INTRODUCTION
Influenza is a major cause of morbidity and mortality worldwide. According to the data from the World Health Organization (WHO), seasonal influenza occurs with an annual attack rate estimated globally at 5–10% in adults and 20–30% in children [1]. Vaccination is an effective way to minimize influenza-related mortality and morbidity; many public health organizations, including the China Centers for Disease Prevention and Control, have recommended all people over 6 months old, particularly those at high risk, receive the influenza vaccine annually [Reference Feng2]. Since 2007, the Beijing Government, ahead of governments in most regions in China, has provided annual influenza vaccination to people aged 60+ years and students in primary or middle schools free of charge, and the policy greatly increased the coverage rates in the qualifying population [Reference Zhang3]. However, children younger than 5 years of age were not included in the target population for free influenza vaccination annually.
To guide influenza vaccine policies, it is important to determine the age-specific disease burden of influenza. Although previous modeling studies have shown that the majority of influenza-associated hospitalization and deaths occurred in older adults [Reference Thompson4–Reference Goldstein6], several modeling and cohort studies have identified a substantial incidence of influenza virus infections in children [Reference Matias7–Reference Hayward11]. Two meta-analyses also confirmed that the attack rate varied significantly by age with the highest in children [Reference Jayasundara12, Reference Van Kerkhove13]. A recent systematic review and meta-analysis estimated that there are about 90 million new cases of influenza occurring worldwide in children younger than 5 years of age per year, while incidence varies between regions [Reference Nair14]. In China, seasonal influenza is a notifiable infectious disease and should be reported to the National Notifiable Infectious Disease Surveillance System. However, the number of influenza cases reported through this system greatly underestimates the true burden of influenza because only a minority of influenza-associated cases and deaths are confirmed with a laboratory test. So far, very few studies were conducted to estimate the incidence of infection and outpatient visits attributable to influenza in China. In this study, we address this lack of information on influenza morbidity in China by combining evidence from hospital and laboratory surveillance systems. Our aim was to estimate the true number of influenza infections and influenza-associated outpatient visits by age group in the 2015–2016 season, and to provide evidence for the modification of seasonal influenza-targeted vaccination strategies in Beijing, the capital of China.
METHODS
Influenza-like illness surveillance
Local regulations require all hospitals in Beijing to participate in the influenza-like illness (ILI) surveillance system throughout the year. The surveillance system was designed and is managed by the Beijing Center for Disease Prevention and Control (BJCDC). During the season 2015–2016, defined as the period from the 27th week of 2015 to the 26th week of 2016, ILI surveillance was conducted in 421 hospitals in Beijing. Under this system, clinicians in internal medicine, the emergency department, the fever clinic, and the pediatric clinic were required to diagnose all ILI cases by using a standard ILI definition (patients presenting with fever ⩾38 °C and cough or sore throat) and to record the numbers of ILI consultations, which referred to outpatient visits attributed to ILI, by age group in a daily report. These data were then reported daily to BJCDC through an internet-based system. In this study, we analyze the weekly numbers of ILI consultations by age group (0–4, 5–14, 15–24, 25–59, and 60+ years).
Influenza virus surveillance
The influenza virus surveillance system, also designed and managed by BJCDC, consisted of 23 sentinel hospitals and 17 collaborating laboratories in the season 2015–2016. In this system, trained clinicians collect pharyngeal swab specimens from a convenience sample of 10–20 outpatient ILI cases per sentinel hospital per week (swabbed within 3 days of symptom onset; patients who had received antiviral drugs were excluded). Sex and age information was collected for swabbed patients. The specimens were transported to collaborating laboratories in viral transport medium at 4 °C for analysis by polymerase chain reaction (PCR). The collaborating laboratories reported the number of respiratory specimens tested and specimens positive for influenza to BJCDC every week. A more detailed description of the surveillance system can be found elsewhere [Reference Yang15]. In this study, we used the weekly numbers of total specimens submitted and specimens positive for influenza by age group (0–4, 5–14, 15–24, 25–59, and 60+ years).
Multiplier model
A multiplier model approach was previously used to estimate the disease burden of pandemic A(H1N1)pdm09 virus infection, hand, foot and mouth disease, and group A streptococcal pharyngitis in China [Reference Wang16–Reference Wu18]. In this study, we used the same model to estimate the burden of seasonal influenza (all symptomatic and asymptomatic cases whether seeking healthcare or not) by age groups in the 2015–2016 season in Beijing, China. Because the ILI surveillance system covered all hospitals and the total population of Beijing, the reported data from this system were assumed approximately to cover the total number of ILI consultations of Beijing population. Because ILI can also be caused by infections other than influenza, correspondingly, we estimated the number of ILI consultations due to laboratory-confirmed influenza by multiplying the number of reported ILI consultations from ILI surveillance by the proportion of positive (laboratory-confirmed) cases from influenza virus surveillance. Furthermore, to estimate the true number of influenza cases, symptomatic and asymptomatic, in the Beijing population (not only those presenting to health care), we built the multiplier model using the number of ILI consultations due to laboratory-confirmed influenza and the following parameters which were identified as a range of proportions from previous studies and surveys: proportion of symptomatic cases among influenza infections [Reference Carrat19], proportion of ILI cases among symptomatic infections [Reference Wang16], general consultation rate [20], sampling success rate, and test sensitivity [Reference Wang16] (see Table 1 and Fig. 1).
Fig. 1. Model parameters for estimating the burden of seasonal influenza, Beijing, 2015–2016 season. ILI, influenza-like illness. T, test sensitivity of detection of polymerase chain reaction; S, success rate for sampling pharyngeal swab specimens; C a, age-specific consultation rates; Q, proportion of ILI cases among symptomatic infections; P, proportion of symptomatic cases among influenza infections; N a, age-specific reported number of ILI consultations from ILI surveillance; R a, age-specific proportion of positive cases from influenza virus surveillance.
Table 1. Model parameters and sources of data for estimating the burden of seasonal influenza, Beijing, 2015–2016 season
ILI, influenza-like illness.
* Age-specific proportion of positive cases was calculated by dividing the number of positive specimens by the total number of specimens within each age group.
The total number of influenza infections was calculated using the following parameters (see Table 1 and Fig. 1): (1) N a was an age-specific reported number of ILI consultations from ILI surveillance. (2) R a was the age-specific proportion of positive cases from influenza virus surveillance. (3) P was the proportion of symptomatic cases among influenza infections. This parameter P was obtained from a review study, and ranged from 58·3% to 74·5% [Reference Carrat19]. (4) Q was the proportion of ILI cases among symptomatic infections. The parameter Q was obtained from a previous study in Beijing, and ranged from 26·0% to 42·0% [Reference Wang16]. (5) C a was age-specific consultation rate. In this study, we assumed that the consultation rate of ILI patients was equal to the general consultation rates available from the fourth National Health Services Survey of China in 2008, which showed that the rate among the five age groups (0–4, 5–14, 15–24, 25–59, and 60+ years) was 72·7%, 59·7%, 50·5%, 50·5% and 71·2%, respectively [20]. (6) S was the success rate for sampling pharyngeal swab specimens, which ranged from 80% to 90%, and was obtained from a study in Beijing [Reference Wang16]. The success rate encodes the proportion of swabs actually collected among patients who were swabbed, which affects positive samples and is lower than 100% due to unpredictable errors in specimen collection operations. (7) T was the test sensitivity of detection of PCR, which ranged from 95% to 100%, and it was obtained from the same study [Reference Wang16] (see Eq. (1)).
The same approach was used to estimate the number of influenza-associated outpatient visits, and the equation was as follows (see Eq. (2)):
First, we estimated the weekly numbers of influenza infections and influenza-associated outpatient visits by using the weekly surveillance data and parameters from previous studies and surveys. Second, we summed the weekly estimates to calculate the annual (July to June) number of influenza infections and outpatient visits. Then the annual attack rate was calculated as the estimated number of cases divided by the population size from the National Population Census in Beijing. In addition, according to the gold standard for indicating the onset of the influenza epidemic in China, we defined the epidemic period as the weeks in which the percentage of positive specimens reached 40% of the maximum weekly positive percentage in this season [Reference Yang15]. We defined the first to 15th week of 2016 as the epidemic weeks of the season 2015–2016. We also estimated the number of influenza infections and outpatient visits during the epidemic weeks, and calculated their rates.
For each parameter included in the model, we used a probability distribution that covered a range of proportions, form which the model randomly sampled 1000 iterations. In this study, we improved our previously published model by assuming a normal or binomial distribution for the data instead of a uniform distribution. Influenza-positive samples from influenza virus surveillance were assumed to be realized as a binomial distribution, and data informing other parameters were assumed to be normally distributed. We accounted for the uncertainty of the assumed data through probabilistic sensitivity analysis (1000 independent simulation trials) using Monte Carlo simulation. Accordingly, we obtained the mean and standard deviation of the estimated numbers from the 1000 simulations, and then calculated their 95% confidence intervals (CIs) by the mean±1·96 times the standard deviation.
RESULTS
ILI surveillance
In the season 2015–2016, a total of 635 454 ILI consultations were reported through the Beijing ILI surveillance system, the majority of children under 15 years of age (see Table 1). In all age groups, the ILI counts showed a peak in winter (see Fig. 2). The highest count for children aged 0–4 and 5–14 years occurred in the third week of 2016, but it peaked in the fourth week for people aged 15–24 years, the fifth week for those aged 25–60 years, and the sixth week for those aged 60+ years. For children aged 0–4 and 5–14 years, after a steady decline from the peak in week 3, there was a slight increase from week 8 which reached a second, smaller peak in week 11 of 2016. This pattern was not observed in other age groups.
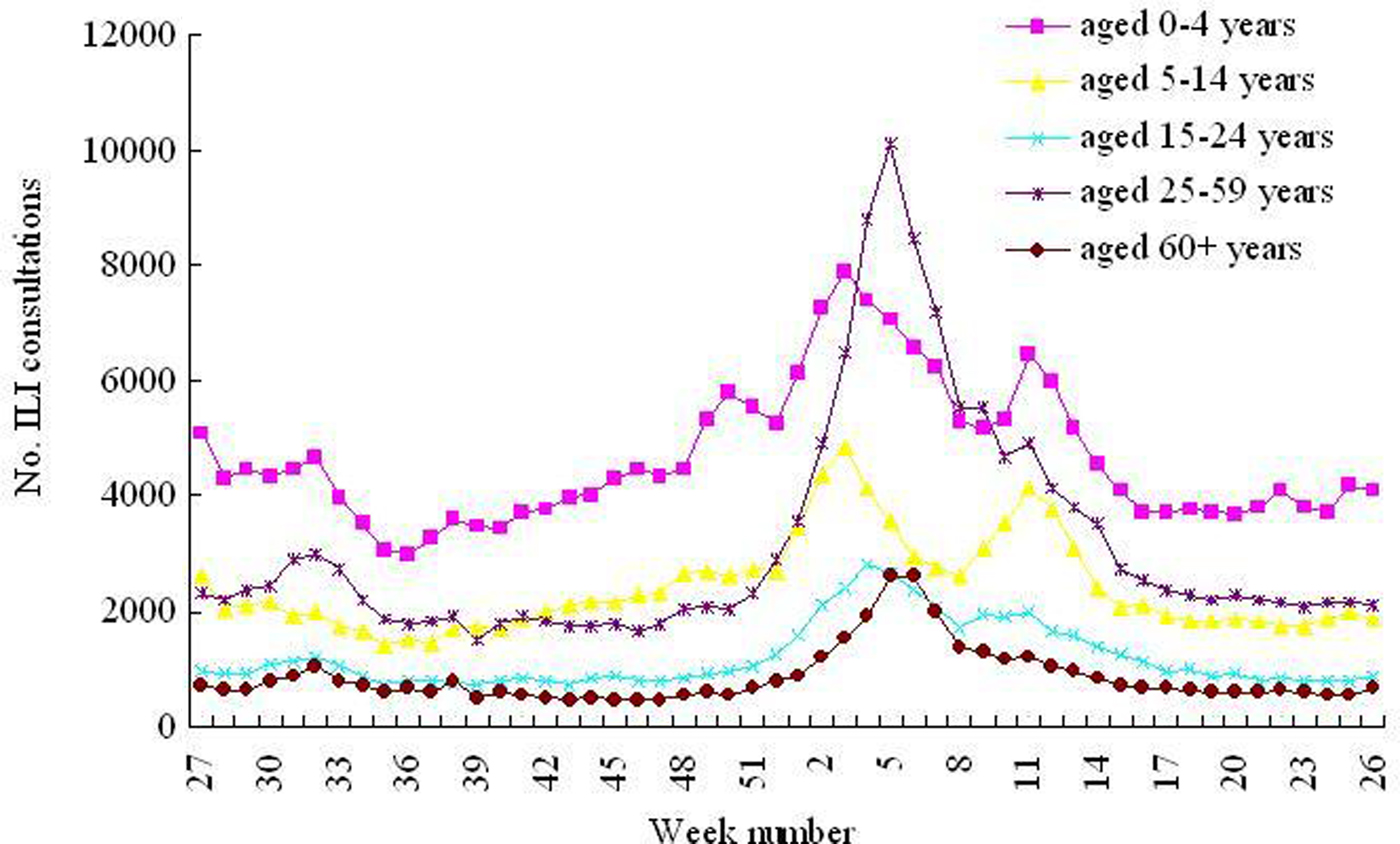
Fig. 2. Weekly reported numbers of ILI consultations from ILI surveillance, Beijing, 2015–2016 season. ILI, influenza-like illness. The starting point in the x-axis is week 27 which refers to the first week of July 2015, and the ending point is week 26 which refers to the last week of June 2016.
Influenza virus surveillance
In the season 2015–2016, a total of 19 464 specimens from ILI patients were collected and tested. An average of 18·0% of specimens tested positive for influenza aggregating over age, and the proportion positive ranged from 10·7% among children aged 0–4 years to 23·9% among older adults (Table 1). However, the proportion positive varied over time; the weekly distribution of positive and negative specimens from influenza virus surveillance is shown in Figures 3 and 4. Influenza A(H3N2) was the predominant subtype during the inter-epidemic weeks, and influenza A(H1N1)pdm09 and A(H3N2) and B Victoria lineage co-circulated during the epidemic weeks. Regarding the difference among the age groups, a higher proportion of positive specimens (an influenza A(H3N2) epidemic) was observed among people aged 60+ years but not among other age groups, indicating a small peak of influenza A(H3N2) epidemic was observed among older adults during the summer weeks (from week 32 to 35 of 2015).
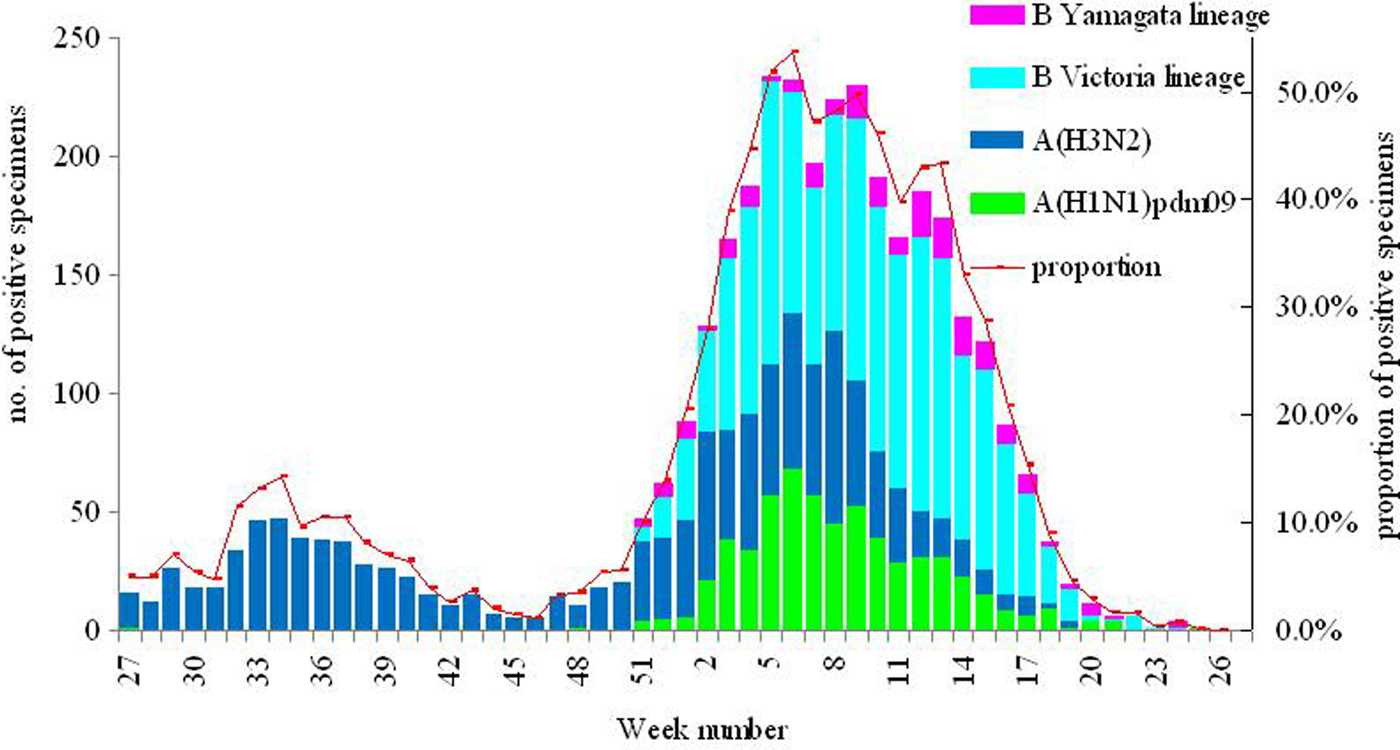
Fig. 3. Weekly reported numbers and proportions of positive specimens from influenza virus surveillance, Beijing, 2015–2016 season. Note: The starting point in the x-axis is week 27 which refers to the first week of July 2015, and the ending point is week 26 which refers to the last week of June 2016.

Fig. 4. Weekly distributions of positive and negative samples specimens from influenza virus surveillance stratified by age group, Beijing, 2015–2016 season. Note: The age-specific graphs have different scales on the y-axis. The starting point in the x-axis is week 27 which refers to the first week of July, 2015, and the ending point is week 26 which refers to the last week of June, 2016.
Estimates of influenza infections
We estimated that there were 1 190 200 (95% CI 830 400–1 549 900) cases of influenza infections, symptomatic and asymptomatic, with an attack rate of 5·5% (95% CI 3·9–7·2%) in Beijing, for the total 2015–2016 season. The attack rate was highest among children aged 0–4 years (31·9%, 95% CI 21·9–41·9%), followed by children aged 5–14 years (18·7%, 95% CI 12·9–24·5%), but much lower among the other age groups (3·6–4·0%). Restricting estimates to the 15 epidemic weeks, there were 1 025 800 (95% CI 716 000–1 335 600) cases of influenza infection, which accounted for 86·2% of influenza infections in the whole season (1 year running from July to June). Regarding the difference between the age groups, a lower proportion of the influenza infections occurred during the 15 epidemic weeks among older adults than among the younger people (77·5% vs. 85·1–89·4%) (see Table 2).
Table 2. Estimated numbers and attack rates of influenza infections (both symptomatic and asymptomatic infections) by age groups and time periods, Beijing, 2015–2016 season
* We defined the first to 15th week of 2016 as the epidemic weeks of the season 2015–2016.
§ The percentage was calculated by dividing estimated numbers of influenza infections during the epidemic weeks by estimated numbers of influenza infections during total 1 year of the season 2015–2016.
Estimates of influenza-associated outpatient visits
Seasonal influenza resulted in 468 300 (95% CI 70 700–606 800) outpatient visits in the 2015–2016 season, with an attack rate of 2·2% (95% CI 0·3–2·8%) (Table 3). The attack rate was significantly different across the five age groups, and much higher among children aged 0–4 and 5–14 years (15·4% (95% CI 10·6–20·1%) and 7·8% (95% CI 1·2–10·2%)) than among the other age groups (1·2–1·8%). During the 2015–2016 season, 86·1% of outpatient visits related to seasonal influenza occurred during the epidemic weeks, but the proportion was lower among older adults than that among other age groups (77·5% vs. 84·8–89·4%) (see Table 3).
Table 3. Estimated numbers and attack rates of influenza-associated outpatient visits by age groups and time periods, Beijing, 2015–2016 season
* We defined the first to 15th week of 2016 as the epidemic weeks of the season 2015–2016.
§ The percentage was calculated by dividing estimated influenza-associated outpatient visits during the epidemic weeks by estimated influenza-associated outpatient visits during total 1 year of the season 2015–2016.
Weekly distribution of influenza infections and influenza-associated outpatient visits
Estimated weekly incidence of influenza infections peaked between the third and fifth weeks of 2016 for people aged 15+ years; but for children aged 0–4 and 5–14 years, two peaks were apparent: before and after the winter holidays (from the fourth to eighth weeks of 2016), first peak in weeks 3 and 5 and the second peak in weeks 11 and 12 for the respective age groups, and decreased incidences were observed during the winter holidays. For 0–4-year olds, this pattern was also observed within outpatient visits related to seasonal influenza but less clearly in 5–14-year olds (see Fig. 5).
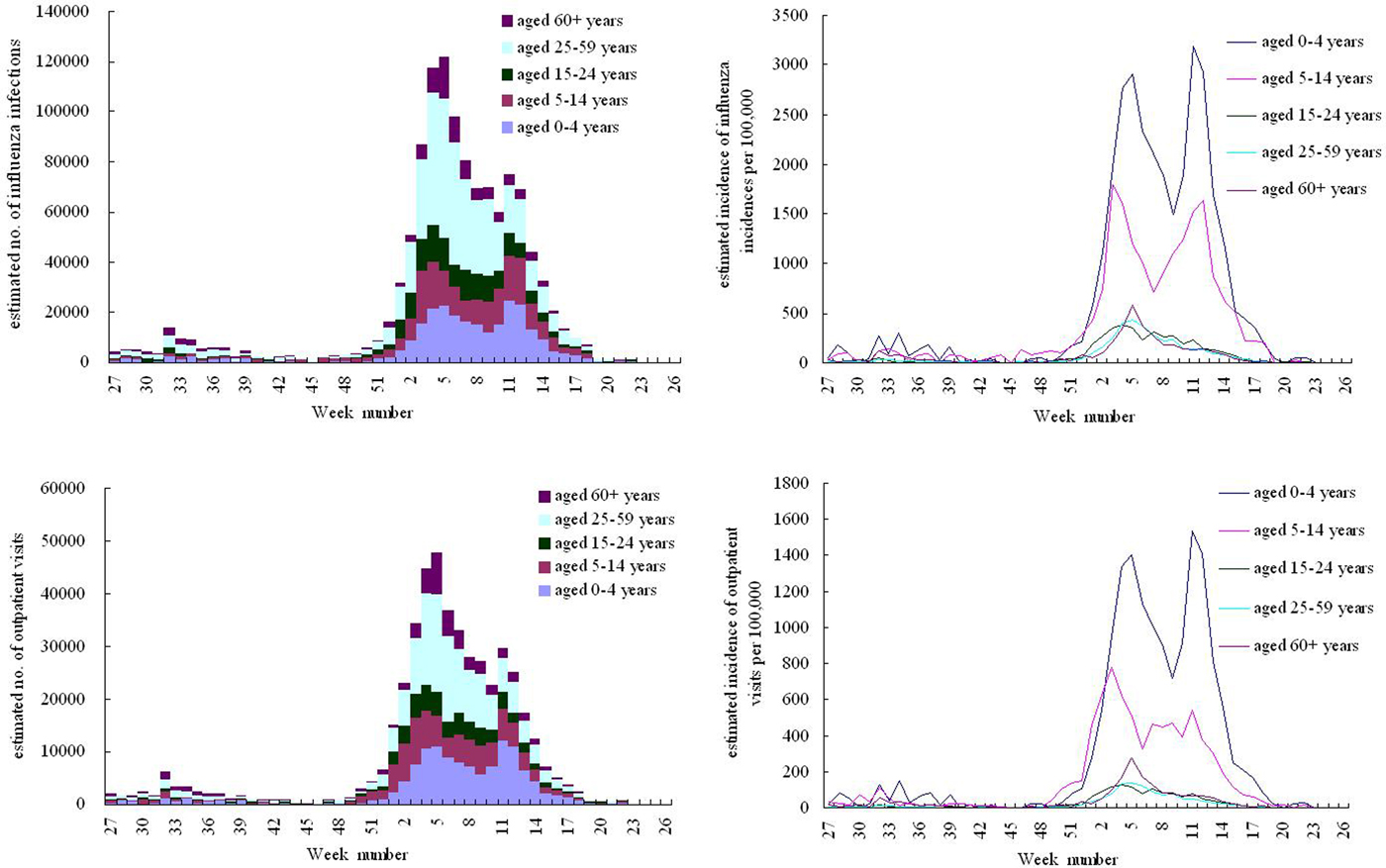
Fig. 5. Weekly estimated numbers and incidences of influenza infections and influenza-associated outpatient visits by age groups, Beijing, 2015–2016 season. Note: The starting point in the x-axis is week 27 which refers to the first week of July 2015, and the ending point is week 26 which refers to the last week of June 2016.
DISCUSSION
This is to our knowledge the first study to estimate the morbidity incidences of seasonal influenza in China. We estimated that a total of 1 190 200 (95% CI 830 400–1 549 900) cases of influenza infection occurred in Beijing during the 2015–2016 season resulting in 468 300 (95% CI 70 700–606 800) influenza-associated outpatient visits. This puts a large burden on health care capacity and financial resources.
We estimated that the attack rate of seasonal influenza among children aged 0–4 and 5–14 years was 31·9% (95% CI 21·9–41·9%) and 18·7% (95% CI 12·9–24·5%), respectively, and much higher than that among the older age groups (3·6–4·0%). This result was consistent with the data from the WHO estimating that seasonal influenza occurs globally with an annual attack rate of 20–30% in children, although our result for adults was lower than the WHO estimates of 5–10% [1]. Considering the health service burden, we estimated that 15·4% (95% CI 10·6–20·1%) of children aged 0–4 years, 7·8% (95% CI1·2–10·2%) of children aged 5–14 years and 1·2–1·8% of people aged 15+ years had influenza-associated outpatient visits in the 2015–2016 season. These data highlighted that children aged 0–14 years have notably higher rates of influenza infection and outpatient visits due to seasonal influenza.
Since 2007, the Beijing Municipal Government has provided annual seasonal influenza vaccination to older adults aged 60+ years and primary and middle school students free of charge, and the coverage rates of influenza vaccination have increased significantly among these groups until approximately 40% [Reference Cowling10, Reference Wu21]. However, preschool children were not included in the target population for free influenza vaccination annually. While many previous studies including the modeling studies from China have shown that the majority of influenza-associated hospitalizations and deaths occurred in older adults [Reference Feng22, Reference Yu23], our study additionally revealed that the preschool- and school-aged children had the highest morbidity incidences of seasonal influenza. A systematic review reported a similar result and concluded that influenza is a common pathogen in children aged younger than 5 years and results in a substantial burden on health services [Reference Nair14]. Therefore, seasonal influenza vaccination strategies could consider to also target populations at high risk for morbidity burden such as the preschool children.
Children are also drivers of community transmission of influenza virus infection. For children aged 0–14 years, we observed an interruption of the epidemic with a decrease of influenza-related morbidity during the 1-month winter holidays. In Beijing, like most northern regions in China, epidemics of seasonal influenza usually peak in January–February. Besides the relatively short public holidays, preschool and school-aged children have two longer holidays: the 2-month summer holidays (July and August) and the winter holidays (for about 1 month around Chinese New Year, which is usually at the end of January or the beginning of February). In the season 2015–2016, the winter holidays and the peak of influenza epidemics overlapped in time which may explain the decrease in influenza infections in children aged 0–14 years during the winter holidays. However, the identified drop in ILI consultation rates and hospital outpatient visits may also be explained by a transitory change in the population denominator, if children are less likely to consult because of family travels outside of Beijing during the school holidays. Nevertheless, our findings are consistent with the modeling studies from Europe [Reference Jackson, Vynnycky and Mangtani24, Reference Cauchemez25]. A study of primary care data from England and Wales found that school holidays reduced the incidence of influenza among children aged 5–14 years by 17% compared with school term time [Reference Jackson, Vynnycky and Mangtani24]. A French study estimated that routine school holidays in France had prevented 18–21% of seasonal influenza cases in children aged <18 years [Reference Cauchemez25]. These results confirmed that school closure due to school holidays could reduce transmission during the influenza epidemics.
China national influenza surveillance data have shown that seasonality patterns of influenza vary by region in China: epidemics peaked in winter in northern China, in summer in southern China, and in both summer and winter in intermediate latitudes [Reference Yu26]. In the current study, a small peak of influenza A(H3N2) epidemic was observed most clearly among older adults during the summer weeks (from weeks 32 to 35 of 2015, the period overlapped with the summer holidays). During the summer holidays, older adults were more likely to travel with their families especially grandchildren to southern or central parts of China, where the level of influenza activity was high and influenza A(H3N2) was the predominant subtype during the same period. Meanwhile, older adults could have been more likely to be infected by influenza A(H3N2) because of low vaccine effectiveness against influenza H3N2 [Reference Kelvin and Farooqui27]. Therefore, greater exposure to children in summer and susceptibility to H3N2 could contribute to an increase in infections among older adults during the summer weeks.
The present study estimated the morbidity incidence of seasonal influenza based on robust surveillance data: ILI data from the ILI surveillance system covered all hospitals in Beijing basically covering the entire population of over 21 million inhabitants, which is unique as most systems globally cover only a small fraction of their population. Further, the data on influenza virus is from a notably large-sample surveillance in Beijing. The reported data from the two surveillance systems well represent influenza circulation in the Beijing population; thus, the estimates of this study would be correspondingly precise estimates of the public health burden of influenza in Beijing. However, this study has several limitations. First, influenza burden varies considerably between seasons because of changing conditions such as the epidemic strength and age distribution of cases, but this study only covers just one season. Second, under-reporting and misclassification of ILI cases may have led to underestimation or overestimation of influenza-related morbidity burden. Third, because there was no special survey on healthcare-seeking behaviors among just ILI cases, our model assumed that the consultation rate of influenza infections was equal to the overall consultation rate for any health complaint by age groups from the fourth National Health Services Survey of China. Nevertheless, our previous studies revealed that the rates from the national survey were almost equal to the consultation rate of patient-defined hand, foot, and mouth disease, indicating that they were reliable for use in the modeling studies [Reference Wang17, Reference Wu18]. Fourth, because Beijing does not have access to local respiratory syncytial virus (RSV) virology data, we were unable to control for RSV co-circulation. Fifth, patients who received antiviral drugs may be more likely to have influenza and belong to particular age groups, and therefore excluding these patients would cause a danger of bias accordingly. Nevertheless, most outpatient ILI cases presented with mild symptoms while most mild influenza infections (95·9%) did not take the antiviral drugs in Beijing [Reference Yang28]. Additionally, the proportion symptomatic or the proportion with symptoms falling within ILI case definition may vary by age groups and virus strains, which could lead to the difference between seasons and age bands. Finally, we could not identify the drop in estimated influenza incidence during the winter school holiday as a reduction in transmission, due to a lack of suitable data.
CONCLUSIONS
Our study demonstrates substantial influenza-related morbidity incidence in the season 2015–2016, in Beijing, China, especially in the preschool- and school-aged children. This suggests that the development or modification of seasonal influenza-targeted vaccination strategies need to recognize that the attack rates are greatest in children. Additionally, we show that a decrease of influenza-related morbidity was observed among children aged 0–14 years during the 1-month winter holidays, while travel-related infections may have contributed to the small peak in influenza incidence among older adults during the inter-epidemic period.
AUTHORS’ CONTRIBUTIONS
SW, PY, and QW designed the study; SW, YP, WD, LZ, YS, YZ, and XZ performed the data collection; PY and QW coordinated and supervised the data collection; SW analyzed the data; SW, LvA, LW, SAM, and WvdH participated in the interpretation of data; SW drafted the initial manuscript; SW, LvA, SAM, EP, TK, WvdH, and MABvdS revised the manuscript. All authors have read and approved the final version of the manuscript.
ACKNOWLEDGEMENTS
The authors thank the laboratories, hospitals, and clinicians of Beijing. The authors also gratefully acknowledge the support from the other Chinese and Dutch participants involved in MoU: Prof Liu Qiyong, Ewout Fanoy, Yang Jun. This work was supported by Beijing Science and Technology Planning Project (Z131100005613048), Beijing Health System High Level Health Technology Talent Cultivation Plan (2013–3–098), Beijing Young Top-notch Talent Project (2014000021223ZK36), and the Memorandum of Understanding between the Ministries of Health of China and the Netherlands.
DECLARATION OF INTEREST
None.











