In health care, the word ‘communication’ covers a wide range of interactions, including interpersonal communication, communication technology, medical education, health policy and mass communication. It takes many forms, from a brief informal talk between colleagues to formalised written documents between professionals. The essence of this verbal and written communication is the sharing of information. To make our information exchange more useful and to give it more meaning, the information communicated needs an appropriate framework. For example, the meaning of the diagnosis ‘schizophrenia’ is greatly enhanced by knowledge of the individual patient within the context (the framework) of his or her past history and family background.
In this paper I consider ways of organising this information to enhance its meaning and thus to improve the quality of communication. I concentrate on aspects of communication, both electronic and paper-based, related to the delivery of care and examine ways of using a common structure for the collation and presentation of information. In the past, the medical profession has communicated in ‘free text’ (ordinary written English), but there is now an increasing trend towards electronic clinical communications. Organising information improves the consistency and quality of communications, which may have a direct impact on clinical outcome. Existing standards, which pre-date the widespread adoption of electronic communication of information, developed to facilitate sharing of information between individuals at various discrete levels. For example, at one level are the doctors, nurses, social workers and others dealing directly with patients; at a higher level, are the departments within an organisation; above them are organisations communicating between themselves; and communication is also required between these levels and the service users (the patients, their families and supporters).
Good communication is clearly essential for good practice. If coordination and communication within different parts of the National Health Service (NHS) and between the NHS and other care providers such as social services breaks down, the consequence is inevitably poorer care for the patients affected (Department of Health, 1998).
The growing national emphasis on the information technology necessary for rapid and efficient communication demands excellent organisation of information.
Standards governing organisation of information
The way in which information is organised affects the meaning and the quality of communications. Standards already exist within health care to facilitate information-sharing. De Moor et al (1991) define these standards as a prescribed set of rules, conditions or requirements concerning definitions of terms, classification of components, performance, delineating procedures, or measurement of quantity and quality in describing practice, service or systems. With insufficient organisation, key information can be lost. Furthermore, insufficient detail within the framework related to the information in a communication may prevent the recipient from making an appropriate and fully informed clinical decision. Taking again the example of schizophrenia, under the framework heading of past history, recording the number of previous episodes of schizophrenia is more useful for communicating the prognosis to other professionals (and the patient) than is stating only that the patient has a history of the disorder.
The need for common standards governing the communication of information applies even more to electronic communication. The Clinical Systems Group (1998) has recommended sytems for organising clinical data and work is currently underway nationally to evaluate semi-structured communications for all professions, including trial evaluation of this approach in mental health care trusts (for further details see http://www.nhsia.nhs.uk/headings/pages/default.asp).
The NHS Executive (1999) has identified a number of areas of particular importance to the meaning and quality of communication within health care: authoring and reading health records; a common clinical language; and communicating information within and between teams.
Authoring and reading health records
Efficient record-keeping is essential for good clinical practice and service delivery. With the move towards electronic communications, electronic health records (EHRs) and electronic patient records (EPRs) have become more common. However, our paper-based records are still very important, especially as electronic information systems have yet to be widely adopted in everyday mental health practice. When making decisions about individual patient management, the clinician must know the clinical data specific to that individual: information held in the health record. Thus, patient-based data are essential and the way in which information in the health record is organised is important.
Poor organisation of a health record increases the chance of error. Studies on medical records have shown that the absence of information or inaccurate information adversely affect information retrieval and, probably, patient care (Reference Tang, Fafchamps and ShortliffeTang et al, 1994). Clinical information has been included in the paper record for many years and the way in which it is organised has developed from a simple chronological listing to a more structured and problem- or task-oriented presentation (Reference TangeTange, 1996). For example, Weed (1968) suggested that clinical information in health records be organised into four different types: subjective (what the patient has told us), objective (what we have observed), assessment (our interpretation of these findings) and plan (the management plan). He suggest the acronym SOAP (subjective, objective, assessment, plan) as a useful mnemonic for this structure. Donnelly et al (1992) later modified this framework, offering HOAP: history (what the patient has told us), observations (what we have observed), assessment (our interpretation of these findings) and plan (the management plan). Wyatt (1994) added patient identifiers and expanded the structure to include actions performed by the health worker (such as therapy initiated) and to combine assessment and plans into hypotheses. Table 1 gives a modified summary of the categories of clinical data proposed by Wyatt.
Table 1 Categories of clinical data (after Reference WyattWyatt, 1994)

| Category | Components | Examples |
|---|---|---|
| Identifiers | Demographics, identity codes | Name, date of birth, NHS number |
| Patient findings | History | Description from patient |
| Observations | Subjective: symptoms | |
| Objective: clinical signs | ||
| Assessment (hypotheses) | Assessment | Diagnosis |
| Plan (hypotheses) | Plan | Proposed treatment, tests |
| Actions | Therapy, referrals, tests, information shared, follow-up | Actual therapy initiated, tests ordered |
| Modifiers | Who recorded data, when, certainty, severity | Who made observation, when, certainty |
A common language: classification and coding
In the authoring of health records, we should use common standards for both recording and communicating information. To achieve this, health and social care professionals need a common clinical language that includes systems of classification and coding.
Classification and coding
Before examining some classification systems, I will attempt to clarify the difference between ‘classification’ and ‘coding’. In classification systems, groups of words or terms are collected together and organised. Each of these terms will be associated with a particular concept. For example, the terms ‘depressed mood’, ‘loss of interest’ and ‘bleak and pessimistic views about the future’ might appear in a classification ‘depressive episode’. Systems of classification have typically been hierarchical (visualised as a tree's roots), meaning that more detail is obtained the further down the hierarchy one proceeds, although ideas are still linked and organised around common attributes (Fig. 1). For example, a depressive episode may be mild or moderate and may occur with or without somatic symptoms.
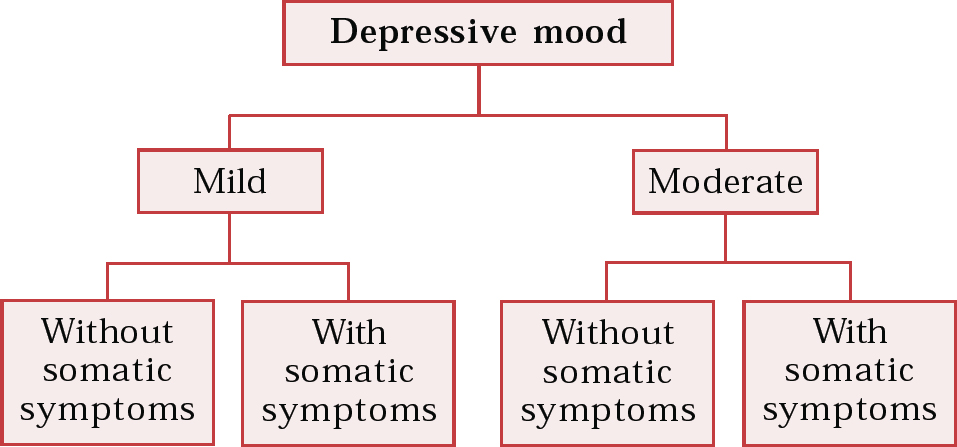
Fig. 1 A simple classification hierarchy
Each concept within a classification system can also be given a numeric or alphanumeric code. Thus, ‘depressive episode’ might have code ‘F32’. The more extensive the coding system, the more detail it can represent. Therefore a code is simply the numeric or alphanumeric system used to specify a classification or hierarchy.
Classification can therefore be used as another way of organising information and can act as a common language between health professionals, enhancing the quality and usefulness of the communication.
Examples of classification and coding systems
A classification system with which readers will be familiar is the ICD–10 (World Health Organization (WHO), 1992), which is widely used in diagnostic practice. It is interesting to note that the original purpose of the ICD was to allow the WHO systematically to collect morbidity and mortality data from all over the world for statistical analysis.
Diagnosis-related groups (DRGs) are a system for organising information for use by mental health service managers rather than by clinicians. Used to determine a service's overall in-patient case mix, DRGs relate diagnoses and costs of interventions. Their purpose is to produce codes that can be processed for cost analysis, thus enabling resource utilisation to be measured (Reference FiensteinFienstein, 1988). The basis of DRGs is ICD–9–CM (American Hospital Association, 2002), a multi-axial system itself based on ICD–9. ICD–9–CM code groupings, according to disease or body organ, are made to reflect the use of resources and treatment. Further grouping of codes according to such factors as length of stay and age are then made, after which a DRG is generated.
A problem with relying on coding alone to communicate clinical information is the size and complexity of the coding system needed to convey sufficient information. Classification systems for clinical use continue to appear that attempt to provide the detail of information required by health professionals and to facilitate communication by creating a common language (through standardised organisation of information). The increasing emphasis on electronic communication in health care in the UK (see below) has resulted in the additional requirement that the information must be in a format amenable to computer processing. Two systems in current use that try to meet these requirements are the Systematized Nomenclature of Human and Veterinary Medicine (SNOMED) and Clinical Terms.
The SNOMED has its origins in pathology. It is a general medical terminology developed to index events in the patient record (Reference Cote, Rothwell and PalotayCote et al, 1993). It is designed to be computer-processable and easily translated into different languages (Reference RothwellRothwell, 1995). Its classification is based on 11 axes, or modules (Box 1), given an alphanumeric code. Each of the 11 modules contains thousands of individual descriptive terms. Terms or descriptions are combined from the axes to give a clinical description from a particular code (the combination of qualifiers).
Box 1 SNOMED axes (after Reference RothwellRothwell, 1995)
Axis or module
Topography
Morphology
Function
Living organisms
Chemicals, drugs and biological products
Physical agents, forces and activities
Occupations
Social context
Diseases/diagnoses
Procedures
General linkage modifiers
Formerly called Read Codes, Clinical Terms were originally introduced for use in primary care and are designed to classify and code events in the EPR (Reference O'Neil, Payne and ReadO'Neil et al, 1995). Earlier versions were hierarchical, but this format could be inadequate for reflecting the true clinical picture. Rather than relying on axes of classification (the branching roots concept), with each code belonging to a particular hierarchy, the latest version allocates a unique code to each concept. Individual terms (words or phrases) describing a particular condition are combined with qualifiers. A list (template) of qualifiers is provided, including, for example, mild, moderate or severe for an illness and first, new or ongoing for an episode.
Thus, one concept (a condition or disease) might be ‘depression’. The Clinical Term ‘depression’ might include describing words such as ‘postnatal’ and ‘depressive disorder’. Add to these qualifiers: the postnatal depression might be moderate and ongoing. Each element of the resulting ‘moderate, ongoing clinical depression’ will have an alphanumeric code, making it amenable to computer processing.
As this structure uses links between concepts and qualifiers, rather than the more hierarchical approach of SNOMED, classification using Clinical Terms gives a richer description than can be obtained using a purely hierarchical structure. The terms are designed to capture and retrieve patient-centred information in natural clinical language within computer systems.
Table 2 summarises the uses of different classification and coding systems, and Table 3 compares the classifications obtained using ICD—10, Clinical Terms and SNOMED.
Table 2 Systems for different classification purposes
| Purpose | Example of system |
|---|---|
| Statistical analysis of morbidity | ICD–10, OPCS–4 |
| Relating diagnosis to cost of treatment | ICD–9–CM |
| Creating an electronic patient record | SNOMED, Clinical Terms |
Table 3 Comparison of classifications

| System | Illness example | Design |
|---|---|---|
| ICD–10 | Depressive episode | Hierarchical |
| → moderate depressive episode | ||
| Clinical Terms (version 3) | Reactive depression (moderate, ongoing) | Conceptual with qualifiers |
| SNOMED | Depressive disorder | Hierarchical |
| → moderate major depression | ||
| → moderate recurrent major depression |
Problems with coding and fully structured records
The current classification systems substantially improve the organisation of information for communication, but we should always be aware of the purpose for which they were intended. For example, DRGs are meant to measure resource utilisation, not quality of care.
SNOMED and Clinical Terms go some way towards refining the information necessary for structuring clinical records and communicating meaningful information. However, each has its problems. SNOMED allows complex terms describing the patient's condition, but because there are no rules governing combination of terms, concepts may be expressed in many different ways that might not be valid. With Clinical Terms the opposite is true: the templates restrict the terms (description of the condition) that may be combined, so forcing the user to choose only the terms allowed. This may mean that not all of the information is communicated in the way that the user intended.
Thus, coding and classifications help us to standardise our clinical language and improve communication, but do not necessarily provide a universal structure sufficient to allow the user to communicate all of the information necessary to provide day-to-day care.
Electronic patient records and electronic health records
Patient records are key to the delivery of quality health care. As patient information has burgeoned over recent years, standards for organising it have developed in parallel with the development of electronic record systems. Electronic records will form the basis of information communication in the near future, and here I will summarise the aspects of electronic systems of most importance to practitioners.
The electronic patient record (EPR) and electronic health record (EHR) are terms used interchangeably to describe electronic versions of health records. Although they seem self-explanatory, the Department of Health's (1998) Information for Health gives explicit definitions. The EPR is a record of the periodic care a patient receives from a particular institution or more specialised service, for example, the record of care from a mental health NHS trust. Essentially it comprises all patient notes, in electronic format. The EHR is a longitudinal record, held in primary care, which contains a note of any contact with health services during the life of the patient; it includes both primary care information and subsets of the EPR information.
Information for Health places a timescale on the adoption of electronic communications, particularly the EPR. The development of the EPR system is divided into six levels (summarised in Box 2). The most basic level, level 1, mainly concerns supporting the administrative functions of an organisation by using a patient administration system (PAS) with a master patient index (MPI), which is also known as a patient master index (PMI). The only support to health workers at this level is indirect, through separate, standalone departmental systems such as those for pathology results and X-rays. At level 2, the principle of common patient identifiers (such as NHS number) is adopted; basic speciality modules, for example, an out-patient clinic module, may also be included. It is only at level 3 that true support is provided to health workers in their daily practice. Systems at this level have many practical uses, all of them ‘electronic’, including preparation for ward rounds, requesting an investigation from pathology and receiving the test results, nursing assessment, care planning, automatic generation of discharge letters, prescribing and recording of drug administration, development of care profiles, and uni-disciplinary to multi-disciplinary care pathways. At level 3 and beyond, the benefits of structure to information for communications are felt the most. Levels 4 to 6 are concerned with increasing interconnectivity, with emphasis on speed, sharing of information and communication, and multi-disciplinary and cross-team working.
Box 2 Main components of the six levels of the electronic patient record
Level 1 Patient administration systems; computerised appointments; case note tracking; standalone pathology records
Level 2 Common patient identifier across department systems; out-patient clinic modules
Level 3 Computerised support for assessment, care planning, investigation requests, electronic prescribing, care pathways
Level 4 Linked knowledge and research to information management and technology clinical care support; decision support systems; electronic prescribing linked to evidence-based medicine
Level 5 Majority of clinical information stored in EPRs; advanced workflow; speciality modules
Level 6 High-speed networks; advanced data-input devices; full case notes online; teleconferencing
Organising information for communication within and between teams
The development of electronic records and communications will further highlight the need for common standards of information organisation for communicating and teamworking. It is essential that day-to-day health communications within a multi-disciplinary team convey the necessary detail and meaning. They should also be couched in an easily understandable common (standard) language and format, which, unfortunately, free text does not always confer. Nor, however, do some of the classification systems outlined here provide sufficient detail and meaning for everyday practice.
The dilemma arises that most classification or coding systems use fully structured records, or set templates, suitable for electronic communication; in our own records, however, we and other health professionals usually use free text. Communication within the NHS is not good and we sorely need standards governing information exchange for key clinical communications (Clinical Systems Group, 1998). The ideal might be a system that combines the advantages of structured records with the richness of free text.
Sharing information has been shown to improve record-keeping (Reference Johnston, Langton and HaynesJohnston et al, 1994) and it might improve outcomes. Adequate written communication is essential for good teamworking, particularly for hand-over, referrals within and to other specialities and in multi-disciplinary care. In these situations, the main source of the information communicated is the health record. The quality of the record determines the quality of the information contained in communications between members of a team, and thus a standard that can provide a common language may improve care.
As discussed above, coding and classification of health records can help in the organisation of information for communication and also in its collection for computer processing. However, at present relatively little information in health records is coded or in a structured format (Table 4). In mental health care most clinical information and communications are in a free-text format.
Table 4 Structure and type of information in typical health records

| Source of information | Example | Structure of information recorded |
|---|---|---|
| Patient/carer | History of auditory hallucinations | Free text |
| Observation | Responding to hallucination | Free text |
| Physical examination | Neurological examination | Free text/diagram |
| Investigations | Full blood count | Free text/table |
| Multi-disciplinary team discussion | Care plan | Free text |
The NHS is currently evaluating a semi-structured system for communications and possibly for health records (American Hospital Association, 2002). Its advantage is that communications are structured to provide information in a standard language, but without the limitations of hierarchical and other classifications. A template of headings for communicating patient information has been developed on the basis of previous evaluations (NHS Information Authority, 2000), and this is being assessed in everyday practice in a number of different specialities. The advantage of the semi-structured system is that its framework should improve the consistency of content of clinical communications. Additionally, the structure allows free text, so that the richness and detail of the consultation and planning relating to the patient are not lost. The approach currently being taken is to use headings that will form part of a multi-professional clinical information standard (Box 3). For further details see the NHS Headings Project website at http//www.nhsia.nhs.uk/headings/pages/default.asp.
Box 3 Headings in the NHS's draft standard for communicating patient information (NHS-Information Authority, 2000)
Health characteristics Actions
History Assessment
Family history Treatment
Social circumstances Clinical administration
Examination findings Participation
Test results
Diagnosis
Outcome
Health characteristics and actions have a past, present and future time component, in which the future health characteristics are the outlook and the future actions are the plan
A semi-structured standard for information communication may enable us to overcome the problems both of the lack of sufficient detail and flexibility associated with existing classification or coding systems and of lack of consistency and structure found in free-text communications.
Multiple choice questions
-
1. With respect to the EHR and EPR:
-
a the EPR is designed to be held in primary care
-
b the EPR contains subsets of the EHR
-
c the EHR contains records of a patient's lifetime contact with health services
-
d implementation of the EPR takes place on levels
-
e no timescale exists for the adoption of EPRs in the NHS.
-
-
2. Regarding authoring and reading health records:
-
a structure increases the chance of error
-
b records have become increasingly task-oriented
-
c subjective, objective, assessment and plan are four types of data described
-
d history, observations, assessment and plan are four types of data described
-
e identifiers, patient findings, hypotheses, actions and modifiers are categories of clinical data.
-
-
3. Regarding coding, classification and clinical language:
-
a ICD–10 is designed to communicate the clinical picture
-
b ICD–9–CM is designed to collect morbidity data on out-patients only
-
c SNOMED is used to measure resource utilisation
-
d SNOMED concepts may be expressed in many different ways
-
e Read Codes are now called Clinical Terms.
-
-
4. Regarding teamworking:
-
a structures are needed for key clinical communications
-
b most information in shared health records is written as free text
-
c separate records aid clinical communication
-
d semi-structured communications may combine the benefits of structured information and free-text information
-
e the draft standard for communicating patient information contains health characteristics.
-
-
5. With respect to communication and health records:
-
a SNOMED has its origins in pathology
-
b Clinical Terms (Read Codes) were initially used in primary care
-
c Clinical Terms contain qualifiers
-
d the sharing of information systems improves record-keeping
-
e structured communication can only be used electronically.
-
MCQ answers

| 1 | 2 | 3 | 4 | 5 | |||||
|---|---|---|---|---|---|---|---|---|---|
| a | F | a | F | a | F | a | T | a | T |
| b | F | b | T | b | F | b | T | b | T |
| c | T | c | T | c | F | c | F | c | T |
| d | T | d | T | d | T | d | T | d | T |
| e | F | e | T | e | T | e | T | e | F |








eLetters
No eLetters have been published for this article.