Introduction
Excited delirium is defined by combativeness, agitation, and altered sensorium. This adrenergic state may result from psychiatric conditions, recreational drug use, or rarely medical conditions.Reference Vilke, Debard and Chan1 Among the most serious deleterious consequences are rhabdomyolysis hyperthermia and sudden death.Reference Vilke, Debard and Chan1
In the prehospital and emergency department (ED) settings, excited delirium requires immediate treatment for the safety of both patients and their caregivers. In the past, physical restraint was the predominant method used to control the patient during transport.Reference O’Connor, Rebesco and Robinson2 Safety issues for patients and caregivers necessitated a re-evaluation of the use of physical restraints.Reference Vilke, Debard and Chan1 Initially, treatments for agitation including antipsychotics and benzodiazepines were used, but more recently, prehospital ketamine has become common.Reference Scheppke, Braghiroli, Shalaby and Chait3–Reference Linder, Ross and Weant6
Ketamine is an N-methyl-D-aspartate (NDMA) receptor antagonist that produces analgesia at lower doses but may precipitate general anesthesia with a dissociative state at higher doses.Reference Linder, Ross and Weant6 Routes of administration include intraosseous (IO), intramuscular (IM), intranasal (IN), and intravenous (IV). Emergency Medical Services (EMS) typically use the IM route due to the difficulty in obtaining IV access in patients with excited delirium. The onset of action is approximately three to four minutes when given IM and approximately 30 seconds when given IV.Reference Linder, Ross and Weant6 In addition to rapid onset of action, ketamine generally maintains airway reflexes and generally has a favorable side effect profile. The higher doses of ketamine IM have a more rapid onset and offer obvious advantages to EMS providers.Reference Linder, Ross and Weant6
Ketamine is safe and well-tolerated when administered in a controlled environment for procedural sedation, as patients rarely lose their airway or respiratory drive.Reference Linder, Ross and Weant6 However, co-ingestants may alter the properties of the drug. While there have been prior studies showing the safety of utilizing large doses of ketamine intramuscularly to treat agitation, a significant subset of these patients require intubation.Reference Parks, Alter, Shih, Solano, Hughes and Clayton7,Reference Olives, Nystrom, Cole, Dodd and Ho8 Risk factors for respiratory arrest and intubation have not been well-established.
In one related study with prehospital use of ketamine for excited delirium, patients subsequently intubated in the ED tended to have higher temperatures and lower Glasgow Coma Scale (GCS) scores compared to those not intubated, although there was no control for possible confounding by co-ingestants.Reference Parks, Alter, Shih, Solano, Hughes and Clayton7 It is known that many patients with excited delirium are intoxicated on illicit substances. Therefore, using data-derived hypothesis generation, this study builds upon the previousReference Parks, Alter, Shih, Solano, Hughes and Clayton7 and describes the association between prehospital ketamine administration in excited delirium with concomitant illicit and prescription substance intoxication and subsequent ED intubation.
Methods
This was a retrospective chart review from January 1, 2017 through April 30, 2019 of patients treated at two South Florida (USA) community hospitals with a combined annual volume of 81,000. This research was approved by the institutional review boards of Florida Atlantic University (Boca Raton, Florida USA; study #1342058) and Baptist Health South Florida (Miami, Florida USA; study #1446400). This study collected new data about patients enrolled in a prior study, whereby the electronic medical records of all ED encounters were queried by the medical records department for the word “ketamine.”Reference Parks, Alter, Shih, Solano, Hughes and Clayton7 Using this previously generated report, all patient charts were individually screened by a medically trained co-investigator, blinded to the hypotheses, for the prehospital use of ketamine for excited delirium. Inclusion criteria were age 18 years or greater and ketamine IM administration for excited delirium by prehospital providers. Patients were excluded if ketamine was used by EMS for post-intubation sedation, pain control, or as an induction agent. The EMS protocol for excited delirium, defined as a patient presenting with bizarre/aggressive behavior, consisted of: ketamine 400mg IM, may repeat one time as needed, with maximum single dose 400mg IM; if patient begins to wake up: midazolam 2.5mg IV/IO slowly over two minutes or midazolam 5mg IN/IM.
After initial screening, a different medically trained co-investigator performed a chart review of the hospital records of eligible patients. Variables collected included age, gender, comorbidities, ketamine dose, height, weight, laboratory values, substance use, need for intubation, and index visit mortality. Laboratory values collected were initial creatine phosphokinase, creatinine, sodium, lactic acid, ethanol level, and urine drug screen (UDS) immunoassay results. Qualitative analysis of urine toxicology included amphetamines, barbiturates, benzodiazepines, cocaine, marijuana, opiates, and phencyclidine (PCP). History of present illness (HPI) documentation from the ED physician notes was evaluated for patient use of illicit substances (barbiturates, cocaine, ecstasy, heroin, lysergic acid diethylamide [LSD], marijuana, methamphetamines, PCP, and synthetic cathinones [bath salts/flakka]); prescription drugs of abuse (benzodiazepines, gabapentinoids, hypnotics, opioids, and stimulants); and alcohol use. Both EMS/ED administration of additional sedatives were recorded (benzodiazepines, typical antipsychotics, atypical antipsychotics, and opioids). The primary outcome variable, whether the patient required intubation, was determined based on review of ED physician notes. Index visit mortality was determined based on hospital disposition. These data were reviewed by a second investigator to confirm data extraction accuracy and minimize bias.Reference Kaji, Schriger and Green9 All study data were entered into Research Electronic Data Capture (REDCap), a Health Insurance Portability and Accountability Act (HIPAA)-compliant web-based data management system with real-time error checking.
Analyses of toxicological laboratory data, first without and second including HPI data, were performed using SPSS Statistics Version 27 (IBM Corporation; Armonk, New York USA). In the first analysis, co-ingestant variables were defined by either UDS results (positive or negative) or blood alcohol levels (a level 100mg/dL or greater was defined as positive). Patients without UDS or blood alcohol level testing were excluded from this analysis. For the second analysis, combined with the toxicological data, if a patient was on an illicit substance based on the HPI, then that substance was defined as positive and all other illicit substances were defined as negative. If an illicit substance was documented as negative, then that substance was defined as negative. For prescription drugs of abuse and alcohol abuse, the same methodology was followed. Any patients that had unknown or not documented illicit substance use, prescription drug abuse, or alcohol abuse in the HPI were excluded from the respective analyses. Patients who used heroin per the illicit substance HPI, used an opioid per the prescription drugs of abuse HPI, or opiates on UDS were combined. Methamphetamines, stimulants, and amphetamines were similarly combined. Since UDS benzodiazepines positivity may reflect both patient abuse as well as medical treatment, an additional analysis was performed excluding patients who received benzodiazepines by EMS or in the ED. To compare patients intubated to those who were not for each of the ingestants, odds ratios (OR) were used as measures of effect with 95% confidence intervals (CI). Fisher’s Exact Test was used to compare proportions, while Student’s T-test was used to compare means.
Results
Of the 86 patients enrolled in the study, 61 had blood alcohol levels tested, 62 had UDS testing performed, 61 had HPI of alcohol use documented, 61 had HPI of illicit substance use documented, and 15 had HPI with prescription drug abuse documented. Baseline characteristics including age, ketamine dose, and body mass index, defined as weight in kilograms divided by height in meters squared, were similar between patients who did or did not undergo intubation (Table 1). Male gender was significantly associated three-fold with increased rate of intubation (26% male versus 9% female; P = .042). There were no deaths during index hospitalization. Table 1 shows that creatinine was significantly higher and sodium significantly lower in the group requiring intubation.
Table 1. Patient Characteristics by ED Intubation

Abbreviations: BMI, body mass index; CPK, creatine phosphokinase; CI, confidence interval.
a Odds ratio (95% CI).
Of the 62 patients who had a UDS performed, patients positive for cocaine were significantly more likely to be intubated than those negative for cocaine (36% versus 10%; OR 5.14; 95% CI, 1.33 to 19.83). Patients positive for benzodiazepines also had a higher rate of intubation (53% versus 7%; OR 15.75; 95% CI, 3.48 to 71.27), though this association became non-significant after excluding patients who were treated with benzodiazepines during their EMS/ED care (20% versus 7%; OR 3.50; 95% CI, 0.29 to 41.99). There was no difference for patients who had any other illicit substance positivity based on UDS testing (Table 2). Alcohol levels of patients intubated (51mg/dL; standard deviation [SD] = 115) versus not intubated (99mg/dL; SD = 150) were not significantly different (−48mg/dL difference; 95% CI, -138 to 42; P = .289).
Table 2. Substance Co-Ingestion Positivity using Laboratory Data by ED Intubation
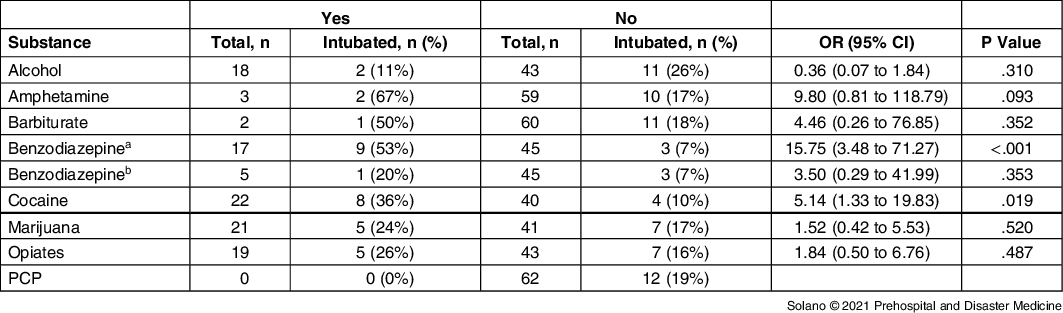
Abbreviations: ED, emergency department; EMS, Emergency Medical Services; PCP, phencyclidine.
a Overall benzodiazepine results.
b Excludes EMS/ED administration.
When combining HPI and laboratory data, there were similar trends to the analyses of laboratory data alone. Table 3 shows that 27 patients had suspected cocaine intoxication. Among these, nine were intubated (33%) compared with only four of the 50 (8%) without cocaine intoxication (OR 5.75; 95% CI, 1.57 to 21.05). There were no patients taking gabapentinoids, LSD, or PCP. Among the remaining substances, there were limited numbers of patients for amphetamines, barbiturates, ecstasy, marijuana, opiates, and synthetic cathinones (Table 3).
Table 3. Substance Co-Ingestion Positivity using Combined HPI and Laboratory Data by ED Intubation
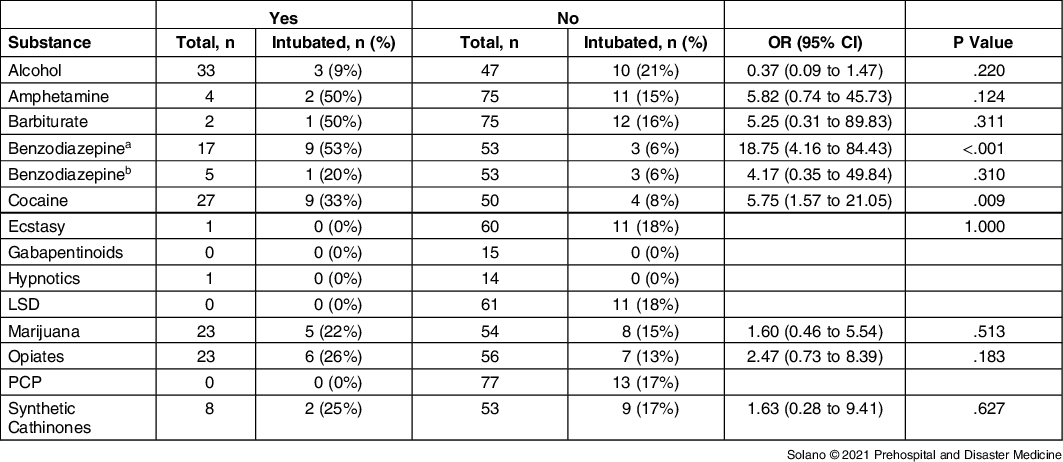
Abbreviations: ED, emergency department; EMS, Emergency Medical Services; HPI, history of present illness; LSD, lysergic acid diethylamide; PCP, phencyclidine.
a Overall benzodiazepine results.
b Excludes EMS/ED administration.
Discussion
These data indicate that patients given prehospital ketamine IM for excited delirium with concomitant cocaine intoxication had a significant 5.75-fold higher risk of subsequent intubation in the ED. Of 62 who had a UDS performed, 35% tested positive for cocaine, and 36% of those required intubation. In a previous study of patients given ketamine IM for excited delirium, 63% required intubation, of which 18.7% tested positive for cocaine; sympathomimetic ingestion was not associated with intubation.Reference Olives, Nystrom, Cole, Dodd and Ho8 In another investigation comparing agitation treatment modalities for prehospital agitation, 11.6% of patients treated with ketamine were intubated, with cocaine co-ingestion present in 18.2% of all patients intubated compared with 14.3% of those not intubated.Reference O’Connor, Rebesco and Robinson2
Although further research is certainly warranted, it is tempting to speculate about possible mechanisms whereby prehospital ketamine IM for excited delirium with concomitant cocaine intoxication may increase subsequent intubation in the ED.Reference Hennekens and Buring10,Reference Hennekens and DeMets11 For example, cocaine may deplete excitatory neurotransmitters and lead to an exaggerated respiratory depression requiring clinical intervention of intubation. In an animal study with toxic doses of cocaine and amphetamines, the use of ketamine led to a significantly higher mortality in these groups.Reference Hayase, Yamamoto and Yamamoto12
In the current data, the sample sizes were too small to draw any firm inferences about concomitant amphetamine or barbiturate intoxication, though there were possible but nonsignificant increased risks of intubation. In this study, there were no patients with PCP, LSD, or gabapentinoid intoxications. Only one patient was found to have taken ecstasy or hypnotics based on HPI. Finally, prehospital ketamine administration to agitated patients with synthetic cathinone, alcohol, and opiate intoxications had no significant increased rates of subsequent intubation.
Limitations
While chance seems unlikely as a plausible alternative explanation, there are many potential sources of bias.Reference Hennekens and DeMets11 For example, use of positive urine toxicology as a surrogate for intoxication of a substance may be influenced by issues associated with urine drug testing, including the prolonged excretion of substances after the physiological effects have ceased. Also, urine immunoassays have issues with false positive and false negative for several categories tested. These measures, while inconclusive, may be the best available to measure intoxication. In addition, elements of HPI with laboratory data that included drugs not routinely assayed in these EDs were combined. Analysis of combinations of illicit and prescription drugs was not performed even though a patient may have had multiple co-ingestants. Finally, since chart reviews were utilized, it is possible the HPI contains errors or omissions of substance use.
With respect to generalizability, the two study hospitals are community suburban EDs with short EMS transport times so the findings may not be applicable to patients admitted to urban or rural EDs.
Conclusion
Patients treated with prehospital ketamine IM for excited delirium who had concomitant cocaine intoxication had a statistically significant 5.75-fold increased rate of subsequent intubation in the ED. No deaths were found in the study group. Amongst other substances, no other trends with intubation were noted, but further study is warranted.
Conflicts of interest
The authors report no conflicts of interest. Presented at: Oral Presentation – the National Association of EMS Physicians 2021.






