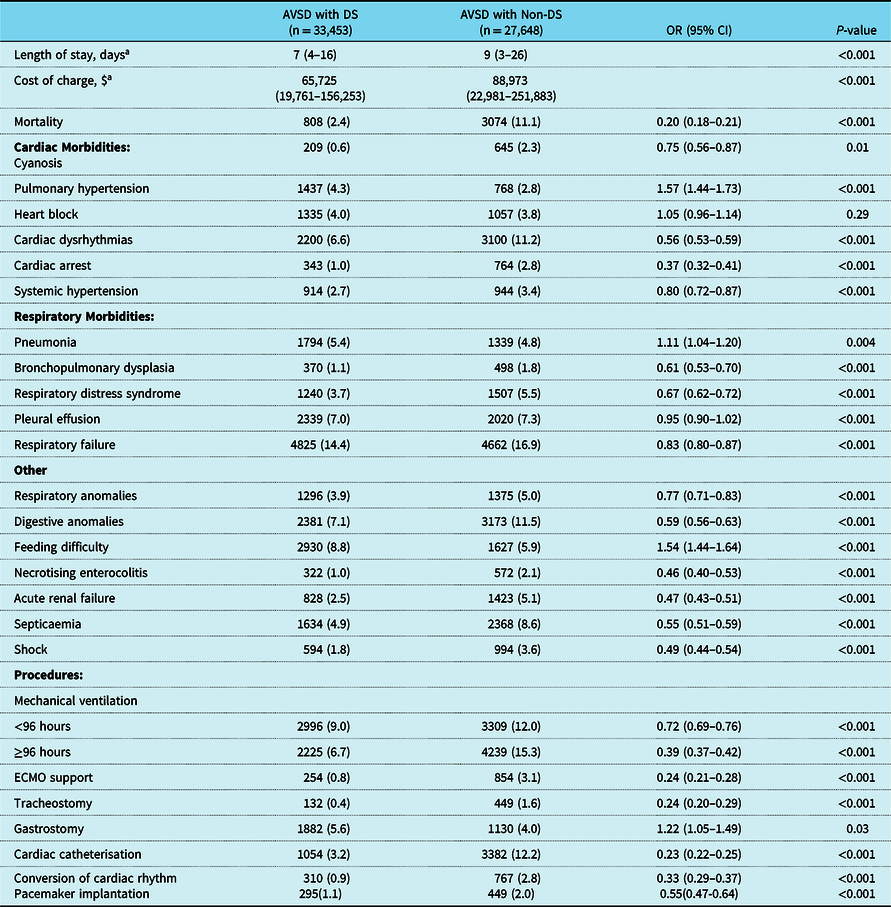
AVSD = atrioventricular septal defects; DS = down syndrome, ECMO = extracorporeal membrane oxygenation.
a that expressed in median (interquartile range); Mann–Whitney U-test was used for analysis.
Data are expressed in frequency (%); chi-square or Fisher’s exact tests were used for analysis except with data.
Atrioventricular septal defect patients with Down syndrome had less incidence of in-hospital non-cardiac complications including sepsis, acute renal failure, and shock (4.9 versus 8.6%, 2.5 versus 5.1%, and 1.8 versus 3.6%, respectively, with p < 0.001 for all). Post-operative pleural effusion was not significantly different in atrioventricular septal defect patients with Down syndrome compared to those without Down syndrome. However, atrioventricular septal defect patients with Down syndrome had a higher frequency of having post-operative chylothorax compared to those without Down syndrome [335 (1%) versus 186 (0.6%), p < 0.001)]. Atrioventricular septal defect patients with Down syndrome had a higher incidence of pneumonia compared to non-Down syndrome patients [5.4 versus 4.8%, CI (95%) 1.11 (1.04–1.20), p = 0.004]. While patients with Down syndrome had a lower incidence of respiratory failure [14.4 versus 16.9% CI (95%) 0.83 (0.80–0.87), P < 0.001] and required a shorter duration of mechanical ventilation compared to the non-Down syndrome group. Similarly, atrioventricular septal defect patients with Down syndrome patients received less tracheostomy, and extracorporeal membrane oxygenation support compared to non-Down syndrome atrioventricular septal defect patients, Table 3.
Feeding difficulties were more frequent in atrioventricular septal defect patients with Down syndrome who underwent more gastrostomy tubes compared to those without Down syndrome (8.8 versus 5.9% and 5.6 versus 3.2%, p < 0.001 and 0.03, respectively).
Mortality
In-hospital mortality of atrioventricular septal defect patients during the study period was reported in 3882 (6.3%) patients. Down syndrome patients with atrioventricular septal defect had significantly less mortality incidence than non-Down syndrome patients (2.4 versus 11.1%, p < 0.001). When excluding patients with severely unbalanced atrioventricular septal defect who underwent SV palliative surgeries, mortality continued to be high in non-Down syndrome patients who underwent biventricular repair compared to patients with Down syndrome (7.6 versus 2.2%, p < 0.001). When excluded any associated CHD other than the simple lesions as secundum atrial septal defects and/or PDA, mortality continued to be high in the isolated atrioventricular septal defect non-Down syndrome patients compared to those with Down syndrome (5.9 versus 1.8%, p = 0.01) Trends in the overall mortality in all atrioventricular septal defect patients with versus without Down syndrome are illustrated in Figure 2.
Figure 2. Trends of in-hospital mortality in atrioventricular septal defect patients with versus without Down syndrome. Down syndrome patients had significantly lower mortality compared to non-Down syndrome during the study period.
Univariate analysis revealed that the patient’s gender was not associated with mortality. White race and elective admission were associated with lower mortality. Higher mortality rates were found in premature (<37 weeks) and low birth weight infants (< 2500 grams) [3.38 (3.14–3.64), p < 0.001 and 3.64 (3.34–3.95), p < 0.001, respectively]. Neonatal repair (less than 28 days) of atrioventricular septal defect was associated with higher mortality rates compared to post-neonatal repair in non-Down syndrome patients (9.1 versus 7.2%, p = 0.02) and in Down syndrome patients (2.6 versus 2.1%, P = 0.04).
The development of pulmonary hypertension, arrhythmias, heart block, acute kidney injury, and sepsis was associated with higher mortality rates. Multivariate regression analysis revealed that the need for extracorporeal membrane oxygenation [15.68 (13.16–18.63)], acute kidney injury [5.21 (4.86–5.92), p < 0.001], mechanical ventilation ≥ 96 hours [2.46 (2.22–2.72), p < 0.001], sepsis [2.21 (1.97–2.48), p < 0.001], and pulmonary hypertension [1.75 (1.46–2.09), p < 0.001] were associated with mortality. Table 4.
Table 4. Univariate and multivariate regression analysis of the risk factors associated with in-hospital mortality after AVSD repair.
Length of stay and charge analysis
Atrioventricular septal defect patients with Down syndrome had shorter hospital stays compared to non-Down syndrome patients [7 (4–16) versus 9 (3–26) days, p < 0.001]. Patients with Down syndrome had lesser cost of hospitalisation compared to non-Down syndrome [$65,725 (19,761–156,253) versus $88,973 (22,981–251,883), p < 0.001). Patients who died had a significantly prolonged median hospital stay and higher cost of hospitalisation.
Discussion
In the current study, we used the largest national multi-centre database for atrioventricular septal defect hospitalisation in the first year of life with 61,101 patients during the period from 2000 to 2018. The primary findings in the current study are as follows: a. atrioventricular septal defect hospitalisation represented 2.6% of CHD admissions during the study period with an overall mortality of 6.3%; b. risk factors associated with perioperative mortality included prematurity, low birth weight, development of pulmonary hypertension, heart block, acute kidney injury, and sepsis; c. Down syndrome was present in 55% of atrioventricular septal defect patients and was associated with a higher incidence of pulmonary hypertension but lower mortality rates, shorter hospital stays, and lesser hospitalisation costs.
Atrioventricular septal defect with versus without Down syndrome
In the current analysis, atrioventricular septal defect represented 2.6% of all CHD hospitalisations in the first year of life. This finding is lower than previously published reports with atrioventricular septal defect representing 4–5% of all CHDs. 5 The numbers presented in the current study probably represent a more reasonable estimate given the large number of patients included over eighteen years.
More than half of atrioventricular septal defect patients had Down syndrome. The association between atrioventricular septal defect and Down syndrome was more prevalent in females, which is consistent with previous reports that suggested a slight female preponderance. Reference Fyler, Buckley and Hellenbrand3,5,Reference Gupta, Gossett, Rycus and Prodhan15 Atrioventricular septal defect was more common in White (43%) followed by Hispanic (17.3%) and Black (12.4%) populations, respectively. Similar to previous reports, racial differences also existed in the association between atrioventricular septal defect and Down syndrome. 5 Black patients with Down syndrome tend to have atrioventricular septal defect more commonly than Whites, while the association between Down syndrome and atrioventricular septal defect was less frequent in Hispanics than in White populations. Reference Fyler, Buckley and Hellenbrand3,5
Isolated atrioventricular septal defect was present in 58.2% of patients in the current analysis. The non-Down syndrome group showed a significantly higher association with CHDs including double outlet right ventricle, coarctation of the aorta, pulmonary atresia, and hypoplastic left heart syndrome. However, tetralogy of Fallot was more pre-dominant in atrioventricular septal defect patients with Down syndrome as previously described. Reference Anderson, Ho, Falcao, Daliento and Rigby1,Reference Anderson and Spicer2 Atrioventricular septal defect and tetralogy of Fallot are thought to develop by distinct mechanisms; nonetheless, their co-occurrence in patients with Down syndrome suggests sharing a common developmental basis with multiple hypothetical theories proposed. 5,Reference Gupta, Gossett, Rycus and Prodhan15,Reference Craig16
Mortality
The overall atrioventricular septal defect mortality in the current study was 6.3%, consistent with perioperative mortality in previous studies ranging between 3 and 10%. The Pediatric Heart Network study of 120 patients with atrioventricular septal defect from 2002 to 2004 reported 3% mortality rates. Reference Atz, Hawkins and Lu12 Similarly, a multi-centre analysis from the Society of Thoracic Surgeons Congenital Heart Surgery Database revealed a 3% mortality rate. Reference St Louis, Jodhka and Jacobs13 The differences in mortality rates between our 18-year analysis of the national database and these reports might reflect the enormous differences in the sample size and variations in the surgical techniques and intensive care management over the study period.
In the current study, perioperative mortality was associated with prematurity, low birth weight, development of pulmonary hypertension, heart block, acute kidney injury, and septicaemia. Atz et al identified age less than 2.5 months and weight less than 5 kg at the time of surgical repair as risk factors for mortality. Reference Atz, Hawkins and Lu12 Conversely, other studies revealed no difference between neonatal surgical outcomes and surgical repairs performed beyond the neonatal period or based on the weight at the time of surgical repair. Reference Craig16 While these differences in outcomes might be due to discrepancies in sample size, associated cardiac lesions, and surgical techniques between different institutions, it is worth mentioning that surgical repair at an earlier age was reported to be associated with higher rates of reinterventions. Reference Craig16–Reference Ono, Goerler and Boethig19
Down syndrome and mortality
In our study, Down syndrome patients with balanced atrioventricular septal defect who underwent biventricular repair had significantly less incidence of mortality compared to non-Down syndrome (2.2 versus 7.6%). This is in alignment with previous reports, St Louis et al reported lower mortality in atrioventricular septal defect patients with Down syndrome. Reference St Louis, Jodhka and Jacobs13.Reference Gupta, Gossett, Rycus and Prodhan15 A study from Leiden, Netherlands, revealed a dramatic decrease in in-hospital mortality after atrioventricular septal defect repair in Down syndrome patients down to 0%. Reference Craig16 However, in the Pediatric Heart Network report of 120 patients with atrioventricular septal defect, mortality did not differ based on the presence or absence of Down syndrome despite the higher incidence of in-hospital complications and reinterventions in the non-Down syndrome patients. Reference Atz, Hawkins and Lu12
In the current report, temporal trends of decreased mortality after atrioventricular septal defect repair existed in the non-Down syndrome patients but not in the Down syndrome group. Dhillon et al recently queried the Texas Inpatient Public Use Data file and reported an improved hospital survival over time after atrioventricular septal defect repair in non-syndromic atrioventricular septal defect patients compared to patients with Down syndrome. Reference Dhillon, Ghanayem and Broda20 The improved survival in non-Down syndrome patients could be secondary to the rising tendency to perform definitive atrioventricular septal defect repair at younger ages, which potentially lowers the risk of developing an advanced pulmonary vascular disease and had been associated with improved survival. Reference Ono, Goerler and Boethig19.Reference Dhillon, Ghanayem and Broda20
Down syndrome and pulmonary hypertension
In our study, pulmonary hypertension was more frequent in atrioventricular septal defect patients with Down syndrome. The link between pulmonary vascular disease and Down syndrome is not clearly understood. 5 Historical and recent histopathological studies failed to show any differences in the extent and progression of pulmonary vascular changes in atrioventricular septal defect patients with versus without Down syndrome despite accounting for the age in the histological findings. Reference Newfeld, Sher, Paul and Nikaidoh21,Reference Hosokawa, Vanderpool, Ishii and Nishiyama22 In contrast, other studies reported earlier development of pulmonary vascular disease in atrioventricular septal defect patients with Down syndrome secondary to pulmonary parenchymal hypoplasia. Reference Clapp, Perry and Farooki8,Reference Cooney and Thurlbeck23 The elevated pulmonary vascular resistance in Down syndrome patients is likely triggered by their higher pre-disposition to having relative hypoxia and carbon dioxide retention secondary to sleep apnoea, hypoventilation, and nasopharyngeal obstruction. Reference Hals, Hagemo, Thaulow and Sorland24 On the other side, the association between Down syndrome and pulmonary vascular disease likely plays a role in limiting the net left to right intra-cardiac shunting. The resultant decreased pulmonary blood flow in these patients might explain their less need for mechanical ventilation in comparison to non-Down syndrome patients as demonstrated in the current study.
Down syndrome and arrhythmias
In our study, 8.7% of patients had arrhythmia and 4.4% had heart block. This is consistent with the previously reported post-operative arrhythmia in atrioventricular septal defect patients between 8–9%. Reference El-Najdawi, Driscoll and Puga25,Reference Kharbanda, Blom and Hazekamp26 In atrioventricular septal defect patients, the inferior displacement of the atrioventricular node and bundle of His makes the conduction system more vulnerable to injury during surgical repair. Reference Thiene, Wenink and Frescura27 Furthermore, the suboptimal conduction tissue properties pre-dispose these patients to a higher risk of complete heart block. Reference Dunlop, Mulholland, Casey, Craig and Gladstone28 However, there is limited data about the differences in conduction disorders between Down syndrome and non-syndromic patients. In the current study, atrioventricular septal defect patients with Down syndrome had less incidence of arrhythmias with no statistically significant difference in the incidence of heart block between the two groups. This is partially in line with a recent study by Kharbanda et al who found less post-operative arrhythmias and post-operative heart block in atrioventricular septal defect patients with Down syndrome compared to those with normal chromosomes. Reference Kharbanda, Blom and Hazekamp26
The impact of Down syndrome on the conduction system and the occurrence of arrhythmia is largely unknown. It is unclear if the extra chromosome in these patients affects the development of cardiac conduction. Blom et al suggested differences in the conduction system between atrioventricular septal defect patients with and without Down syndrome. Reference Blom, Ottenkamp, Deruiter, Wenink and Gittenberger-de Groot29 While there was no statistically significant difference in the incidence of heart block between the two groups, Down syndrome patients needed less pacemaker implantation. The presence of an abnormal left atrioventricular valve often requires reoperation and is considered a risk factor for complete heart block, and the need for pacemaker implantation is less likely to occur in Down syndrome patients. Reference Al-Hay, MacNeill, Yacoub, Shore and Shinebourne30,Reference Formigari, Di Donato and Gargiulo31
Hospital stay and resource utilisation
In the current study, non-Down syndrome atrioventricular septal defect patients had longer median hospital stay and higher cost of hospitalisation compared to Down syndrome patients. This finding is inconsistent with previous studies that showed longer hospital stay in Down syndrome patients with CHD. Reference Purifoy, Spray, Riley, Prodhan and Bolin32,Reference Fudge, Li and Jaggers33 Our finding could be explained by the significantly higher incidence of cardiac and non-cardiac complications, concomitant cardiac procedures, and longer durations of mechanical circulatory and respiratory support in non-Down syndrome patients.
Feeding difficulties and gastrostomy tube placement were significantly higher in Down syndrome patients. This is not surprising and consistent with studies that demonstrated significant feeding problems, neurologic impairment, and subsequent need for gastrostomy tube in Down syndrome patients. Reference Stanley, Shepherd and Duvall34,Reference Srinivasan, Irvine and Dalzell35
While the feeding difficulties were more common in Down syndrome patients, the pre-operative planning in Down syndrome patients might have led to a shorter duration of hospital stay compared to non-Down syndrome patients. For example, a Down syndrome patient with a G-tube in place before the surgical repair will presumably be discharged earlier than one that had a G-tube during the admission for surgical repair. Reference Delany, Gaydos and Romeo36,Reference Dimopoulos, Constantine and Clift37
Limitations
The use of the National Inpatient Sample database has its own limitations including a. Inability to identify the specific details of surgical repair including the exact weight at the time of surgical repair and the presence of any post-operative residual lesions, b. The transition from International Classification of Disease, Ninth Revision to International Classification of Disease, Tenth Revision codes that occurred during the study period might have contributed to coding errors. However, there were no significant differences in the results when we ran an analysis using only International Classification of Disease, Tenth Revision codes to examine the difference between atrioventricular septal defect patients with versus without Down syndrome as illustrated in Supplemental Table 1, and c. In the International Classification of Disease, Ninth Revision version, Down syndrome was represented by only one code while in the International Classification of Disease, Tenth Revision version; three different codes were available for the three different Down syndrome subtypes: trisomy 21 (nondisjunction), translocation, and mosaicism. In the current study, we used all available codes for Down syndrome instead of only using trisomy 21code, which represents ∼ 95% of Down syndrome patients. This might have limited our ability to examine any differences in outcomes related to the Down syndrome subtype.
Conclusion
Trends in atrioventricular septal defect hospitalisation have been stable over time. Higher mortality after surgical repair was associated with prematurity, low birth weight, pulmonary hypertension, heart block, acute kidney injury, and septicaemia. More than half of atrioventricular septal defect patients had Down syndrome, which was associated with a higher incidence of pulmonary hypertension, less arrhythmia, less mortality, shorter length of hospital stay, and less resource utilisation.
Supplementary material
The supplementary material for this article can be found at https://doi.org/10.1017/S1047951123003116.
Acknowledgements
None.
Financial support
None.
Competing interests
None.









