There is continuing interest among researchers and policy-makers in the relationship between cannabis use and schizophrenia. Reference van Os, Bak, Hanssen, Bijl, de Graaf and Verdoux1-Reference Moore, Zammit, Lingford-Hughes, Barnes, Jones and Burke3 This has revived interest in the nature of the conditions that attract the clinical diagnosis of drug-induced psychosis. Reference Curran, Byrappa and McBride4 The concept of drug-induced psychosis has been criticised Reference Poole and Brabbins5 and it remains unclear whether the diagnosis reflects a valid diagnostic category or whether it is based on arbitrary assumptions regarding the causation of symptoms. A systematic review concluded that the inference of causation is not secure and that the condition would be better understood in terms of an association. Reference Mathias, Lubman and Hides6 One possible criterion for the validity of a diagnostic category is stability during periods of follow-up, at least in the short term. This study aims to assess the extent to which the clinical diagnosis of drug-induced psychosis remains stable over a follow-up period of at least 2 years.
Method
The study was conducted in a large National Health Service mental health trust in the north-west of England, with a predominantly urban catchment area. It contains areas of urban social deprivation as well as more prosperous suburbs and coastal towns.
The trust's IT department records ICD-10 diagnoses 7 on all patients under the care of the mental health service. After an in-patient admission, diagnosis is recorded by the patient's psychiatrist, normally the consultant. Where there is no ICD-10 code recorded in the discharge summary, trained coders assign a code on the basis of the clinical diagnosis. In cases of ambiguity, coders clarify the diagnosis by contacting the treating clinician.
The IT system was used to identify all patients experiencing first-episode drug-induced psychosis (ICD-10 codes F10.5-F19.5) following an in-patient admission ending between January 2002 and April 2006. Clinical information about each patient was then gathered by two researchers (A.K. and R.H.) from the IT computer system and from mental health service case records, with particular reference to alterations in diagnosis. Data were collected from May 2008, generating follow-up data for a minimum of 2 years or until discharge from specialist mental health services.
Patients were excluded from the study if they had been given any psychiatric diagnosis before the index diagnosis of drug-induced psychosis, if they had been unintentionally lost to follow-up within 2 years of the index admission (e.g. if they moved away from the area) or if there was insufficient information in their case records to assess the stability of the diagnosis (e.g. where clinical records had been lost). The most recent clinical diagnosis made in the case record by a senior psychiatrist was regarded as the ‘outcome diagnosis’.
Results
Overall, 98 in-patients were diagnosed with drug-induced psychosis in the study period. Twenty were excluded from analysis: ten had a previous psychiatric diagnosis, four were lost to follow-up because they were sent to prison and one was lost because they moved away, and there was insufficient clinical information available on five patients. The initial ICD-10 diagnoses of patients included in the study are set out inTable 1.
Table 1 Index diagnosis of patients included in study (n = 78)
| ICD-10 coding | Psychotic disorder due to the use of | n (%) |
|---|---|---|
| F12.5 | Cannabis | 32 (41) |
| F19.5 | Multiple drugs | 22 (28) |
| F14.5 | Cocaine | 14 (18) |
| F15.5 | Amphetamines and other stimulants | 6 (8) |
| F10.5 | Alcohol | 3 (4) |
| F16.5 | Hallucinogens | 1 (1) |
Of the 78 patients included in the analysis, 55 were male and 23 were female. Thirty-two patients (41%) were discharged to general practitioner (GP) care within 2 years of diagnosis and only one of these patients was re-referred to specialist mental health services after discharge to GP.
At the time of data collection 46 patients were still in follow-up (‘retained patients’). This generated follow-up periods of between 2 and 6 years. Only five patients had an outcome diagnosis of drug-induced psychosis. In the case of a further five patients the outcome diagnosis was unclear from the clinical notes. Just over half of the retained patients (31% of patients included in the study) had a firm outcome diagnosis of schizophrenia or schizoaffective disorder. Outcomes at each stage in the study are summarised in Fig. 1 and the outcome diagnoses of the retained group are shown inTable 2.
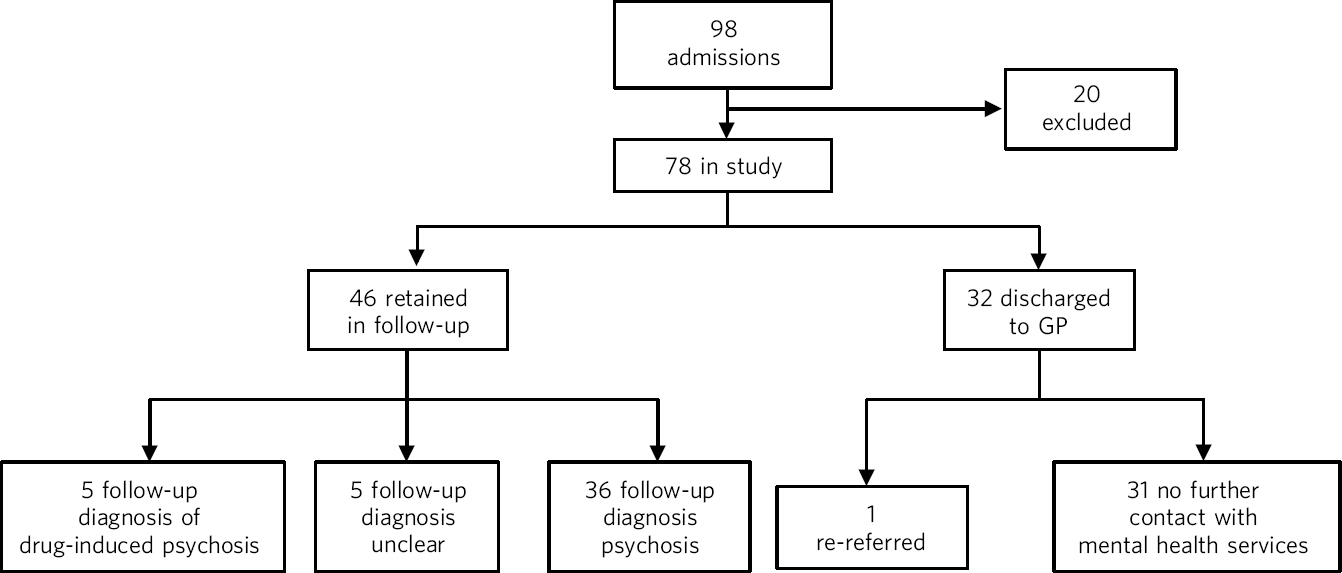
Fig 1 Flow chart of patient outcomes. GP, general practitioner.
Table 2 Outcome diagnosis of patients retained in follow-up (n = 46)
| Diagnosis | Number | Percentage of total sample (N = 78), % |
|---|---|---|
| Schizophrenia | 18 | 23 |
| Schizoaffective disorder | 6 | 8 |
| Drug-induced psychosis | 5 | 6 |
| Bipolar affective disorder | 4 | 5 |
| Psychosis not otherwise specified | 4 | 5 |
| Acute and transient psychosis | 3 | 4 |
| Delusional disorder | 1 | 1 |
| Diagnosis unclear | 5 | 6 |
Mean duration of the index admission for patients subsequently discharged to primary care follow-up was 14.4 days (median 11, range 1-54) and for patients retained in follow-up it was 20.4 days (median 16, range 1-76). This difference is statistically significant (Mann-Whitney U-test, P = 0.05).
Thirty-two of the patients were diagnosed with psychosis induced by cannabis and 23 of these were retained in follow-up. Only one had an outcome diagnosis of drug-induced psychosis and in four cases there was no clear diagnosis. The most common outcome diagnosis was schizophrenia.
Further, 46 patients were diagnosed with psychosis induced by drugs other than cannabis or by poly-drug misuse; 23 were retained in follow-up. Four had a current diagnosis of drug-induced psychosis and 18 had a different current diagnosis, predominantly schizophreniform disorder. In one case there was no clear current diagnosis.
Of the 22 patients who were diagnosed with psychosis due to poly-drug misuse, 12 were retained in follow-up. Three had a current diagnosis of drug-induced psychosis whereas nine had a current diagnosis of a different psychosis, predominantly schizophreniform disorder.
There was no statistically significant difference in the proportion of patients retained in follow-up between psychosis attributed to cannabis, other drugs or poly-drug misuse (non-parametric χ2, P = 0.129).
The use of the diagnosis of drug-induced psychosis increased during the study period. The rate of new diagnosis from 2002 to 2004 appeared stable at approximately 1 per month (s.d. = 0.6). In 2005 this increased to 2.5 per month. The rate for the first 4 months of 2006 was 3 per month. It should be noted that a new service for early intervention with adolescents at risk of psychosis became operational in March 2005. The proportion of patients that were retained in follow-up for at least 2 years increased in the later period: from 2002 to 2004, 48.6% were retained in follow-up, but among patients diagnosed after 1 January 2005, 67.4% were retained in follow-up.
Discussion
Comparison with other studies
Our findings are consistent with two similar studies, one from the USA Reference Caton, Hasin, Shrout, Drake, Dominguez and First8 and one from the UK. Reference Crebbin, Mitford, Paxton and Turkington9 Our follow-up was longer than that in the US study and our sample was larger than the sample in the UK study, although both studies had methodological advantages over ours. Our findings suggest that in-patients diagnosed with drug-induced psychosis on first presentation to mental health services fall into two groups of approximately equal size. The first group appear to make a prompt recovery and, once discharged by services, are not re-referred for specialist care over the next few years. The second group have a longer index admission, are retained in long-term follow-up, and are very likely to have a change in diagnosis to a functional psychosis, most commonly schizophrenia.
Our findings are also consistent with those reported in a large study of cannabis-induced psychosis using data from the Danish Psychiatric Central Register. Reference Arendt, Rosenberg, Foldager, Perto and Munk-J⊘rgensen10 Compared with that study, our sample is relatively small, but it does allow some comparison of episodes attributed solely to cannabis with other drug-induced psychoses. Although there was a non-significant trend for more patients with cannabis-induced psychosis to remain in follow-up, half of the patients where a different drug, or poly-drug misuse, was implicated also remained in follow-up. There was no statistically significant difference between the patients with cannabis-induced psychosis and other drug-induced psychosis in the pattern of diagnostic change when those patients were retained in follow-up.
It is well established that there is an association between cannabis use and schizophrenia. Reference Regier, Farmer, Rae, Locke, Keith and Judd11,Reference Zammit, Allebeck, Andreasson, Lundberg and Lewis12 However, the causal link between drug use and drug-induced psychosis rests on an assumption of causality made by the clinician and that assumption may be wrong. It is possible that the initial presentation in the retained group was causally related to drug use, and that the disorder then evolved into persistent functional psychosis. It is equally possible that the patients who were eventually diagnosed with functional psychosis were actually experiencing that disorder all along, and that drug use was simply a complicating factor. In contrast with many other authors who have written on this subject, we believe that the latter interpretation is as plausible as the former, and should be taken just as seriously as a hypothesis. It has the advantage of compatibility with Occam's razor.
Limitations
There remains a large group, roughly half of our sample, who were discharged from follow-up. The major limitation of our study is that we collected very limited information on these individuals after discharge to primary care - all we could record was their utilisation of local secondary mental health services. This group tended to have shorter admissions. It is impossible to make a definitive statement regarding clinical outcome for them. However, it seems unlikely that many of them had a further acute and florid psychotic episode during the study period. The most plausible explanation for their index episode is that they experienced transient psychotic symptoms due to intoxication with drugs and that the symptoms subsided once the drug was eliminated. If this inference is correct, then these individuals did not experience drug-induced psychosis but acute drug intoxication.
Our study has some further limitations. Data were collected post hoc from case notes and the clinical IT system. We did not collect comparative data regarding the stability of diagnosis in patients who had not taken drugs. Of the original 98 patients, 10 were excluded because there was inadequate information available. In a further five cases, the outcome diagnosis was unclear. However, it seems unlikely that these limitations or causes of missing data created a bias that would invalidate our principle findings.
It was suggested more than a decade ago that the clinical diagnosis of drug-induced psychosis is heterogeneous, based on an inference regarding causality of uncertain validity and potentially misleading. Reference Poole and Brabbins5 Our interpretation of our findings, together with similar studies, would tend to support these assertions. It was also predicted that, despite these problems, the diagnosis was likely to continue to be used. Our study clearly confirms this prediction and even shows that the use of the diagnosis may be increasing.
Clinical implications
The main clinical implication of our study is that a significant proportion of patients presenting with apparent drug-induced psychosis experience long-term mental health problems, and that this may be especially true when initial psychotic symptoms are slow to resolve. This suggests that psychosis should be attributed to drug misuse with caution and that the expectation that further episodes can necessarily be prevented solely through avoidance of drug misuse is unrealistic in a high proportion of cases.
Acknowledgement
We are grateful to Sarah Jennings for her assistance with the statistical analysis.






eLetters
No eLetters have been published for this article.