Medically unexplained symptoms (MUS) are common in primary and secondary care. There is a wide spectrum of presentation, from relatively mild and transient symptoms to more severe and persistent states. MUS are associated with considerable healthcare and societal costs, including increased use of healthcare services, over-investigation of symptoms, delivery of ineffective treatments, considerable sickness absence and significant disability benefit payments. Addressing MUS is a priority for NHS England, and current plans involve delivering treatment via the Improving Access to Psychological Therapies (IAPT) programme (IAPT 2015).
Reference Hartman, Blankenstein and MolenaarHartman et al (2013), in guidelines prepared for Dutch general practitioners, review the wide range of theoretical models suggested as underpinning MUS, and briefly mention the possible role of early attachments. There is now an extensive body of evidence that insecurity of attachment is related to both the onset of illness and disease, and the ways that people interact with healthcare services (Reference Maunder and HunterMaunder 2008).
In this article, we focus on attachment theory as a heuristic framework. This is not to dismiss other theories, but because we think it is a theory that has particular practical value for clinicians in terms of treatment and clinical role. MUS are perplexing disorders that involve not just the individual concerned, but also their relationships with healthcare professionals, and the language of distress and medical processes (Reference Eriksen, Kirkengen and VetlesenEriksen 2013).
We include reference to research addressing the relationship between attachment security and the ways that people with long-term organic physical disease seek care from healthcare professionals. There are important parallels between how people respond to enduring physical symptoms that have an organic cause and how they respond to symptoms that are medically unexplained. In clinical settings, patients often present with symptoms of both types rather than one or the other. Attachment theory helps in understanding not only how conditions may develop, but also how they may become persistent and enduring. Understanding the pathogenesis of MUS is an important step in developing management and care pathways for these complex conditions.
Background
Medically unexplained symptoms is a term used to refer to bodily symptoms such as headache, fatigue and abdominal pain that cannot be explained by a recognised physical disease, and it includes a range of different symptoms and presentations. In primary care, the prevalence of MUS is thought to be between 10 and 30%; in secondary care the prevalence is even higher, with presentations of MUS accounting for between 35 and 55% of all new medical out-patient referrals (Reference Creed, Barksi, Leiknes, Creed, Henningsen and FinkCreed 2011a). Particularly high rates of MUS have been reported in neurology clinics (Reference Stone, Carson and DuncanStone 2009), in patients both with and without neurological disease (Reference Sharpe, Stone and HibberdSharpe 2010). It is important to be aware that MUS commonly occur in people who have recognised physical illness but their ‘symptoms’ cannot be explained by the underlying physical disorder (e.g. non-epileptiform seizures in patients with known epilepsy) or the disability associated with the symptoms is far greater than expected.
Medically unexplained symptoms vary in severity, from mild to severe. They tend to cluster into subgroups, and many so-called functional somatic syndromes such as chronic fatigue syndrome, irritable bowel syndrome and fibromyalgia are considered to be part of the MUS spectrum (Reference Aggarwal, McBeth and ZakrzewskaAggarwal 2006). There is much overlap between these conditions, but there are also clear differences in pathogenic pathways (Reference Hamilton, Gallagher and ThomasHamilton 2009). For example, gastroenteritis is a risk factor for the development of irritable bowel syndrome but not for chronic fatigue syndrome. There is conflicting evidence as to whether these conditions reflect a general underlying tendency to ‘somatise’ (i.e. focus on bodily symptoms) or whether they are discrete, separate conditions.
Both physical and psychological factors may play a role in the pathogenesis of these disorders. MUS are more common in women and they are often comorbid with depression and anxiety. There is increasing evidence that certain conditions may be triggered by an inflammatory response, such as a gut infection, which then develops into a functional somatic syndrome. Those most at risk of this happening are people who report psychological distress or vulnerability at the time of the index infection (Reference Gwee, Read and GrahamGwee 1996).
Medically unexplained symptoms are distinguished from other abnormal illness behaviours such as malingering for profit or active deception of professionals for some other purpose. Individuals with MUS are genuinely experiencing physical distress – just not the kind that is usually caused by recognised organic disease. As both patients and therapists attest, the pain and bodily distress are real to the individual, and it can be hard to distinguish symptoms that are medically explained from those that are not.
Relevance of attachment systems as caregiving and care-eliciting systems
The attachment system is a neurophysiological system found in social mammals, including nonhuman primates, and associated with a range of social behaviours, including caregiving to off-spring and care-eliciting from others. In human infants, attachment behaviours are activated at times of stress and distress and are usually manifested as careseeking behaviours such as vocal cries and seeking proximity to an identified attachment figure. The attachment figure reciprocates with caregiving behaviours: usually reduced distance and physical soothing that reduces distress and arousal. Over time, the infant learns to self-soothe when distressed, possibly by developing psychological cognitive representations of soothing and comfort that can be activated either consciously or unconsciously. In adulthood, the individual will use those childhood representations as a basis for beliefs about whether they are worthy of care (model of self) and whether others can be trusted to provide care (model of other) (Fig. 1).
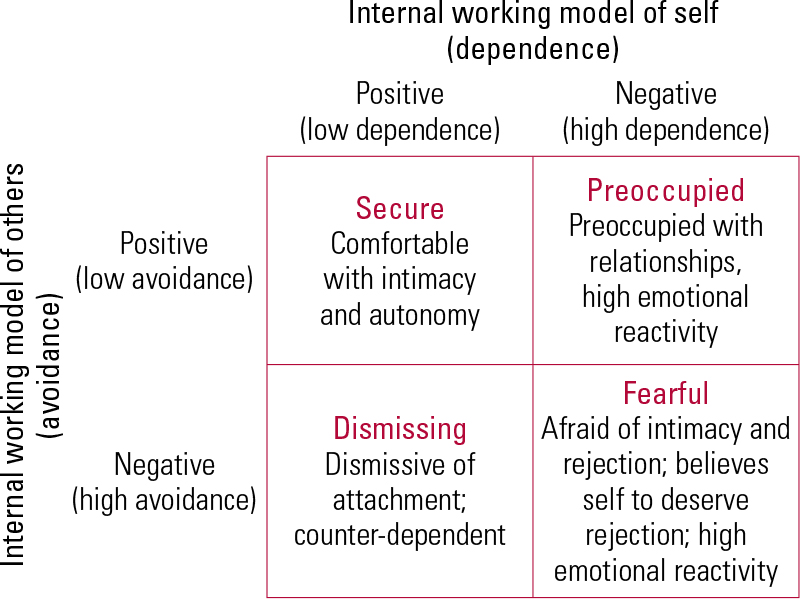
FIG 1 The four-category model of adult attachment (from Reference MaMa 2006, after Reference Bartholomew and HorowitzBartholomew 1991).
Studies of relationship behaviours between infants and carers (e.g. Reference Ainsworth and BellAinsworth 1970) have established that it is possible to reliably identify both secure and insecure attachment systems. Insecurity of attachment in childhood has been shown in both animal and human studies to persist across the lifespan and affects relationships with others in adulthood. Patterns of attachment security and insecurity are similar in all human populations, regardless of gender, class or culture.
Insecurity of attachment is not in itself a pathology, but it represents a vulnerability in terms of effective stress and distress management. It is common in the general population; large meta-analytical studies suggest that 40% of the population have an insecure attachment pattern, fairly equally divided between ambivalent and avoidant attachment (Reference Bakermans-Kranenburg and van IJzendoornBakermans-Kranenburg 2009). Childhood adversity is strongly associated with insecure adult attachment.
Insecure attachment subtypes
Insecurity of attachment has been empirically divided into three subtypes: avoidant (dismissing), ambivalent and disorganised. Some researchers add a fourth type: anxious or fearful. Those who are avoidant of attachment tend to dismiss distress and need, and avoid closeness to others. A subgroup of avoidant individuals may be actively derogatory about neediness and those who offer care. Those who are anxiously attached may be fearful, preoccupied or both. They typically seek closeness to others and express great neediness, but then withdraw or become distressed about help-seeking. Those with disorganised insecurity show elements of avoidant and anxious attachment, and this group is more likely to be diagnosed with clinical psychiatric disorders (Reference Bakermans-Kranenburg and van IJzendoornBakermans-Kranenburg 2009).
The common factor across patterns of attachment insecurity is that encounters with attachment figures are unsatisfactory in terms of stress relief and arousal reduction. When people become ill, their attachment systems are activated because illness (and perceived illness) is a life threat and vulnerability is increased. When people identify themselves as ‘patients’, they usually experience heightened dependence on professional caregivers, which may trigger early internal working models of careseeking behaviour. Insecurity of attachment could theoretically result in both dysfunctional care-eliciting as adults and unsatisfactory relationships with professional caregivers (Table 1).
TABLE 1 How attachment style affects care-eliciting behaviour and relationships with professional caregivers
Assessing attachment: a brief comment
There is a wide variety of measures with various psychometric properties for assessing different aspects of adult attachment using interview or self-report questionnaires (Reference Roisman, Holland and FortunaRoismann 2007; Reference Ravitz, Maunder and HunterRavitz 2010). In general, interview methods assess the individual’s unconscious representation of childhood care experience and relational dependency, and the defences against any attachment anxiety, whereas self-report questionnaires assess the individual’s conscious attachment style, most commonly in relation to other adults as peers or partners.
The most common interview is the Adult Attachment Interview (AAI) (reviewed in Reference Hesse, Cassidy and ShaverHesse 2008). This generates a narrative text which is analysed linguistically with reference to a manual. The AAI is unwieldy and expensive to administer (although it arguably provides the best assessment of childhood attachment representation). The Parental Bonding Instrument (PBI) (Reference Parker, Tupling and BrownParker 1979) is a self-report instrument that is easier to administer and also gives an approximation of recalled childhood care.
There are many self-report measures, most of which focus on adult relationships in the ‘here and now’. The most commonly used (Reference Fraley, Waller and BrennanFraley 2000) include the Relationships Questionnaire (Reference Bartholomew and HorowitzBartholomew 1991) and the Experiences in Close Relationships (ECR) scale (Reference Brennan, Clark, Shaver, Simpson and RholesBrennan 1998). Attachment researchers such as Shaver and Fraley recommend the use of dimensional measures such as the ECR-R because most individuals’ attachment styles involve a degree of security, anxiety, ambivalence and avoidance that changes in different relational contexts.
Attachment insecurity and organic conditions
Chronic pain
There has been increasing recognition of the role of adult attachment style in the experience of pain (Reference Meredith, Ownsworth and StrongMeredith 2008). Insecure attachment may be a risk factor for chronic pain that does not respond to ordinary analgesia (Reference Davies, Macfarlane and McBethDavies 2009). Studies have found that insecure attachment in healthy adults is associated with hypochondriacal beliefs, hypervigilance to pain, increased pain-related fears, reduced pain threshold and poor coping with pain.
Among individuals with chronic pain, insecure attachment is associated with more negative appraisals of pain, increased pain perception and disability, increased psychological distress and impaired coping with pain, and greater utilisation of healthcare services (Reference Ciechanowski, Sullivan and JensenCiechanowski 2003).
Diabetes: severity and treatment adherence
Reference Ciechanowski, Katon and RussoCiechanowski et al (2001) investigated attachment security in people with type I and type II diabetes attending primary care clinics. Of 367 patients, only 106 (28.9%) were rated as having a secure attachment style: 89 (24.2%) showed dismissing/avoidant attachment, 85 (23.2%) preoccupied/ambivalent attachment and 73 (19.9%) fearful attachment. There was a significant association between attachment style and glycosylated haemoglobin HbA1C (P = 0.03). Patients with a dismissing attachment style had significantly higher HbA1C than the other groups, indicating such individuals are at a much higher risk for retinopathy because of their higher HbA1C scores. Patients with a dismissing style who rated the quality of provider communication as poor had the worst control over their glucose levels.
Ciechanowski and his team repeated their study of self-care in diabetes in a larger population-based sample (Reference Ciechanowski, Russo and KatonCiechanowski 2004). In this group of 4095 patients, only 44.2% were rated as having a secure attachment style; 35.8% were rated as having a dismissing style. Rates for other insecure styles were lower than usual: 7.9% for preoccupied and 12.1% for fearful. The patients with a dismissing attachment style were significantly more likely to take less exercise, have poorer foot care, eat a less healthy diet and smoke, and less likely to adhere to oral hypoglycaemic medication. In a further study of missed appointments in primary diabetic care (Reference Ciechanowski, Russo and KatonCiechanowski 2006a), again there was an excess of insecure attachment styles (over 60%) and also a high prevalence of depression.
Poor adherence may be mediated by the effect of patients’ attachment style in their relationships with healthcare professionals. In a qualitative study of 27 patients with type II diabetes (purposively sampled), Reference Ciechanowski and KatonCiechanowski & Katon (2006b) found that a subgroup with fearful and dismissing attachment style described low levels of trust and an inability to collaborate with others. These patients also perceived a distinct power differential between healthcare providers and themselves that made them reluctant to engage. The study suggested that the rushed, impersonal nature of modern healthcare interfered with insecure patients’ ability to engage.
Other chronic conditions
Reference Rossi, Di Lorenzo and MalpezziRossi et al (2005) evaluated 200 patients suffering chronic migraine or episodic migraine without aura using the Beck Depression Inventory and the Attachment Style Questionnaire. Disability was more severe in patients with more severe depressive symptoms and insecure style of attachment. In 146 patients, Reference Maunder, Lancee and HunterMaunder et al (2005) investigated the influence of attachment style (attachment anxiety and avoidance) on depression during active phases of ulcerative colitis. Attachment insecurity moderated the relationship between disease activity and depressive symptoms. Two more recent studies have found an adverse effect of insecure attachment on the relationships of oncology patients with their doctors (Reference Holwerda, Sanderman and PoolHolwerda 2013; Reference Hillen, De Haes and StalpersHillen 2014).
Attachment security and symptom reporting
In a survey of women enrolled with a US health maintenance organisation (Reference Ciechanowski, Walker and KatonCiechanowski 2002), 701 of the 1119 individuals contacted completed a self-rating attachment questionnaire. Only 34% were rated as having secure attachment: almost half of what would be expected in a non-clinical community sample. The insecure attachment styles were fairly evenly divided between fearful (21%), preoccupied (22%) and dismissing (23%). Attachment style was significantly associated with the number of somatic symptoms reported during a 6-month period (after adjusting for covariables). Individuals with preoccupied and fearful attachment had a significantly greater number of reported somatic symptoms compared with secure individuals; those with dismissing attachment did not. The same study showed greater costs for call outs and attendance for all patients with insecure attachment styles compared with secure.
Reference Taylor, Mann and WhiteTaylor et al (2000) specifically investigated attachment style and MUS in a primary care (general practitioner) sample of 2042 consecutive attenders, using the General Health Questionnaire (GHQ) and the Attachment Style Questionnaire. The distribution of attachment security was as would be expected in a community sample, with higher levels of security (77%) than insecurity (16% avoidant, 7% anxious attachment). However, those with insecure attachment styles had higher GHQ scores than normal, with mean scores of 20 (avoidant) and 19 (anxious), compared with the normal mean score of 12. They were also more likely to attribute any physical discomfort to a physical cause. Patients who presented with unexplained physical symptoms (MUS) were 2.47 times more likely to have insecure attachment. A later study (Reference Taylor, Marshall and MannTaylor 2012) found that insecure attachment style was related to frequent attending in primary care.
Reference Waller, Scheidt and HartmannWaller et al (2004) used the AAI to assess attachment security in 37 patients with ICD-10 somatoform disorder (without severe physical or mental illness) attending a university hospital, comparing them with 20 matched healthy controls. Only 26% of the patients were rated as having a secure attachment style, compared with 60% of the controls. The controls showed the expected frequency of insecure attachment: 25% dismissing and 15% preoccupied. In contrast, the patients had high levels of dismissing (48.6%) and preoccupied (25.7%) attachment styles.
Attachment insecurity as risk factor for MUS: possible pathogenic mechanisms
The development of the attachment system might influence the risk of later MUS in a variety of ways, for example greater susceptibility to stress in adulthood, increased use of external sources of affect regulation and altered help-seeking behaviour (Reference Hunter and MaunderHunter 2001). We discuss here two further possibilities.
Attachment insecurity, embodied cognition and somatic markers of emotion
Reference DalgleishDalgleish (2004) reviews the theoretical basis for understanding how emotions are embodied. He describes a variety of brain areas that are thought to be active in the experience of embodied cognitions. These include the right orbitofrontal cortex, the limbic system and the anterior cingulate cortex. The development of these areas is a complex process that begins at birth and continues into the second decade of life (Reference Smith and GasserSmith 2005).
Newborn babies develop neural systems that integrate somatic experience into responses that are discriminating and fine tuned. By 2 or 3 years of age, children can reliably identify where a pain is on the body; and by school age, they can report pain that does not have an organic basis. The attachment relationship between infant and carer influences the development of both the sympathetic and parasympathetic (autonomic) nervous systems. Specifically, it affects arborisation and dendritisation of neural networks across the cortex and subcortical areas (Reference SchoreSchore 2001). Exposure to traumatic stress, including severe disruptions to the attachment relationship, interferes with the development of the frontal cortical executive that acts to regulate unconscious inputs from the parasympathetic nervous system innervating the gut, cardiac system, endocrine system and muscles.
Reference Damasio, Everitt and BishopDamasio et al (1996) have hypothesised that the emotions are experienced first in the body, which acts as an unconscious ‘somatic marker’ for cognitive ‘feelings’. Emotions are communicated to the brain in the unconscious parasympathetic system and elaborated by the neocortex into the ‘feelings’ that we appreciate consciously. The work of both Schore and Damasio et al emphasises the role of the frontal cortex in organising and managing somatic experience within an entire framework of self-experience. The right orbitofrontal cortex in particular seems to be important for correct identification of somatic perceptual experience.
Techniques involving the study of the brain are still in their relative infancy and it remains to be seen whether specific cognitive/emotional processes map onto discrete areas of the brain. Connections and processing far more complex than can be studied at present are likely to be involved in this complicated area. It is clear that the experiencing of physical sensation involves both peripheral and central processing, but the balance may vary widely even in the same individual. As knowledge develops in this area, the term ‘medically unexplained’ will become redundant, as evidence suggests that it is the total number or ‘burden’ of somatic symptoms and the patients’ concern about those symptoms that best predict both disability and future healthcare use (Reference Tomenson, Essau and JacobiTomenson 2013).
Childhood trauma, attachment insecurity and MUS
Early childhood adversity is a known risk factor for both poor physical health and MUS in adulthood. This risk relationship may be mediated by insecurity of attachment, which is also known to be associated with early childhood adversity. Children who are exposed to maltreatment by a carer not only experience repeated physical pain and fear arising from these assaults, but also are unable to turn to that carer to manage their distress. Repeated stress and hyperarousal owing to lack of care may damage normal development, in terms of either the somatic response to stress or dysregulation of cognitive and affective responses to somatic stimuli (Reference Weich, Patterson and ShawWeich 2009; Reference Norman, Byambaa and DeNorman 2012).
Dysfunction in the patient–doctor relationship
Attachment might also mediate the relationship between childhood trauma and MUS in adulthood through its effect on relationships with healthcare professionals from whom the person has to elicit care. Repetition of an insecure attachment pattern can lead to dysfunctional relationships with healthcare professionals that influence illness management and treatment adherence. Some people with MUS perceive healthcare professionals to be insufficiently caring, interested or concerned, just like their original carers. Some at the severe end of the spectrum have thick medical files because they go from doctor to doctor, repeating a complex and dysfunctional attachment relationship. Reference Maunder, Panzer and ViljoenMaunder et al (2006) found that the difficulties that doctors experienced with patients were related to the patients’ attachment styles.
The dysfunction in the caring relationship goes both ways: there is an extensive literature on the negative response of doctors to patients who ‘don’t or won’t get better’. Examples from general practice include the ‘heartsink’ patient (Reference O'DowdO’Dowd 1988) and the ‘hateful patient’ (Reference GrovesGroves 1978), and it is likely that hostility from healthcare professionals has a negative effect on the care offered to patients with MUS. Reference Salmon, Wissow and CarrollSalmon et al (2008) describe how doctors’ own attachment styles influence what they offer to patients with MUS.
Alexithymia
Another possible mechanism linking trauma, attachment theory and MUS is alexithymia: the inability to put feelings into words. There has been considerable study of whether people with psychosomatic disorders have higher than usual levels of alexithymia compared with normal populations; there is evidence both for and against the hypothesis (Reference KooimanKooiman 1998). Some researchers have postulated a general role for alexithymia in MUS, suggesting that it night be a mediating factor for somatisation in adults who have experienced childhood trauma (Reference Waldinger, Schulz and BarskyWaldinger 2006). Alexithymia may influence the way that patients with MUS can talk to healthcare professionals and thus adversely affect the medical relationship.
Interventions
At the primary care level in the UK, IAPT services offer brief interventions for MUS. A wide variety of psychological techniques have been shown to be of benefit (Reference Creed, Kroenke, Henningsen, Creed, Henningsen and FinkCreed 2011b), including cognitive–behavioural therapy, psychodynamic interpersonal therapy, mindfulness-based approaches and hypnosis. Multicomponent behavioural packages and antidepressants have also been successful.
Most of the psychological approaches involve working with the person’s physical symptoms and obtaining the person’s story of their illness and how it has affected them and their family. There is evidence that people with MUS in primary care may be receptive to ideas about stress as a causative factor and value doctors who can develop with them a shared understanding and model of illness. The cognitive–behavioural therapies tend to focus on developing positive coping strategies and encouraging physical function. Mindfulness-based cognitive therapy (MBCT) and mindfulness-based stress reduction (MBSR) have been shown to be helpful for both chronic depression and chronic pain, and they may therefore indirectly improve MUS (Reference Bohlmeijer, Prenger and TaalBohlmeijer 2010). Mindfulness-based practices may also help with MUS by improving regulation of negative affect and helping patients change their awareness and relationships with bodily experience and pain.
Another therapy that pays particular attention to ‘here-and-now’ bodily experience is psychodynamic interpersonal therapy (Reference HobsonHobson 1985). The focus is on ‘forms of feelings’. This notion involves not just emotions, but physical bodily feelings that connect with an image, idea or other similar experience. People are encouraged to stay with their ‘feelings’ in the session, so that these are experienced here and now, in the context of a relationship. As the forms of feeling develop, links emerge between physical experience, emotions and relationships.
Severe symptoms
At the more severe end of the spectrum, some people with MUS will experience their body as alien, uncomfortable or ‘sick’ in a variety of ways. Such people may feel hostility and/or fear in relation to their discomfort and distress, in addition to a sense of being overwhelmed and helpless. They may lack compassion towards their bodies and minds (Reference Raque-Bogdan, Ericson and JacksonRaque-Bogdan 2011) and experience anger with ‘carers’ who fail to relieve their distress. Reassurance, information and/or logical analysis alone are unlikely to transform such people’s experiences of bodily distress. What is needed is a ‘change of tack’, as described by Reference Bass and GlaserBass & Glaser (2014a), away from any sense of confrontation or challenge and towards a way of working that emphasises positive function and activity while also taking seriously attachment-based affects of anger, fear and hostility towards the self and others. Clinical experience suggests that more intensive therapies addressing underlying cognitive schema or affectful beliefs may be helpful, and in-patient treatment programmes using a range of interventions, including interpersonal and family work, have shown promise.
Patient-specific intervention
An appreciation of attachment theory suggests that it may also be important to offer different types of intervention to different groups, distinguished by attachment insecurity. Assessment of attachment style as part of a general assessment is likely to give some idea of how a person deals with their own dependency needs and relates to healthcare professionals. People with different attachment styles will respond in different ways to different interventions. Dismissing individuals may be unlikely to engage with any intervention that focuses on psychological distress, but they may accept interventions that address their physical experience, such as mindfulness practices, health information and exercise programmes. People with fearful and preoccupied attachment may respond better to an intervention that actively invites reflection on the link between their psychological distress, physical experience and childhood trauma.
A modified version of this approach is described by Reference Ciechanowski, Russo and KatonCiechanowski et al (2006a), who divided 324 patients with diabetes and comorbid depression into two groups: those with an insecure attachment (relationship) style, who were deemed ‘independent’; and those with a secure attachment style, who were deemed ‘interactive’. Patients in both groups were randomly assigned either to an intervention designed to improve quality of depression care or to care as usual. For patients deemed ‘independent’, the intervention resulted in significantly more pain-free days at 12-month follow-up compared with care as usual, whereas for patients deemed ‘interactive’ (i.e. with a secure relationship style) there was no significant difference in depression outcomes. The authors speculated that the secure group did not benefit from the programme of care because they were already able to do for themselves many of the things that were offered. The insecure patients, however, were not able to do these thing without help, and therefore got the most benefit from the intervention. The marked differences in outcome between the groups suggest that further work in this area would be of value. It may be that people with secure attachments require minimal input in relation to treatment, and we should be focusing attention much more on people with insecure attachment styles. This is the only study of which we know that has examined differential response rates to therapy according to attachment status.
Somatising disorders in parents
It is vital that parents with somatising disorders are identified and treated early, especially mothers who are largely responsible for their young children’s healthcare and interactions with healthcare professionals. There is evidence of transmission of somatising behaviours and health beliefs across the generations (Reference Craig, Cox and KleinCraig 2002; Reference Marshall, Jones and RamchandaniMarshall 2007), and children who are frequent attenders in primary care tend to have parents who have complex relationships with healthcare providers (Reference Little, Somerville and WilliamsonLittle 2001). A subgroup of mothers with somatising disorders form highly dysfunctional relationships with professional carers and expose children to unnecessary examinations, investigations and treatments (Reference Bass, Acosta, Adshead and Huline-DickensBass 2014b).
Conclusions
There is extensive evidence that attachment security influences how people experience their body on a day-to-day basis; how they interpret pain or dysfunction; how they manage stress associated with illness; and how they relate to caregivers, both personal and professional. Attachment style can buffer or increase the perceived stress of illness (either explained or unexplained) and can influence response to psychological interventions aimed at reducing MUS. Attachment style may mediate between childhood abuse and adult somatisation. Consequently, when assessing patients who struggle with physical illness, it is essential to take an extensive developmental history that addresses not only childhood experience of loss and stress, but also histories of illness and distress in the family. Clinicians need to develop interventions that ‘fit’ the attachment narratives of individual patients, rather than forcing patients into one-size-fits-all psychological therapeutic techniques.
MCQs
Select the single best option for each question stem
-
1 The prevalence of medically unexplained symptoms (MUS) in primary care is:
-
a 0–0%
-
b 10–15%
-
c 10–30%
-
d 30–55%
-
e 50–70%.
-
-
2 High rates of MUS have been reported in:
-
a paediatrics
-
b dermatology
-
c obstetrics
-
d neurology
-
e pathology.
-
-
3 In human interactions, the attachment system is not activated in:
-
a loss events
-
b threat of injury events
-
c situations of vulnerability
-
d educational events
-
e situations where authority is exerted.
-
-
4 Which of the following is not an empirically based attachment pattern in adults?
-
a secure
-
b insecure avoidant
-
c insecure ambivalent
-
d insecure fearful
-
e insecure toxic.
-
-
5 In interactions with healthcare professionals, attachment style has been shown to be irrelevant in relation to:
-
a complaints
-
b adherence to medication
-
c attendance at appointments
-
d therapeutic engagement
-
e requests for pain relief.
-
MCQ answers
| 1 | c | 2 | d | 3 | d | 4 | e | 5 | a |





eLetters
No eLetters have been published for this article.